Abstract
About one third of adolescents in the USA are overweight and/or obese. Obesity during the adolescent years is associated with many adverse health consequences, including type 2 diabetes, hypertension, hyperlipidemia, and psychosocial problems. Because of substantial advances in technologies and wide acceptance by adolescents, it is now possible to use technology for healthy weight management and prevention of obesity. This systematic review used Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines and aimed to evaluate the existing literature reported on the effectiveness of technology-based intervention (web-based, e-learning, and active video games) in preventing obesity in adolescents. The primary aim of this review was to explore if components of specific interventions were associated with a reduction in body mass index. Research articles obtained from CINAHL, Embase, PubMed, PsycInfo, and the Cochrane database from1990 to 2014 were reviewed. A total of 131 published articles were identified, and 14 met the inclusion criteria of a randomized or nonrandomized clinical study with body mass index as primary outcome and/or secondary outcomes of diet/physical activity and/or psychosocial function, tested lifestyle interventions to prevent obesity, used technology, and studied adolescents (aged 12–18 years). The results indicated that six of 14 studies found body mass index and/or body fat decreased at short-term (less than 12 months) follow-up. Six of eleven studies that examined physical activity or physical activity-related outcomes found an improved physical activity outcome (time playing active video games and increase in physical activity time), while five of seven studies which assessed dietary outcomes indicated improvement in dietary behaviors. Five of seven studies suggested an improvement in psychosocial function (reduced depression, improved self-esteem and efficacy, improvement on Behavior Assessment Scale) in adolescents involved in the technology-based intervention. All effective interventions utilized dietary and physical activity strategies as part of intervention components. Because of the variation in duration of intervention (range 10 weeks to 2 years), it is not clear what length of intervention is most effective. Future research should assess the long-term impact of technology-based interventions and evaluate mediators and moderators for weight change in adolescents.
Introduction
Obesity among adolescents has reached epidemic proportions worldwide.Citation1 Approximately one third of adolescents in the USA are currently overweight or at risk for becoming overweight.Citation2 Obesity in adolescence predisposes this age group to obesity in adulthood and is a major risk factor for a number of serious health conditions, including diabetes, hypertension, heart disease, stroke, osteoarthritis, and certain types of cancer.Citation3–Citation5 Because 80% of obese adolescents will become obese adults,Citation6 with increased susceptibility to type 2 diabetes mellitus and cardiovascular disease,Citation7–Citation9 management of obesity in adolescents is critical. Many intervention studies have been conducted to address this epidemic health concern.Citation10–Citation12 As technology has become such an important part of daily life, especially among adolescents, technology-based interventions, including Internet-based weight management tools, social media, apps for smartphones, and active video games, have been developed as methods to prevent obesity in this age group.Citation13–Citation15
The most recent research suggests that 78% of adolescents in the USA have cell phones (47% smartphones), 23% have a tablet computer, and 93% have access to a computer and use one at home.Citation12 Due to the high use of technology among adolescents, there are health promotion opportunities that include tapping into the new media channels integral to youth culture.Citation13 The use of mobile technologies may offer a practical and reliable means of managing obesity in busy primary care clinics. In the last decade, several interventions using technology to prevent obesity have been tested in schools, in after school programs, and in the clinic setting. Few systematic reviews have been conducted to examine the impact of technology-based interventions on childhood obesity.Citation16,Citation17 An et al examined the effect of web-based weight management on children and adolescents,Citation16 and Lu et al explored the effect of health video games on prevention of childhood obesity.Citation17 The review by An et al explored multiple types of intervention, including home Internet interventions, interventions with parents, and interactive websites.Citation16 Although their review included weight-related variables (body mass index [BMI], BMI percentile, physical activity, and diet) it included studies testing for multiple other outcomes and included various targeted populations (children, parents) which made comparison of studies difficult. In contrast, Lu et al reviewed studies that focused only on health video games in overweight or obese children.Citation17 There is a dearth of knowledge on the impact of technology-based interventions, including both web-based and active video games, on weight management and weight-related health behaviors (physical activity, sedentary activity, and diet) in adolescents.
The purpose of this review is to assist health care providers and researchers in making more informed decisions about which types of technology-based interventions for adolescent obesity prevention are most suitable and achieve sustainable weight reduction, impact on amount of physical activity, a reduction in sedentary activity, improved dietary behaviors, and/or positive psychosocial outcomes. With the advancement of technology and the opportunity to explore the use of technology as an approach to adolescent obesity, it is important to systematically review the methodological rigor of technology-based interventions and their impact on BMI, and to identify types of interventions that work best for prevention of obesity in adolescents. The two specific objectives of this review were to evaluate the existing literature reported on the effectiveness of technology-based interventions in preventing obesity in adolescents and to explore components of these interventions that are associated with significant BMI outcomes.
Methods
Data sources
This systematic review was conducted and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines that have been used for other obesity-related systematic reviews.Citation18 Our search covered all available years from January 1990 to January 2014 in CINAHL, Embase, PubMed, PsycINFO, and the Cochrane Library. The bibliographies of included articles were hand-searched, and promising titles were reviewed in order to locate articles not catalogued in the major databases. If the reviewer was unable to determine if an article pertained to the study by title, then the abstract was reviewed. The search terms used were (Adiposity[mh] OR Body Mass Index[mh] OR Body Weight[mh:noexp] OR Body Weight Changes[mh] OR Obesity[mh] OR Overweight[mh] OR Weight Gain[mh] OR Weight Loss[mh] OR Weight Reduction Program[mh] OR “abdominal fat”[tiab] OR adiposity[tiab] OR bmi[tiab] OR “body mass index”[tiab] OR “body weight”[tiab] OR obese[tiab] OR obesity[tiab] OR overweight[tiab] OR “visceral fat”[tiab] OR “weight loss”[tiab] OR “weight management”[tiab] OR “weight reduction”[tiab]) AND Blogging[mh] OR Cellular Phone[mh] OR Computer-Assisted Instruction[mh] OR Computer Graphics[mh] OR Computer Systems[majr] OR Computers[majr] OR Computers, Handheld[mh] OR Educational Technology[mh] OR Electronic Mail[mh] OR Interactive Tutorial[pt] OR Internet[mh] OR Multimedia[mh] OR Software[mh:noexp] OR Technology[majr:noexp] OR Telecommunications [majr:noexp] O R Telemedicine[mh:noexp] OR Text Messaging[mh] OR User-Computer Interface[mh] OR Videoconferencing[mh] OR Video Games[mh] OR Webcasts as Topic[mh] OR Wireless Technology[mh].
To assure the quality of the study findings reported, we selected papers that used either a randomized controlled trial approach or a quasi-experimental study design. Inclusion criteria consisted of: randomized clinical trials or clinical trials without randomization or a control group; a primary outcome including BMI or BMI z-score (both self-report and measurement collected using the World Health Organization classification) and one of the health behaviors (diet and physical activity); trials that tested lifestyle/weight management interventions (through physical activity or diet modification using Internet or active video games) intended to prevent obesity or excessive weight gain; trials that tested lifestyle interventions using at least one of the eHealth/mHealth (term used for the practice of medicine and public health supported by mobile devices) intervention components including web (Internet)-based, social media, and mobile communication technology; and participants included adolescents aged from 12–18 years. Papers were excluded if they described primary prevention interventions or if the majority of participants were over 18 years of age and if the articles were published in a language other than English.
Data extraction
This systematic review compares randomized controlled trials and pre-post test (quasi-experimental) studies that utilized technology-based interventions including active video games and the Internet as interventions to decrease BMI or percent body fat. The studies focused primarily on increasing physical activity, decreasing sedentary activity, improving dietary outcomes, and/or improving diet skills (increased fruit and vegetables, decreased sugary drinks and high fat foods) as well as improving psychosocial well-being (weight concerns, self-efficacy, self-esteem, and peer support). This review involves assessing educational, behavioral, and health promotion interventions delivered through technology including web/Internet-based, social media, and mobile communication technology aimed to prevent obesity in adolescents.
Outcome variables
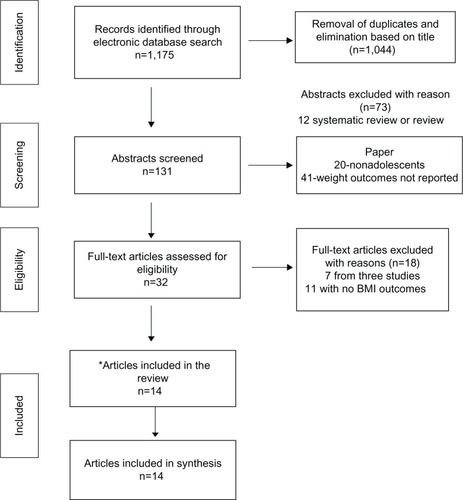
The initial search generated a total of 1,175 papers from all the search databases. To obtain rigorous scientific evidence, only randomized controlled trials and pre-post test studies were selected for this systematic review in terms of key outcomes and interventions used. One reviewer screened the study title and abstract as the first screening stage and narrowed the articles to 131 papers. Two reviewers then reviewed the abstract and narrowed the search from 131 articles to 32 articles by eliminating duplicate papers based on the same research. Articles that were nonintervention studies, such as review papers, and cross-sectional studies were also excluded. The primary outcome was reduction of BMI in adolescents with the use of technology. Studies that did not target obesity, were not technology-based, and not conducted in adolescents were excluded. Based on the inclusion criteria, two reviewers examined the full papers and identified 14 studies that met the inclusion criteriaCitation13,Citation21–Citation33 (see ).
Figure 1 Preferred reporting items for systematic reviews and meta-analyses flow diagram for articles identified, screened eligible, and included in this paper.
Abbreviation: BMI, body mass index.
The 14 studies reviewed used a variety of outcome measures, including weight-related measures (ie, BMI, BMI z-score) which were the primary outcomes reviewed in this paper, as well as several secondary outcomes including percentage of body fat, physical activity level, physical fitness, dietary intake, and psychosocial variables (ie, self-esteem, self-competence). In this review, the effects of the interventions were evaluated in terms of weight-related measurements, specifically BMI and BMI z-score, as they were used in the studies included in the review.
Intervention components
Detailed examination of the following components of effective interventions was conducted: behavior change targets, method used to effect weight changes, frequency of contact, and duration of the intervention. The effectiveness of the intervention was determined by reviewing the results of the study and reporting the study findings.
Assessment of methodological rigor
We adapted the methodological rigor assessment for the included articles from those in use by the Cochrane Effective Practice and Organization of Care Review Group and recent systematic reviews.Citation19,Citation20 The nine criteria were scored objectively using published data and reflect potential bias (see ). Studies were rated independently by two reviewers. Disagreements were discussed until consensus was reached. Disagreement between reviewers was due to confusion in meaning of “intent to treat”, and once clarified, consensus was reached. Each item was rated as “yes” (1), “no” (0), or “not applicable”. A total methodological quality score (ranging from 0 to 9) was calculated by summing up all “yes” items. Studies were rated as having good methodological quality if they met at least 80% of the criteria (seven of nine items or five of six items).
Table 1 Methodological rigor of included studies
Results
Effectiveness of technology-based intervention in preventing adolescent obesity
BMI/percentage body fat
Six studies (42.8%) found a significant decrease in BMI or percentage body fat after the intervention.Citation13,Citation23,Citation25,Citation27,Citation28,Citation33 Four Internet-based intervention studiesCitation23,Citation25,Citation27,Citation33 and two active video game-based interventionsCitation13,Citation34 reported that adolescents in the intervention group had significantly reduced BMI and/or percentage body fat immediately after the intervention or up to 9 months post intervention. Short-term effects of technology-based interventions were found (less than 12 months of follow-up) in all six studies, while one study (by Williamson et al)Citation33 found no beneficial effect on BMI at assessment 2 years post baseline (see for study description).
Table 2 Study description
Physical activity, sedentary activity time, and dietary behavior
Six of the eleven studies that examined physical activity or physical activity-related outcomes found improved physical activity outcomes (four Internet-based interventions and two active video gaming interventions).Citation13,Citation21,Citation23,Citation26,Citation28,Citation35 Two of three studies that assessed the impact of technology-based interventions on reducing sedentary activity time found a significant decrease in sedentary behaviors (all active video game interventions).Citation13,Citation28 For dietary behavior, five of eleven studies assessed dietary outcomes indicating improvement in dietary behaviors (ie, increased fruit/vegetable intake, decreased sugary drinks and snacking) in adolescents in the intervention groups (four Internet-based interventions and one active video game intervention).Citation13,Citation22–Citation24,Citation33 For instance, a study by Chen et alCitation22 on tailored web-based interventions for Chinese-American adolescents (aged 12–15 years) found a significant decrease in sedentary activity associated with improved physical activity and fruit/vegetable intake at 6 months post intervention. Maddison et alCitation28 examined an active video game upgrade package in adolescents aged 10–14 years and found that youth in the intervention group increased the time playing active video games while decreasing the time in nonactive video games (see ).
Table 3 Outcome measured by study: arrows indicate significant increase or decrease on the outcomes
Other psychosocial outcomes
Seven studies assessed the impact of technology-based interventions on psychosocial outcomes (ie, self-efficacy, weight concern, peer support, and self-competence).13,22,25–27,29,31,32 Five of the seven studies suggested improvement in psychosocial function in adolescents using the technology-based interventions.Citation13,Citation22,Citation25,Citation27,Citation31,Citation32 For example, Wagener et alCitation32 found that adolescents in an exer-gaming program had improved self-perceived psychological adjustment and competence to exercise after the intervention, and Jones et alCitation27 found that adolescents in their intervention group reported fewer weight and body shape concerns (see ).
Components of effective interventions
Seven Internet-based interventions and seven active video game-based interventions were included in this systematic review. Six of 14 studies (four Internet-based and two active video game-based interventions) found that BMI and/or body fat decreased.Citation13,Citation23,Citation25,Citation27,Citation28,Citation33 All effective interventions utilized dietary and physical activity strategies as part of the intervention components. Six Internet-based interventions required weekly logins whereas active video game interventions recommended daily use. Based on the results, it is recommended that the intervention intensity that was based weekly has the potential to decrease obesity (see for significant BMI outcomes with intervention components).
Table 4 Significant BMI outcome (decreased BMI or percent body fat)
Discussion
The present systematic review investigates the potential impact of recent technological innovations (such as the Internet or active video games) for adolescents and the effect of these technology-based interventions on weight-related outcomes. Based on our review of 14 clinical intervention studies, there is no clear evidence that technology-based interventions decrease obesity in adolescents. We found that slightly less than half of the studies reviewed in this paper supported the use of technology in reducing unhealthy weight in adolescents. All effective interventions included improving physical activity and healthy eating habit as key components. However, each of these interventions only had a short-term impact on weight management. This is consistent with other obesity prevention interventions in children that are either home-based or school-based.Citation36–Citation38 Because of the variation in duration of intervention (ranging from 10 weeks to 2 years) and dose (daily to weekly), the literature to date does not provide enough evidence on the optimal dose or duration of the most effective intervention for prevention of obesity in adolescents, although the trend pointed toward dosing a minimum of one hour/weekly for 10–16 weeks for best results. This is consistent with a systematic review done for obesity prevention in a primary care setting.Citation39
In comparing the various modalities of technology and their delivery (Internet versus active video games), there is no clear evidence that one format is more effective than another. Depending on the age of the participants, different modalities might be more attractive than others. For example, a younger adolescent might prefer exer-games and interacting with peers, while an older adolescent might prefer a smartphone app or Internet-based program for weight management that could be used privately.
The literature currently available is also insufficient to examine the impact of technology-based obesity prevention interventions on weight-health related outcomes such as physical activity, sedentary activity, dietary behaviors, or psychosocial outcomes. In eleven studies that examined the impact of technology-based obesity prevention on physical activity and dietary behaviors, only six reported positive improvement in these outcomes. Even fewer studies examined the impact of interventions on sedentary behaviors and psychosocial outcomes. Therefore, it is challenging to determine the effect of technology-based intervention on weight-related health behaviors, and we do not know whether improvement of these behaviors led to decreased weight among adolescents. One plausible reason for this lack of evidence might be the wide range of ages encompassed by these studies. Participants in the various studies ranged in age from 10–19 years. These years encompass later childhood (9–12 years), early adolescence (13–14 years), and late adolescence (15–17 years) as well as young adulthood (18–19 years). The developmental differences and the prevalence of using technology among these age groups may impact any potential trend seen in the data. Depending on the age group being investigated, interest in technology and use may vary.
This review suggests that both active video games and Internet-based interventions including diet and physical components have the potential to decrease obesity in adolescence, especially Internet-based interventions. Because of the variation in duration of intervention (10 weeks to 2 years), it is not clear what length of intervention is most effective. Only one study included long-term follow-up data (more than 12 months after the intervention), and the intervention did not support long-term efficacy with regard to healthy weight management.Citation33
Our review indicates that several interventions provide short-term improvements in BMI but none that seem to be sustainable. Sustained weight loss is an ongoing struggle, regardless of the sample being studied or the interventions used, and is no different in this population. Very few interventions seem to specifically focus on lifelong lifestyle modifications. Many of the interventions that were investigated either provided the participants with the necessary equipment (ie, loaning Wii Fit, allowing temporary upgrades to active video games) or were activities that were set up for a limited time period at school (GameBike or Dance-Dance Revolution). After the intervention, participants no longer had access to these exercise opportunities, so likely reverted back to the prestudy lifestyle habits that lead to their overweight or obesity. Technology-based intervention for weight management needs to be developed in such a way that it incorporates resources that will continue to be available in order to see sustainability.
The goal of this review was to determine ways in which health care providers and researchers can make more informed decisions about which types of technology-based interventions for adolescent obesity are most suitable and achieve sustainable weight reduction, impact the amount of physical activity, reduce sedentary activity, improve dietary behaviors, and/or positive psychosocial outcomes. Although we found no clear evidence of an effect of technology-based intervention for prevention of obesity in adolescents, the use of developmentally appropriate technology has the potential to assist health care providers in dealing with the obesity epidemic, especially when interventions focus on both physical activity and healthy dietary behaviors. Future research should include rigorous evaluation of cost- effectiveness as well as the mediating and moderating factors associated with effective technology-based interventions, and should also include more long-term follow-up. In addition, assessment of weight-related health outcomes, such as physical activity, sedentary activity, dietary behaviors, self-efficacy, and quality of life, should be included in future research.
Disclosure
The authors report no conflicts of interest in this work.
References
- WangYLobsteinTWorldwide trends in childhood overweight and obesityInt J Pediatr Obes200611112517902211
- IannottiRJWangJTrends in physical activity, sedentary behavior, diet, and BMI among US adolescents, 2001–2009Pediatrics2013132460661424043281
- BjorgeTEngelandATverdalASmithGDBody mass index in adolescence in relation to cause-specific mortality: a follow-up of 230,000 Norwegian adolescentsAm J Epidemiol20081681303718477652
- LeviZKarkJDBarchanaMMeasured BMI in adolescence and the incidence of colorectal cancer in a cohort of 1.1 million malesCancer Epidemiol Biomarkers Prev201120122524253122056504
- ReillyJJKellyJLong-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic reviewInt J Obes (Lond)201135789189820975725
- RademacherERJacobsDRJrMoranASteinbergerJPrineasRJSinaikoARelation of blood pressure and body mass index during childhood to cardiovascular risk factor levels in young adultsJ Hypertens20092791766177419633567
- LloydLJLangley-EvansSCMcMullenSChildhood obesity and adult cardiovascular disease risk: a systematic reviewInt J Obes (Lond)2010341182819434067
- LloydLJLangley-EvansSCMcMullenSChildhood obesity and risk of the adult metabolic syndrome: a systematic reviewInt J Obes (Lond)201236111122041985
- WeissRCaliAMDziuraJBurgertTSTamborlaneWVCaprioSDegree of obesity and glucose allostasis are major effectors of glucose tolerance dynamics in obese youthDiabetes Care20073071845185017475938
- Feliu RoviraAParis MiroNZaragoza-JordanaMClinical and metabolic effectiveness of a new motivational therapy for the treatment of obesity in adolescents (OBEMAT)An Pediatr (Barc)2013783157166 Spanish22832041
- GourlanMSarrazinPTrouilloudDMotivational interviewing as a way to promote physical activity in obese adolescents: a randomised-controlled trial using self-determination theory as an explanatory frameworkPsychol Health201328111265128623756082
- MaddenMLenhartADugganMCortesiSGasserUTeens and Technology2013 Available from: http://www.pewinternet.org/Reports/2013/Teens-and-Tech.aspxAccessed March 9, 2014
- ChristisonAKhanHAExergaming for health: a community-based pediatric weight management program using active video gamingClin Pediatr (Phila)201251438238822157430
- PellegriniCADuncanJMMollerACA smartphone-supported weight loss program: design of the ENGAGED randomized controlled trialBMC Public Health201212104123194256
- WoolfordSJClarkSJStrecherVJResnicowKTailored mobile phone text messages as an adjunct to obesity treatment for adolescentsJ Telemed Telecare201016845846120959393
- AnJHaymanLParkYDusajTAyresCWeb-based weight management programs for children and adolescents a systematic review of randomized controlled trial studiesAdv Nurs Sci2009323222240
- LuASKharraziHGharghabiFThompsonDA systematic review of health videogames on childhood obesity prevention and interventionGames Health J20132313114124353906
- LavelleHVMackayDFPellJPSystematic review and meta-analysis of school-based interventions to reduce body mass indexJ Public Health (Oxf)201234336036922267291
- SargentGMPilottoLSBaurLAComponents of primary care interventions to treat childhood overweight and obesity: a systematic review of effectObes Rev2011125e219e23520630025
- TobiasDKZhangCvan DamRMBowersKHuFBPhysical activity before and during pregnancy and risk of gestational diabetes mellitus: a meta-analysisDiabetes Care201134122322920876206
- AdamoKBRutherfordJAGoldfieldGSEffects of interactive video game cycling on overweight and obese adolescent healthAppl Physiol Nutr Metab201035680581521164552
- ChenJLWeissSHeymanMBCooperBLustigRHThe efficacy of the web-based childhood obesity prevention program in Chinese-American adolescents (qeb ABC study)J Adolesc Health201149214815421783046
- DoyleACGoldschmidtAHuangCWinzelbergAJTaylorCBWilfleyDEReduction of overweight and eating disorder symptoms via the Internet in adolescents: a randomized controlled trialJ Adolesc Health200843217217918639791
- EzendamNPBrugJOenemaAEvaluation of the Web-based computer-tailored FATaintPHAT intervention to promote energy balance among adolescents: results from a school cluster randomized trialArch Pediatr Adolesc Med2012166324825522064878
- HungSHHwangSLSuMJAn evaluation of a weight-loss program incorporating E-learning for obese junior high school studentsTelemed J E Health200814878379218954248
- JagoRBaranowskiTBaranowskiJCFit for Life Boy Scout badge: outcome evaluation of a troop and Internet interventionPrev Med200642318118716458955
- JonesMLuceKHOsborneMIRandomized, controlled trial of an internet-facilitated intervention for reducing binge eating and overweight in adolescentsPediatrics2008121345346218310192
- MaddisonRFoleyLNi MhurchuCEffects of active video games on body composition: a randomized controlled trialAm J Clin Nutr201194115616321562081
- NguyenBShrewsburyVAO’ConnorJTwo-year outcomes of an adjunctive telephone coaching and electronic contact intervention for adolescent weight-loss maintenance: the Loozit randomized controlled trialInt J Obes (Lond)201337346847222584456
- OwensSGGarnerJC3rdLoftinJMvan BlerkNErminKChanges in physical activity and fitness after 3 months of home Wii Fit useJ Strength Cond Res201125113191319721993031
- StaianoAEAbrahamAACalvertSLAdolescent exergame play for weight loss and psychosocial improvement: a controlled physical activity interventionObesity (Silver Spring)201321359860123592669
- WagenerTLFedeleDAMignognaMRHesterCNGillaspySRPsychological effects of dance-based group exergaming in obese adolescentsPediatr Obes201275e68e7422767495
- WilliamsonDAWaldenHMWhiteMATwo-year internet-based randomized controlled trial for weight loss in African-American girlsObesity (Silver Spring)20061471231124316899804
- MaddisonRMhurchuCNJullAPrapavessisHFoleyLSJiangYActive video games: the mediating effect of aerobic fitness on body compositionInt J Behav Nutr Phys Act201295422554052
- BerensonGSAgirbasliMNguyenQMChenWSrinivasanSRGlycemic status, metabolic syndrome, and cardiovascular risk in childrenMed Clin North Am2011952409417 ix21281842
- BarnettACerinEBaranowskiTActive video games for youth: a systematic reviewJ Phys Act Health20118572473721734319
- O’BrienA“Web-based weight management programs for children and adolescents: a systematic review of randomized controlled trial studies” by An, Hayman, Park, Dusaj, and Ayres (Jul–Sep 2009, Vol 32, No 3, pp 222–240)ANS Adv Nurs Sci2010331220154526
- KatzDLSchool-based interventions for health promotion and weight control: not just waiting on the world to changeAnnu Rev Public Health20093025327219705560
- JacobsonDGance-ClevelandBA systematic review of primary healthcare provider education and training using the Chronic Care Model for childhood obesityObes Rev2011125e244e25620673280
