Abstract
Background
Several benefits of peer tutoring in medical school teaching have been described. However, there is a lack of research on the perceptions of peer tutoring, particularly from tutees who partake in a long-term clinical skills scheme integrated into the medical school curriculum. This study evaluates the opinions of preclinical tutees at the end of a 2-year peer-tutored clinical skills program and peer tutors themselves.
Methods
A cross-sectional study was conducted in a UK-based medical school that primarily utilizes peer tutoring for clinical skills teaching. A questionnaire was designed to assess the views of preclinical tutees and peer tutors. Likert scales were used to grade responses and comment boxes to collect qualitative data.
Results
Sixty-five questionnaires were collected (52 tutees, 13 peer tutors). Seventy-nine percent of students felt satisfied with their teaching, and 70% felt adequately prepared for clinical placements. Furthermore, 79% believed that peer tutoring is the most effective method for clinical skills teaching. When compared to faculty teaching, tutees preferred being taught by peer tutors (63%), felt more confident (73%), and were more willing to engage (77%). All peer tutors felt that teaching made them more confident in their Objective Structured Clinical Examination performance, and 91% agreed that being a tutor made them consider pursuing teaching in the future. Thematic analysis of qualitative data identified 3 themes regarding peer tutoring: a more comfortable environment (69%), a more personalized teaching approach (34%), and variation in content taught (14%).
Conclusion
Preclinical tutees prefer being taught clinical skills by peer tutors compared to faculty, with the peer tutors also benefitting. Studies such as this, looking at long-term schemes, further validate peer tutoring and may encourage more medical schools to adopt this method as an effective way of clinical skills teaching.
Introduction
Background
The use of peer tutors can be traced back to the time of Ancient Greece.Citation1 In the modern day, peer tutors are often senior students teaching junior students on the same course. “Peer tutoring,” “peer-assisted learning,” and “near-peer teaching” are all terms used currently in the literature to describe a collaborative teaching and learning strategy where learners are active equal partners.Citation2,Citation3
Peer tutoring has been studied for over 40 years, with a variety of research showing its benefits and potential applications.Citation4 This method has been used in a range of contexts such as school teaching, adult learning environments, and medical school settings.Citation5 Implementation of peer tutoring in the medical school curriculum has been called for since 2006, in areas including problem-based learning, anatomy teaching, and revision lectures.Citation6 This approach has also been integrated into the curriculum of some UK-based medical schools for the teaching of clinical skills.Citation7
There are several benefits of peer tutoring in medical school. These have been divided into benefits to tutees, peer tutors themselves, and institutions.
Peer tutors have been shown to create an atmosphere that allows tutees to exchange ideas in a stress-free manner.Citation3 Furthermore, peer tutors are often more accustomed with their courses than faculty staff (professional academic staff employed to teach by the university) and readily integrate new learning experiences and techniques into the curriculum.Citation7
The word “doctor” is derived from the Latin docere, meaning “to teach.” This reflects the fundamental role of a doctor acting as a teacher to students, junior colleagues, and patients themselves.Citation9 This is emphasized by the General Medical Council which states that medical students “must demonstrate basic teaching skills.”Citation10 Therefore, medical schools encouraging students to act as peer tutors may fulfill this. Tutors are also able to reinforce their knowledge of the topic being taught while developing teaching skills and receiving constructive feedback.Citation11 During this process, some faculty members suggest that inexperienced peer tutors can impart inaccurate information.Citation12 However, training peer tutors thoroughly and introducing an evaluation process are suggested ways to tackle this. This institutional support, alongside the practicing of peer tutoring, means that tutors gain relevant skills if they wish to formally pursue teaching in the future.Citation13
There is a suggestion of potential institutional benefits from a cost analysis perspective. Peer tutors may be an economic solution to teach increasing numbers of medical students.Citation14 A further advantage to the use of peer tutors is that clinician recruitment and retention for clinical skills teaching can often be problematic.Citation15
“Clinical skills” is a recognized term used in medical school curriculum to refer to system examinations and practical procedures. Traditionally, clinical skills teaching has been facilitated by faculty members and clinicians on the ward.Citation9 A variety of methods is employed to teach clinical skills, including the use of simulated patients, lecture-based teaching, and ward-based teaching on real patients.Citation16 The use of peer tutors to formally teach clinical skills has been explored.Citation7 A recent meta-analysis looking at 10 studies found that students being taught by peer tutors or faculty performed equally well in OSCEs (Objective Structured Clinical Examinations) and written examinations.Citation8 The majority of studies on peer tutoring look at the effectiveness of clinical skills peer tutoring using exam results as a measure of outcome.Citation17–Citation19
Aims
A limited number of studies evaluate the perceptions of tutees on clinical skills peer tutoring. Of these, students’ views are often assessed after a single session or a short-term program. Our study is unique as it assesses tutees’ perceptions after they have been through a 2-year clinical skills peer tutoring program, integrated into the medical school curriculum.
This study aims to look at tutees’ satisfaction with peer tutoring, how confident they feel being taught by peer tutors, and whether they prefer being taught clinical skills by peer tutors or faculty. Analyzing these perceptions allows for a more representative view due to the tutees’ long-term exposure to the peer tutoring method. We also aim to find out the perspectives of peer tutors themselves on their own learning and teaching progression.
Methods
At St George’s, University of London, a UK-based medical school, all medical students in years 1 and 2 are defined as “preclinical.” As part of their curriculum, these students partake in an integrated 2-year clinical skills peer tutoring scheme which involves weekly 1.5 hour sessions in small groups of 5 or 6. Peer tutors who teach sessions are in years 3, 4, and 5 – “clinical” years. These peer tutors are recruited and trained each year by the university as formal employees via a competitive application process.
In addition to the peer tutoring sessions, preclinical students receive clinical skills demonstrative lectures and small group tutorials from faculty members over the 2 years. Hence, the course structure in preclinical years involves both faculty and peer-tutored teaching. This allows each student to make a direct informed comparison between the 2 techniques. Furthermore, these students undertake 3 weeks of early year clinical experience placements in a range of specialties, aiming to give them an insight into the requirements for placement when in their clinical years.
Study design
A cross-sectional study was conducted using a questionnaire, with 1 section for preclinical students in their 2nd year and one section for current peer tutors (Supplementary materials). The first step of questionnaire design was identifying the gap in the existing research for qualitative and quantitative analysis of perceptions of peer tutors and tutees. Based on this, statements were designed using the standard technique of Likert scales. Comment boxes were used to collect qualitative data via free text responses. The questionnaire was then tested through a pilot study to ensure the questions were concise and easy to understand, and that definitions and meanings were clear. The term “effectiveness” was left to personal interpretation of the respondent, allowing each tutee to express how effective peer tutoring is to them as individuals depending on the factors that they personally value.
Data collection
Preclinical second-year medical students and clinical year peer tutors at this UK-based university were invited to complete the relevant questionnaire section. Recruitment methods included convenience sampling, voluntary sampling via social media platforms, and word of mouth. Each participant gave informed written consent before completing the questionnaire. All questionnaires were completed confidentially with no identifiable data being collected. This study was exempt from ethical approval due to noninterventional, minimal risk and nonidentifiable nature of the data.
Data analysis
Data was entered and checked twice to minimize errors. Statistical Package for the Social Sciences Version 25.0 (IBM Corporation, Armonk, NY, USA) was used to calculate the percentages on the discrete Likert scale data collected. Thematic analysis of the qualitative data involved the data being coded to allow identification of themes. Methods regarding thematic analysis are described in more detail by Braun and Clarke.Citation20
Results
Demographics
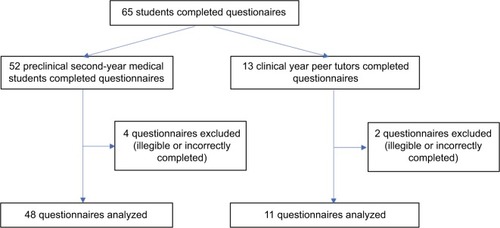
Participant recruitment and exclusion are represented as a flow diagram in . Sixty-three tutees were reached. Of these, 52 filled out questionnaires, giving a response rate of 83%. The cohort of 2nd year MBBS preclinical students was 187. Hence, 34% of the year group was reached. Four questionnaires were excluded due to illegible or incorrectly completed responses, leaving 48 to be analyzed. Twenty-nine students filled the comment boxes.
Sixteen active peer tutors were approached, of whom 13 filled questionnaires, thus giving a response rate of 81%. Two questionnaires were excluded due to illegible or incorrectly completed responses, leaving 11 to be analyzed.
Preclinical students believe peer tutoring is the most effective method for clinical skills teaching
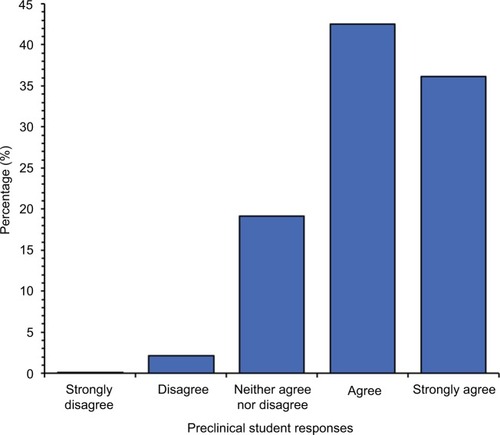
Of the preclinical medical students that responded to our questionnaire, 79% either agreed or strongly agreed that peer tutoring is the most effective method of teaching clinical skills (). Sixty-three percent of students either agreed or strongly agreed that they prefer being taught by peer tutors compared to faculty teachers, with only 14% disagreeing or strongly disagreeing.
Figure 2 Preclinical student responses to the statement “Peer tutoring is the most effective method of clinical skills teaching,” scored on a Likert scale.
When compared to faculty teachers, 73% of students agreed or strongly agreed that they felt more confident learning from peer tutors. Seventy-seven percent of students agreed or strongly agreed that they were more willing to engage in sessions taught by peer tutors compared to faculty teachers. Only 2% of students disagreed that the knowledge of peer tutors was appropriate for the level of teaching they received ().
Table 1 Preclinical students’ perception on being taught by peer tutors compared with faculty teachers, scored on a Likert scale
Preclinical students were also asked to give written feedback on the clinical skills peer tutoring they received (n=29). The 3 themes identified were:
Peer tutoring provides a more comfortable environment (69% of students) eg, “easier to ask older students questions.”
Peer tutors deliver more personalized teaching (34% of students), eg, “peer tutors pitch the content at the right level.”
Variation in content taught by peer tutors (14% of students), eg, “sometimes different tutors say different things which contradict.”
Preclinical students believe peer tutoring of clinical skills is effective at preparing them for clinical placements
With regard to the peer tutor-led clinical skills teaching received in their preclinical years, 79% of students agreed or strongly agreed that they were satisfied ().
Figure 3 Preclinical student responses to the statement “I am satisfied with the peer-tutored clinical skills teaching I received in 1st and 2nd years,” scored on a Likert scale.
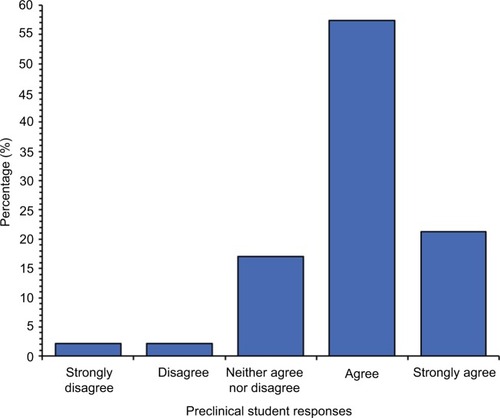
In response to whether they felt their clinical skills tutoring prepared them for clinical year placements, 70% agreed or strongly agreed ().
Table 2 Preclinical students’ satisfaction of peer tutoring and whether peer tutoring was sufficient for clinical year placement preparation, scored on a Likert scale
Peer tutoring has a positive impact on tutors’ learning and development as teachers
The results show that 100% of students agreed or strongly agreed that being a clinical skills peer tutor increased their confidence in their own OSCE performance. Additionally, 91% of tutors agreed or strongly agreed that being a peer tutor has made them consider pursuing teaching in the future ().
Table 3 Peer tutors’ perceptions about confidence in OSCE and pursuing teaching, scored on a Likert scale
Discussion
This study found that preclinical students taught via a 2-year program believe that peer tutoring is the most effective way to learn clinical skills. This may be related to our findings that students feel more confident and more willing to engage in the sessions taught by peer tutors. Additionally, thematic analysis of our study indicates that students feel more comfortable in peer tutoring sessions and that peer tutors provide a more personalized teaching style. These findings can be explained by the theories of social and cognitive congruence.Citation21,Citation22 Tutor and tutee are likely to have similar demographics as well as personal experiences, and hence, peer tutoring sessions tend to have an atmosphere in which an open exchange of ideas is facilitated.Citation6 These similarities between the tutees and tutors are unique to peer tutoring as opposed to more traditional faculty teaching. This may explain our findings that the tutees prefer being taught by peer tutors compared to faculty.
Most studies that compare peer tutoring to faculty teaching within clinical skills only use examination results as an outcome. There are a limited number of studies exploring tutee satisfaction, and these look at problem-based learning and communication skills.Citation23,Citation24 However, 1 study that did look at clinical skills found that tutee satisfaction was similar when taught by peer tutors or faculty, but results were gathered after a single session, rather than after a long-term program of weekly sessions as assessed in our study.Citation25
Another study used focus groups with both peer tutors and tutees, concluding that peer tutor sessions are well received and tutees are satisfied.Citation26 However, results were based on short-term intervention and consisted of entirely qualitative data. This points to a gap in the literature for quantitative analysis of student perspectives into which our study fits. The majority of tutees recruited into our study were satisfied with the peer-tutored clinical skills teaching they received in first and second (preclinical) years.
The tutees in this study believed that the clinical skills peer tutoring scheme has prepared them sufficiently for clinical year placements, indicating this is an effective method of teaching. As these preclinical students have undergone early year clinical experience placements, they have an understanding of what is required of them in clinical year placements, hence supporting the validity of this result.
A small number of students in our study raised the concern that there can be variation among what is taught between peer tutors. In this UK-based medical school, this issue is tackled by recruiting peer tutors through a competitive process that looks at OSCE results. Additionally, peer tutors are briefed by faculty members prior to the session, and standardized teaching documents for each session are provided from which peer tutors are expected to deliver the content. Moreover, peer tutors are expected to teach using Peyton’s 4-step approach, which further standardizes the teaching style.Citation27 Furthermore, there is a circulating faculty member throughout the session to aid with queries that may arise. Tutors must undergo 1 peer review and 2 tutee evaluations each year allowing development of teaching skills. These standardization methods may be why over three-quarters of students in our study agreed that they felt confident in the level of peer tutors’ knowledge.
When analyzing the results of peer tutors, we found that they felt more confident in their OSCE performance due to their involvement in the peer tutoring scheme. This finding of increased confidence fits with Halsted’s concept of surgical training where individuals are encouraged to “learn one, do one, teach one” as the most optimal method of learning new skills.Citation28 Therefore, peer tutors who have learned a clinical skill, used this skill in their clinical year placements, and then taught the skill to preclinical students, have increased confidence in carrying out these skills in examination settings. However, whether this translates to better examination results is unclear.Citation29
The tutors in our study felt that they were more likely to consider teaching in the future, showing that the motivation to teach can start as early as medical school. This is supported by a study which found that tutors, as a result of taking part in a tutoring program, felt more likely to undertake further teacher training and to make teaching a major part of their career.Citation30 Results may be biased due to the phenomenon of reverse causality – do students become more interested in teaching after becoming peer tutors? Or are students with a preexisting interest in teaching more likely to apply to and succeed in the competitive application process to become peer tutors? This bias is minimized in our study due to the added incentive of being a paid employee of the university. This ensures that having the opportunity to teach is not the only motivation for tutors to join the scheme. Furthermore, questions were phrased to specifically assess the impact of being a clinical skills peer tutor, independent of any preexisting interest in teaching.
Limitations
This study included a small sample size, notably in the thematic analysis, which included only 29 respondents. Selection bias is a further limitation as students who volunteered to take part in the study are likely to have stronger views on peer tutoring. Furthermore, the use of Likert scales may not be ideal for assessing a deeper understanding of tutee views. Lastly, there may be other confounding factors that influenced the results, such as variation in the quality of peer tutors and the individual learning styles of the tutees.
Future work
Along with the benefits of peer tutoring that this study has found, some uncertainties remain which need to be addressed. To allow direct comparison, it may also be useful to evaluate the perceptions of 2 groups of students being taught clinical skills, with 1 group taught by peer tutors and 1 by faculty. Following up peer tutors in their medical careers to assess whether they did indeed remain involved in teaching or experienced long-term benefits of being part of the scheme would be valuable in identifying the true extent of advantages. Studies researching the most effective methods for selection and training of tutors would be useful, as these factors can affect the quality of teaching provided. Further research on cost analysis of the scheme, in order to assess the applicability of peer tutoring schemes in medical schools, would also be beneficial.
Conclusion
Despite a myriad of research supporting the use of peer tutoring, there is a lack of quantitative analysis of tutees’ perspectives from a longer-term integrated clinical skills peer tutoring scheme. Our study investigated this unexplored area, concluding that tutees have higher levels of satisfaction, confidence, and engagement levels with peer tutors compared to faculty teachers. Tutees believe that peer tutoring of clinical skills in preclinical years prepares them sufficiently for clinical placement expectations. This study also finds that the perceived benefits extend to the peer tutors themselves, as evidenced by their increased motivation to pursue teaching and improved confidence in their own OSCE performance. This relatively novel style of teaching has already found a footing in medical education. Studies such as this, looking at long-term schemes, further validate peer tutoring and may encourage more medical schools to implement this method.
Disclosure
The authors report no conflicts of interest in this work.
References
- WagnerLPeer teaching: historical perspectives [Internet]Westport, CTGreenwood Press1982 [cited February 16, 2018266 (Contributions to the study of education no. 5. Available from: https://catalog.hathitrust.org/Record/000310721Accessed April 25, 2018
- SecombJA systematic review of peer teaching and learning in clinical educationJ Clin Nurs200817670371618047577
- Ten CateODurningSPeer teaching in medical education: twelve reasons to move from theory to practiceMed Teach200729659159917922354
- HarrisVWShermanJAEffects of peer tutoring and consequences on the math performance of elementary classroom studentsJ Appl Behav Anal19736458759716795443
- Walker-BartnickLABergerJHKappelmanMMA model for peer tutoring in the medical school settingJ Med Educ19845943093156708069
- CateOTDurningSPeer teaching in medical education: twelve reasons to move from theory to practiceMed Teach200729659159917922354
- FieldMBurkeJMMcAllisterDLloydDMPeer-assisted learning: a novel approach to clinical skills learning for medical studentsMed Educ200741441141817430287
- ReesELQuinnPJDaviesBFotheringhamVHow does peer teaching compare to faculty teaching? A systematic review and meta-analysisMed Teach201638882983726613398
- BarrowsHSAn overview of the uses of standardized patients for teaching and evaluating clinical skillsAcad Med1993686443451 discussion 451–4538507309
- General Medical Council, Medical Schools CouncilMedical students: professional values and fitness to practiseLondonGeneral Medical Council2009
- CasagrandJSemsarKRedesigning a course to help students achieve higher-order cognitive thinking skills: from goals and mechanics to student outcomesAdv Physiol Educ201741219420228377433
- RudlandJRRennieSCMedical faculty opinions of peer tutoringEduc Health (Abingdon)20142714924934936
- DandavinoMSnellLWisemanJWhy medical students should learn how to teachMed Teach200729655856517922358
- BenèKLBergusGWhen learners become teachers: a review of peer teaching in medical student educationFam Med2014461078378725646829
- DahlstromJDorai-RajAMcGillDOwenCTymmsKWatsonDAWhat motivates senior clinicians to teach medical students?BMC Med Educ200552716022738
- HudsonJRatnapalanSTeaching clinical skills with patient resourcesCan Fam Physician2014607674677e372e37525022643
- HeckmannJGDütschMRauchCLangCWeihMSchwabSEffects of peer-assisted training during the neurology clerkship: a randomized controlled studyEur J Neurol200815121365137019049555
- HaistSAWilsonJFFossonSEBrighamNLAre fourth-year medical students effective teachers of the physical examination to first-year medical students?J Gen Intern Med19971231771819100143
- BüscherRWeberDBüscherAEvaluation of the peer teaching program at the University Children’s Hospital Essen – a single center experienceGMS Z Med Ausbild2013302Doc2523737922
- BraunVClarkeVUsing thematic analysis in psychologyQual Res Psychol20063277101
- SchmidtHGMoustJHWhat makes a tutor effective? A structural-equations modeling approach to learning in problem-based curriculaAcad Med19957087087147646747
- LockspeiserTMO’SullivanPTeheraniAMullerJUnderstanding the experience of being taught by peers: the value of social and cognitive congruenceAdv Health Sci Educ Theory Pract200813336137217124627
- MillsJKDalleywaterWJTischlerVAn assessment of student satisfaction with peer teaching of clinical communication skillsBMC Med Educ20141421725306897
- CiancioloATKiddBMurraySObservational analysis of near-peer and faculty tutoring in problem-based learning groupsMed Educ201650775776727295480
- AbayEŞTuranSOdabaşıOElçinMWho is the preferred tutor in clinical skills training: physicians, nurses, or peers?Teach Learn Med201729324725428296513
- BurgessADornanTClarkeAJMenezesAMellisCPeer tutoring in a medical school: perceptions of tutors and tuteesBMC Med Educ2016168526956642
- MünsterTStoschCHindrichsNFranklinJMatthesJPeyton’s 4-steps-approach in comparison: medium-term effects on learning external chest compression – a pilot studyGMS J Med Educ2016334Doc6027579360
- CarterBNThe fruition of Halsted’s concept of surgical trainingSurgery195232351852712984268
- BurgessAMcGregorDMellisCMedical students as peer tutors: a systematic reviewBMC Med Educ20141411524912500
- BuckleySZamoraJEffects of participation in a cross year peer tutoring programme in clinical examination skills on volunteer tutors’ skills and attitudes towards teachers and teachingBMC Med Educ200772017598885