Abstract
From 30 November to 3 December 2010, the 14th edition of the International Symposium on Progress in Clinical Pacing was held in Rome. During this event, experts in the field of electrophysiology and cardiac pacing had the opportunity to meet and exchange their opinions, with the aim of discussing the results of recent studies and to outline future perspectives. In this edition of the congress there was a large attendance of electrophysiologists and clinical cardiologists, with more than 2300 delegates attending from over 50 countries and more than 400 faculty members. The conference was sponsored by the major international arrhythmological scientific societies, including the Heart Rhythm Society, the European Heart Rhythm Association, the Sociedad Latinoamericana and the Asia-Pacific Heart Rhythm Society. In parallel with the medical conference, the fifth edition of the ‘Advanced Course of Electrophysiology and Cardiac Pacing’, dedicated to cardiological nurses and technicians, was held. The role of the nurse is becoming increasingly important in clinical practice in order to replace physicians in performing noninvasive procedures.
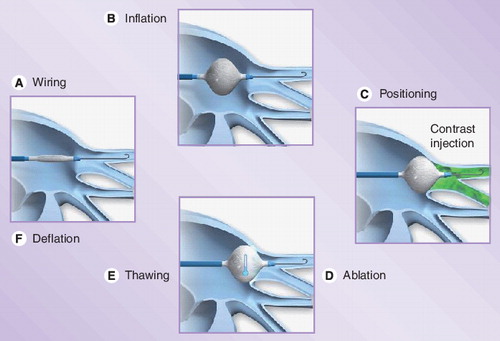
Figure provided courtesy of Medtronic (MN, USA).
During the opening ceremony, held on the first day of the congress, two magistral lectures on relevant and debated arrhythmological topics were presented. The first, given by Stuart Connolly (McMaster University, ON, Canada), dealt with the complications, mainly thromboembolic, of atrial fibrillation (AF) and their prevention strategy. Connolly presented an interesting overview of the most frequent complications of AF encountered in clinical practice, exhaustively describing the strategies that were used in the last two decades and the possible future perspectives. The second lecture was given by Arthur Moss (University of Rochester Medical Center, NY, USA), one of the greatest experts in sudden cardiac death prevention. During his lecture he gave a broad and detailed overview of the major randomized clinical trials on sudden death prevention by implantable cardioverter defibrillator (ICD) implant during the last 10 years.
During the four congress days, all the current issues were debated by the faculty members, ranging from the pathophysiology of cardiac pacing to new devices, which will very likely be used in the coming years and will lead a real revolution in the field. One of the hottest topics, discussed in more than one session, focused on the optimization of cardiac output by pacing. After the description of cardiac physiology in normal and decompensated hearts, with particular attention to the interatrial, atrioventricular (AV) and intraventricular (VV) intervals, the central part of the topic concerned the description of some physiological sensors that have the ability to monitor and regulate ventricular contractility and heart rate. Such devices may also find a specific use in cardiac resynchronization therapy (CRT) in order to optimize some programmable parameters, such as AV and VV intervals, which may change over time in the same patient. Another factor responsible for the deterioration of cardiac output during cardiac pacing is left ventricular desynchronization induced by artificial stimulation. This aspect has been definitively identified after the analysis of large randomized, prospective studies comparing dual-chamber pacemaker with single-chamber pacemaker pacing (DANISH, Canadian Trial of Physiological Pacing, Mode Selection Trial). Two strategies have been proposed in order to prevent this deleterious effect:
• The development of algorithms that are able to minimize the percentage of ventricular pacing to be used in patients in whom AV conduction is good;
• The identification of alternative ventricular pacing sites, which allow a significant reduction of the left ventricle desynchronization in patients with impaired AV conduction.
The algorithms cited earlier were described analytically by several scientists who detail the specific characteristics of each. With regard to the alternative ventricular pacing sites, the right ventricular outflow tract seems to be the most promising, mainly due to the relatively easy achievement with the currently available leads . However, no conclusive data on the superiority of right ventricular outflow tract with respect to right ventricular apex pacing could be given. An alternative promising site, although difficult to implement in clinical practice, could be the direct stimulation of the His bundle. Unfortunately, owing to the small amount of available data and the difficulty in achieving the correct lead positioning, the judgment on this pacing site is still very controversial.
Cardiac resynchronization therapy was also one of the most debated topics, with particular interest in the selection of candidates and in alternative techniques for left ventricular lead delivering and positioning (trans-septal, transapical and subxifoideal approaches). These new techniques allow a higher success rate, particularly in reaching the optimal pacing site in each individual patient. The problem of ‘nonresponders’ to CRT, in fact, is still a real challenge in this heart failure treatment and has been discussed widely in several sessions. The most common new implant indication to CRT was confirmed to be in patients with wide QRS and good functional class. On the other hand, AV node ablation in CRT patients with permanent AF may also be considered a valid therapeutic strategy. Finally, great interest arose during the debate concerning the association of defibrillation function and CRT. This issue, in fact, was debated not only with regard to clinical benefits, but mainly to ethical and religious issues. Certainly, in the near future this aspect will trigger much more debate.
In nearly all the sessions on ICDs, it emerged that these devices are being progressively transformed from life-saving tools, only able to recognize and treat a life-threatening ventricular tachyarrhythmia, to monitoring instruments useful in optimizing drug therapy and anticipating adverse events. In the new devices, mainly in those with CRT function, diagnostic capabilities have been significantly improved, particularly those dedicated to the early detection of chest fluid accumulation. Another important diagnostic feature, recently introduced and arousing considerable interest in the dedicated sessions, was the capability of the ICD to detect myocardial ischemia by analyzing changes in the intracavitary ST segment, allowing an early detection of silent ischemic events and early treatment. The ST segment changes are evaluated by looking at the intracavitary electrogram, recorded several times a day and compared with a baseline, in order to catalog the deviations that exceeded a threshold value. The available data on algorithm sensitivity and specificity are now limited, but it is easy to predict that, if the reliability of the system is confirmed, the clinical applications will be wide ranging and would radically alter the management of patients.
The diagnostic functions of implanted devices have gradually improved with the changing of device periodic controls. Currently, in fact, periodic monitoring of the devices is performed at previously scheduled visits, which often leads to a delayed diagnosis of clinical changes and/or system malfunctions (recall, device advisory), and a delay in assessing the therapeutic effects of pharmacological changes, as well as a waste of time and an inconvenience for patients. The remote control has been introduced through the use of computer and telecommunications technology; this synergic use allows the performance of periodic remote controls and to receive warning of events classified as hazardous (alert). In the scientific sessions dedicated to the devices remote control, the discussion focused mainly on two aspects:
• Optimizing the system, in order to obtain the most detailed information on the patients clinical status;
• Solving the difficulties, mainly administrative and organizational, that are still present and that limit the widespread use of remote controls.
Regarding the first point, the two main diseases that can be better managed with the remote control are AF and heart failure. AF can sometimes be asymptomatic or minimally symptomatic; therefore, its management with antiarrhythmic or rate-control drugs and, more importantly, with anticoagulants, is often delayed. All the speakers stressed that, through the daily transmission of data on atrial function, it is possible to manage this arrhythmia effectively, primarily by reducing the incidence of stroke. Regarding the second point, it was widely noted that biventricular ICDs and pacemakers, able to broadcast informations on the patient’s overall compensation (such as the average heart rate at rest, heart rate variability, the hours of physical activity, the daily burden of AF and ventricular ectopic activity), can greatly facilitate the management of drug therapy. Finally, it was widely emphasized that the benefits of individual patients go together with the improvement of the whole system. More specifically, it is possible to obtain an optimization of resources dedicated to patient monitoring, an improvement of in-hospital access management, an increased appropriateness and quality of periodic controls and, finally, a better time management of health operators. The difficulties mentioned earlier are inherent in the organizational aspect, in the economic reimbursement, and in medical–legal liability. Because the device’s remote control is currently limited a to few implanting centers and to a small number of patients, a standard organizational model is still lacking. For this reason, the discussion between the experts on this topic was very vivid and interesting for all participants. Similarly, the comparison between different countries with regard to the reimbursement (not yet approved in all countries) has enabled a fruitful discussion among the physicians.
Atrial fibrillation was the subject of several sessions and its treatment, both pharmacological and electrical, together with the prevention of its complications, mainly thromboembolic, have been the focus of heated debates. The discussion of drug treatment was mainly focussed on new drugs, such as dronedaron and dabigatran. Regarding the former, after promising early data, initial enthusiasm has slightly cooled, so that the various speakers not only described the potential of this drug, but also underlined its limitations. On the contrary, dabigatran was given a warm reception. After the demonstration of its substantial equivalence to anticoagulation therapy in the prevention of thromboembolic complications of AF, all the speakers called for its rapid introduction into clinical practice.
The electrical therapy of AF consists mainly of conventional ablation with radio frequency (RF). However, when applied to AF this procedure is successful only in a limited percentage of cases. For this reason, variations are often proposed to the classical use of RF. During the sessions dedicated to this procedure, the attention focused primarily on phased RF, cryoablation and surgical ablation. The speakers described the engineering properties of phased RF catheters, particularly for electrical isolation of pulmonary veins and/or linear ablation, or for treatment of fragmented potentials. These catheters are inserted into the left atrium with a single atrial septal puncture with trans-septal catheterization. With a single electrode it is possible to map, pace and deliver RF; in particular the delivery of RF can occur simultaneously from all electrodes or from selected matched pairs. Furthermore, each catheter has a shape designed to reach very specific anatomical sites, which, on the basis of the literature, are those containing the foci responsible for AF maintenance.
The clinical use of these catheters has many advantages in terms of efficacy and safety. Given the large contact surface, the novel placement of temperature sensors and the delivery alternating between unipolar and bipolar, low energy is sufficient to reach the temperature required to produce the lesion. This feature avoids the phenomena of carbonization, perforation and/or esophageal damage, reducing the risks related to the procedure. Moreover, the possibility of delivering RF simultaneously from more electrodes results in a reduction of ablation time. Finally, these catheters do not necessarily require the use of a 3D-mapping system. This last feature is also common to cryoablation. During the meeting, many lectures were presented on this topic in order to compare the various experiences with these two new ablation techniques. The basic difference between the cryoablation and the conventional or phased RF is the use of cold rather than hot temperature. In addition, catheters designed as balloons may be more effective and safe to use for circumferential ablation. Briefly, an over-the-wire catheter with an inner and an outer balloon is inserted into the left atrium. After positioning the guidewire in the distal part of a pulmonary vein (PV), the deflated balloon catheter is advanced to the PV ostium. Using the central balloon marker, the balloon position in the vein can be estimated before inflation. Once positioned, the balloon is inflated and pressurized liquid N2O is delivered to the catheter tip. By sudden expansion of the liquid gas, it evaporates and absorbs heat from the adjacent tissue and low temperatures are achieved down to -80°C. To ensure good balloon PV antrum contact, an occlusion PV angiography is performed via the central lumen of the catheter. If optimum pulmonary venous occlusion is achieved, cryoablation is started for at least 5 min. The most crucial issue with circumferential cryoablation is achieving an optimum contact between the balloon and PV antrum. Finally, surgical ablation probably represents the last frontier of AF ablative therapy. The development of different mini-invasive surgical ablation techniques for ‘lone-AF’ has allowed a success rate ranging from 50 to 100%, with low complication incidence. The European Society of Cardiology (ESC) guidelines still do not give clear indications on surgical ablation, owing to few available clinical data. In patients who are candidates for major surgical interventions, such as mitral valve replacement/repair or coronary artery bypass graft, the ESC recommends to concomitantly perform the surgical ablation in all the patients if there are low additive risks and reasonable success chances since AF is an independent risk factor for increased post-surgical mortality. Furthermore, standalone AF surgery should be considered for symptomatic AF patients who prefer a surgical approach, have failed one or more attempts at catheter ablation, or are not candidates for catheter ablation. The procedure includes pulmonary vein isolation, ganglionic plexi ablation, Marshall ligament resection and left atrial appendage exclusion by means of minimally invasive bilateral thoracoscopy (a 6.0-cm incision in the third or fourth right intercostal space and a small incision on the midaxillary line in the sixth intercostal space for the camera port). The most interesting issue that emerged from many lectures concerned the organizational problems that must be solved in order to promote the spread of this therapeutic strategy and make it easy to reach fruition. Currently, while ECG laboratories are increasingly overloaded, cardiac surgery operating rooms are underemployed. An appropriate centralized ‘AF unit’ could provide an optimized management strategy for patients with AF, based on a constant cooperation between cardiology and cardiac surgery departments aimed at providing the optimal therapy for each patient.
Some sessions were dedicated to the spread of now technologies, which were mainly dedicated to the cardiac pacing or other devices able to obtain diagnostic data. Regarding the pacing devices, early experiences were presented about the use of systems, which, using echo waves at specific frequencies, can induce the contraction of the heart, and, therefore, do not require an endocardial catheter. Similarly, a new type of ICD, which uses the dipole created between the case, placed in the axillary region, and a coil in a subcutaneous precordial position, was presented. In addition, this device does not require any endocardial lead and could result in a drastic reduction of complications and a more straightforward management of infections. These devices are still under clinical evaluation and can be used only in clinical trials. Conversely, the wearable defibrillator is now available and represents a very interesting bridge system for patients with low ejection fraction and recent myocardial infarction or after a revascularization procedure, until the implantation of a permanent device. The wearable defibrillator would also be useful in patients who undergo complete removal of the ICD system before the new implant. Finally, in a more futuristic vision, a so-called ‘Innovation Village’, where some very pioneering devices were exposed, was set up in the exhibition area and proved very popular among attendees. Certainly these innovations will be the subjects of the next edition of Progress in Clinical Pacing in 2012.
Financial & competing interests disclosure
Massimo Santini is an investigator and speaker for Medtronic, St Jude Medical and Biotronik. Carlo Pignalberi is an investigator for Medtronic. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.