Abstract
Aim
To evaluate the impact of COVID-19 on the clinical training of paediatric trainees during the pandemic at a regional hospital in Victoria, Australia.
Methods
In response to a survey and feedback from paediatric trainees, a retrospective analysis was conducted to investigate the effects of the COVID-19 pandemic on medical staff attendance at onsite training in the Department of Paediatrics at a regional hospital in Victoria. The study spanned from January 2019 to December 2021. Variables collected included the number of participants attending the paediatric clinical and education meetings. A comparative analysis of attendance during the pre-COVID-19 year (2019) and the COVID-19 years (2020–2021) was conducted.
Results
The total number of meetings held was 292 in 2019, which declined to 184 in 2020 and further declined to 171 in 2021, with a minimal increase in existing virtual meetings. The total attendance in paediatric clinical meetings dropped from 2190 attendees in 2019 to 1332 in 2020, and further declined to 1230 in 2021. Paediatric registrar attendance was 477 in 2019, which decreased by 29.35% to 330 in 2020 and further decreased by 38.57% to 293 in 2021. Paediatric hospital medical officer attendance showed the worst trend among paediatric trainees, with 445 attending clinical meetings in 2019 and decreasing by 50.78% to 219 in 2020 and a 52.58% decrease to 211 in 2021.
Conclusion
The sudden outbreak of COVID-19 led to significant disruptions in medical education globally. This study showed a noticeable reduction in paediatric departmental clinical meetings and teaching sessions during the pandemic, as well as a significant decline in attendance by paediatric trainees and medical students. These findings confirm the experiences of paediatric trainees, who reported losing valuable teaching opportunities due to the pandemic and a demand for attention.
Introduction
Coronavirus SARS-CoV2 disease (COVID-19) was formally declared a pandemic by the World Health Organisation (WHO) on the 11th of March 2020.Citation1 Since then, the world has experienced multiple variants, each with its level of virulence.Citation2 The effects on the health care system have been astronomical; however, the impact on medical students and junior medical staff on their clinical training has likely been under-estimated.Citation3 Emergency lockdown strategies disrupted junior medical staff training in academic and clinical settings.Citation4
Preparing the future healthcare workforce is a key priority for governments.Citation5 Doctors, nurses and allied health professionals have trained for decades by observing and learning from experienced clinical practitioners through work-integrated learning.Citation6 Osler introduced formalised education programs, with training in a clinical environment in the late 19th century.Citation7 This resulted in a progressive shift of the responsibility of training medical students and junior doctors from the academic facilities to that of the healthcare system and it has reached a point where the principal source of education is clinically based.Citation8 There is a strong link between the clinical environment on trainee education and that of learner outcomes, highlighting the crucial significance of the impact of learning environments.Citation9
The COVID-19 pandemic has significantly impacted mental health, education, and daily routines.Citation10 A significant challenge during the pandemic was balancing the education, clinical experiences, and risk considerations in the clinical environment.Citation10 This study aims to evaluate the impact of COVID-19 on the clinical training of junior medical staff during the pandemic at a regional hospital in Victoria, Australia.
The regional hospital’s paediatric department in this study comprises of five paediatric consultants, five paediatric advanced trainee registrars, and three hospital medical officers, including two paediatric basic trainees. During any given rotation, there are usually three rotating medical students who change over every six weeks. Department clinical meetings included paediatric multidisciplinary team (MDT) meetings, radiology meetings, paediatric morbidity and mortality (M&M) meetings, morning clinical handover rounds, journal clubs and teaching sessions. Meetings held virtually with other hospitals include virtual grand rounds with two tertiary children’s hospitals and teaching held with another local regional facility’s paediatric department. Meetings were open to all staff members.
Department meetings were generally held on a regular basis; with paediatric MDT meetings, radiology meetings, paediatric M&M meetings, and journal clubs held on average once a month. Morning paediatric clinical handover meetings were done in person. Meetings held weekly in the paediatric department and attended virtually included grand round teaching with the two tertiary children’s hospitals and virtual paediatric case discussion with another local regional paediatric department.
This research was carried out in response to feedback from the paediatric training consortium, with a focus on the experiences of basic paediatric trainees during their rotation at the department of paediatrics in a regional facility. An anonymous survey was conducted by the consortium among trainees who had completed a three-month paediatric rotation program between August 2021 and July 2022. Out of the seven junior doctors invited to provide feedback, six responded. The results indicated that during the COVID-19 pandemic, trainees experienced a lack of formal and informal teaching, high clinical workload, staff shortages, and an unpredictable roster.
Methods
We conducted a retrospective analysis that looked at the potential effects of the COVID-19 pandemic on attendance by medical staff to onsite training in the department of paediatrics at a regional hospital in Victoria. The study covered three-years, from January 2019 to December 2021. The Human Research Ethics Committee at Latrobe Regional Health, Victoria granted ethics approval for the study. The participants included in the study were the senior and junior medical staff of the department of paediatrics, rotating medical students, and nursing and allied health staff. The participants would have attended the medical training at the hospital between the years 2019 to 2022. Data was captured on site and no study subject identifiers were entered into the database minimising loss of confidentiality. Attendance records for various meetings were maintained within the paediatric department situated on the hospital premises and were subsequently accessed for the purpose of this study. The data retrieved from these records was captured utilizing Microsoft Excel.
Inclusion criteria included senior medical staff (paediatric consultants), junior medical staff (the hospital medical officers or residents, senior registrars [advanced trainees]), medical students, nursing staff and allied health staff. The attendance sheets after December 2021 were excluded from the study.
Variables collected between 2019 and 2021 included the number of participants attending clinical meetings and teaching sessions. A comparison was conducted between the pre-COVID-19 year (2019) and the COVID-19 years (2020–2021).
Results
In 2019, the year before the COVID-19 pandemic, the total number of meetings held was 292, which declined by 36.98% in 2020 and a further decline by 41.43% in 2021 to 171 meetings per annum. The meetings that had the highest number annually were the daily morning clinical handover meetings with 172 (58.9% of the total number of meetings per annum) in 2019, 120 (65.3%) in 2020 and 109 (63.7%) in 2021. Nearly all the clinical meetings showed a decline in numbers annually from 2019 to 2020 and 2021. Meetings that showed a minimal increase in numbers annually from 2020 to 2021 included radiology meetings from 5 (2.7%) to 7 (4.1%), GR virtual meetings with the out-of-state children’s hospital from 14 (17.6%) to 19 (11.1%), and virtual meetings held with the local regional facility from 8 (4.3%) to 21 (12.3%) ().
Table 1 Table Showing the Total Number of Meetings Held per Annum from 2019 to 2021
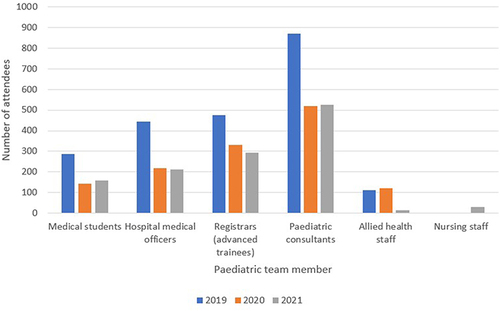
Data analysis shows total attendance dropped substantially from 2190 attendees in 2019 to 1332 in 2020, with a further decline in attendees to 1230 in 2021. Paediatric registrars and hospital medical officers had similar attendance numbers to paediatric department meetings, 477 and 445 respectively, with both groups’ attendance numbers declining from 2019 to 2021 (). Paediatric registrar attendance decreased by 29.35% to 330 in 2020 and further decreased by 38.57% to 293 in 2021. Paediatric hospital medical officer attendance decreased by more than half, decreasing by 50.78% to 219 in 2020 and a 52.58% decrease to 211 in 2021. Medical student attendance in 2019 was 286 and decreased by 50.34% to 142 in 2020 and by 44.40% to 159 in 2021. Paediatric consultants had the highest attendance among staff members with 871 attendees in 2019 and declined in 2020 and 2021 (519 [40.41% drop] in 2020 and 525 [39.72% drop] in 2021 respectively). The group overall with the lowest attendance were the allied health care practitioners (111 in 2019, 122 in 2020 and 13 in 2021) ().
Figure 1 Bar graph comparing attendance of various members of the paediatric team from 2019 to 2021.
Regarding the attendance at departmental meetings, morning clinical handover had the highest rates of attendance compared to the other sessions, with 1226 attendees in 2019, but with a drop-down to 818 in 2020 and 806 in 2021. Numbers throughout the groups declined in 2020 and 2021 during the COVID-19 pandemic. Before the COVID-19 pandemic, in 2019, the grand rounds with the children’s hospital based in a different state had the second most attendees after the daily paediatric morning clinical handover meetings (). This differed during the two years of the COVID-19 pandemic. In 2020, teaching sessions were the second most attended paediatric meeting, and in 2021, virtual meetings with another local regional facility were the second most attended. However, in both cases, the number of attendees in 2020 and 2021 decreased compared to 2019.
Table 2 Comparison of the Total Attendees per Meeting During 2019, 2020 and 2021
Discussion
This study investigated the impact of the COVID-19 pandemic on providing paediatric medical education and training at a regional facility in Victoria. The findings reveal a stark and concerning contrast in attendance at paediatric clinical and educational meetings between the pre-pandemic and COVID-19 era. It is noteworthy that the decrease in attendance was more significant among junior medical staff than senior medical staff, which corroborates the experiences of paediatric trainees who had fewer learning opportunities during the pandemic. Furthermore, there is a dearth of data specifically looking at the effects of the COVID-19 pandemic on paediatric training, and to our knowledge, this is one of the few studies examining the impacts of the COVID outbreak on paediatric training at a regional teaching hospital. Previous studies have evaluated the impact of the COVID-19 pandemic on surgical training and fellowships, radiology residency, gastroenterology residency and assessment of medical students, showing between 40% to 100% of surgical residents reported severe impact of the COVID-19 pandemic on their training.Citation11–14
Our study showed that there was a significant reduction in paediatric clinical and teaching meetings during COVID pandemic and negligible increase in virtual meetings to compensate for the loss. The attendance of junior medical staff was drastically affected with the attendance of junior most paediatric trainees reduced by over half.
With the negative effects of the COVID-19 pandemic on medical education, emergency solutions must be implemented to improve the teaching experience.Citation15 This involves blended modes of training including online lectures and face-to-face sessions for practical training tailored to junior doctor’s training requirements.Citation15 COVID-19 disrupted the traditional format and process of medical training for the vast majority of junior medical doctors worldwide.Citation16 Education and educational techniques had to accommodate the virus within the community and adjust to public health considerations in order to deliver optimal educational quality, with most facilities utilising online learning platforms instead of the traditional face-to-face teaching sessions.Citation17–20 Junior doctors are accustomed to acclimatising to different workplace settings, often in rotating roles.Citation21 The pandemic presented new challenges, including disruptions to work patterns, responsibilities, and contexts.Citation21 Interruptions in educational delivery have been reported and are well documented.Citation20 Formal examinations were postponed, clinical encounters were restricted to those classified as essential, and bedside teaching was either non-existent or defaulted to virtual learning.Citation21 Most clinical specialties reduced clinical attendance in favour of telehealth, resulting in less face-to-face time with patients, limited attendance during ward rounds, and a reduced elective surgery lists, further limiting the education and training of junior medical staff.Citation3 Various studies showed that online learning had limitations, including students not having access to online education and others reporting technical difficulties, students lacking motivation, lack of personal interaction, whilst others felt that it lacked the engaging qualities of face-to-face learning.Citation20,Citation22 However, the study revealed certain advantages of online learning, which included flexibility, availability of learning materials (audio and video), and less commuting costs.Citation20
The impact of the change in teaching and learning, on both learners and teachers, is largely unknown.Citation23 Engaging with a curriculum that transitioned to online teaching from in-person is likely to have effects on the way staff learn and how they can contextualise that learning into their clinical practice especially the influence of online education on the development of practical skills and graduate readiness to practice.Citation23 A study by Gard et alCitation21 analysed the implications for paediatric training and the workforce from pandemic disruptions showing that with limited numbers of clinicians at the bedside, junior doctors felt that they were usually the first to be excluded, resulting in lost opportunities to observe and model senior clinicians’ approach to clinical encounters.Citation21
The COVID-19 pandemic has changed the landscape of medical education by leading facilities to act innovatively using advanced digital technology.Citation22 The existing pandemic has forced departments to transform educational methods, modalities and processes whilst still keeping pace with the latest in technological advancements.Citation22 Remote learning before the COVID-19 pandemic found that students felt it was not an acceptable replacement for in-person learning. However, now various studies have revealed that interactive remote learning lectures have helped medical students and other junior trainee doctors to adjust to a new way of medical teaching during these emergent times.Citation22 A study by Dergham et alCitation24 revealed that during emergencies due to the pandemic, online teaching not only enabled continuity of medical education but was also efficient. Their study further showed a higher level of interaction.Citation24 Previous studies reported that online teaching covered practical lessons allowing interactive and constructive discussions, which are also effective in achieving learning outcomes.Citation24
Limitations
The main limitation of this retrospective study was an inability to obtain all the relevant data due to missing attendance sheets. Differences in the record keeping pre-COVID-19 and during COVID-19 pandemic were also a limitation of this study in that likely not all attendees included their names on the attendance sheets.
Conclusion
The impact of the COVID-19 pandemic on medical education, clinical training and daily routine of medical staff has been significant.Citation10,Citation25 The sudden outbreak of COVID-19 led to significant disruptions in medical education globally.Citation10 The present study highlights a significant and worrisome decline in paediatric training education during the COVID-19 pandemic. The effect of this decline is reflected in the negative learning experiences reported by trainees during the pandemic. The findings of the study underscore the challenges faced by the healthcare industry in sustaining the quality and effectiveness of paediatric training programs amid the pandemic. More studies are needed to investigate the effect on paediatric training and psychological effects on junior medical staff and their perceptions of the change to their clinical training, especially in rural settings. There is also a need to review the current teaching and learning methods to suit teaching and learning during pandemics of highly infectious diseases to allow for an effective learning experience.Citation15
Abbreviations
COVID-19, Coronavirus SARS-CoV2 disease; GR, Grand round; M&M, Morbidity and Mortality; MDT, Multidisciplinary team.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
Monash University medical students Angela Chau, Alice Song and Oliver Wang provided assistance with data collection and their help is much appreciated.
References
- World Health Organization. WHO Timeline - COVID-19; 2020. Available from: https://wwwwhoint/news-room/detail/27-04-2020-who-timeline---covid-19. Accessed May 29, 2024.
- Cordato DJ, Fatima Shad K, Soubra W, Beran RG. Health research and education during and after the COVID-19 pandemic: an Australian clinician and researcher perspective. Diagnostics. 2023;13(2):289. doi:10.3390/diagnostics13020289
- Savage N, Jain A, Ng SC. Impacts of the COVID −19 pandemic on medical students in Australia. ANZ J Surg. 2020;90(7–8):1244–1245. doi:10.1111/ans.16103
- Connolly N, Abdalla ME. Impact of COVID-19 on medical education in different income countries: a scoping review of the literature. Med Educ Online. 2022;27(1):2040192. doi:10.1080/10872981.2022.2040192
- Transforming. And Scaling Up Health Professionals’ Education and Training: What are the Key Policy Issues and Possible Responses? Geneva: World Health Organization; 2013.
- Bleakley A. Pre-registration house officers and ward-based learning: a ‘new apprenticeship’ model. Medical Education. 2002;36(1):9–15. doi:10.1046/j.1365-2923.2002.01128.x
- Custers E, Cate OT. The history of medical education in Europe and the United States, with respect to time and proficiency. Acad Med. 2018;93(3S Competency–Based, Time–Variable Education in the Health Professions):S49–s54. doi:10.1097/ACM.0000000000002079
- Kneebone R. Surgical Education: A Historical Perspective, in Advancing Surgical Education. Singapore: Stringer Nature; 2019.
- Haertel GD, Walberg HJ, Haertel EH. Socio‐psychological environments and learning: a quantitative synthesis. Br Educ Res J. 1981;7(1):27–36. doi:10.1080/0141192810070103
- Jhajj S, Kaur P, Jhajj P, et al. Impact of Covid-19 on medical students around the globe. J Community Hosp Intern Med Perspect. 2022;12(4):1–6. doi:10.55729/2000-9666.1082
- Huamanchumo-Suyon ME, Urrunaga-Pastor D, Ruiz-Perez PJ, Rodrigo-Gallardo PK, Toro-Huamanchumo CJ. Impact of the COVID-19 pandemic on general surgery residency program in Peru: a cross-sectional study. Ann Med Surg. 2020;60:130–134. doi:10.1016/j.amsu.2020.10.031
- Gupta T, Nazif TM, Vahl TP, et al. Impact of the COVID-19 pandemic on interventional cardiology fellowship training in the New York metropolitan area: a perspective from the United States epicenter. Catheterization Cardiovasc Interventions. 2021;97(2):201–205. doi:10.1002/ccd.28977
- Odedra D, Chahal BS, Patlas MN. Impact of COVID-19 on Canadian radiology residency training programs. Canad Associat Radiolog J. 2020;71(4):482–489. doi:10.1177/0846537120933215
- Marasco G, Nardone OM, Maida M, Boskoski I, Pastorelli L, Scaldaferri F. Impact of COVID-19 outbreak on clinical practice and training of young gastroenterologists: a European survey. Digestive Liver Dis. 2020;52(12):1396–1402. doi:10.1016/j.dld.2020.05.023
- Bongomin F, Olum R, Nakiyingi L, et al. Internal medicine clerkship amidst COVID-19 pandemic: a cross-sectional study of the clinical learning experience of undergraduate medical students at makerere university, Uganda. Adv Med Educ Pract. 2021;12:253–262. doi:10.2147/AMEP.S300265
- Brown A, Kassam A, Paget M, Blades K, Mercia M, Kachra R. Exploring the global impact of the COVID-19 pandemic on medical education: an international cross-sectional study of medical learners. Can Med Educ J. 2021;12(3):28–43.
- Reimers F, Schleicher A, Saaverdra J, Ourminen S. Supporting the continuation of teaching and learning during the COVID-19 pandemic annotated resources for online learning. OECD. 2020;1(1):1–38.
- Rose S. Medical student education in the time of COVID-19. JAMA. 2020;323(21):2131–2132. doi:10.1001/jama.2020.5227
- Roe A, Blikstad-Balas M, Dalland CP. The Impact of COVID-19 and homeschooling on students’ engagement with physical activity. Front Sport Active Liv. 2020;2:589227. doi:10.3389/fspor.2020.589227
- Kaifi R, Subahi A, Alqarni S, Jaddawi A, Alghamdi A, Alshamrani KM. The impact of COVID-19 on radiological science students and interns at king Saud bin Abdulaziz university for health sciences: cross-sectional study. Adv Med Educ Pract. 2023;14:563–571. doi:10.2147/AMEP.S407289
- Gard J, Cisternino A, Polley C, Gray A. Implications for paediatric training and workforce from pandemic disruptions: a view from a tertiary hospital. J Paediatr Child Health. 2022;58(12):2190–2196. doi:10.1111/jpc.16180
- Arja SB, Fatteh S, Nandennagari S, Pemma SSK, Ponnusamy K, Arja SB. Is emergency remote (online) teaching in the first two years of medical school during the COVID-19 pandemic serving the purpose? Adv Med Educ Pract. 2022;13:199–211. doi:10.2147/AMEP.S352599
- Kumar A, Sarkar M, Davis E, et al. Impact of the COVID-19 pandemic on teaching and learning in health professional education: a mixed methods study protocol. BMC Med Educ. 2021;21(1):439. doi:10.1186/s12909-021-02871-w
- Dergham P, Saudagar FNI, Jones-Nazar CC, et al. Medical students’ perceptions towards online teaching during the Covid-19 pandemic: a cross-sectional study from Saudi Arabia. Adv Med Educ Pract. 2023;14:407–419. doi:10.2147/AMEP.S396912
- Martin P, McGrail M, Fox J, Partanen R, Kondalsamy-Chennakesavan S. Impact of the COVID-19 pandemic on medical student placements in rural Queensland: a survey study. Aust J Rural Health. 2022;30(4):478–487. doi:10.1111/ajr.12862
