Abstract
Background
Lower- and middle-income countries (LMICs) are disproportionately impacted by human papillomavirus (HPV) and would benefit from implementing the HPV vaccine. In the context of competing health priorities, utilizing scarce domestic infrastructure and human resources for HPV vaccination remains challenging for many LMICs. Given the high benefits of the HPV vaccine, the World Health Organization (WHO) is now encouraging for all countries, particularly LMICs, to introduce HPV vaccines into their routine immunization programs. Understanding the barriers and facilitators to HPV adolescent vaccine programs in LMICs may help strengthen how LMICs implement HPV vaccine programs, in turn, increasing HPV vaccine acceptance, uptake, and coverage.
Objective
To identify and assess barriers and facilitators to implementing adolescent HPV vaccination programs in LMICs.
Methods
This study comprised a review of literature assessing adolescent HPV vaccination in LMICs published after 2020 from a sociocultural perspective.
Results
Overall, the findings showed that LMICs should prioritize increasing HPV vaccine availability and HPV vaccine knowledge, particularly focusing on cancer prevention, as knowledge reduces misinformation and increases vaccine acceptance. Evidence suggests that factors promoting HPV vaccine uptake include fostering low vaccine hesitancy, integrating HPV vaccination as a primary school routine vaccination, and vaccinating both genders. A one-dose HPV vaccine may enable many LMICs to increase vaccine acceptance, uptake, and coverage while controlling financial, infrastructure, and human resource costs.
Conclusion
As HPV is one of the leading causes of death in many LMICs, implementing the HPV vaccine may be highly beneficial. Cohesive national HPV vaccine buy-in and understanding the success and challenges of prior LMIC HPV vaccine implementation is crucial to developing effective, efficient, and sustainable HPV vaccination programs.
Introduction
People in low- and middle-income countries (LMICs) suffer disproportionately higher incidence and mortality rates from cervical cancer and other human papillomavirus (HPV)-associated cancers, including oropharyngeal and anogenital cancer compared to high income countries.Citation1 Approximately 84% of new cervical cancer cases and between 80% and 90% of cervical cancer deaths occur in LMICS.Citation1,Citation2 Cervical cancer is the second most common cancer among women in LMICs and is the most common cancer in half (23/46) of the countries in sub-Saharan Africa.Citation3 Without utilizing preventative measures to decrease HPV, deaths in LMICs from cervical cancer is projected to increase by 50% by 2040.Citation4
The HPV vaccine is one of the most cost-effective primary prevention tools against cervical cancer as it can protect against 70% to 90% of all HPV-attributable cancers.Citation5 The HPV vaccine may have a particularly significant impact on the burden of HPV-associated cancers in LMICs where screening is sparse or non-existent, limited in scale, or of poor quality.Citation6 While robust research has supported the HPV vaccine’s safety, efficacy, and cost-effectiveness, there has been limited HPV vaccine implementation, particularly in LMICs. Clinical interventions in LMICs have found that vaccinating against HPV can reduce cervical cancer cases by 50% to 75%.Citation7 Every five-year delay in HPV vaccine roll-out contributes to 2 million cervical cancer deaths.Citation8 The HPV vaccine needs to be given promptly to adolescents as the vaccine is most effective against HPV-related disease outcomes when given at younger ages.Citation9 As less than 25% of LMICs have introduced the HPV vaccine into their immunization schedules, the need for timely implementation of the HPV vaccine to adolescents within LMICs is substantial.Citation4 Given the benefits of the HPV vaccine, WHO is now encouraging for all countries, particularly LMICs, to introduce HPV vaccines into their routine immunization programs.Citation10,Citation11
Formative research has identified three major barriers to the HPV vaccine’s introduction into LMICs: sociocultural, health system, and political.Citation12 Studies or reviews focusing primarily on understanding the socio barriers and facilitators holistically in LMICs are scarce.Citation13,Citation14 By synthesizing findings from the literature review on HPV vaccine implementation in LMICs, this paper considers barriers and facilitators that could improve HPV vaccination uptake among adolescents from a sociocultural and socioeconomic perspective. A socio perspective is influenced by individuals’ beliefs, expectations, subjective norms, and attitudes towards health and the healthcare service, which determines their utilization of services.Citation15
This review examined steps to enhancing HPV vaccine uptake among adolescents in LMICs using a sociocultural and socioeconomic lens. The review considered HPV knowledge and misconceptions, societal values and stigma, and cost-benefit perception and attitude. Models such as HBM, social norms, and social determinants were used to focus on the social aspect of addressing HPV vaccine uptake.
Materials and Methods
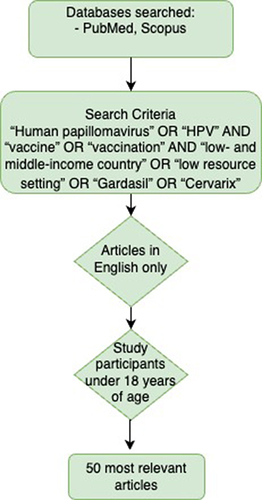
The authors conducted a rapid review of the empirical evidence on HPV vaccination programs in LMICs from a sociocultural and socioeconomic perspective. A literature review of relevant articles identified through a search of electronic databases on PubMed, and Scopus using the following title search terms: “Human papillomavirus” OR “HPV” AND “vaccine” OR “vaccination” AND “low- and middle-income country” OR “low resource setting” OR “Gardasil” OR “Cervarix”. The search was restricted to English language items published since 2020, the year the United Nations started actively promoting that all countries should have 90% of girls fully vaccinated with the HPV vaccine by 15 years of age and created consistent HPV vaccination guidelines.Citation10,Citation16 provides a flowchart of the search strategy.
Articles focusing solely on high income countries were excluded; however, items that included a mix of high- and low-income countries were included for thematic analysis. The World Bank classification system was used to define country income groups.Citation17 The articles were restricted to include only children and adolescents, defined as those under 18 years of age. We included literature that reported HPV vaccine implementation, including pilot projects in LMICs. The authors reviewed the 50 most relevant peer-reviewed qualitative and quantitative scientific literature on sociocultural and socioeconomic barriers and facilitators that could improve HPV vaccination uptake among adolescents in low-resource settings.
Through a theory-driven approach, several psychosocial models have been understood to enhance sociocultural behavior change for vaccine uptake. For this review, we employed the Health Belief Model (HBM), which focuses on beliefs regarding the presence of a threat and the potential actions to address that threat.Citation18,Citation19 Also critical in HBM is considering the perceived susceptibility of the adverse health outcomes compared to the perceived barriers.Citation20,Citation21 HBM can be supplemented with the social norm’s framework and the WHO social determinants of health model to influence HPV vaccine uptake.Citation21–23
Results
Low HPV and HPV Vaccine Knowledge and Misconceptions
Despite the WHO recommending that all countries should have 90% of girls fully vaccinated with the HPV vaccine by 15 years of age, low knowledge of HPV remains a challenge in enhancing vaccine uptake.Citation24–26 Many individuals may not know that HPV is associated with the prevention of cervical and other cancers.Citation14 In Uganda, there is low HPV vaccine uptake despite it being free of charge because of the lack of education materials on HPV vaccination available to adolescents and parents such as education about cervical cancer, prevention, and HPV vaccination benefits.Citation25 Health stakeholders should ensure HPV vaccine information is accessible to those with higher socio-economic status and those with less opportunities to access health knowledge and support resources. In Tanzania and Senegal, HPV health literacy is associated with reduced understanding of the need to vaccinate, increased risk of vaccine misinformation, and negative HPV vaccine attitude.Citation14
Without clear, consistent, transparent communication about vaccine risks and benefits, misinformation about the vaccine is shared among community members, creating poor HPV vaccine attitude and uptake. HPV vaccine hesitancy stemming from misinformation is often the primary reason parents and adolescents decline vaccination.Citation27 Common parental and adolescent concerns of side effects stem from misinformation such as the HPV vaccine being a birth control method, potentially leading to fertility issues and sterilization of adolescents, and it can even cause cervical cancer.Citation28–30 There is also the misconception that cervical cancer is caused by witchcraft and prevention by witch doctors and traditional medicine could substitute for the HPV vaccine.Citation31 Health stakeholders should prioritize addressing vaccine hesitancy and misconceptions through increasing vaccine knowledge. Parent and adolescent knowledge about the HPV vaccine, particularly its cancer prevention benefits and its effectiveness in adolescents’ early years, were associated with enhancing positive vaccine attitude, trust, uptake, and coverage.Citation26,Citation29,Citation31–34 To address the low HPV knowledge and awareness, culturally sensitive education and community vaccine promotion is critical.
Word of mouth communication about the HPV vaccine was most effective at reaching caregivers and adolescents, and increasing HPV vaccine uptake.Citation35 HPV health literacy and vaccine information should be provided by multiple trust worthy sources and integrated into other health communications for the greatest accessibility and reach.Citation36 Initially, HPV vaccine education support should prioritize health workers, such as providers, nurses, and community health workers, as they are the most preferred source of vaccine information and markedly influence vaccine uptake decisions. Health workers should receive training on optimizing their presentation of HPV vaccine information.Citation25,Citation37 Greater health worker knowledge and education on the importance of the HPV vaccine may also encourage clinician reminders about the vaccine and improve patient-provider vaccine communication. As communication needs to be tailored to the community’s concerns, local community mobilized social support and advocates such as parents, village, and religious leaders may serve to increase knowledge and decrease misinformation.Citation38 Training teachers from schools on basic health topics to become school health vaccine coordinators greatly supported HPV vaccination campaigns.Citation35 For long-term HPV health literacy sustainability, peer influence is key to vaccine uptake as many adolescents who had completed the HPV vaccine on time were encouraged to do so by their peers.Citation29 Empowering women within the community as HPV vaccine leaders may ensure continuous HPV communication with less misinformation within the community, increasing the likelihood of sustained vaccine uptake and completion.Citation14
Societal Values and Stigma
There are many societal values and stigmas that challenge HPV vaccine uptake.
As HPV is a sexual infection, the conversation surrounding HPV often evokes negative moral connotations in many communities, decreasing HPV vaccine discussion and uptake. Sexually conservative countries that have sensitivities regarding the dissemination of sex-related information often face barriers to enabling the wide reach of vital sexual health practices for families and communities. Cultural taboos may view premarital sexual intercourse as deviant behavior and uphold the norms of sexual abstinence before marriage, particularly for girls. As a result, the widespread prioritization and discourse on providing HPV vaccine for girls and decreasing cervical cancer may detrimentally affect the perception and uptake of the vaccine. Even seeking the HPV vaccine may be stigmatized as it may connote that the adolescent is already sexually active or desiring to engage in premarital sex.Citation13 Gender-specific immunization has been historically challenging and has resulted in many stigmatizing HPV rumors targeted toward girls.Citation39,Citation40 It may not be best for HPV vaccine campaigns to focus solely on vaccinating girls and prioritizing reducing cervical cancer as the main goal of the vaccine. Focusing on communicating the HPV vaccine’s cervical cancer benefits increases the stigma that HPV is a female disease and places the blame and burden of the issue on females when both genders could benefit.
Boys are rarely considered for HPV vaccination despite many male-related HPV cancers, creating a large HPV vaccination gap. The lack of encouraging male HPV vaccine participation may further stigmatize HPV as a female disease. As there are no significant gender differences in the safety and effectiveness of HPV vaccines and with the high likelihood of cross-infection of HPV to females, vaccinating only girls unfairly shifts the responsibility for preventing HPV predominantly onto women.Citation41,Citation42 When vaccination rates among women are high, men receive secondary protection and receive the benefits of the vaccine without participation; however, this places unnecessary vaccine burden and stigmatization on women. Adolescent boys are willing to vaccinate once they obtain knowledge of the HPV vaccine’s effectiveness in preventing penile, anal, mouth, and throat cancers.Citation26 Many communities have skepticism and hesitancy on why the vaccine is only for girls and not boys.Citation43 Targeting HPV vaccine to both genders before sexual exposure also increases the likelihood of reducing HPV hesitancy and increasing vaccine uptake within the community and there is support for this approach among health workers.Citation43–45 In settings where the coverage of female vaccination is less than 75%, gender neutral vaccination strategies prove cost-effective by rapidly building herd immunity for boys and indirectly protecting those who are unvaccinated.Citation38
Providing gender-neutral HPV vaccination knowledge including its cancer-reducing benefits for both genders may reduce HPV stigma and help desensitize the sexual aspect of the vaccine. HPV and HPV vaccine information is often not disseminated among males. Male partners and fathers often reported low HPV knowledge; however, they considered the vaccine more acceptable once they were well informed.Citation46 Empowering both genders to understand HPV and the importance of the HPV vaccine is vital to vaccine acceptance and uptake.Citation47 Gender-neutral HPV vaccine awareness and implementation provides gender equity, enabling women to obtain the HPV vaccine, particularly in countries where women’s health issues are largely ignored.Citation48
Caregivers’ Acceptance and Attitude Towards Vaccination
Caregiver consent is a crucial factor in enabling adolescent HPV vaccination. As the adolescent’s caregivers are the primary decision-makers for adolescent healthcare choices, health stakeholders need to consider caregivers’ HPV vaccine knowledge, beliefs, and attitudes. Health stakeholders need to consider the caregiver’s education, social status, income, and cultural and religious preferences when explaining why their child needs an HPV vaccine.Citation49 Comprehensive HPV vaccine communication and education campaigns tailored to the caregivers’ perspectives must be implemented prior and during HPV vaccination campaigns to reduce vaccine misinformation.Citation50 The lack of HPV vaccination awareness campaigns preceding and during the vaccination program may cause for caregivers, particularly those with low general vaccine knowledge, to be heavily influenced by negative vaccine information on social media and distrust the HPV vaccine.Citation51 HPV vaccine education campaigns prior to vaccine rollout must target both caregivers and health providers as it is difficult for caregivers to trust the vaccine if health providers have difficulties explaining it.Citation49 Health provider vaccine recommendation also significantly increases caregiver’s likelihood to provide vaccine consent.Citation52
Cost-Benefit Perception and Attitudes
National buy-in is essential to ensuring sustainable HPV vaccination.Citation53,Citation54 In the context of competing health priorities, utilizing scarce domestic infrastructure and human resources for HPV vaccination remains challenging for many LMICs.Citation43 Policymakers debating the implementation of the HPV vaccine will need to consider the HPV disease burden within the country, the country’s health system, and its capacity to sustain the vaccination program.Citation55 Many LMICs do not have sufficient data on vaccine impact such as the disease burden and cost saving, which poses barriers to advocating for national HPV vaccination plans.Citation43 However, the high perceived HPV vaccine cost and logistical challenges may not be as insurmountable with current changes in HPV vaccine implementation. New HPV vaccine implementation methods may enable a shift in attitude that the benefit of the HPV vaccine outweighs the barriers and other competing health priorities.
A key method to reduce infrastructure, human resource and vaccine cost challenges is to consider a one-dose HPV vaccine schedule. Many LMICs have yet to implement HPV vaccination programs, and those who do, often have lower vaccine completion rates compared to higher-income countries because of multi-HPV vaccine dosage schedules.Citation56,Citation57 A one-dose HPV schedule has been shown to deliver comparable HPV protection to a 2 or 3-dose schedule for those ages 9 to 20.Citation58,Citation59 In LMICs, low HPV vaccine coverage is often due to barriers in the cost and logistics of providing a multi-dose vaccine schedule; hence, a one-dose schedule increases vaccine supply and reduces associated resources and costs.Citation57,Citation59–61 Boosting the feasibility of the HPV vaccine may enhance positive attitudes towards the benefits and ease in implementation of the HPV vaccine, encouraging health stakeholders to implement widespread vaccination across various age groups and for both genders.Citation43,Citation62 Lower overall HPV vaccine costs per person may also enable the vaccine to be available for free or at low cost, which has been shown to be a key issue in vaccine acceptance and uptake.Citation63,Citation64 With evidence of the effectiveness of a one-dose schedule, many LMICs are starting to implement the HPV vaccine. Nigeria, for example, introduced a routine immunization program with a single-dose schedule in 2023 and plans to vaccinate 7.7 million girls.Citation16 With increasing HPV vaccination in LMICs, vaccine costs may be further reduced with time. Over the last five years, prices for the HPV vaccine have consistently decreased across all sourcing and income categories; should there be a substantial demand for the vaccine, prices will drop further due to increased competition from new market entrants.Citation65,Citation66
Encouraging the HPV vaccine to be readily available in the community without requiring a specific HPV vaccine health appointment enhances accessibility and promotes greater opportunities for HPV vaccination.Citation67 Adolescents use health services minimally in most LMICs and most tend not to have a primary care doctor or nurse.Citation26,Citation56 Many LMICs have implemented school-based HPV vaccination programs, which have seen relatively high HPV vaccination rates with great potential for sustainability and scalability particularly in primary schools.Citation7,Citation13,Citation68–71 School-based delivery strategies on average had higher coverage and performed better than facility-based programs and the majority (90%) of LMIC vaccination campaigns utilized school-based or a mix of school and facility-based programs.Citation56 Integrating the HPV vaccine into other school-based health services and other community outreach services for adolescents not enrolled in school may further decrease delivery cost and increase vaccine coverage.Citation38,Citation60,Citation68 To further promote HPV vaccination in schools, it is necessary to develop a detailed school-based vaccine communication and education plan so that school educators and health workers can provide sound HPV vaccine recommendations, thereby positively influencing vaccine acceptance and uptake.Citation72 The plan should include training programs with frequent refreshers for educators and health workers, customized school messages, and parental vaccine information materials.Citation39 Health stakeholders must ensure that consistent scheduling and coordination are employed between the education sector and those providing the HPV vaccine so that all stakeholders can provide persistent and holistic vaccine messaging and timely vaccination.Citation73,Citation74
Discussion
This study reviews current literature on the sociocultural and socioeconomic barriers and facilitators that could improve HPV vaccination uptake among adolescents in low-resource settings. The study summarizes the current experiences of implementing the HPV vaccine in LMICs to enable countries considering introducing or improving their national HPV vaccine programs to build upon these lessons and establish best practices. Key factors enhancing HPV vaccine uptake are summarized in . Many LMICs have overstretched and under-resourced public health systems.Citation43 A one-dose, gender-neutral, primary school routine HPV knowledge and vaccination program may be an efficient and cost-effective HPV vaccination strategy.
Box 1 Key Factors Enhancing HPV Vaccine Uptake
Increasing positive vaccine attitudes and decreasing vaccine hesitancy is crucial to successful vaccine uptake. Having a one-dose vaccine increases the affordability of the HPV vaccine with lower human resource and infrastructure costs decreasing vaccine implementation constraints. A lower-cost HPV vaccine schedule is a good initial step to increasing vaccine uptake likelihood; however, only considering economics is insufficient. If the parental and adolescent social norms in the country stigmatize and discriminate against the HPV vaccine, there will be low vaccine acceptance. Overall, community knowledge of the high disease burden associated with HPV infection and the high cancer prevention benefits of the HPV vaccine is paramount to LMIC vaccine initiation, coverage, and sustainability. Regardless of whether the HPV vaccine is delivered through a school, facility, or community platform, the acceptability of the vaccine and the engagement of adolescents and communities are essential to enhancing HPV uptake.Citation24
To increase community HPV cancer and vaccine knowledge, responsible sexuality should be taught to both adolescents in schools and adults in the community. Gender-neutral HPV health literacy decreases vaccine stigma. Desensitizing the community to perceive discussions on sexual health as a taboo would ease the dissemination of sexual health knowledge, enabling more parents and adolescents to accept the vaccine. Having broader, open community HPV discussions would encourage early preparedness to manage HPV rumors and misconceptions. In many LMICs, being female with low education and income decreased the individuals’ vaccine intention potentially because they received vaccine information from non-health sources, eg, relatives, leading to misconceptions and fears about vaccine safety.Citation75 Consistent, broad, vaccine communication within the community by trained health workers, school personnel, and community leaders would enhance vaccine uptake as misconceptions and rumors are the main reason for vaccine hesitancy.Citation27,Citation74,Citation76 A broader HPV vaccine discussion may also enable those who are not enrolled in school to learn about HPV and seek opportunities to vaccinate when they seek health facility services or other community outreach services.
Encouraging vaccination among both boys and girls encourages HPV discussions to reach the entire community and reduces community hesitancy on why the vaccine is only available to girls.Citation43 Countries with male dominance in the household may benefit from gender-neutral HPV vaccine discussions as males who understand the risk of HPV cancers gain more sympathy and support towards addressing HPV for women.Citation46–48 Having gender-neutral vaccine communication may make HPV vaccination easier to develop into a standard policy and operating procedure, so there is not much of a discussion on the need to vaccinate as it is a norm to vaccinate within the community. Normalizing HPV vaccination for both genders before sexual intercourse may promote more timely and wider vaccine coverage, increasing the chances of herd immunity and eventually HPV eradication.Citation77 Creating sustainable HPV vaccine routines may be cost-beneficial and increase health equity for many LMICs. For every $1 US invested into reducing HPV through 2050, an estimated $26 US is gained in societal and economic benefits.Citation78 Cohesive national HPV buy-in should be a health priority for LMICs.
In addition to cervical cancer, the HPV vaccine may reduce adverse outcomes of pre-cancerous lesions. Surgical treatment for cervical carcinoma from HPV increases birth risks among young women who are seeking pregnancy and being immunized for HPV reduces the occurrence of precancerous lesions and cervical carcinoma, helping reduce the significant pregnancy risks.Citation79 Future research may consider providing the HPV vaccine to adult women as research shows that women who had treatment for HPV-related diseases still benefited from the HPV vaccine.Citation80
In sum, there is an urgent need for government ownership and support in HPV vaccine implementation. Health stakeholders should recognize that, given today’s current global society, eliminating the disease burden of HPV is not feasible without addressing the disproportionate rates of HPV morbidity and mortality in LMICs.
Limitations and Future Directions
Several of the studies reviewed had methodological limitations. For example, some studies used data collection methods with a high risk of self-report bias. There is inadequate financial support for cancer surveillance in many LMICs, making it difficult to understand the burden on HPV and the effectiveness of HPV vaccination in those countries.Citation3 The review was restricted to only literature in English, potentially missing literature published in other languages. We have limited knowledge of the efficacy of single dose-HPV vaccine after ten years.Citation57 However, decreasing cost and resource constraints through a single dose schedule may encourage greater vaccine implementation and coverage which may increase herd immunity even with somewhat lower vaccine efficacy. With the greater implementation, vaccine costs may decrease further, making it easier to implement a second dose to the populations needing a booster later in life.
In the future, further cost-effectiveness value analysis for a gender-neutral one-dose HPV vaccine schedule is needed. Future studies should consider how to allocate critical resources to primary school-based vaccine delivery while maintaining cost-effectiveness and ensuring sustainability and scaling-up potential.
Conclusion
HPV vaccination remains crucial to decreasing many HPV-related cancers among males and females. The literature found that limited HPV health literacy is associated with reduced understanding of the need to vaccinate, increased risk of vaccine misinformation, and negative HPV vaccine attitude. To accelerate progress to reach the 90-70-90 goals, LMICs should prioritize increasing HPV vaccine knowledge particularly on its cancer prevention benefits, as knowledge reduces misinformation and increases vaccine acceptance. To ensure timely vaccination before adolescent sexual intercourse, it may be effective to integrate the HPV vaccination as a primary school routine vaccine for both boys and girls. A one-dose HPV vaccination may enable many LMICs to increase vaccine acceptance, uptake, and coverage while reducing financial and human resource costs.
Disclosure
The authors declare no conflicts of interest in this work.
Additional information
Funding
References
- Hull R, Mbele M, Makhafola T. et al. Cervical cancer in low and middle-income countries. Oncol Lett. 2020;20(3):2058–2074. doi:10.3892/ol.2020.11754
- Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. A Canc J Clin. 2018;68(6):394–424. doi:10.3322/caac.21492
- Jedy-Agba E, Joko WY, Liu B, et al. Trends in cervical cancer incidence in sub-Saharan Africa. Br J Canc. 2020;123(1):148–154. doi:10.1038/s41416-020-0831-9
- World Health Organization. Global Strategy to Accelerate the Elimination of Cervical Cancer as a Public Health Problem. World Health Organization; 2020.
- De Martel C, Plummer M, Vignat J, Franceschi S. Worldwide burden of cancer attributable to HPV by site, country and HPV type. Int J Cancer. 2017;141(4):664–670. doi:10.1002/ijc.30716
- Adams M, Jasani B, Fiander A. Human papilloma virus (HPV) prophylactic vaccination: challenges for public health and implications for screening. Vaccine. 2007;25(16):3007–3013. doi:10.1016/j.vaccine.2007.01.016
- Frianto D, Setiawan D, Diantini A, Suwantika AA. Economic evaluations of HPV vaccination in targeted regions of low-and middle-income countries: a systematic review of modelling studies. International Journal of Women’s Health. 2022;2:1315–1322.
- Agosti JM, Goldie SJ. Introducing HPV vaccine in developing countries — Key challenges and issues. New Engl J Med. 2007;356(19):1908–1910. doi:10.1056/NEJMp078053
- Ellingson MK, Sheikha H, Nyhan K, Oliveira CR, Niccolai LM. Human papillomavirus vaccine effectiveness by age at vaccination: a systematic review. Hum Vacc Immunother. 2023;19(2):2239085. doi:10.1080/21645515.2023.2239085
- Wilailak S, Kengsakul M, Kehoe S. Worldwide initiatives to eliminate cervical cancer. Int J Gynaecol Obstet. 2021;1(55 Suppl 1(Suppl 1)):102–106. doi:10.1002/ijgo.13879
- UNICEF. Closing the gap: UNICEF bolsters country efforts to increase HPV vaccination; 2023. Available from: https://www.unicef.org/supply/stories/closing-gap-unicef-bolsters-country-efforts-increase-hpv-vaccination. Accessed July 18, 2024.
- Wigle J, Coast E, Watson-Jones D. Human papillomavirus (HPV) vaccine implementation in low and middle-income countries (LMICs): health system experiences and prospects. Vaccine. 2013;31(37):3811–3817. doi:10.1016/j.vaccine.2013.06.016
- Wong LP, Wong P-F, Megat Hashim MMAA, et al. Multidimensional social and cultural norms influencing HPV vaccine hesitancy in Asia. Hum Vacc Immunother. 2020;16(7):1611–1622. doi:10.1080/21645515.2020.1756670
- Kutz J-M, Rausche P, Gheit T, Puradiredja DI, Fusco D. Barriers and facilitators of HPV vaccination in sub-saharan Africa: a systematic review. BMC Public Health. 2023;23(1):974. doi:10.1186/s12889-023-15842-1
- Cabieses B, Bird P. Glossary of access to health care and related concepts for Low- and Middle-Income Countries (LMICs): a critical review of international literature. Int J Health Serv. 2014;44(4):845–861. doi:10.2190/HS.44.4.j
- World Health Organization. Global Partners Cheer Progress Towards Eliminating Cervical Cancer and Underline Challenges. Geneva, Switzerland: World Health Organization; 2023.
- World Bank. Country and Lending Groups. The World Bank; 2024.
- Maiman LA, Becker MH. The health belief model: origins and correlates in psychological theory. Health Educ Monograp. 1974;2(4):336–353. doi:10.1177/109019817400200404
- Sheeran P, Abraham C. The health belief model. Pred Health Behav. 1996;2:29–80.
- Janz NK, Becker MH. The health belief model: a decade later. Health Educ Quart. 1984;11(1):1–47. doi:10.1177/109019818401100101
- Fallucca A, Immordino P, Riggio L, Casuccio A, Vitale F, Restivo V. Acceptability of HPV vaccination in young students by exploring health belief model and health literacy. Vaccines. 2022;10(7):998.
- Stout ME, Christy SM, Winger JG, Vadaparampil ST, Mosher CE. Self-efficacy and HPV vaccine attitudes mediate the relationship between social norms and intentions to receive the HPV vaccine among college students. J Commu Health. 2020;45(6):1187–1195. doi:10.1007/s10900-020-00837-5
- Kurani S, Maclaughlin KL, Jacobson RM, et al. Socioeconomic disadvantage and human papillomavirus (HPV) vaccination uptake. Vaccine. 2022;40(3):471–476. doi:10.1016/j.vaccine.2021.12.003
- Morgan C, Giattas MR, Holroyd T, et al. Integration of other services with human papillomavirus vaccination; lessons from earlier in the life course highlight the need for new policy and implementation evidence. Vaccine. 2022;40:A94–A99. doi:10.1016/j.vaccine.2021.12.066
- Nabirye J, Okwi LA, Nuwematsiko R, et al. Health system factors influencing uptake of Human Papilloma Virus (HPV) vaccine among adolescent girls 9–15 years in Mbale District, Uganda. BMC Public Health. 2020;20(1):171. doi:10.1186/s12889-020-8302-z
- Asare M, Agyei-Baffour P, Lanning BA, et al. Multi-theory model and predictors of likelihood of accepting the series of HPV vaccination: a cross-sectional study among Ghanaian adolescents. Int J Environment Res Pub Health. 2020;17(2):571.
- Milondzo T, Meyer JC, Dochez C, Burnett RJ. Human papillomavirus vaccine hesitancy highly evident among caregivers of girls attending South African private schools. Vaccines. 2022;10(4). doi:10.3390/vaccines10040503
- Njuguna DW, Mahrouseh N, Isowamwen OV, Varga O. Knowledge, attitude and practice of main stakeholders towards human papilloma virus infection and vaccination in Mombasa and Tana-river counties in Kenya: a qualitative study. Vaccines. 2021;9(10):1099.
- Patrick L, Bakeera-Kitaka S, Rujumba J, Malande OO. Encouraging improvement in HPV vaccination coverage among adolescent girls in Kampala, Uganda. PLoS One. 2022;17(6):e0269655. doi:10.1371/journal.pone.0269655
- Li AJ, Manzi F, Kyesi F, et al. Tanzania’s human papillomavirus (HPV) vaccination program: community awareness, feasibility, and acceptability of a national HPV vaccination program, 2019. Vaccine. 2022;40(Suppl 1):A38–a48. doi:10.1016/j.vaccine.2021.06.047
- Zibako P, Tsikai N, Manyame S, Ginindza TG. Knowledge, attitude and practice towards cervical cancer prevention among mothers of girls aged between 9 and 14 years: a cross sectional survey in Zimbabwe. BMC Women’s Health. 2021;21(1):426. doi:10.1186/s12905-021-01575-z
- Kassa HN, Bilchut AH, Mekuria AD, Lewetie EM. Practice and associated factors of human papillomavirus vaccination among primary school students in Minjar-Shenkora district, North Shoa Zone, Amhara regional state, Ethiopia, 2020. Cancer Management and Research. 2021;3:6999–7008.
- Mabeya H, Odunga J, Broeck DV. Mothers of adolescent girls and Human Papilloma Virus (HPV) vaccination in Western Kenya. Pan Afr Med J. 2021;38:126. doi:10.11604/pamj.2021.38.126.21359
- Wilson R. HPV vaccine acceptance in West Africa: a systematic literature review. Vaccine. 2021;39(37):5277–5284. doi:10.1016/j.vaccine.2021.06.074
- Garon JR, Mukavhi A, Rupfutse M, et al. Multiple cohort HPV vaccination in Zimbabwe: 2018–2019 program feasibility, awareness, and acceptability among health, education, and community stakeholders. Vaccine. 2022;40:A30–A37. doi:10.1016/j.vaccine.2021.05.074
- Wirtz C, Mohamed Y, Engel D, et al. Integrating HPV vaccination programs with enhanced cervical cancer screening and treatment, a systematic review. Vaccine. 2022;40:A116–A123. doi:10.1016/j.vaccine.2021.11.013
- Kulkarni S, Sengeh P, Eboh V, et al. Role of information sources in vaccination uptake: insights from a cross-sectional household survey in Sierra Leone, 2019. Glob Health. 2022;10(1):e2100237. doi:10.9745/ghsp-d-21-00237
- Dorji T, Nopsopon T, Tamang ST, Pongpirul K. Human papillomavirus vaccination uptake in low-and middle-income countries: a meta-analysis. E Clin Med. 2021;34:100836. doi:10.1016/j.eclinm.2021.100836
- Doshi RH, Casey RM, Adrien N, et al. Feasibility and acceptability of nationwide HPV vaccine introduction in Senegal: findings from community-level cross-sectional surveys, 2020. PLOS Glob Pub Health. 2022;2(4):e0000130. doi:10.1371/journal.pgph.0000130
- Rujumba J, Akugizibwe M, Basta NE, Banura C. Why don’t adolescent girls in a rural Uganda district initiate or complete routine 2-dose HPV vaccine series: perspectives of adolescent girls, their caregivers, healthcare workers, community health workers and teachers. PLoS One. 2021;16(6):e0253735. doi:10.1371/journal.pone.0253735
- Sundaram N, Voo TC, Tam CC. Adolescent HPV vaccination: empowerment, equity and ethics. Hum Vacc Immunother. 2020;16(8):1835–1840. doi:10.1080/21645515.2019.1697596
- Karanja-Chege CM. HPV vaccination in Kenya: the challenges faced and strategies to increase uptake. Front Pub Health. 2022;10:802947. doi:10.3389/fpubh.2022.802947
- Guillaume D, Waheed D-E-N, Schleiff M, Muralidharan KK, Vorsters A, Limaye RJ. Global perspectives of determinants influencing HPV vaccine introduction and scale-up in low- and middle-income countries. PLoS One. 2024;19(1):e0291990. doi:10.1371/journal.pone.0291990
- Chowdhury S, Ara R, Roy S, et al. Knowledge, attitude, and practices regarding human papillomavirus and its’ vaccination among the young medical professionals and students of Bangladesh. Clin Exp Vaccine Res. 2022;11(1):63–71. doi:10.7774/cevr.2022.11.1.63
- Grandahl M, Nevéus T. Barriers towards HPV vaccinations for boys and young men: a narrative review. Viruses. 2021;13(8):1644.
- De Fouw M, Stroeken Y, Niwagaba B, et al. Involving men in cervical cancer prevention; a qualitative enquiry into male perspectives on screening and HPV vaccination in Mid-Western Uganda. PLoS One. 2023;18(1):e0280052. doi:10.1371/journal.pone.0280052
- Engel D, Afeli ADJ, Morgan C, et al. Promoting adolescent health through integrated human papillomavirus vaccination programs: the experience of Togo. Vaccine. 2022;40:A100–A106. doi:10.1016/j.vaccine.2021.11.021
- Guillaume D, Meyer D, Waheed D-E-N, et al. Factors influencing the prioritization of vaccines by policymakers in low- and middle-income countries: a scoping review. Health Pol Plan. 2022;38(3):363–376. doi:10.1093/heapol/czac092
- Bal-Yılmaz H, Koniak-Griffin D. Knowledge, behaviors, and attitudes about human papilloma virus among nursing students in izmir, Turkey. J Canc Educ. 2018;33(4):814–820. doi:10.1007/s13187-017-1163-1
- Babi A, Issa T, Issanov A, et al. Knowledge and attitudes of mothers toward HPV vaccination: a cross-sectional study in Kazakhstan. Womens Health. 2023;19:17455057231172355. doi:10.1177/17455057231172355
- Aimagambetova G, Babi A, Issa T, Issanov A. What factors are Associated with attitudes towards HPV vaccination among Kazakhstani women? Exploratory analysis of cross-sectional survey data. Vaccines. 2022;10(5):824.
- Rancic NK, Miljkovic PM, Deljanin ZM, et al. Knowledge about HPV Infection and the HPV vaccine among parents in Southeastern Serbia. Medicina. 2022;58(12):1697.
- Asempah E, Wiktorowicz ME. Understanding HPV vaccination policymaking in Rwanda: a case of health prioritization and public-private-partnership in a low-resource setting. Int J Environ Res Public Health. 2023;20(21). doi:10.3390/ijerph20216998
- Brisson M, Kim JJ, Canfell K, et al. Impact of HPV vaccination and cervical screening on cervical cancer elimination: a comparative modelling analysis in 78 low-income and lower-middle-income countries. Lancet. 2020;395(10224):575–590. doi:10.1016/s0140-6736(20)30068-4
- Guillaume D, Waheed DE, Schlieff M, Muralidharan K, Vorsters A, Limaye R. Key decision-making factors for human papillomavirus (HPV) vaccine program introduction in low-and-middle-income-countries: global and national stakeholder perspectives. Hum Vaccin Immunother. 2022;18(7):2150454. doi:10.1080/21645515.2022.2150454
- Bruni L, Saura-Lázaro A, Montoliu A, et al. HPV vaccination introduction worldwide and WHO and UNICEF estimates of national HPV immunization coverage 2010–2019. Preventive Medicine. 2021;144:106399. doi:10.1016/j.ypmed.2020.106399
- Prem K, Choi YH, Bénard É, et al. Global impact and cost-effectiveness of one-dose versus two-dose human papillomavirus vaccination schedules: a comparative modelling analysis. BMC Med. 2023;21(1):313. doi:10.1186/s12916-023-02988-3
- World Health Organization. One-dose Human Papillomavirus (HPV) vaccine offers solid protection against cervical cancer; 2022. Available from: https://www.who.int/news/item/11-04-2022-one-dose-human-papillomavirus-(hpv)-vaccine-offers-solid-protection-against-cervical-cancer. Accessed July 18, 2024.
- Barnabas RV, Brown ER, Onono MA, et al. Efficacy of single-dose HPV vaccination among young African women. NEJM Evid. 2022;1(5):EVIDoa2100056. doi:10.1056/EVIDoa2100056
- Amponsah-Dacosta E, Blose N, Nkwinika VV, Chepkurui V. Human papillomavirus vaccination in South Africa: programmatic challenges and opportunities for integration with other adolescent health services? Front Public Health. 2022;10:799984. doi:10.3389/fpubh.2022.799984
- Mahumud RA, Gow J, Alam K, et al. Cost-effectiveness of the introduction of two-dose bi-valent (Cervarix) and quadrivalent (Gardasil) HPV vaccination for adolescent girls in Bangladesh. Vaccine. 2020;38(2):165–172. doi:10.1016/j.vaccine.2019.10.037
- Basu P, Malvi SG, Joshi S, et al. Vaccine efficacy against persistent human papillomavirus (HPV) 16/18 infection at 10 years after one, two, and three doses of quadrivalent HPV vaccine in girls in India: a multicentre, prospective, cohort study. Lancet Oncol. 2021;22(11):1518–1529. doi:10.1016/s1470-2045(21)00453-8
- Lintao RCV, Cando LFT, Perias GAS, et al. Current status of human papillomavirus infection and cervical cancer in the Philippines. Front Med. 2022;9:929062. doi:10.3389/fmed.2022.929062
- Milondzo T, Meyer JC, Dochez C, Burnett RJ. Misinformation drives low human papillomavirus vaccination coverage in South African girls attending private schools. Front Public Health. 2021;9:598625. doi:10.3389/fpubh.2021.598625
- World Health Organization. WHO HPV Vaccine Global Market Study. World Health Organization; 2022.
- Llave CL, Uy MEV, Lam HY, et al. The cost-effectiveness of human papillomavirus vaccination in the Philippines. Vaccine. 2022;40(27):3802–3811. doi:10.1016/j.vaccine.2022.05.025
- Casey RM, Adrien N, Badiane O, et al. National introduction of HPV vaccination in Senegal-Successes, challenges, and lessons learned. Vaccine. 2022;40(Suppl 1):A10–a16. doi:10.1016/j.vaccine.2021.08.042
- Tsu VD, Lamontagne DS, Atuhebwe P, Bloem PN, Ndiaye C. National implementation of HPV vaccination programs in low-resource countries: lessons, challenges, and future prospects. Prev Med. 2021;144:106335. doi:10.1016/j.ypmed.2020.106335
- Rosen JG, Guillaume D, Mlunde LB, et al. Feasibility and sustainability of a school-based platform for integrated delivery of HPV vaccination with adolescent health services in Tanzania: qualitative insights from stakeholders. Health Policy and Planning. 2023;38(4):486–495. doi:10.1093/heapol/czad014
- Baussano I, Sayinzoga F, Tshomo U, et al. Impact of human papillomavirus vaccination, Rwanda and Bhutan. Emerg Infect Dis. 2021;27(1):1–9. doi:10.3201/eid2701.191364
- Sayinzoga F, Umulisa MC, Sibomana H, Tenet V, Baussano I, Clifford GM. Human papillomavirus vaccine coverage in Rwanda: a population-level analysis by birth cohort. Vaccine. 2020;38(24):4001–4005. doi:10.1016/j.vaccine.2020.04.021
- Amponsah-Dacosta E, Kagina BM, Olivier J. Health systems constraints and facilitators of human papillomavirus immunization programmes in sub-Saharan Africa: a systematic review. Health Policy Plan. 2020;35(6):701–717. doi:10.1093/heapol/czaa017
- Ebrahimi N, Yousefi Z, Khosravi G, et al. Human papillomavirus vaccination in low- and middle-income countries: progression, barriers, and future prospective. Front Immunol. 2023;14:1150238. doi:10.3389/fimmu.2023.1150238
- Mphuru A, Li AJ, Kyesi F, et al. National introduction of human papillomavirus (HPV) vaccine in Tanzania: programmatic decision-making and implementation. Vaccine. 2022;40(Suppl 1):A2–a9. doi:10.1016/j.vaccine.2021.04.025
- Moola S, Gudi N, Nambiar D, et al. A rapid review of evidence on the determinants of and strategies for COVID-19 vaccine acceptance in low- and middle-income countries. J Glob Health. 2021;11:05027. doi:10.7189/jogh.11.05027
- Xu MA, Choi J, Capasso A, Diclemente R. Patient-provider health communication strategies: enhancing HPV vaccine uptake among adolescents of color. Healthcare. 2023;11(12):1702.
- Jit M, Prem K, Benard E, Brisson M. From cervical cancer elimination to eradication of vaccine-type human papillomavirus: feasibility, public health strategies and cost-effectiveness. Prev Med. 2021;144:106354. doi:10.1016/j.ypmed.2020.106354
- Torode J, Kithaka B, Chowdhury R, Simelela N, Cruz JL, Tsu VD. National action towards a world free of cervical cancer for all women. Prev Med. 2021;144:106313. doi:10.1016/j.ypmed.2020.106313
- Golia D’augè G, Cuccu I, Etrusco A, et al. State of the art on HPV-related cervical lesions. Italian J Gynaecol Obst. 2024. doi:10.36129/jog.2024.161
- Bogani G, Sopracordevole F, Ciavattini A, et al. HPV-related lesions after hysterectomy for high-grade cervical intraepithelial neoplasia and early-stage cervical cancer: a focus on the potential role of vaccination. Tumori J. 2024;110(2):139–145. doi:10.1177/03008916231208344