Abstract
Background
The emergency medical services program at the College of Applied Medical Sciences, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Kingdom of Saudi Arabia, was adapted from the integrated problem-based learning curriculum of Flinders University, Adelaide, South Australia.
Purpose
The purpose of this article is to discuss the major adaptations required for adoption of the full-fledged PBL curriculum, use of sequential blocks, and multilayer alignment of the curriculum.
Methods
A logical model and step-by-step approach were used to design the curriculum. Several studies using Delphi methods, focus group interviews, and expert opinions were performed to identify the priority health problems; related competencies, learning objectives, and learning strategies; the web-based curriculum for delivery; student assessment; and program evaluation.
Results
Sixty priority health problems were identified for inclusion in different blocks of the curriculum. Identified competencies matched the satisfaction of different stakeholders, and ascertained learning objectives and strategies were aligned with the competencies. A full-fledged web-based curriculum was designed and an assessment was created that aligned with a blueprint of the objectives and the mode of delivery.
Conclusion
Step-by-step design ensures the multilayer alignment of the curriculum, including priority health problems, competencies, objectives, student assessment, and program evaluation.
Introduction
King Abdulaziz Medical City, Riyadh, Kingdom of Saudi Arabia (KSA), commenced its operations in May 1983. Since then, it has continued to expand, while providing services for a rapidly growing patient population in all of its catchment areas. The King Saud bin Abdulaziz University for Health Sciences includes the College of Applied Medical Sciences, a multifacility medical center. Under the university structure, the College of Applied Medical Sciences includes the colleges of medicine, academic affairs, training and development, medical and nursing education, the research center, a 900-bed tertiary care hospital, and a large emergency center (encompassing pediatric emergency care, adult emergency care, critical care, and urgent care centers) that offers primary teaching for the emergency medical services (EMS) students.Citation1
Over the last 3 decades, the KSA has experienced a sharp improvement in its economic status and development. Health services in particular have developed to a great extent, as witnessed by accessibility and coverage indicators, and complemented by improvement in health indicators such as mortality, morbidity, and life expectancy.Citation2 However, national health professional development has not kept pace with infrastructural growth. The percentage of Saudi nationals working in the health field is very low (25%) compared with the education and agriculture sectors. The College of Applied Medical Sciences is the first college in the KSA that aims to produce graduates of EMS, to implement a compatible program that is community oriented,Citation3 and to use teaching and learning strategies that are student centered.Citation4 These strategies foster an active role for students and provide delivery of knowledge to them in an integrated and multidisciplinary fashion.
The urgent need for an expansion in health professions education to fill the sizeable gap in health manpower in KSA is well justified. The need to train EMS professionals at the same rate of provision of infrastructural facilities is a high priority. Currently the KSA should have one ambulance for every 5000 persons and therefore 27.6 million persons would require 5520 ambulances. Each ambulance requires a staff of six trained EMS personnel, 24 hours a day, 7 days a week – that is, two per shift for three rotating shifts. As a corollary, an approximate number of 33, 120 trained EMS personnel are required in the KSA. Currently there are 1550 emergency medical technicians (EMTs) spread across different regions of the KSA and 19 paramedics available only in Riyadh. National Guard Health Affairs in Riyadh has five paramedics, six intermediate EMTs, 21 basic EMTs, ten advanced life support and ten basic ambulances, and a record of transporting 300 emergency cases per month to the hospital from the community.Citation1
The rationale for establishing the EMS program at the College of Applied Medical Sciences, King Saud bin Abdulaziz University for Health Sciences, Riyadh, KSA, is the need to address the shortage of national Saudi paramedics, in terms of both quality and quantity; to provide a state-of-the-art model for EMS education; to promote research that enhances the standards of emergency health care provided to the citizens of the KSA; and to avail the college of the educational potential in the existing health facilities in the National Guard Health Affairs for proper training of students and for high-quality research. This ensures a cost-effective and efficient utilization of national resources and provides collaboration with regional and international EMS institutions to promote globally the standards of emergency services. Evidently, the cost-effective and efficient utilization of national resources is important not only globally but also locally: intensive care units of Saudi hospitals are a particular challenge for health managers in this respect.Citation5 The college’s EMS program is based on student participation in learning through reflective exercisesCitation6 and a problem-based approach, in a web-based simulation or a traditional class room,Citation7 to promote analytical thinking and engagement in lifelong learning, together with a strong focus on health research and a philosophy of defining professionalism through both qualitative and quantitative research – practical field experience. Problem-based cases (ie, patient-centered learning)Citation8 need to be tailored together with supervision, otherwise they may not serve the purpose of problem-based learning (PBL)Citation9: the integration of students within and across years; the use of new health information technologies; a focus on clinical reasoning; assessment that emphasizes relevance, feedback, and comprehensiveness.
The EMS program has four themes: (1) basic and clinical sciences, (2) community and paramedical, (3) patient and paramedical, and (4) personal and professional development. These themes provide the framework for both the new curriculum and the assessment. The basic and clinical sciences theme, the most substantial of the four, includes the preclinical and major paraclinical and clinical disciplines, with a focus on medical emergencies; the community and paramedical theme deals with population health issuesCitation10; the patient and paramedical theme encompasses a range of clinical skills, including emergency skills, that students need to acquire; and the personal and professional development theme covers ethics, medical humanities, and professionalism.Citation11,Citation12 There are many sources for comprehensive information regarding how to design various bachelor degree curriculums, Citation13,Citation14 but the team approachCitation15 utilized by Flinders University, Adelaide, South Australia, is relatively unique in developing a student-based, problem-based, work-integrated, and patient-based curriculum.Citation16
Curriculum design, structure, and management
While the themes of the EMS program provide the framework for the whole curriculum, the central feature of the curriculum’s education methods is PBL, Citation17 conducted in small groups and supported by lectures and theme sessions. Curriculum design has been based on sound national and international standards and research in teaching and learning. Curriculum design draws on the principles of symbiosis between clinical learning and the broad health care system, which includes influences such as the social, psychological, and epidemiological context of health, and the political, ethical, and economic environment. There is a holistic approach to the role a paramedic plays in the broad health care system.Citation18 Furthermore, in the broad health care system an emphasis is placed on local, national, and international clinical practice guidelines – these ensure that clinical competence of students is based on the most current evidence-based data available. Furthermore, students need to be exposed to the practical field early in the curriculum, which aims for students to acquire generic skills of communication in the emergency setting together with systematic history taking and complete physical examination skills.Citation12,Citation19
With regard to a model of clinical reasoning, the aim is to offer a model that will allow students to develop sophisticated reasoning skills applicable in clinical environments.Citation19,Citation20 Utilizing information health technology to support the learning process means presenting a “trigger” in a multimedia format. Starting with the problem trigger, the reasoning model then determines the way in which resources are presented to the students. During tutorial sessions, individual students identify the cues, formulate the problem, generate and organize hypotheses, and make a differential diagnosis. Furthermore, the students plan inquiry, seeking patient and epidemiological data to distinguish between hypotheses and reformulate the problem in order to identify learning issues to guide individual study. During tutorial sessions, the student may reach a diagnostic decision and research questions feedback on the problem.Citation21
Problems and clinical scenarios were designed to introduce important medical emergency issues across all four themes of the EMS program. A condition or disease state could be submitted if it met one or more of the following criteria: common in terms of incidence/prevalence or as a cause of death; life-threatening; illustrative of an important clinical or scientific principle; and problem covering a spectrum of illness that is related to EMS across all age groups, in both urban and rural settings, and encompassing various ethnic groups of the Saudi community. In the real-life emergency setting every presenting case is not clear, and clinical reasoning may be helped by script concordance if a problem scenario is uncertain.Citation22
Curricular phases of the EMS program
The EMS program has two curricular phases. Phase I covers one semester and includes 2 preprofessional years. Phase II comprises semesters 1–4 of 2 professional years, like that of the Flinders University curriculum. The paramedic curriculum follows a logical progression from basic emergency care in the first semester, through advanced concepts of pathophysiology of major body systems coupled with advanced life support practiced in the second and third semesters. Psychology and mental illness management form a significant portion of the third semester. The fourth semester focuses on building the skills and knowledge into a biopsychosocial, holistic approach to case management, incorporating leadership, safety, clinical assessments, and administration of therapies. Throughout this progression through the semesters, there is an emphasis on learning practical skills and their application in medical emergencies. Learning on campus is supported by ambulance clinical placements and a limited number of placements within other health care facilities.
Sixty priority health problems were identified for inclusion as sequential blocks of the curriculum in Phase II. These blocks vary in length from 4 to 10 weeks, with a problem presented each week. Up to eight key issues or learning topics are identified within each block, with the topics expected to arise naturally during the week as the basis for self-directed learning. These major issues are addressed in lectures and theme sessions that include practical sessions, clinical tutorials, evidence-based medicine exercises, and class discussions. In the final semester the students have 10 weeks of hospital rotation, which aims to obtain experience in the major clinical fields of the pediatric intensive care unit, pediatric emergency care, the adult intensive care unit, adult emergency care, trauma emergency care, and the obstetric unit. Students also have 10 weeks of the aforementioned applied paramedic practice, which aims to provide the students with an integration of all the paramedic-related skills, knowledge, and attitudes, in order to enable them to graduate with confidence and with a thorough grounding in paramedic practice in preparation for their internship.
Objectives of the project
The two objectives were (1) adaptation and modification of the EMS program from Flinders University to fit local regulations and university strategies and (2) to provide a state-of-the-art model for EMS education that is student centered and community oriented. More details of the Flinders University curriculum for bachelor of health sciences degrees for paramedics are available online.Citation16
Method
Five studies, which will be described briefly, were conducted (). The aim of the first study (study 1) was to identify the common emergency problems. Study 1 involved 20 participants: ten paramedics (male = 8; female = 2), all of whom held a bachelor degree from the United States and had over 7 years’ experience, and ten male emergency consultants, including one pediatric emergency consultant, all of whom had more than 5 years’ experience. Modified Delphi method in two roundsCitation23 was used with all participants. The first round was used to list the most common problems (cases) the participants encounter in emergency services in the cardiovascular system (CVS) and in the respiratory system (RS). The second round involved reaching consensus on the list of most common problems.
Table 1 Brief summary of the five studies
The aim of the second study (study 2) was to prioritize the health problems. The study design was cross-sectional. The breakdown of participants for study 2 was as follows: 25 emergency consultants; five paramedics; ten EMTs; and five medical educationists. The indicators suggested by McDonald et alCitation24 were used for rating the problems: prevalence; 1-year case fatality rate; level of remaining quality of life; urgency of the illness condition; prevention (availability and applicability); diagnostic process (accuracy and applicability); intervention in established cases (efficacy); and educational impact ().
Appendix 1 The health problems evaluation grid suggested by MacDonald et alCitation24
The aims of the third study (study 3) were to identify competencies, learning objectives, and learning strategies. The design was the Modified Delphi method in two roundsCitation25 and the participants were the same participants as in study 1. In the first round, the participants were asked to list statements regarding competencies, learning objectives, and learning strategies. In the second round, each participant was requested to rate each statement on a five-point Likert scale according to the importance of the statement after analysis. A statement with a mean score less than 3 was excluded and a final list of competencies, learning objectives, and learning strategies was formulated.
The fourth study (study 4) aimed to reach a consensus on the EMS program and its mission, vision, and values. The adopted design was focus group discussion, which comprised two professors of medical education with more than 20 years’ experience in teaching, two paramedics, and three project designers.
The aims of the fifth study (study 5) were to work on designing problems and weekly learning objectives and to design CVS and RS blocks. The participants comprised five paramedics, two professors, two ER consultants, and two block designers. In the first round (step 1), a workshop was organized and the participants, divided into two groups, discussed designing problems and learning objectives: one group was responsible for deciding about the learning objectives of a specific week and the other group was asked to design problems. To achieve the CVS and RS block design objective, an expert focus group (step 2) comprising the same participants as for step 1 discussed block designing. The designed problems were switched between the two groups to finally reaching a consensus.
The integrated problem-based learning curriculum of Flinders UniversityCitation16 was selected for adaptation to the Saudi context, and the following exercises were performed for the purposes of adoption, synchronization, adaptation, modification, implementation, and evaluation. The details of the adoption process and, especially, of the justifications for this are given in the Results section. The author would like to emphasize that there are no set definitions for the terms “modification” and “adaptation”. As a result, these terms are often used imprecisely and interchangeably. Generally, modifications and adaptations refer to individualized curriculum changes that reduce the difficulty and size of a student’s workload. However, accommodations usually refer to tools and techniques that help students keep up with a standard workload identical to that of their peers. In other words, modifications and adaptations change what a student is expected to learn while accommodations change how a student learns. The author uses both terms adaptation and modification throughout this article.
Results
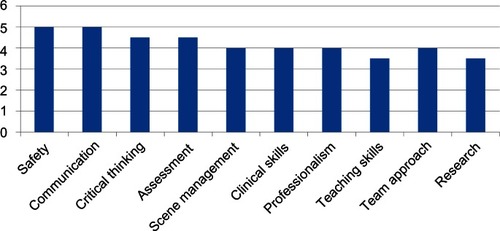
The identification of emergency health and prioritized health problems was used to modify the curriculum, and most relevant emergencies were retained in the final curriculum. Using a modified Delphi method,Citation23 the expert group identified the following cardiovascular problems (), given in the order reflected by their scores (highest to lowest on a scale from 0 to 14 [where 0 is the lowest magnitude and 14 indicates the highest magnitude]): heart failure, acute coronary syndrome, shock, myocardial infarction, arrhythmia, hypertension emergency, myocarditis, aortic dissection, heart block, cardiomyopathy, and deep vein thrombosis. The respiratory problems (), also given in order of score (highest to lowest on scale 0–14), were as follows: acute respiratory syndrome, bronchial asthma, foreign body aspiration, chronic obstructive pulmonary disease, acute respiratory failure, pulmonary embolism, pneumonia, bronchiolitis, and bronchitis.
Figure 1 Cardiovascular problem magnitude.
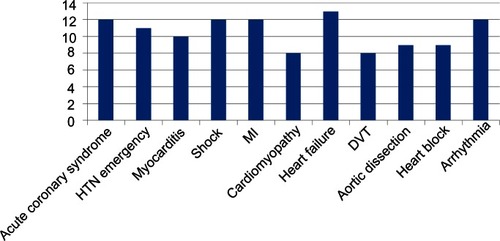
Figure 2 Respiratory problem magnitude.
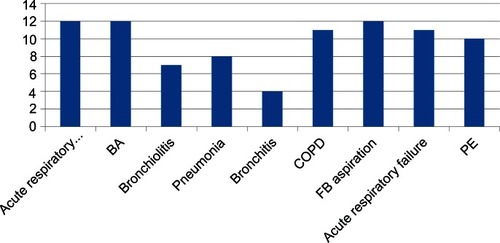
Using a modified Delphi method,Citation23 the expert group identified the following competencies as reflected by their scores (highest to lowest, on a scale from 0 to 6) (): safety and communication; critical thinking and assessment; scene management, clinical skills, professionalism, and team approach; and teaching skills and research.
Expert group formulated vision statement that EMS programCitation16 must be recognized as an excellence degree course that utilizes advanced concepts of best evidence-based medical emergency services education to attract the best students and faculty. The mission of the EMS center of excellence is to provide outstanding prehospital medical education that covers not only paramedic-specific learning but also learning related to the political, administrative, social, epidemiological, and medicolegal environment, which is applicable to the entire Saudi health care system. The identified values were (1) faculty, staff, and students who demonstrate the highest ethical standards; (2) faculty, staff, and students who demonstrate integrity; (3) faculty, staff, and students who demonstrate professionalism throughout their teaching and practice careers; (4) relevance, in terms of the faculty, staff, and students being responsive to the needs of the community through addressing priority emergency health problems; (5) respect and cultural sensitivity, ie,. faculty, staff, and students treat others with respect and dignity, honoring community culture and traditions; and (6) high-quality leadership and teamwork that faculty and students teach and learn, as well as high-quality education models with leadership behavior and performance and a spirit of sharing and teamwork.
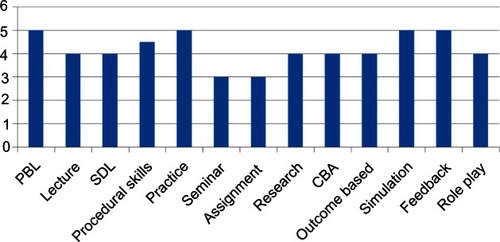
With regard to the learning objectives and strategies (), the expert panel tailored five objectives of the Flinders University EMS programCitation16 by scoring objectives from least important (scoring 1) to most important (scoring 5). The two standing objectives were (1) to develop competence at patient assessment, generation of diagnoses, administration of therapy, and evaluation of care provided (scored as 5) and (2) to demonstrate proficiency in basic life support, advanced cardiac life support, pediatric advanced life support, and advanced trauma life support (scored as 5). The other three objectives identified were as follows: students must (1) demonstrate understanding of anatomical and physiological organs and system functions (scored as 4), (2) demonstrate understanding of pathophysiology of commonly encountered medical and surgical emergencies (scored as 3), and (3) advise and offer health education to patients and their families (scored as 3). The identified learning strategies, in decreasing order of score, were as follows: problem-based learning, practice, simulation and feedback (all scored at 5); procedural skills (scored at 4.5); lecture, self-directed learning, research, curriculum-based assessment and outcome based (all scored at 4); and seminar and assignment (both scored at 3).
Figure 4 Learning objectives and strategies.
Curriculum adoption
The details of curriculum adoption and the various other related stages, including initial proposed curriculum, synchronization, adaptation, implementation, assessment, and evaluationsCitation24–Citation27 are demonstrated in –. The various topics finally selected, objectives of studies 1 and 2 are also presented in the proposed initial and the final curriculum for the EMS program. The modifications made to the Flinders University curriculum are outlined as follows.
Table 2 Semesters by block design
Table 3 Curriculum modifications
Table 4 Adopting stage
Abbreviations: EMT, emergency medical technician; KSAU-HS, King Saud bin Abdulaziz University for Health Sciences; Sem, semester.
Table 5 Initial proposed curriculum
Table 6 Synchronization
In the first semester, Paramedic Practice 1 and communications skills cover the basics of primary and secondary surveys of resuscitation, patient examination and history taking, making judgements of life threats, communicating in the health care setting, and providing medical handover and documentation. These foundation skills tend to be delivered early. Amalgamating Paramedic Practice 1 and communications has a logical synergy, as communication skills are requisite to effective clinical skills. Paramedic Practice 3, with its medical emergency theme, should be the next block. It contains some important concepts of physiology, which will be useful to the subsequent Paramedic Practice 2. Paramedic Practice 2 falls comfortably at the end of this semester, with a focus on trauma management.
The second semester includes the pathophysiology of the CVS. It is logical to run this topic in the second semester, as advanced concepts of managing shock, acute myocardial infarction, and heart failure are covered. Skills in intravenous cannulation, fluid resuscitation, and electrocardiogram interpretation can be applied in subsequent pathophysiology topics. Because of close synergies between the CVS and RS, pathophysiology of the RS should be presented next. Applied pharmacology could then be taken. This topic does have some reliance on knowledge from the previous pathophysiology topics and should provide an enhanced understanding of the pathophysiology from a clinical pharmacological perspective.
The third semester includes pathophysiology of the nervous system (NS) – a demanding topic with a wide range of material covered. Mental health and mental illness is the next obvious topic, which has some important linkage with the pathophysiology of the NS. It was scheduled after pathophysiology of the NS, followed by pathophysiology of other body systems. The third semester has a focus on a variety of body systems and also introduces more advanced concepts of physical examination and clinical assessment. This topic provides a good platform to move into Applied Paramedic Practice, which lies in the fourth semester.
The fourth semester includes health research, a full and demanding topic with a practical focus on research methodologies. In order to perform well in this topic, students should be well acquainted with academic life; hence the topic is scheduled in the final semester. Professional studies prepare students with attitudes, knowledge, and responsibilities for moving into the profession and hence it is appropriate in the final semester. Applied Paramedic Practice takes the students on a journey through application of all the previous learning and provides the student with opportunities to develop different competencies. It prepares them for clinical work and hence should be the final topic taken ( and ).
Modifications
The main modifications in the curriculum included the following items; learning objectives, weekly specific objectives, aligned assessment, weekly problems, learning topics, mode of teaching in terms of lectures, PBL, practical fields, simulation, self-directed learning, basic and clinical sciences, patient and paramedics and community and paramedics, and, finally, personal and professional themes.
Discussion
Curriculum development and evaluation is important because of the huge impact the curriculum has on student learning and on the quality of the health services that students will ultimately deliver in the field. Content that is targeted and well sequenced ensures that students receive integrated, coherent learning experiences that contribute towards their personal, academic, and professional learning and development. The design and development of curriculums for degree courses and major and minor sequences of such courses focus on how the educational experience contributes to students’ development of the graduate qualities. These qualities provide a key reference point for the curriculum development process. They must be related to the conceptual frameworks, language, and practices of the student’s field of study through quality learning experiences. This is the strength of the current adoption of the Flinders curriculum for EMS.
Key elements and relationships in curriculums include, at the heart of the curriculum, faculty staff and students. The relationships between them are shaped by the educational aims of courses, curriculum management principles, implementation steps, sequences and topics, intended learning outcomes for students, feedback materials from students, assessment, content, learning interactions, and the connections among these elements.Citation28–Citation30 Similarly, the final adopted curriculum reflects all of these elements: the input of faculty staff and students into the overall frame of the EMS curriculum means their chosen contextual emergency medical problems, prioritized medical problems of the CVS and the RS, and basic sciences and practical field exercises are included, as well as several competencies and teaching strategies chosen on a consensus basis in various workshops and related studies guided by highly experienced faculty staff.
Blocks and their timelines were organized in such a way that knowledge of preceding blocks was essential in order for students to move to the next block and its complete understanding. The unproblematic transition and diversification, two qualities of curriculum design and development, need to be shown to students during the learning processes.Citation16 Students’ transition to university should be an easy and lively experience that would depend on curriculum components facilitating that process and dynamic step. For this purpose attitudes, aptitudes, and cultural qualities of students should be considered as part of curriculum development, helping in learning, understanding, and encouraging positive interactions during implementation of courses.Citation16,Citation31 The adopted EMS curriculum is modeled on the work-integrated learning also used in nursing educationCitation32 and as supported by the UK organization JISC; this work-integrated learning encourages digital technology in designing curriculums.Citation33 Intended learning outcomes frame and shape the detail and alignment of assessment learning interactions and content, Citation34 as also exercised in developing the EMS curriculum. Intended learning outcomes describe the characteristics that a student should be able to show on successful completion of a course. Assessment gauges the extent of students’ achievement of the intended outcomes; learning interactions and content should help to build towards students’ achievement of those outcomes. In related development, novel curriculums supported by computerized human patient simulators are implemented for improving the performance of the medical emergency team.Citation35 Digital technology is globally revolutionizing the designing of medical education curriculums.Citation34
Conclusion
A step-by-step curriculum design ensures the multilayer alignment of the curriculum. The layers include priority health problems, competencies, themes and objectives, block design and learning methods, implementation, diversification and transition, student assessment and feedback, and program evaluation. There is a need to “localize/adopt” curriculums to specific regions (taking into account health priority areas and cultural norms and practices) and not just to implement existing curriculums from other universities.
Acknowledgments
The author would like to thank Prof Mohi Eldin M Magzoub and Dr KhalidAl-Harbi for their advice and constant support during this project. The author also acknowledges the constant support given by Tim Pointon and his team at Flinders University during adaptation of the curriculum.
Disclosure
The author reports no conflicts of interest in this work.
References
- National Guard Health AffairsKing Abdulaziz Medical City: Riyadh [updated 2011 May 16] Available from: http://www.ngha.med.sa/ENGLISH/MEDICALCITIES/AlRiyadh/Pages/default.aspxAccessed November 2, 2011
- Ministry of HealthHealth Statistical Yearly BookRiyadhDepartment of Statistics, Ministry of Health2009
- SimoyanOMTownsendJMTarafderMRDeJosephDStarkRJWhiteMVPublic health and medical education: a natural alliance for a new regional medical schoolAm J Prev Med2011414 Suppl 3S220S22721961668
- ChengCIntroducing student-centred teaching strategies to improve teaching and learning in Theory of Machines and MechanismChina Papers2003 Available from: http://sydney.edu.au/science/uniserve_science/pubs/china/vol2/charlescheng.pdfAccessed September 15, 2011
- ArabiYAl-ShimemeriAImproving resource utilization in the intensive care units: a challenge for Saudi hospitalsSaudi Med J200324213113712682674
- WaldHSReisSPBeyond the margins: reflective writing and development of reflective capacity in medical educationJ Gen Intern Med201025774674920407840
- SpinelloEFFischbachRUsing a web-based simulation as a problem-based learning experience: perceived and actual performance of undergraduate public health studentsPublic Health Rep2008123Suppl 2788418770921
- CroccoTJMorenoRJauchECTeaching ACLS stroke objectives to prehospital providers: a case-based approachPrehosp Emerg Care20037222923412710784
- MacLeodASix ways problem-based learning cases can sabotage patient-centered medical educationAcad Med201186781882521617504
- HarperACA proposal to incorporate a public health perspective into clinical teachingClin Teach20118211411721585672
- OcekZACicekliogˇluMGursoySTPublic health education in Ege University Medical Faculty: developing a community-oriented modelMed Teach2008309–10e180e18819117215
- BuczackiSShalhoubJGeorgePMVearncombeLMByrnePDAlazawiWBenefits of knowledge-based interprofessional communication skills training in medical undergraduate educationJRSM Short Rep2011286721912733
- Orlandohealth.comOrlando (FL)Orlando Health2012 Available from: http://orlandohealth.comAccessed Novermber 13, 2011
- ChouCTsaiCCDeveloping web-based curricula: issues and challengesJCS2002346623636 Available from: http://faculty.ed.uiuc.edu/westbury/jcs/Vol34/CHOU.HTMAccessed November 15, 2011
- WaddoupsGLWentworthNEarleRPrinciples of technology integration and curriculum development: a faculty design team approachComputers in the Schools200421121523 Available from: http://essentialconditionswiki.pbworks.com/f/CurrDesignTeam.pdfAccessed November 15, 2011
- Flinders UniversityAdelaide, AustraliaFlinders University Available from: http://www.flinders.edu.au/courses/rules/undergrad/bpara.cfm#programofstudyAccessed on February 21, 2012
- AzerSAIntroducing a problem-based learning program: 12 tips for successMed Teach2011331080881321942480
- SturmbergJHow to teach holistic care: meeting the challenge of complexity in clinical practiceEduc Health (Abingdon)200518223624516009617
- MookherjeeSChouCLBedside teaching of clinical reasoning and evidence-based physical examinationMed Educ201145551921486342
- RadomskiNRussellJIntegrated case learning: teaching clinical reasoningAdv Health Sci Educ Theory Pract201015225126419760511
- PelacciaTTardifJTribyECharlinBAnanalysis of clinical reasoning through a recent and comprehensive approach: the dual-process theoryMed Educ Online201116
- HumbertAJBesingerBMiechEJAssessing clinical reasoning skills in scenarios of uncertainty: convergent validity for a script concordance test in an emergency medicine clerkship and residencyAcad Emerg Med201118662763421676061
- University of Illinois ExtensionLocal government education Available from: http://www.communitydevelopment.uiuc.eduAccessed November 10, 2011
- MacDonaldPJChongJPChongtrakulPSetting educational priorities for learning the concepts of population healthMed Educ19892354294392796798
- NicolDJMacfarlane-DickDFormative assessment and self-regulated learning: a model and seven principles of good feedback practiceStud High Educ2006312199218
- SadlerDRFormative assessment: revisiting the territoryAssess Educ1998517784
- WalkerMAn investigation into written comments on assignments: do students find them usable?Assess Eval High Edu20093416778
- WeaverMRDo students value feedback? Student perceptions of tutors’ written responsesAssess Eval High Edu2006313379394
- BurkeDStrategies for using feedback students bring to higher educationAssess Eval High Edu20093414150
- GloverCBrownEWritten feedback for students: too much, too detailed or too incomprehensible to be effective?BEE-j200673 Available from: http://www.bioscience.heacademy.ac.uk/journal/vol7/beej-7-3.pdfAccessed November 9, 2011
- KiftSMThe next, great first year challenge: sustaining, coordinating and embedding coherent institution-wide approaches to enact the FYE as “everybody’s business” Available from: http://www.fyhe.qut.edu.au/past_papers/papers08/FYHE2008/content/pdfs/Keynote%20-%20Kift.pdfAccessed November 13, 2011
- McAllisterMMcKinnonJThe importance of teaching and learning resilience in the health disciplines: a critical review of the literatureNurse Educ Today200929437137919056153
- JISCManaging curriculum change: transforming curriculum design and delivery through technologyBristolHigher Education Funding Council for England2009 Available from: http://www.jisc.ac.uk/media/documents/publications/managingcurriculumchange.pdfAccessed November 18, 2011
- BiggsJTeaching for Quality Learning at University: What the Student DoesBuckinghamSociety for Research into Higher Education and Open University Press2003
- DeVitaMASchaeferJLutzJWangHDongilliTImproving medical emergency team (MET) performance using a novel curriculum and a computerized human patient simulatorQual Saf Health Care200514532633116195564