Abstract
Study objectives
Multiple curricula have been designed to teach medical students the basics of ultrasound; however, few focus on critical problem-solving. The objective of this study is to determine whether a theme-based ultrasound teaching session, dedicated to the use of ultrasound in the management of the hypotensive patient, can impact medical students’ ultrasound education and provide critical problem-solving exercises.
Methods
This was a cross-sectional study using an innovative approach to train 3rd year medical students during a 1-day ultrasound training session. The students received a 1-hour didactic session on basic ultrasound physics and knobology and were also provided with YouTube hyperlinks, and links to smart phone educational applications, which demonstrated a variety of bedside ultrasound techniques. In small group sessions, students learned how to evaluate patients for pathology associated with hypotension. A knowledge assessment questionnaire was administered at the end of the session and again 3 months later. Student knowledge was also assessed using different clinical scenarios with multiple-choice questions.
Results
One hundred and three 3rd year medical students participated in this study. Appropriate type of ultrasound was selected and accurate diagnosis was made in different hypotension clinical scenarios: pulmonary embolism, 81% (95% CI, 73%–89%); abdominal aortic aneurysm, 100%; and pneumothorax, 89% (95% CI, 82%–95%). The average confidence level in performing ultrasound-guided central line placement was 7/10, focused assessment with sonography for trauma was 8/10, inferior vena cava assessment was 8/10, evaluation for abdominal aortic aneurysm was 8/10, assessment for deep vein thrombus was 8/10, and cardiac ultrasound for contractility and overall function was 7/10. Student performance in the knowledge assessment portion of the questionnaire was an average of 74% (SD =11%) at the end of workshop and 74% (SD =12%) 3 months later (P=0.00).
Conclusion
At our institution, we successfully integrated ultrasound and critical problem-solving instruction, as part of a 1-day workshop for undergraduate medical education.
Introduction
Curriculum for undergraduate medical education is continuously analyzed with significant emphasis placed on the acquisition of knowledge and critical problem-solving skills. Team-based learning and case-based instruction have gained increasing popularity in recent years and have been adopted, in some format, by medical schools across the country based on the belief that these techniques will help foster the development of critical problem-solving skills.Citation1,Citation2 A study by Schmidmaier et al,Citation3 has demonstrated that conceptual knowledge alone is insufficient for the successful application of critical problem-solving skills when making clinical decisions. In fact this study discovered that clinical experiences play a larger role in clinical decision making.Citation3 Despite the merits of traditional undergraduate medical education as well as problem-based learning, research suggests that training using full-scale, high-fidelity simulation models is superior for the attainment of critical assessment and management skills.Citation4,Citation5
The benefits of sound critical problem-solving skills are most actualized when physicians face critically ill patients. Hypotensive patients, for example, frequently perplex clinicians, because the differential diagnosis of this patient population is both extensive and complex. Furthermore, the physical exam, the most easily accessible tool a physician can use, has been demonstrated to be inadequate to differentiate the etiology of hypotension.Citation6,Citation8 Another disconcerting aspect to this patient population is that hypotension carries high mortality rates (16%–25%).Citation9,Citation10 In addition, 39% of all deaths following traumatic injury are results of uncontrolled hemorrhage with unrecognized or inadequately treated hypotension.Citation11
Early diagnosis and management of the hypotensive patient has been shown to decrease mortality and improve patient care, as a result it would seem prudent to develop high-fidelity learning models for the acquisition of the skills necessary to best care for these patients.Citation12,Citation13 Point-of-care ultrasound has been demonstrated to help clinicians narrow the differential diagnosis of the hypotensive patient. Furthermore, goal-directed ultrasound protocols have been implemented to reduce time to ultrasound evaluations, and these techniques are taught at many residency programs.Citation10,Citation12,Citation14
Research in ultrasound education has confirmed that early exposure can improve ultrasound skills.Citation15,Citation16 As a result, medical schools have started to implement curricula to teach point-of-care ultrasound skills.Citation17–Citation22 Currently, the most commonly used sonographic protocol is the “extended focused assessment with sonography for trauma” (EFAST), and this protocol is taught during medical school at numerous institutions.Citation5,Citation18 Simulation training for undergraduate medical education has also demonstrated strengths over traditional education due to the combination of immediate feedback, repetitive practice, curriculum integration, and clinical relevance.Citation23 To our knowledge, no prior study has incorporated the use of ultrasound to build critical problem-solving skills. The focus of this study was to evaluate a protocol-driven ultrasound education model for undergraduate medical education, with an emphasis on how the use of sonography in the evaluation of hypotension can help direct clinical problem-solving.
Methods
Study design/setting/population
This cross-sectional study was conducted at an academic medical center. This study was reviewed by the institutional review board of the University of Arizona and arbitrated as not systematic research. The institutional review board did not require informed consent from participants be obtained. The study participants were 3rd year medical students with minimal or no prior ultrasound training experience. Participation in the study was voluntary. Data were collected from September 2013 to March 2014.
Study protocol
At our institution, 3rd year medical students have periodic breaks from clinical rotations in which they meet as a group in the classroom setting. During this week, students are exposed to topics they will encounter in their clinical rotations, such as high-value health care, general procedures, pathology stations, and review of cardiopulmonary resuscitation. A 1-day educational workshop focusing on the use of point-of-care ultrasound for clinical problem-solving was integrated into one of these weeklong sessions. This ultrasound workshop was geared toward the use of “sonography in the evaluation of the hypotensive patient.” Instructors for this course were department of emergency medicine faculty, fellows, and residents with expertise in point-of-care ultrasound. The components of ultrasound workshop included asynchronous learning, 1-hour didactic lecture, a hands-on workshop, and an assessment survey administered at the end of the workshop and at 3 months following the workshop.
Asynchronous learning assignments, which included reading materials, YouTube hyperlinks, and information regarding other ultrasound educational websites were provided to the students prior to the workshop. These educational tools describe or demonstrate the point-of-care ultrasound applications relevant to the evaluation of the hypotensive patient. Additionally, a 1-hour didactic lecture was provided to participating 3rd year medical students. The purpose of this lecture was to review basic ultrasound physics, machine knobs/controls, and review the sonographic protocol for evaluation of hypotension. The hands-on skill sessions were developed based on recommendations made by the Council of Emergency Medicine Residency Directors and the Academy of Emergency Ultrasound regarding the competency skills required to assess the hypotensive patient.Citation24 Trained human models were used at the skill stations. Instruction at skill stations included different components of sonographic protocol for the evaluation of the hypotensive patient (). During the cardiac station, students were taught to look for sonographic signs consistent with cardiogenic hypotension: decreased cardiac contractility in the case of decompensated heart failure; dilated right ventricle, decreased right ventricle free wall motion, and plethoric inferior vena cava (IVC) in the case of pulmonary embolism; and pericardial effusion in the case of cardiac tamponade.
Table 1 Skills station descriptions
At the end of the workshop, knowledge assessment was conducted using a 28-item questionnaire aimed to assess the following components: knowledge of the use of ultrasound for the evaluation of the hypotensive patient, self-assessed confidence of various ultrasound applications, opinions of the ultrasound workshop, opinions of protocol-based clinical problem solving, and evaluation of exposure to ultrasound. In order to assess knowledge retention, a portion of the questionnaire was comprised of multiple-choice questions and clinical scenario questions. The multiple-choice questions assessed clinical management, sonographic findings, and basic ultrasound skills acquired during the workshop. The clinical scenario questions were two part questions that required students to choose the most appropriate diagnostic ultrasound application and to identify the pathology students were anticipating. Students were asked to assess their confidence in each of the sonographic skills that were taught during the workshop. The questionnaire was administered at the end of the workshop and 3 months following the workshop.
Data analysis
All analyses were performed using Stata 11 (StataCorp LP, College Station, TX, USA). Data are presented as means and percentages with 95% confidence intervals. Continuous variables were compared between the two groups (post-test immediately after workshop versus 3-month post-test) using Student’s t-test and Wilcoxon signed-rank test. The statistical level of significance was set at P<0.05.
Results
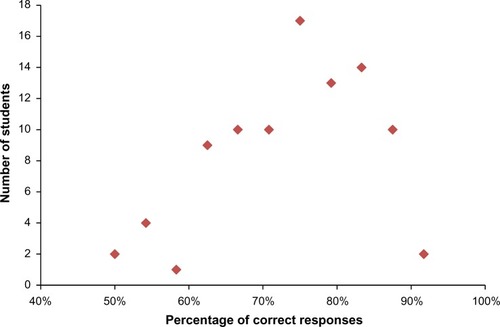
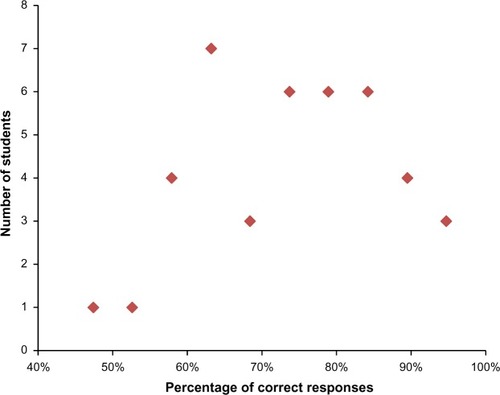
A total of 101 subjects participated in this ultrasound workshop, and 92% (93/101) completed the questionnaire at the end of the workshop. Forty-one percent of the students responded to our 3-month follow-up questionnaire. Only 17% (95% CI, 9%–25%) of students had been taught how to use ultrasound to assess a patient with hypotension prior to the workshop. Ninety-one percent (95% CI, 86%–97%) had interest in learning ultrasound and would enroll in an optional ultrasound curriculum if given the opportunity. Ninety-six percent (95% CI, 92%–100%) of students agreed that the use of “ultrasound protocol for the evaluation of the hypotensive patient” workshop helped them understand how ultrasound could be effectively integrated into clinical problem-solving. Similarly, 95% (95% CI, 90%–100%) felt that protocol-driven education was an effective teaching technique. Eighty percent (95% CI, 72%–88%) of students also felt that the ultrasound workshop helped them understand how ultrasound can change outcomes in acutely ill patients. After completing the ultrasound workshop, 100% of the medical students were able to complete the EFAST challenge within 3 minutes. Student performance in the knowledge assessment portion of the questionnaire was an average of 74% (SD=11%) at the end of workshop and 74% (SD=12%) 3 months later (P=0.00; and ). The confidence levels in each of the sonographic skills reported by students are summarized in .
Table 2 Students self-reported confidence with ultrasound skills on day 1 and day 90
Discussion
Our results suggest use of sonography for clinical problem solving such as in the evaluation of the hypotensive patient can be effectively taught to medical students. With increasing use of bedside sonography in the evaluation and management of critically ill patients, it is crucial for medical students to have ultrasound skills as they enter residency. To our knowledge, no prior studies have evaluated the integration of sonography into clinical problem solving sessions. We believe this approach generates more interest among medical students. Overall the students’ response to the workshop was positive. Although the majority of students had not previously received ultrasound training, they were easily able to integrate its use in the evaluation of hypotension and quickly picked up on the skills required to scan.
This is the first ultrasound workshop designed to teach medical students the ultrasound applications used to evaluate hypotensive patients. Unlike traditional ultrasound education, which is organ based, our curriculum was protocol driven. As the students rotated through the stations within the ultrasound protocol for the hypotensive patient, they learned about the possible hypotensive pathologies associated with each ultrasound application. For example, when rotating through the Aorta station, students were taught that although an abdominal aortic aneurysm is enlarged at 3 cm; in a hypotensive patient, an aneurysm greater than or equal to 6 cm is presumed ruptured. In addition, during the IVC station, students learned that IVC measurements are useful in extremes (flattened IVC = intravascular depletion and plethoric IVC = heart failure/pericardial effusion).
Incorporating hands-on training sessions is paramount to teaching ultrasound as this requires spatial motor skills that have been shown to improve with experience.Citation25 Our educational curriculum provided ample opportunities for students to gain hands-on experience with direct and immediate feedback from trained physicians. Based on previous experience, our goal was to create small groups with student to instructor ratios of 5:1. This increased the dedicated hands-on learning experience, and with minimal training students were able to acquire images for each of the stations. In fact, all students were able to complete an EFAST exam within the 3-minute timed station. Our results indicate that protocol-based ultrasound education was well received by the medical students. The ultrasound workshop created a comfortable learning environment in which students were able to learn diagnostic skills as well as procedural skills. In addition, critical thinking skills and conceptual knowledge was demonstrated on the post-test questionnaire. In fact, the average score on the questionnaire was 74% after the workshop despite the fact that the majority of students were ultrasound naïve.
Our study results indicate that students’ knowledge was maintained beyond 3 months. However, the self-reported confidence in sonographic skills was significantly reduced (). It is possible that the students’ lack of confidence is attributed to the lack of practice. In fact, 92% of the students had performed fewer than three ultrasounds in the preceding 3 months. Although the true impact of a 1-day workshop is unknown, students require practice in order to maintain and improve upon the spatial motor skills acquired during the workshop. In an era where ultrasound is easily accessible, developing an understanding of how to apply sonography to the bewildering patient will empower the next generation of critically thinking clinicians.
Limitations
Our study has several limitations including a small sample size. Although 92% of students responded to the questionnaire immediately after the 1-day event, only 41% of the students responded to the follow-up questionnaire 3 months after the event. Student knowledge retention was assessed, however, we did not test students’ competency in acquiring ultrasound images. Another limitation of the study was that some of the results were based on student self-assessment. Furthermore, it is possible that students with greater interest in ultrasound participated in this study and in the follow-up questionnaire. One educational limitation was the number of ultrasound applications being taught during a 1-day workshop. These students were ultrasound naïve and although the students demonstrated comprehension and skill development, it was challenging and complex. Lastly, our study was not designed to assess overall impact of the ultrasound protocol nor was it designed to assess the impact of integrating ultrasound into critical problem-solving. Long-term sonographic skill retention, usage, and impact on patient care were not assessed.
Conclusion
At our institution, we successfully integrated ultrasound and critical problem solving instruction, as part of a 1-day workshop for undergraduate medical education.
Acknowledgments
We would like to thank Mindray Medical International (Shenzhen, People’s Republic of China) for providing ultrasound machines for this event.
Disclosure
The authors report no conflicts of interest in this work.
References
- BurgessAWMcGregorDMMellisCMApplying established guidelines to team-based learning programs in medical schools: a systematic reviewAcad Med20148967868824556770
- AminiRStolzLAGrossATheme-based teaching of point-of-care ultrasound in undergraduate medical educationIntern Emerg Med201510561361825764053
- SchmidmaierREiberSEbersbachRLearning the facts in medical school is not enough: which factors predict successful application of procedural knowledge in a laboratory setting?BMC Med Educ2013132823433202
- SteadmanRHCoatesWCHuangYMSimulation-based training is superior to problem-based learning for the acquisition of critical assessment and management skillsCrit Care Med20063415115716374169
- AminiRKartchnerJZStolzLABiffarDHamiltonAJAdhikariSA novel and inexpensive ballistic gel phantom for ultrasound trainingWorld J Emerg Med20156322522826401186
- McGeeSAbernethyWBSimelDLThe rational clinical examination. Is this patient hypovolemic?JAMA19992811022102910086438
- WoCCShoemakerWCAppelPLBishopMHKramHBHardinEUnreliability of blood pressure and heart rate to evaluate cardiac output in emergency resuscitation and critical illnessCrit Care Med1993212182238428472
- MooreCLRoseGATayalVSSullivanDMArrowoodJAKlineJADetermination of left ventricular function by emergency physician echocardiography of hypotensive patientsAcad Emerg Med2002918619311874773
- JonesAEStiellIGNesbittLPNontraumatic out-of-hospital hypotension predicts inhospital mortalityAnn Emerg Med20044310611314707949
- JonesAETayalVSSullivanDMKlineJARandomized, controlled trial of immediate versus delayed goal-directed ultrasound to identify the cause of nontraumatic hypotension in emergency department patientsCrit Care Med2004321703170815286547
- SauaiaAMooreFAMooreEEEpidemiology of trauma deaths: a reassessmentJ Trauma1995381851937869433
- PereraPMailhotTRileyDMandaviaDThe RUSH exam: Rapid Ultrasound in SHock in the evaluation of the critically lllEmerg Med Clin North Am2010282956vii19945597
- VolpicelliGLamorteATullioMPoint-of-care multiorgan ultrasonography for the evaluation of undifferentiated hypotension in the emergency departmentIntensive Care Med2013391290129823584471
- AminiRAdhikariSFiorelloAUltrasound competency assessment in emergency medicine residency programsAcad Emerg Med201421779980125039680
- ButterJGrantTHEganMDoes ultrasound training boost Year 1 medical student competence and confidence when learning abdominal examination?Med Educ20074184384817696983
- KobalSLTrentoLBaharamiSComparison of effectiveness of hand-carried ultrasound to bedside cardiovascular physical examinationAm J Cardiol2005961002100616188532
- HoppmannRCookTHuntPUltrasound in medical education: a vertical curriculum at the University of South Carolina School of MedicineJ S C Med Assoc200610233033417703842
- RaoSvan HolsbeeckLMusialJLA pilot study of comprehensive ultrasound education at the Wayne State University School of Medicine: a pioneer year reviewJ Ultrasound Med20082774574918424650
- BahnerDPRoyallNAAdvanced ultrasound training for fourth-year medical students: a novel training program at The Ohio State University College of MedicineAcad Med20138820621323269306
- BahnerDPJasneABooreSMuellerACortezEThe ultrasound challenge: a novel approach to medical student ultrasound educationJ Ultrasound Med2012312013201623197555
- DreherSMDePhilipRBahnerDUltrasound exposure during gross anatomyJ Emerg Med20144623124024113480
- HoyerRMeansRRobertsonJUltrasound-guided procedures in medical education: a fresh look at cadaversIntern Emerg Med Epub2015815
- IssenbergSBMcGaghieWCPetrusaERLee GordonDScaleseRJFeatures and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic reviewMed Teach200527102816147767
- LewissREPearlMNomuraJTCORD-AEUS: consensus document for the emergency ultrasound milestone projectAcad Emerg Med20132074074523859589
- NichollsDSweetLHyettJPsychomotor skills in medical ultrasound imaging: an analysis of the core skill setJ Ultrasound Med2014331349135225063399
- BernardiECamporeseGBüllerHRSerial 2-point ultrasonography plus D-dimer vs whole-leg color-coded Doppler ultrasonography for diagnosing suspected symptomatic deep vein thrombosis: a randomized controlled trialJAMA20083001653165918840838