Abstract
Compared to other health-care workers, dental health-care workers come in close contact with patients and use a variety of sharp and high-speed rotating instruments. It is important to understand the characteristics of the occupational accidents that occur. We reviewed incident reports from April 1, 2005, to March 31, 2010, at Matsumoto Dental University Hospital. In addition, questionnaires dealing with identification of occupational safety issues, especially splash exposures, were conducted for dentists, dental hygienists, and nurses. Thirty-two occupational injuries were reported during the study period, including 23 sharp instrument injuries (71.9%), 6 splash exposures (18.8%), and 3 others. Of the six splash exposures, only two cases involved potential contamination with blood or other potentially infectious patient material. Of the 66 workers who experienced sharps injuries, 20 workers (30.3%, 20/66) reported them to the hospital work safety team. The questionnaire revealed high incident of splash exposures and conjunctiva exposures: 87.9% (51/58) and 60.3% (35/58) in dentists and 88.6% (39/44) and 61.4% (27/44) in dental hygienists. The compliance rate for routine use of protective eyewear was 60.3% (35/58) for dentists and 34.1% (15/44) for hygienists. Of the presented informational items included in the questionnaire, those that strongly persuaded respondents to use protective eyewear were ‘splatters from the patient’s mouth contain blood’ (90%, 99/110) and ‘dental operations at our clinic are performed based only on a questionnaire without serious examinations for HBV, HCV, and HIV’ (71.8%, 79/110). The reason of low compliance of protective eyewear among dentists might relate to fine dental procedures. Appropriate information is important for the motive of wearing personal protective equipment, and an early educational program may have a potential to increase compliance with the use of that equipment.
Introduction
The number of percutaneous injuries with sharp instruments is estimated to be 600,000–800,000 events annually among US health-care workers.Citation1 All health-care workers who performed invasive procedures with sharp instruments are at risk for those injuries. In addition to percutaneous injuries, splash exposure to blood and serum also has a risk of transmitting blood-borne infection, ranging from 2% to 15.3%Citation2–Citation4 of total accidental blood exposure incidents. Surgeons and surgical assistants are frequently exposed to microbial pathogens via sharps injuriesCitation5 and splashes.Citation6
In particular, dental health-care workers come in close contact with a patients’ mouth during their treatment, as documented by the finding that dental students tended to show greater rates of tuberculosis infection than medical students.Citation7 Additionally, high-speed rotating instruments, which produce large amounts of contaminated splatters and aerosols,Citation6,Citation8–Citation10 are frequently used in dental procedures. Therefore, dental health-care workers face a significant risk of splash exposure and occupational infection via mucous and conjunctival membranes. However, only 15% are recognized by the surgeon intraoperatively, as most blood splashes are less than 0.6 mm in diameter.Citation11
Thus, the present study of occupational incidents, especially with sharp injury and splash exposure in a dental hospital, was conducted by reviewing incident reports, and their prevalence and frequency were determined in our hospital. Furthermore, to investigate the concern regarding splash exposures during dental procedures, a questionnaire survey was conducted.
Materials and methods
This investigation was designed as a retrospective study and conducted at a single educational center, Matsumoto Dental University Hospital, Nagano, Japan. The medical workers consisted of 188 dentists, 45 dental hygienists, and 23 nurses at the hospital. An average total of 100,000 outpatients visited the hospital annually, and approximately 400 outpatients were cared per day. When an adverse event occurred, an incident report was systematically submitted from the person concerned to the Risk Management Work Team immediately after the event.
In order to provide information feedback, each month, the Risk Management Work Team of our hospital provided a written summary of incident reports to all staff regarding the place of occurrence and suggestions for the prevention and control of recurrence of such adverse events. We investigated the number and the content of events, the job title, the department, and clinical years of the involved staff using the summarized reports of the work team from April 1, 2005, to March 31, 2010.
In addition, questionnaires were distributed, aiming to investigate occupational safety issues, especially splash exposures. The individuals who participated in the questionnaires were 60 dentists, 45 dental hygienists, and 18 nurses.
The survey asked about the number of years of postgraduate clinical experience, the department, the sex of the respondent, the number of injuries from sharp instruments in the past, the type of instrument, the number of splash exposures, the number of conjunctival splatters, routine wearing of goggles or face shields, and reporting when events occurred.
Next, a second survey was performed regarding motivation for wearing protective eye shield equipment by years of clinical experience, department, and sex of the respondent ().
Table 1 Contents of occupational injuries
Results
Review of incident reports regarding occupational injuries
A total of 183 documented reports were submitted during the study period. Seventy-one cases were categorized as harmful events, such as wrong medication, foreign object (dental materials) ingestion, and unexpected injury for patients, and of the 71 cases, 32 events were classified as occupational injuries. These occupational injuries occurred in 6.4 cases annually, and the incident rate was 0.0064% or one event per 15,625 outpatient visits.
The reported 32 cases regarding occupational injuries were mainly caused by sharp instrument injuries and splash exposures (). The incidents were reported commonly by dental hygienists and dentists (). Of the 14 reports from dental hygienists, 8 were about sharp instrument injuries and 5 were about splash exposures. Of the nine reports from dentists, eight were about sharps injuries and one was about a splash exposure. The three cases from nurses were needle stick injuries (two cases with a suture needle and one with a syringe needle). Of the five reports from undergraduate students, three were about sharp instrument injuries. Of the sharps injuries, five of the eight cases in dentists and seven of the eight cases in hygienists involved a sharp dental instrument, with the remainder being caused by a needle. Six splash exposures involving a dentist and hygienists were caused by liquid chemical materials for dental treatment, with five cases to the conjunctival mucosa (eye) and one cutaneous injury (face). Only one case had a potential for contamination with patient blood or other potentially infectious material (OPIM).
Table 2 Title of injured worker
Questionnaire regarding sharp instrument injuries
A total of 120 responses was obtained from 58 dentists, 44 dental hygienists, and 18 nurses. The response rate was 96.7% (58/60), 97.8% (44/45), and 100% (18/18) from dentists, dental hygienists, and nurses, respectively.
Percutaneous occupational injuries with sharp instruments were experienced among 50%–60% of responded staff, and there was no significant difference of the prevalence among job title ().
Table 3 Prevalence of occupational injury
Among dentists, percutaneous injuries occurred in none (0%, 0/11) in the first-year dentists, 8 (57.1%, 8/14) in the second-year dentists, 3 (42.9%, 3/7) in the third-year dentists, 2 (50%, 2/4) in the fourth-year dentists, 6 (66.7%, 6/9) in the fifth- to ninth-year dentists, and 10 (76.9%, 10/13) in the tenth-year or later dentists. Among dental hygienists, percutaneous injuries occurred in four (50%, 4/8) in the first-year dental hygienists, three (50%, 3/6) in the second-year dental hygienists, three (50%, 3/6) in the third-year dental hygienists, four (50%, 4/8) in the fourth-year dental hygienists, five (62.5%, 5/8) in the fifth- to ninth-year dental hygienists, and seven (87.5%, 7/8) in the tenth-year or later dental hygienists.
Of the 29 dentists who had experienced sharps injuries, only 3 dentists (10.3%, 3/29) had reported their injuries to the work safety team in the hospital (because of incomplete answers, one dentist was excluded). Of the 26 dental hygienists with sharps injuries, 10 (38.5%, 10/26) had reported them. Of the 11 nurses with sharps injuries, 7 nurses (63.6%, 7/11) had reported them.
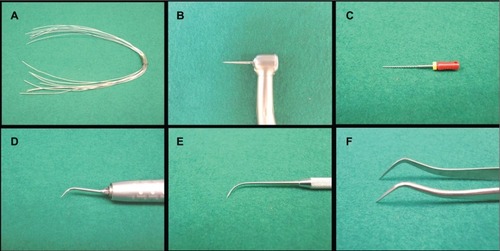
The number of sharps injuries among dentists accounted for 96 cases, and the kinds of instrument that caused injury included 26 cases of a syringe needle, 12 of a suture needle, 18 of a stainless wire (), 22 of a bur (), 11 of a file (), and 7 of a scalar tip (). Sharps injuries among dental hygienists accounted for 81 cases, including 23 cases of a file, 18 cases of a bur, 16 cases of a scalar tip, 10 cases of an explorer (), 6 cases of a syringe needle, 4 cases of a suture needle, 2 cases of a scalpel, and 2 cases of other sharps (a spatula and a stainless mole). Sharps injuries among nurses accounted for 17 cases or more, including 9 cases of a syringe needle, 4 cases of a suture needle, 2 cases of a stainless wire, and 2 cases of dental forceps ().
Questionnaire regarding splash exposures
Of the 58 dentists, 35 (60.3%, 35/58) routinely wore goggles or protective eyewear, including their own glasses. Of the 44 dental hygienists, 15 (34.1%, 15/44) routinely used protective eyewear. Of the 14 nurses, 4 (28.6%, 4/14) wore protective eye equipment.
Splash exposures were more frequently (88.0% and 88.6%) experienced among responded staff of dentists and dental hygienists than nurses, and there was significant difference of the prevalence among job title (). Splash exposures occurred in 51 dentists (88.0%, 51/58), 39 dental hygienists (88.6%, 39/44), and 6 nurses (42.9%, 6/14) (), and conjunctiva exposures occurred in 35 dentists (60.3%, 35/58), 27 dental hygienists (61.4%, 27/44), and 2 nurses (14.3%, 2/14).
Reporting to the Risk Management Work Team in the hospital regarding splash exposure incidents was recognized in 9 dentists (15.5%, 9/58), 12 hygienists (27.3%, 12/44), and 6 nurses (37.5%, 6/16). The motive for using appropriate personal protective equipment was obtained in 52 dentists (94.5%, 52/55), 43 dental hygienists (97.7%, 43/44), and 15 nurses (93.8%, 15/16) after they were provided with the information on the high incidence, approximately 90%, of blood-contaminated splatters during dental surgery.Citation6
Second questionnaire regarding protective eyewear
Three months after the first questionnaire, an additional questionnaire survey was performed regarding compliance with protective eyewear and the motivation for it.
There was a total of 110 respondents (71 dentists and 39 dental hygienists). Of the 70 dentists and 38 hygienists who responded, 31 dentists (44.3%, 31/70) and 18 hygienists (47.4%, 18/38) routinely used protective eyewear.
The information or assumptions that strongly persuaded them to use protective eyewear were #1 (90%, 99/110), #5 (71.8%, 79/110), #12 (66.4%, 73/110), and #2 (58.2%, 64/110) in order (). There was a significant difference between dentists who did and did not routinely wear protective eyewear for #5 and #12 (). No differences were noted between hygienists who did and did not wear protective eyewear and between dentists and hygienists.
Table 4 Questionnaire regarding motivation for wearing protective eyewear and the answers
Table 5 Rate of agreement with the information or assumption that most strongly persuade one to use protective eyewear
Discussion
Reporting splash exposure incidents was not recognized by most of the workers, despite a high incidence of exposure to blood and OPIMs during dental procedures with high-speed instruments. This study demonstrated that dental health-care workers had a low level of concern regarding splash exposures to OPIMs. Saliva is recognized as an OPIM regardless of whether blood is visible, because even when blood is not visible, it can still be present in limited quantities.Citation12,Citation13 Even a small amount of splash exposure during dental procedures are an important issue of occupational safety. In this section, we focus on the splash exposures, comparing them with sharps injuries, which should increase compliance with protective eyewear.
Review of incident reports
Based on daily clinical experience, approximately 90% of oral surgeons have been exposed to blood-contaminated splatters during third molar surgery,Citation6 and even scaling with an ultrasonic hand scalar produced blood-contaminated aerosols,Citation8,Citation9 but the occurrence of splash exposures, which accounted for 18.8% (6/32) of all reported harmful events among health-care workers, seemed low. In addition, six splash exposure incidents reported by dentists and hygienists were mainly caused by liquid chemical materials for dental treatment, and only two cases had the potential for OPIM contamination. Because even needle stick injuries, which are recognized as carrying a more concentrated infection than splash exposures, among surgeons were often not reported to an employee health service,Citation5,Citation14,Citation15 the persons concerned might disregard the events. UK studies estimated that the degree of underreporting of sharps injuries might be as much as 10-fold.Citation16 Cases of occupational splash exposure to blood and OPIMs seemed to occur more often than reported.
Questionnaire regarding sharp instrument injuries
Percutaneous injuries among dentists and hygienists increased with years of clinical experience to approximately 90%, as reported previously.Citation5 Of all 66 workers who had experienced sharps injuries, only 20 workers (30.3%, 20/66) had reported them to the workplace safety team in the hospital. Low compliance with reporting was observed in other articles, ranging from 22% to 49%.Citation5,Citation14,Citation15 This underscores the need for ongoing attention to strategies to reduce such injuries in a systematic way and improve reporting systems so that appropriate medical care can be delivered.Citation5
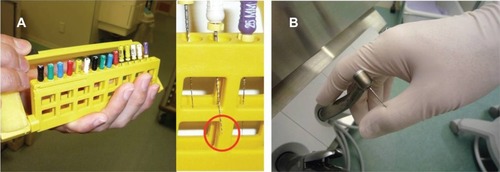
The instruments that caused sharps injuries differed by job title for dentists, hygienists, and nurses. Syringe needles were common instruments among dentists and nurses, while files and burs were common among dental hygienists (). Dental hygienists in our hospital are usually involved in oral care for periodontitis patients as assistants to a dentist and in cleaning instruments () and the dental chair unit (). Unlike dentists and nurses, they were injured during cleaning after treatment, not during treatment. The same result was reported from the UK; that is, more injuries occurred after the treatment session.Citation17 On the other hand, among dental students in training, significantly more incidents occurred while a patient was being treated than during cleanup procedures.Citation18 Hurrying because of multiple procedures and time pressure, as well as a feeling of being ‘rushed’ may result in further medical errors or occupational risks.
Questionnaire regarding splash exposures
The rates of obvious incidents of splash exposures were extremely high – 87.9% (51/58) in dentists and 88.6% (39/44) in dental hygienists – while the rate was approximately half (42.9%, 6/14) in nurses. Dental procedures generally produce splatters and aerosols,Citation8 and protective eyewear should be routinely used by dentists and their assistants according to the University policy, which was written in conformity with CDC guideline.Citation12 However, compliance with routine protective eyewear was low – 60% in dentists and 34% in hygienists – similar to the 44% reported previously.Citation15 Because of the existence of imperceptible contaminated splatters and aerosols,Citation10,Citation19 effective educational information is needed to provide motivation.
The reasons given for not routinely using protective eyewear were, not carrying such eyewear, no time for wearing, unsatisfactory function, and low concern for precautions (data not shown). The answers regarding unacceptable function of protective eyewear among workers who did not use such eyewear routinely were, unclear view with fog and reflection. Though safety devices have been developed, product improvements are needed more, such as clear, nonfog, nonreflective shields that are convenient to carry.
In the second questionnaire, participants most frequently identified the following reasons for wearing protective eye-wear: #1 splatters from the patients’ mouth contain blood, #5 dental operations at our clinic are performed based only on a questionnaire without serious examinations for HBV, HCV, and HIV, #12 most splatters are not recognized by the surgeon intraoperatively, and #2 three splatter exposure incidents pose an infection risk equivalent to one needle stick injury. A significant difference between dentists who did and did not routinely use protective eyewear was recognized in the responses to #5 and #12; the degree of recognition of the need for precaution to avoid eye injuries and conjunctiva exposure may be a factor. Although the number of people infected with HIV is increasing in Japan and is a medico-social problem, the awareness of the potential risk for HIV infection is still low. Quite different results may be obtained if the questionnaire were done at the medical institution where many patients infected with HIV visit. The protective eyewear seemed to be used depending on the risk for infectious pathogens and the equipment quality. Appropriate information from an early educational program appears to play an essential role in increasing compliance with the use of personal protective equipment. To confirm this, further investigations on the effect of interventions, such as reorganization of curriculum for occupational safety especially splash exposures, and educational program for wearing goggle or face shield are required.
Disclosure
The authors report no conflicts of interest in this work.
References
- NIOSHAlert: Preventing Needlestick Injuries in Health Care SettingsWashington (DC)National Institute for Occupational Safety and Health1999 (Publication no. 2000–108)
- YounaiFSMurphyDCKotelchuckDOccupational exposures to blood in a dental teaching environment: results of a ten-year surveillance studyJ Dent Educ200165543644811425248
- TarantolaAKoumaréARachlineAA descriptive. Retrospective study of 567 accidental blood exposures in healthcare workers in three West African countriesJ Hosp Infect200560327628216021690
- Machado-CarvalhaisHPRamos-JorgeMLAuadSMMartinsLHPaivaSMPordeusIAOccupational exposure to potentially infectious biological material in a dental teaching environmentJ Dent Educ200872101201120818923101
- MakaryMAAl-AtterAHolzmuellerCGNeedlestick injuries among surgeons in trainingN Engl J Med2007356262693269917596603
- IshihamaKIidaSKoizumiHHigh incidence of blood exposure due to imperceptible contaminated splatters during oral surgeryJ Oral Maxillofac Surg200866470471018355594
- ShawBATuberculosis in medical and dental studentsLancet1952240040414956023
- HarrelSKMolinariJAerosols and splatter in dentistry: a brief review of the literature and infection control implicationsJ Am Dent Assoc2004135442943715127864
- YamadaHIshihamaKYasudaKAerial dispersal of blood-contaminated aerosols during dental proceduresQuintessence IntIn press2010
- IshihamaKKoizumiHWadaTEvidence of aerosolised floating blood mist during oral surgeryJ Hosp Infect200971435936419201057
- CollinsDRiceJNicholsonPBarryKQuantification of facial contamination with blood during orthopaedic proceduresJ Hosp Infect2000451737510833347
- CDCUpdated US public health service guidelines for the management of occupational exposures to HBV, HCV, and HIV and recommendations for postexposure prophylaxisMMWR Recomm Rep200150152
- US Department of Labor, Occupational Safety and Health AdministrationOccupational exposure to bloodborne pathogens; needlesticks and other sharps injuries; final ruleFed Regist20016653175325
- NagaoMIinumaYIgawaJAccidental exposures to blood and body fluid in the operation room and the issue of underreportingAm J Infect Control200937754154419362389
- WickerSRabenauHFOccupational exposures to bloodborne viruses among German dental professionals and students in a clinical settingInt Arch Occup Environ Health2010831778319626335
- ElderAPatersonCSharps injuries in UK health care: a review of injury rates, viral transmission and potential efficacy of safety devicesOccup Med (Lond)200656856657417065314
- StewardsonDAMcHughSPalenikCJBurkeFJOccupational exposures occurring among dental assistants in a UK dental schoolPrim Dent Care2003101232612621857
- StewardsonDAPalenikCJMcHughESBurkeFJOccupational exposures occurring in students in a UK dental schoolEur J Dent Educ20026310411312269865
- IshihamaKSumiokaSSakuradaKKogoMFloating aerial blood mists in the operating roomJ Hazard Mater20101811179118120554383