Abstract
Background
Previous studies have indicated that suicidal ideation is prevalent in medical students. The factors related to school admission processes and medical school environments contribute to this high prevalence. The consequences of suicidal ideation include suicide attempts and completed suicide. This article reviewed the recent literature on suicidal ideation in medical students.
Materials and methods
A systematic review of the literature was conducted to identify the articles published on the prevalence of suicidal ideation and associated factors in medical students. Original articles published from 2011 were included.
Results
Seventeen studies comprising a total of 13,244 medical students from 13 Western and non-Western countries were included. The prevalence of suicidal ideation ranged from 1.8% to 53.6%. The most frequent factors associated with suicidal ideation in medical students were depression and depressive symptoms, a previous diagnosis of a psychiatric disorder, lower socioeconomic status/financial difficulties, having a history of drug use, and feeling neglected by parents. We did not find studies on interventional studies on suicidal ideation in medical students published in recent years.
Conclusion
We identified a number of non-Western studies published in recent years, overcoming the previous scarcity of research in this area. Findings confirmed that suicidal ideation in medical students remains a significant concern. Future studies should focus on preventive and treatment programs targeting the identified factors associated with suicidal ideation in medical students.
Introduction
About 1 million people die from suicide every year, and in the past 45 years, the rate of suicide has increased by 60% worldwide.Citation1 Suicide is the second leading cause of death among young people after car accident.Citation1 Medical doctors are one of the high-risk groups for suicide.Citation2,Citation3 It seems that this problem arises during medical school.Citation4,Citation5 Medical students in their first year of studies have similar rates of psychological morbidity to the age-matched general population, but experience a worsening of their mental health as they progress through medical studies.Citation6–Citation8 In addition to depression, suicidal ideation is a strong predictor of attempted suicide.Citation9 Suicidal ideation includes thinking about, considering, or planning suicide.Citation10 The rates of suicidal ideation in medical students vary widely, ranging from 6.0% to 43.0%.Citation4,Citation11–Citation13 In addition, female medical students have been found to have higher rates of suicidal ideation than male students.Citation4 Medical students are vulnerable to suicidal ideation because of personal and professional distress resulting from several factors.Citation4 These include information overload, lack of leisure time, financial debt, being away from home, academic load, and work pressure.Citation14 Also, contact with suffering, confronting with death, and caring for vulnerable persons could be other factors that trigger emotional problems in medical students. Some studies also showed that medical students experience depression, burnout, and mental disorders at higher rates than the general population, with deterioration over the medical course.Citation12,Citation15 Research has also reported that school admission processes led to the selection of individuals at risk of vulnerability to depressive disorders and suicidal ideation, namely the traits of perfectionism, obsession, neuroticism, and introversion, as well as low self-esteem.Citation16,Citation17 Negative consequences of poor mental health among medical students include poorer academic performance, substance use (including alcohol), dropout, and suicide.Citation11,Citation18,Citation19 Despite their knowledge of the negative consequences, alcohol and drug use are quite high among medical students and do not differ significantly from other university students.Citation20
Despite easy access to medical care, medical students are often reluctant to seek psychiatric help.Citation21 Concerns about time, confidentiality, stigma, and the potential negative effects on their careers are associated with undertreatment of medical students for mental health problems.Citation21,Citation22 Identification of the prevalence and factors associated with suicidal ideation in medical students can help the timely detection and provision of appropriate interventions to reduce the magnitude of the problem. Furthermore, intervening at an early stage of medical training provides a way to help prevent later mental health problems, including the risk of suicide once students become practicing physicians.
This systematic review accumulated recent knowledge about suicidal ideation in medical students in both Western and non-Western countries.
Materials and methods
Our group conducted a systematic review of suicidal ideation in medical students including articles published up to June 2011.Citation5 In the current systematic review, we provided an update to this research by including articles published between July 2011 and May 2018. PubMed and Cochrane databases were searched for published articles using the keywords “suicidal ideation,” “suicidal behavior,” and “medical students”. In addition, we screened the reference lists of identified articles for any additional relevant studies. The articles surviving selection were downloaded, read in full, and evaluated for eligibility. The articles were included in the systematic review if they were original articles, written in English, and included a sample of medical students. We excluded the following studies from current review: 1) duplicate reports; 2) articles with insufficient data on the prevalence of suicidal ideation for analysis, meta-analysis, or reviews; 3) articles reporting a sample of mixed college students and where medical students were not analyzed as a specific group; and 4) articles published in languages other than English. In the case of multiple publications deriving from the same study sample, we selected the articles reporting the largest or the most recent data.
Results
Article selection
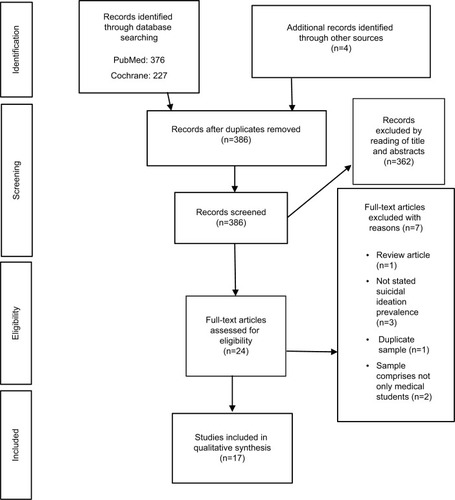
A total of 603 records were obtained from the PubMed and Cochrane database searches. A further four articles were identified through screening the references of these articles. After reading articles titles and abstracts, we selected 24 articles for further evaluation. Of these articles, seven articles were excluded after reading the full text. Finally, 17 studies were included in this systematic review. shows the selection of articles following PRISMA guidelines.
Review of study characteristics
Seventeen studies comprising an overall total of 13,244 medical students recruited in 13 different countries were included.Citation9,Citation23–Citation38 The mean number of medical students included per study was 779, ranging from 114 to 4,402. All studies were cross-sectional in design. Suicidal ideation was assessed relating to the current time, over the past 12 months, during medical studies, and lifetime. The majority of studies measured suicidal ideation using specific questions.Citation23,Citation24,Citation26,Citation28,Citation29,Citation31–Citation34,Citation36,Citation37 The following scales were used to measure suicidal ideation in the previous studies: item 9 from the Beck Depression Inventory,Citation25 Beck’s Suicidal Ideation Scale (BSI),Citation27 the Suicide Behaviors Questionnaire,Citation30 item 9 of the Patient Health Questionnaire (PHQ),Citation9 and item 6 of the Kutcher Adolescent Depression Scale.Citation38 One study used questions about suicidal ideation as well as the General Health Questionnaire.Citation35 summarizes all the included studies, including country, year of training, number of students, instruments used to measure suicidal ideation, the prevalence of suicidal ideation, and other significant findings in each study.
Table 1 Characteristics of included studies
Prevalence of suicidal ideation
The prevalence of suicidal ideation ranged from 1.8% to 53.6%, reflecting some heterogeneity among the studies. In consideration of prevalence according to timeframe, current suicidal ideation ranged from 1.8% to 24.6%, during medical school time from 3.7% to 4.7%, over the past 12 months from 7% to 35.6%, and lifetime from 2.9% to 53.6%. One study explicitly stated that the prevalence of suicidal ideation identified among medical students was higher than that for the age-matched general population.Citation34
One study found a significantly higher prevalence of suicidal ideation in male students than female medical students,Citation26 four studies found a significantly higher prevalence in female students than male students,Citation27,Citation29,Citation36,Citation37 and the remaining 12 studies did not find any statistically significant differences between the two genders.Citation9,Citation23–Citation25,Citation28,Citation30–Citation35,Citation38
Regarding the relationship between suicidal ideation and year of study, one study found that students in clinical years had a higher prevalence of suicidal ideation than those in preclinical years,Citation23 two studies did not find any significant differences regarding year of study,Citation25,Citation34 and a further two studies found a higher prevalence of suicidal ideation in the first/pre-clinical years of medical studies.Citation27,Citation35
The factors most frequently associated with suicidal ideation in medical students were depression and depressive symptoms,Citation9,Citation23,Citation25,Citation33,Citation34 previous diagnosis of a psychiatric disorder,Citation29,Citation34 lower socioeconomic status/financial difficulties,Citation33,Citation36 having a history of drug use,Citation10,Citation29 and feeling neglected by parents.Citation10,Citation29 Other factors associated with suicidal ideation included dissatisfaction with academic performance as a primary concern,Citation10 a history of impulsive or reckless behavior in difficult situations,Citation37 feeling of being better off dead,Citation37 nonworking mothers,Citation37 living alone,Citation25 thoughts of abandoning the course,Citation25 sleep disorders,Citation33 previous suicidal attempts,Citation34 mother’s education level,Citation26 and mother’s parenting style.Citation26
It is interesting to note that some studies reported similar levels of cannabis use in medical students compared to that in the general population, despite medical students having a better knowledge about the associated risks to both their own health status and that of their future patients.Citation31
Few studies have been conducted on the protective factors of suicidal ideation in medical students. However, being married was identified as a factor associated with lower odds of suicidal ideation within the previous 12 months.Citation32
Discussion
This systematic review included 17 studies about suicidal ideation in medical students published between July 2011 and May 2018. We found evidence that suicidal ideation in medical students presents a concern. Three studies were published in 2017, four in 2016, one in 2015, four in 2014, and five in 2012. Our previous systematic review consisted of 10 studies published between January 2005 and June 2011.Citation5
Recently, an increase in the articles published outside US/Canada and Europe was observed, with the current systematic review including three studies from Europe (Portugal, Germany, and Serbia),Citation28,Citation30,Citation36 two from USA,Citation31,Citation32 nine from Asia (Nepal, United Arab Emirates, China, Pakistan, and India),Citation9,Citation10,Citation23,Citation24,Citation26,Citation29,Citation33,Citation37,Citation38 two from Africa (Egypt and South Africa),Citation27,Citation34 and one from South America (Brazil).Citation25 In contrast, the overwhelming majority of studies published before 2011 were from USA, Canada, and Europe. Thus, suicidal ideation is a problem worldwide, independent of geographical location, for both Western and non-Western countries. The prevalence of suicidal ideation seems not to differ between countries from different continents or locations. Interestingly, we did not find any published articles from Australia or New Zealand.
The range in prevalence of suicidal ideation in medical students is quite large among studies. Two important factors contribute to this: the different instruments used to measure suicidal ideation and the different timeframes in which suicidal ideation was evaluated. The use of different instruments hampered comparisons of the prevalence of suicidal ideation among studies. This systematic review indicates that suicidal ideation is a relevant problem in medical students and probably higher than age-matched general population.
The results are inconsistent regarding the association between suicidal ideation and gender. This is similar to the pattern found in studies published before 2011. Recent findings show some trend toward indicating being female as a risk factor for suicidal ideation in medical students, as the majority of studies either did not find a statistically significant difference between genders or found that females are more prone to suicidal ideation.
Our results were also inconclusive regarding the year of study in medical school and prevalence of suicidal ideation. The results are almost equally divided in findings taking into account the year of study in medical school. Therefore, we cannot state whether suicidal ideation prevalence progressively increases with time spent in medical school.
As mentioned earlier, there is a paucity of published research on preventive and treatment interventions. We found only one recent intervention study for suicidality, and this was not in medical students but in paramedical students (and therefore excluded from the current review).Citation39 Muriungi and Ndetei conducted a clinical trial across seven campuses in Kenya Medical Training College involving an experimental group (n=1181) and a control group (n=1926) to determine the effectiveness of psychoeducation on suicidality as well as other symptoms (depression, hopelessness, anxiety, and risk of substance abuse). Suicidal ideation was measured using Beck’s Scale for Suicidal Ideation at baseline, 3 months, and 6 months. The experimental group was assigned to four psychoeducation sessions (totaling 16 hours), which included lectures, simulations, group discussions, and role-plays about the factors associated with suicidality and other symptoms relating to mental health. There were no interventions in the control group. Results revealed no statistically significant reduction in symptom severity between the experimental and control groups at 3 months, but there was a significant difference at 6 months follow-up. This study demonstrates that a simple and easy intervention like psychoeducation can be effective in reducing not only suicidal ideation but also depression, hopelessness, suicide plans, suicide attempts, anxiety, depression, and risk of substance abuse.
The current systematic review has several limitations. We only included articles published in English, and in doing so, we could have excluded other important researches. Also, we did not perform a meta-analysis because the use of different instruments and timeframes limited the application of this approach. Future studies should focus on the contribution of medical school culture in suicidal ideation, trying to identify which particular factor in medical education could contribute to suicidal ideation in medical students.
Also, future research should study interventions to reduce suicidal ideation experienced by medical students. Two of the factors found here to be associated with suicidal ideation were drug use and financial status, and interventions addressing these could be useful. Identifying depression and depressive symptoms, the most frequent factors associated with suicidal ideation in medical students, as well as the treatment for psychological distress, should be included in interventions. Preliminary data suggest that simple and general well-being interventions could have significant results in lowering rates of mental health problems, including suicidal ideation, in medical students. Also, we think self-care and self-reflecting in medical education, for example groups of reflecting students, could be a way of a preventive method for suicidal ideation and other psychological problems. Approaching ways of reducing the reluctance of help-seeking in medical students should be addressed, reducing de-stigmatization of mental health problems.
Conclusion
The articles published in recent years overcame the scarcity of published non-Western studies in previous years. Recent findings confirm that suicidal ideation is a significant problem for medical students. The major risk factors for medical students in terms of suicidal ideation included having depression or depressive symptoms, any other psychiatric diagnoses, feeling neglected by parents, having a history of drug use, low socioeconomic status, and/or financial difficulties. Future studies should focus on preventive as well as treatment programs to reduce suicidal ideation in medical students, and thus reducing suicidal attempts and completed suicides.
Disclosure
The authors report no conflicts of interest in this work.
References
- World Health OrganizationPreventing Suicide: A Global ImperativeGenevaWorld Health Organization2014 Available from: http://apps.who.int/iris/bitstream/10665/131056/1/9789241564779_eng.pdf?ua=1&ua=1Accessed July 18, 2018
- ShanafeltTDBalchCMDyrbyeLSpecial report: suicidal ideation among American surgeonsArch Surg20111461546221242446
- SchernhammerESColditzGASuicide rates among physicians: a quantitative and gender assessment (meta-analysis)Am J Psychiatry2004161122295230215569903
- DyrbyeLNThomasMRMassieFSBurnout and suicidal ideation among U.S. medical studentsAnn Intern Med2008149533434118765703
- Moutinho CoentreRLuisa FigueiraMDepression and suicidal behavior in medical students: a systematic reviewCurr Psychiatry Rev201511286101
- CarsonAJDiasSJohnstonAMental health in medical students. A case control study using the 60 item General Health QuestionnaireScott Med J200045411511611060914
- RosalMCOckeneISOckeneJKBarrettSVMaYHebertJRA longitudinal study of students’ depression at one medical schoolAcad Med19977265425469200590
- YusoffMSBMat PaMNEsaARAbdul RahimAFMental health of medical students before and during medical education: a prospective studyJ Taibah Univ Med Sci2013828692
- SobowaleKZhouNFanJLiuNShererRDepression and suicidal ideation in medical students in China: a call for wellness curriculaInt J Med Educ20145313625341209
- MenezesRGSubbaSHSathianBSuicidal ideation among students of a medical college in Western Nepal: a cross-sectional studyLeg Med2012144183187
- TyssenRVaglumPGrønvoldNTEkebergOSuicidal ideation among medical students and young physicians: a nationwide and prospective study of prevalence and predictorsJ Affect Disord2001641697911292521
- GoebertDThompsonDTakeshitaJDepressive symptoms in medical students and residents: a multischool studyAcad Med200984223624119174678
- MartinacMSakićMSkobićHJakovljevićMSuicidal ideation and medical profession: from medical students to hospital physiciansPsychiatr Danub2003153–418518819114926
- YiuVSupporting the well-being of medical studentsCMAJ2005172788989015795410
- DyrbyeLNThomasMRPowerDVBurnout and serious thoughts of dropping out of medical school: a multi-institutional studyAcad Med20108519410220042833
- HirschfeldRMKlermanGLPersonality attributes and affective disordersAm J Psychiatry197913616770758831
- HumphrisGKaneySThe encouragement of ‘perfect’ health professionalsMed Educ199832545245510211284
- MidtgaardMEkebergØVaglumPTyssenRMental health treatment needs for medical students: a national longitudinal studyEur Psychiatry200823750551118774273
- MandalAGhoshASenguptaGBeraTDasNMukherjeeSFactors affecting the performance of undergraduate medical students: a perspectiveIndian J Community Med201237212612922654287
- WebbEAshtonCHKellyPKamahFKamaliFAn update on British medical students’ lifestylesMed Educ19983233253319743790
- TjiaJGivensJLSheaJAFactors associated with undertreatment of medical student depressionJ Am Coll Heal2002535219224
- GivensJLTjiaJDepressed medical students’ use of mental health services and barriers to useAcad Med200277991892112228091
- AdhikariADuttaASapkotaSChapagainAAryalAPradhanAPrevalence of poor mental health among medical students in Nepal: a cross-sectional studyBMC Med Educ201717123229183315
- AmiriLVoracekMYousefSSuicidal behavior and attitudes among medical students in the United Arab EmiratesCrisis201334211612323195458
- TorresARCamposLMLimaMCPRamos-CerqueiraATASuicidal ideation among medical students: prevalence and predictorsJ Nerv Ment Dis201820616016828837427
- SunLZhouCXuLLiSKongFChuJSuicidal ideation, plans and attempts among medical college students in china: the effect of their parental characteristicsPsychiatry Res201724713914327889604
- AhmedSAOmarQHAbo ElamaimAAForensic analysis of suicidal ideation among medical students of Egypt: a crosssectional studyJ Forensic Leg Med2016441427589377
- CoentreRFaravelliCFigueiraMLAssessment of depression and suicidal behaviour among medical students in PortugalInt J Med Educ2016735436327794561
- OsamaMIslamMYHussainSASuicidal ideation among medical students of Pakistan: a cross-sectional studyJ Forensic Leg Med201427656825287803
- MileticVLukovicJARatkovicNAleksicDGrgurevicADemographic risk factors for suicide and depression among Serbian medical school studentsSoc Psychiatry Psychiatr Epidemiol201550463363825205334
- MacleanLBoozaJBalonRThe impact of medical school on student mental healthAcad Psychiatry2016401899125749920
- DyrbyeLNWestCPSateleDBurnout among U.S. medical students, residents, and early career physicians relative to the general U.S. populationAcad Med20148944345124448053
- FanAPKosikROMandellGASuicidal ideation in medical students: who is at risk?Ann Acad Med Singapore201241937738223052431
- van NiekerkLScribanteLRaubenheimerPJSuicidal ideation and attempt among South African medical studentsS Afr Med J20121026 Pt 237222668910
- MenezesRGSubbaSHSathianBSuicidal ideation among students of a medical college in Western Nepal: a cross-sectional studyLeg Med (Tokyo)201214418318722522041
- WegeNMuthTLiJAngererPMental health among currently enrolled medical students in GermanyPublic Health20161329210026880490
- GoyalAKishoreJAnandTRathiASuicidal ideation among medical students of DelhiJ Ment Heal Hum Behav20121716070
- YoussefMDaudSShafiqueMMGender difference in depression and suicidal ideation of medical studentsPJMHS201610310531056
- MuriungiSKNdeteiDMEffectiveness of psycho-education on depression, hopelessness, suicidality, anxiety and substance use among basic diploma students at Kenya Medical Training CollegeSouth African Journal of Psychiatry201319210