Dear editor
As medical students, we found ‘Suicidal ideation in medical students: recent insights’ interesting to read. Based on this article, we propose suggestions for the next systematic review.Citation2
Concerning the associated factors contributing to suicidal ideation (SI) in medical students we can only infer the ranking from the order in which they are mentioned. Hence, these claims could be substantiated with the percentages for each.
We agree with the author that there is a correlation between stigma and the under-treatment of SI. Rivera-Segarra et al, 2018Citation3 suggest educating the medical students about stigma, which could prove beneficial for both students and their future patients. Of those who completed suicide, at least 50% contacted their physicians in the preceding month. Moreover, stigma can also co-exist with non-disclosure of SI; in the male medical student population, a greater suicide stigma was observed.Citation3
To broaden the investigation, the method can be modified to search for “suicid*” or specific words such as “suicidality” or “suicide intervention” or “suicide literacy”, along with “medical students” in the advanced search.
To provide more relevant insight into the causes of SI in medical students, we suggest that the author includes recent articles that take into account the Big-Five personality traits (especially stability and dominance), in work related settings using the Business-Focused Inventory of Personality 6 Factors (BIP-6F) scale, since those possessing these traits can be more susceptible.Citation1
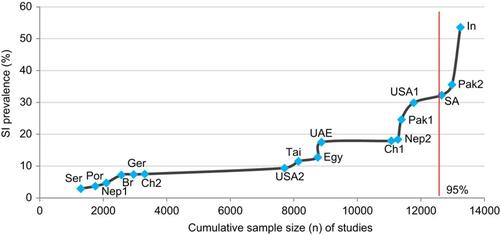
To address the heterogeneity of SI prevalence between the studies, we have plotted SI prevalence against cumulative sample size of studies ordered by increasing SI prevalence. The “India” study seems to be an outlier (), as it lies outside the top 5%. To probe this further, we estimated the mean and standard deviation () and obtained values of 13.8% and 10.3% respectively. The 95% confidence interval is [−6.3(0), 34.0]. The “India” (and perhaps ‘Pakistan 2ʹ) study lies outside this; hence it inflates the range of SI prevalence by almost double. It may be worthwhile to take this into account, as it had the fourth lowest sample size (the geographical proximities of the outliers India and Pakistan might suggest a geographical stratification of SI).Citation2
Table 1 Standard deviation (SD) estimation indicates that the “India” study is an outlier
Moreover, to estimate the SI prevalence during university from the lifetime SI data, one should search for SI prevalence up to the age of 18 (assumed to be the same for both medical and non-medical students). Then, subtract this value from the lifetime SI rate of medical students to give SI rate within medical school.
From personal experience, we feel that graduate medical students may be more equipped to deal with the pressure of medical school. We would be interested to see if the type of program the student is in and their year of study affects SI prevalence. We predict that doing medicine as a first degree correlates with an increased SI prevalence.
Finally, we believe this article has given us a better perspective on this subject and identifying suicidal ideation in individuals can hopefully lead to more effective suicide prevention strategies.
Disclosure
The authors report no conflicts of interest in this communication.
References
- Chow WS, Schmidtke J, Loerbroks A, Muth T, Angerer P. The relationship between personality traits with depressive symptoms and suicidal ideation among medical students: a cross-sectional study at one medical school in Germany. Int J Environ Res Public Health. 2018;15(7):1462. doi:10.3390/ijerph15061188
- Coentre R, Góis C. Suicidal ideation in medical students: recent insights. Adv Med Educ Pract. 2018;9:873–880. doi:10.2147/AMEP.S162626
- Rivera-Segarra E, Rosario-Hernández E, Carminelli-Corretjer P, Tollinchi-Natali N, Polanco-Frontera N. Suicide stigma among medical students in Puerto Rico. Int J Environ Res Public Health. 2018;15(7):1366. doi:10.3390/ijerph15061188