Abstract
Background
Junior doctors are at high risk of involvement in medication errors. Educational interventions to enhance human factors and specifically nontechnical skills in health care are increasingly reported, but there is no work in the context of prescribing improvement to guide such education. We set out to determine the elements that influence prescribing from a human factors perspective by recent medical graduates and use this to guide education in this area.
Methods
A total of 206 recent medical graduates of the North Western Foundation School were asked to describe their views on safety practices and behaviors. Free text data regarding prescribing behaviors were collected 1, 2, and 4 months after starting their posts. A 94.1% response rate was achieved. Qualitative analysis of data was completed using the constant comparison method. Five initial categories were developed, and the researchers subsequently developed thematic indices according to their understanding of the emerging content of the data. Further data were collected through group interviews 8–9 months into the placement to ensure thematic saturation.
Results
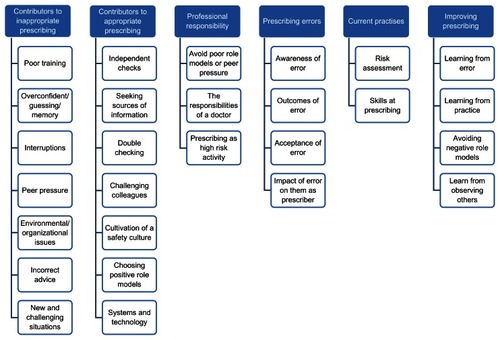
Six themes were established at the axial coding level, ie, contributors to inappropriate prescribing, contributors to appropriate prescribing, professional responsibility, prescribing error, current practices, and methods for improvement of prescribing. Utilizing appropriate theoretical elements, we describe how recent medical graduates employ situational and error awareness to guide risk assessment.
Conclusion
We have modeled the human factors of prescribing behavior by recent medical graduates. As these factors are related to a number of recognized elements of nontechnical skills training within health care, educators should consider design elements from such existing interventions to support prescribing improvement programs. Future research should seek to assess the effectiveness of prescribing focused nontechnical skills training.
Introduction
Prescribing errors are amongst the commonest of adverse events in health care,Citation1–Citation3 with junior doctors often noted to be at high risk of making such errors.Citation4–Citation7 A large UK study suggests that recent graduate error rates are comparable with those made by other prescribers,Citation5 but found that they are responsible for 75% of all inpatient prescriptions, hence increasing the overall incidence of errors amongst this cohort. Recent graduates lack contextual prescribing knowledgeCitation5 and have expressed dissatisfaction with their training,Citation7 suggesting that poor knowledge could be a factor. Improved education has been a mainstay of techniques to combat medication errors. Whilst there has been some published work investigating educational tools to improve prescribing knowledge and skills, the overall evidence base guiding interventional design is limited,Citation8 with minimal work demonstrating the effectiveness of such interventions in reducing errors affecting patients.
It is recognized that prescribing errors are not solely caused by deficits in knowledge or clinical skills, but are often multifactorial with several active failures and error-provoking conditions acting together.Citation9 In 2000, the UK Department of Health published a report outlining strategies to reduce risk from preventable errors in health care caused by human factors.Citation10 Guidance on how to achieve this goal was mostly focused on system-based improvement strategies, which has led to changes, such as electronic prescribing, computerized order entry systems, and an enhanced role of clinical pharmacy services.Citation11 However, errors still occur with alarming frequency.Citation12
Extensive work in high-stakes industries as early as the 1970s demonstrated that reducing error is not just about the right technical skills or systems-based human factor avoidance techniques, but addressing the nontechnical (cognitive and interpersonal) skills of staff that may also contribute to error.Citation13 There have been successful attempts to design education to improve nontechnical skills within other high-risk sectorsCitation14 and there is a small but growing evidence base to direct nontechnical skills education to enhance safety within health care.Citation15 Despite the complexities of introducing such relatively novel forms of education and the clear potential for applications to reduce medication errors, there is no published work investigating their design or use. Such forms of education would not replace other methods of reducing medication error, but support improvement as part of a package of measures, which may include knowledge-based education sessions and organizational system based error reduction strategies.
These are a number of published works that guide understanding of how technical and nontechnical factors may impact prescribing. Previously, a perceived “blame culture” surrounding prescribing has been reported, which may actually promote nontechnical errors.Citation16 Denial of personal roles and responsibilities as a barrier to safe prescribing has also been found.Citation17 In the context of other patient safety issues, increasing general error awareness to enhance practice has been proposed,Citation18,Citation19 and this has been used in prescribing improvement with some success.Citation20 Finally, a computer-based prescribing error model of writing prescriptions has previously been designedCitation21 based on control theory, a psychological theory of human performance which explains skilled behaviors, giving insight into how prescribing decisions are made.
All these elements form a conceptual framework that can allow us to understand the relationship between people and systems of work, known as the human factors perspective,Citation22 within the context of prescribing education. Whilst nontechnical skills and systems factors in surgery have been carefully studied,Citation23 there is a lack of clarity as to how these different elements interact to affect prescribing. Human factors models can assist in achieving that analytical balance between person and system. We set out to investigate the internal and external factors which impact on recent graduate prescribing, understand their responses to these factors, and by considering the conceptual elements discussed, use this to model safe prescribing behavior from a human factors and nontechnical skills perspective to support educational design in this area.
Materials and methods
Data collection
Participants were newly qualified doctors who had volunteered for a randomized controlled trial of an e-learning intervention to improve prescribing, with full methodological details previously published.Citation24 This research had ethical and research and development approval from the University of Dundee. This study was carried out prospectively, in parallel and independently to the randomized controlled trial to answer its distinct research question.
All doctors within the Foundation school were invited to take part, with exclusions including those who had previously worked in prescribing roles, those who had limitations on their prescribing, or those who had come from a background in the pharmaceutical industry. The study began one month into Foundation training, with 161 in Foundation year 1 (FY1) and 45 in Foundation year 2 (FY2). The participants were randomized to receive a knowledge-based e-learning intervention or no intervention. Participants completed prescribing assessment, attitude, and confidence questionnaires online pre-intervention and 4 and 12 weeks post-intervention as part of the trial. In addition, at each of these data collection points, participants were also asked to report details of their views on prescribing safety, practices, and behaviors at that time. This request was as a free text response, which was also returned online. Reminders were sent to nonresponders at 1 and 2 weeks, respectively.
For triangulation and confirmation of saturation of these data, at the conclusion, participants from both study groups were invited to attend semistructured interviews. A total of 20 participants responded, which consisted of a representative mix of participant demographics. These interviews were completed by two of the authors after the last assessment and again focused on prescribing safety. A thematic index was developed to code the data. Five initial categories were developed, based on the conceptual frameworks already discussed before the study began () and prior to analysis of the free text data. A total of five questions were devised for the interview schedule, based on each of the areas within this framework. Eleven participants were randomly selected for interview before it was deemed that saturation had been achieved, with no new themes emerging.
Table 1 Initial categories for data coding, based on the proposed conceptual framework
Data analysis
Whilst our initial thematic index () formed a starting point for analysis, we avoided making a priori hypotheses and conclusions, in keeping with a grounded theory approach.Citation25 Free text responses were held pseudoanonymously using study IDs. Following collection and processing, the data were coded using Nvivo (QSR International Pty Ltd, Doncaster, Australia).
The initial thematic indices were developed, with the addition of emerging thematic categories according to interpretation of the content of the data. The analysis proceeded through three stages, consisting of open, axial, and selective coding, with constant comparison taking place throughout each phase.Citation26 Each stage provided categories that could be used to explore the themes of the data. After the baseline data were analyzed, the post-intervention data for the control and intervention groups were initially analyzed separately. The group interviews were completed and transcribed externally with pseudonyms for anonymity and these data were also coded into the thematic framework to ensure theoretical saturation had been reached. Delineation between human and system was facilitated using the SEIPS (Systems Engineering Initiative for Patient Safety) model.Citation22
Results
A total of 205 participants were recruited, with 106 participants randomized to the control group and 99 to the intervention group, with demographics such as gender, age, and previous degrees equally distributed between groups.Citation24 A total of 388 of a possible 412 potential text responses were received (94.1%). shows the open and axial themes. In the open coding stage, 27 categories were developed from the initial thematic indices. The next stage of the analysis established six comprehensive themes, ie, contributors to inappropriate prescribing, contributors to appropriate prescribing, professional responsibility, prescribing error, improving prescribing, and current practices. Analysis of the two study groups post intervention revealed no divergence in the data, so the data sets will be discussed together.
The first two themes were the focus of many responses, essentially mirroring each other, with the participants suggesting solutions to each of the problems they identified. Seeking information sources was widely cited, with 244 of 1242 items coded into this category. The use of the British national formulary, pocket prescribing books, local guidelines, and national policies were all mentioned. Some cited positive role models behavior, while others cited inexperience or concerns with the possibility of error. There was an increase in the reported use of prescribing resources over time (). This does not appear to be influenced by whether participants had received the extra knowledge and skills training offered as part of the trial, but rather seemed to be a direct response by the recent graduates to their experiences:
Table 2 Use of external sources of prescribing information, number of open coded responses from free text data at baseline, and final data collection point
“I think that I am increasingly cautious with my prescriptions. I double check everything but the more I prescribe, the more I am aware of complications that may occur.”
gives details of responses for each of the categories within these first two themes reported in line with the SIEPS model for understanding the structures, processes, and outcomes in health care from a patient safety perspective.Citation22
Table 3 Open coded responses and excerpts for two axial coding themes: contributions to inadequate and adequate prescribing, organized in line with the SIEPS modelCitation22
The next theme, professional responsibilities, describes how recent graduates viewed their ability to prescribe not as a right or duty, but as a task they complete as a professional, accepting the associated risks and hence responsibilities. In the initial baseline data set, the weight of this responsibility led to apprehension:
“It is you signing it, so ultimately you are responsible for that prescription if anything goes wrong.”
“I feel I am scared and am conscious that I am newly qualified so don’t want to harm any patients by my mistakes with my prescribing.”
In the subsequent data sets, this theme surfaced in how the prescribers responded to those around them. In particular, there were 19 coded items which all occurred at the final data collection point that related to peer pressure from medical or nursing colleagues to prescribe:
“I might not do what the nurses want me to do, ie, prescribe that particular drug and they’ll get quite angry with me.”
“When you want to question, they’d just say ‘what do you mean? Just get on with it.”
In this way, professionalism in the context of prescribing was linked to the next theme, prescribing errors. The recent graduates are clearly aware of the many factors leading to error and how to start negating these, as discussed in the first two thematic areas. This awareness of error was a key theme, but many participants commented on their own experience of error, how it affected them, and frequently discussed the potential outcomes of error:
“The most serious consequences can happen, they can be fatal.”
“You ultimately are legally responsible. We can also get into a lot of trouble with the GMC!”
While it was expected that fear of blame would be a barrier to speaking up, in fact the reverse was true:
“I’ve seen quite a lot of drug errors and people have said ‘Oh you know there was an F 1 who did this’ but no one’s ever said they were stupid, they’ve just said this is an error.”
The next theme was current practices. This comprised two aspects: firstly, that generally trainees felt prepared to prescribe, but were cautious in doing so, and, secondly, risk assessment. This related to a number of the categories, discussing how error changed behavior and methods to improve prescribing, often to negate the risks they identified. Some specific examples included:
“To prescribe safely, I must look things up, which prohibits me prescribing quickly, for example during a ward round, so maybe there is a risk of things not being prescribed as I have to list things to go back and prescribe later.”
“I often choose a drug I am familiar with rather than a new one, to reduce risk.”
“I try to treat prescribing like a procedure, with preparation phase involving checking the correct patient, indication and any allergies. I always use a calculator to do even the simplest drug calculations. I am very aware that prescribing is one of the riskiest things doctors do.”
Risk assessment seemed to determine when and to what extent they would prescribe safely. Occasionally, the outcome of this risk assessment would lead them to prescribe in a suboptimal way:
“When asked to prescribe something by a senior without checking, it would depend on the person and depend on the drug, if you knew it was a sort of dangerous drug, I’d double check it.”
“I think junior doctors can easily panic and assume it’s more important to get something done fast so they can get on with all their other jobs than it is to do something safely.”
“If I don’t know a drug I look it up. The exception to this is if I am rewriting a drug card and I need to be quick. If I know it has been checked by a pharmacist I don’t look it up if I haven’t got time.”
The final theme was improving prescribing. Error is clearly identified as a source of learning. This occurs on a personal level, with errors constantly shaping behavior, but also in peer groups, with several participants mentioning root course analysis as a method employed within the workplace:
“In our hospital we learn in teaching, somebody will bring up something that’s happened, they’ve mismanaged the patient, and its lessons learned at the end.”
“With a facilitator from ITU and somebody volunteers to present a case and then the facilitator breaks everyone up into groups and each person gets a different thing to look at, like the human errors … and you sit and discuss them at the end with the facilitators.”
The importance of learning from experience was emphasized:
“Prescribing is best learnt actually doing it and having to look up doses yourself. Also helps if you have to prescribe the same drug for lots of patients – helps drum it in.”
“I take every opportunity to rewrite and check drug charts in order to increase practice prescribing.”
This experience often involved examples of poor practice and actively avoiding these negative role models.
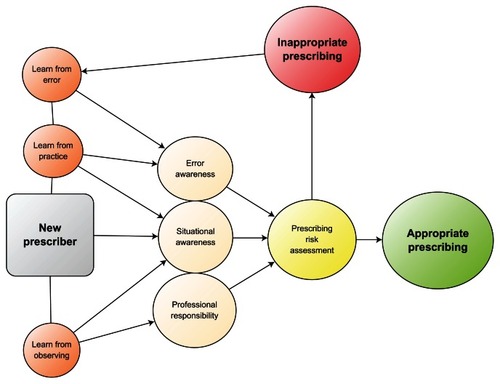
In the final selective coding level of analysis, these themes were bound by the authors in a nontechnical skills model of recent graduate prescribing behavior (), which was influenced by our conceptual framework, but grounded in the data analyzed. This model initially denotes the prescriber receiving input to improve prescribing from the sources identified (learning from error, practice, and observation). These then go on to influence the prescriber in three main areas. The first is awareness of error in prescribing, both as presented in teaching and experienced in their own practice. The second is situational awareness, around the contributors to error they encounter and how these may be tackled. The final area is professional responsibility to prescribe. This is also heavily influenced by their role as a trained professional, but in particular by observing poor role models, peer pressure to prescribe irresponsibly, and, finally, from an increasing awareness of risk. These areas are represented as tightly bound, because one clearly influences the other, with heightened professional responsibility improving situational awareness and improved knowledge of error influencing professional responsibility. Finally, these elements all encourage risk assessment which should facilitate good prescribing.
Discussion
Within these data, there were clear behavior shifts over time, with increasing referencing for information, double-checking, and use of technology to support prescribing. Participants explained that whilst they felt competent to prescribe on graduation, they began to feel that other practices are increasingly needed to support safer prescribing. It seems that over time, the participants learned not just to practice the clinical skills they had acquired, but to understand that their performance and safe prescribing was enhanced by their nontechnical (cognitive and social) skills situated within the systems context in which they were working. Sometimes there was a gap between those systems and skills which lead to risks; sometimes it was those systems of work or the good application of teamwork and cognitive skills that led to improved care and safety. This is clearly in line with a human factors view that would predict how practitioners learn to work safely within a complex sociotechnical system.Citation27
Previous reports have suggested an organizational culture of blame, prescriber’s unwillingness to accept responsibility for error,Citation17 and a culture of lack of safety amongst recent graduates.Citation5 However, we found little concern with blame surrounding prescribing errors and indeed a culture of acceptance at an institutional level, again aligning with a human factors perspective of such activities. This reinforces the value of exploring activity at the sharp end of care, before generating solutions “top down” which might otherwise be based on limited or erroneous assumptions.
Our participants clearly exhibited heightened awareness of error, from their own experience and observations. They often reflected on negative behaviors, how they may lead to error and on changes to their own practice. There was substantial consideration of contributors to poor prescribing, for which clear solutions to each were suggested. Whilst positive prescribing role models were seen to enhance practice, the trainees did not seem to be adversely effected by negative behaviors. Rather, in an extension of the internal process already described, they used these experiences to shape their own practice further. From a number of comments from the participants, it seems that negative examples of prescribing enhanced their sense of professional responsibility and improved their prescribing risk assessments.
The model synthesized () shows how recent medical graduates use these different elements to inform their personal assessment of prescribing risk. Whilst this usually produces appropriate prescribing, if errors are made or observed, behavior-determining processes are enhanced, leading to a more informed and inherently safer risk assessment, following the principles identified in our conceptual frameworks. Thus, a substantial part of the work of new practitioners had been to adapt behavior to create safety, and there may be an opportunity to assist this process.
Our participants clearly learn the tenets of safe prescribing through an explorative and iterative process of behavioral modification. Experience and, in particular, experience of poor prescribing, drives this process. Interestingly, the perspective was inwardly directed, with no mention of a desire to effect change in colleagues, their environment, or systems. Thus, the new practitioners learned to adapt to the environment in which they found themselves without substantial sharing of their learning or a uniformly well structured theoretical understanding. Certainly, many behaviors seemed positive, but there should remain a concern that the outward “systems” perspective was becoming lost, and that more generally, the lessons that were being learned were not shared or universal. Thus, each was developing his or her own way of working. Clearly, there might be value in structured education to ensure uniform safety and nontechnical skill acquisition. Further, because experience of actual error is key to this process, education that can allow such nontechnical skills to be acquired without error occurring is clearly of benefit to patients.
Therefore, we would propose that educators wishing to train in any aspect of prescribing should pay attention to the key principles of this model. Several areas of this model are already parts of educational techniques to enhance patient safety.Citation15 Although crew resource management may form a good basis for development, most current publications describing crew resource management in health care focus on “whether” it is effective, and although nontechnical skills training has been carefully defined in some areas,Citation23 how it should be delivered and the mechanisms of learning have been poorly investigated.Citation15 This lack of theoretical underpinning or evidence-based construction offers little of use to educators. Moreover, the assumption that this learning is not taking place is erroneous; clearly it is, and is impacting behavior in a significant way. This study may be the first to demonstrate this, and we need to take care not to fall into the trap of offering prescribing training that does not fit easily with and complement this workplace learning. Such superimposition of “sharp end” knowledge and skills from other industries that may not consider the context of learning in health care has perhaps been the biggest disincentive for crew resource management and nontechnical skills training, and is reflected in high costs, mixed benefits, and heterogeneity of courses that have been described.Citation15
Our model offers a simple structure that will aid in the better translation of safety skills training into a prescribing environment and could be used to guide the design of interventions for improvement and ultimately support better outcomes for patients. Whilst this may lead to stand alone interventions, these findings can be used to enhance all prescribing education by carefully considering the relationship between humans and systems.
This study has several limitations. The method of data analysis we have used is clearly open to interpretation bias on the part of the researchers, with our own preconceived ideas shaping the analysis. Every effort has been made to minimize such bias, in line with accepted methodology.Citation24 Although it covers a wide range of hospitals, specialties, genders, and ages, this was a volunteer sample, with the possibility that this may be a source of bias. In particular, it is possible that the participants may have been involved in more errors and be more disposed to improvement of prescribing at enrolment. Social acceptability bias is also possible, with respondents censoring opinions they felt would be unacceptable. Given these limitations, further study is needed to confirm the features of our proposed model and, in particular, its utility for educators planning nontechnical educational interventions for prescribing skills. Further, given that there is minimal evidence to suggest that nontechnical skills training in health care can change behavior or outcomes for patients, attention should be paid to these areas when investigating educational packages.
Conclusion
We have studied and modeled prescribing behaviors of recent medical graduates from a nontechnical skills perspective to demonstrate how several factors influence a constant process of prescribing risk assessment. Given that these factors are related to a number of recognized elements of nontechnical skills training within health care, educators should consider design elements from these interventions to support prescribing improvement programs, although future work is needed to assess the application of our findings in other settings and to assess the role of prescribing focused nontechnical skills training in general.
Acknowledgment
The author is grateful to the North Western Deanery for transcription of the interviews.
Disclosure
The authors report no conflicts of interest in this work.
References
- GhalebMABarberNFranklinBDYeungVWKhakiZFWongICSystematic review of medication errors in pediatric patientsAnn Pharmacother2006401766177616985096
- KohnLTCorriganJMDonaldsonMSTo Err is Human: Building a Safer Health SystemWashington, DCInstitute of Medicine, National Academies Press1999
- BerdotSSabatierBGillaizeauFCarubaTPrognonPDurieuxPEvaluation of drug administration errors in a teaching hospitalBMC Health Serv Res201212;1260
- DeanBSchachterMVincentCBarberNCauses of prescribing errors in hospital inpatients: a prospective studyLancet20023591373137811978334
- DornanTAshcroftDHeathfieldHAn in-depth investigation into the causes of prescribing errors by foundation trainees in relation to their medical education: EQUIP study2009Final report to the General Medical Council, University of Manchester: School of Pharmacy and Pharmaceutical medicine Available from: http://psnet.ahrq.gov/resource.aspx?resourceID=17269Accessed December 13, 2012.
- RossSBondCRothnieHThomasSMacleodMJWhat is the scale of prescribing errors committed by junior doctors? A systematic reviewBr J Clin Pharmacol20096762964019094162
- HeatonAWebbDJMaxwellSRJUndergraduate preparation for prescribing: the views of 2413 UK medical students and recent graduatesBr J Clin Pharmacol20086612813418492128
- RossSLokeYKDo educational interventions improve prescribing by medical students and junior doctors? A systematic reviewBr J Clin Pharmacol20096766267019594535
- TullyMAshcroftDDornanTLewisPTaylorDWassVThe causes of and factors associated with prescribing errors in hospital inpatients: a systematic reviewDrug Saf20093281983619722726
- Department of HealthOrganization with a MemoryLondon, UKThe Stationery Office2000
- WongICKWongIYICranswickNEMinimising medication errors in childrenArch Dis Child20099416116418829622
- National Patient Safety AgencyQuarterly Data Summaries Available from: http://www.nrls.npsa.nhs.uk/resources/collections/quarterly-data-summaries/Accessed December 13, 2012.
- LernerSMagraneDFriedmanETeaching teamwork in medical educationMt Sinai J Med20097631832919642146
- WeinerELNagelDHuman Factors in AviationNew York, NYAcademic Press1988
- GordonMDarbyshireDBakerPNon-technical skills training to enhance patient safety: a systematic reviewMed Educ2012461042105423078681
- TobaiqyMMcLayJRossSFoundation year 1 doctors and clinical pharmacology and therapeutics teaching. A iretrospective view in light of experienceBr J Clin Pharmacol20076436337217506779
- CoombesIDMitchellCAStowasserDASafe medication practice: attitudes of medical students about to begin their intern yearMed Educ20084242743118338996
- AroraVMJohnsonJKMeltzerDOHumphreyHJA theoretical framework and competency-based approach to improving handoffsQual Saf Health Care200817111418245213
- GordonMFindleyREducational interventions to improve handover of care: a systematic reviewMed Educ2011451081108921933243
- GordonMBose-HaiderBA novel system of prescribing feedback to reduce errors: a pilot studyInt J Risk Saf Med20122420721423135335
- MarkenRSA model-based approach to prioritizing medical safety practicesHenriksenKBattlesJBMarksESLewinDIAdvances in Patient Safety: From Research to Implementation (Volume 2: Concepts and Methodology)Rockville, MDUS Agency for Healthcare Research and Quality2005
- CarayonPSchoofs HundtAKarshBTWork system design for patient safety: the SEIPS modelQual Saf Health Care200615 Suppl 1i50i5817142610
- FlinRYoungsonGYuleSHow do surgeons make intraoperative decisions?Qual Saf Health Care20071623523917545353
- GordonMChandratilakeMBakerPImproved junior paediatric prescribing skills after a short e-learning intervention: a randomised controlled trialArch Dis Child2011961191119422080459
- PattonMQQualitative Research and Evaluation Methods3rd edThousand Oaks, CASage Publications2002
- StraussALCorbinJMBasics of Qualitative Research: Procedures and Techniques for Generating Grounded Theory2nd edThousand Oaks, CASage Publications1998
- DekkerSFailure to adapt or adaptations that fail: contrasting models on procedures and safetyAppl Ergon20033423323812737923