Abstract
Background
Tumescent mastectomy refers to usage of a mixture of lidocaine and epinephrine in a diluting saline solution that makes flaps firm and tense, thus minimizing systemic drugs toxicity and making surgery possible with minimal bleeding. This technique is very useful in elder women and those with American Society of Anesthesiologists; score III and IV. The objective was to establish an alternative safe technique to general anesthesia in some selected mastectomy patients.
Patients and methods
Twenty candidate women for total mastectomy and axillary dissection were enrolled and consented to participate. After preparation, an anatomically directed infiltration was made under sedation, using a cocktail of lidocaine, bupivacaine, and epinephrine, followed after 20 minutes by the surgical incision and completion of mastectomy. All intraoperative and postoperative outcomes were recorded.
Results
Although 7 cases required added analgesic medications, no conversion for general anesthesia was recorded. Mean operative time was 81±15.8 minutes. Mean blood loss was 95.8±47.5 mL. There was no recorded intraoperative hemodynamic instability. Postoperative visual analog score was not exceeding 4 till the end of the first 24 hours. Opioids were not required in any case, and the mean dosage of Ketorolac used was 30±8.75 mg. Drains output and the incidence of postoperative complications were acceptable.
Conclusion
We can consider tumescent mastectomy in well-selected patients a safe alternative for performing mastectomy when general anesthesia is hazardous, with minimal blood loss and long lasting postoperative analgesia without an additive effect on the operative time, hospital stay, and intraoperative and postoperative complications.
Keywords:
Introduction
Tumescent anesthesia is not a new technique. It has been routinely used in liposuction with a great success. Then, it was transferred to the field of plastic surgery and dermatology.Citation1 The concept of tumescent anesthesia depends on using a mix of lidocaine and epinephrine together with sodium bicarbonate in a diluting saline solution that is injected subcutaneously by infiltration till tissues become firm and tense, and this is the meaning of the word “tumescent”.Citation2 The reported safety of this technique was guaranteed by many authors due to slow systemic absorption of the lidocaine owing to the vasoconstrictive effect of epinephrine and partly due to vessel compression by hydrostatic effect of the solution itself.Citation2 The peak plasma level of lidocaine was reported after 4–12 hours, and the clinical local analgesia was reported to last for 18–24 hours.Citation3,Citation4 The use of this technique in mastectomy with or without reconstruction was limited and was reserved for elderly patients with comorbidities for whom general anesthesia is hazardous.Citation5 In spite of emergence of regional anesthetic techniques such as epidural anesthesia,Citation6 the intercostal blocks,Citation7 and the paravertebral block (PVB),Citation8 many problems were associated with these techniques as failure, risk of complications including pneumothorax, and accidental dural puncture, beside the need for specific skills and time consumption.Citation7 The aim of the current study is to address the suitable patients and the proper technique for doing mastectomy entirely by using the tumescent anesthesia.
Patients and methods
Patient selection
Twenty patients were enrolled into this prospective study that was carried out in the period from January 2014 until September 2015 after approval of the Mansoura Faculty of Medicine local institutional review board (Code number; R/16.06.03) with fulfillment of the criteria of Helsinki Declaration. The patients’ informed written consent to participate in the study was obtained after explanation of the technique and its possible hazards. This study included all patients with operable breast carcinoma who were candidates for total mastectomy with axillary clearance and were risky for general anesthesia, which was based on American Society of Anesthesiologists (ASA) scoring system around III–IV.Citation9
Patients with orthopnea, cardiomyopathy, poorly controlled arrhythmia, renal impairment, pheochromocytoma, hyperthyroidism, history of myocardial infarction or cerebral stroke, bedridden patients, those with advanced or metastatic local disease, those with prior chemotherapy or chest irradiation, those on long-term steroid therapy, noncompliant patients, and those with hypersensitivity to the tumescent cocktail were excluded from this study.
Method
Patient preparation
All demographic data were collected; standard laboratory investigations, ECG, ECHO cardiography, and other requested investigations according to patient comorbidities were made. The technique, its hazards, and the possibility of conversion to general anesthesia was explained before taking consent from patients. Premedication with midazolam 1–3 mg and dextrose 5% at a rate of 125 mL/h was given preoperatively starting at 6 am. Cardiovascular drugs were given, except for angiotensin receptor blockers and angiotensin-converting-enzyme inhibitors.
The tumescent technique
The tumescent cocktail
The volume of infiltrate was roughly estimated as two times the volume of the breast.Citation10 The breast volume was estimated using the following equation; Breast volume =0.973× (breast circumference/6.28)Citation3.Citation11
Components:
Lidocaine 2% in a total maximum dose of 20 mg/kg. The estimated safe dosage for tumescent lidocaine was shown to be at least 35 mg/kg.Citation4
Bupivacaine 0.5% was added at a dose of 2 mg/kg to prolong the postoperative analgesic effect.Citation12 A study by Swanson confirmed the safe use of bupivacaine in doses up to 550 mg (up to 9.2 mg/kg).Citation13 As a mixture, we used lower doses of lidocaine and bupivacaine to avoid additive toxicity.
Epinephrine 2 mg of 1/1,000 epinephrine/L of Ringer lactate solution.Citation5
Tumescent fluid infiltration and surgical procedure
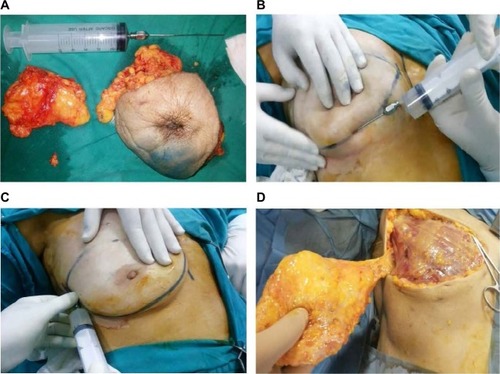
After establishing standard monitoring, local infiltration was done using a blunt tipped liposuction needle with 5 mm gauge (), which was introduced through a very small skin snip under a mild sedation using a combination of propofol (1 mg/kg intravenous [IV] bolus, with 0.1 mg/kg/min infusion), midazolam (0.03 mg/kg IV), and fentanyl (1 μg/kg IV) as tolerated by the patient.Citation5
Two infiltrations were used
The first entailed a wide subcutaneous infiltration of the surgical site, thereby creating a tumescence area till the breast became tense and blanched ().
The second technique was a field block to infiltrate the piercing intercostal nerves and subglandular space. This was made by infiltration under the superior skin flap in the subdermal plane along the caudal border of the clavicle (to block infraclavicular nerves), along the midaxillary line extending high in the axilla to block the lateral cutaneous branches of the second to seventh intercostal nerves (), under the inferior skin flaps, along the sternum in the subdermal planes to block the anterior intercostal nerves, and finally through the retromammary space infiltrating nerves under the pectoral fascia.
The breast, overlying skin, and fascia of the pectoralis major muscle were removed en bloc using the scalpel dissection with cauterization of bleeding points by diathermy, and this was followed by a limited axillary dissection of levels I and II.
Usually the incision was started 15 minutes after the end of infiltration to allow a proper anesthesia and analgesia.Citation3
We used an oxygen face mask in all patients with ischemic heart disease (IHD) and when SaO2 was below 92%.
Intraoperative management and measurements
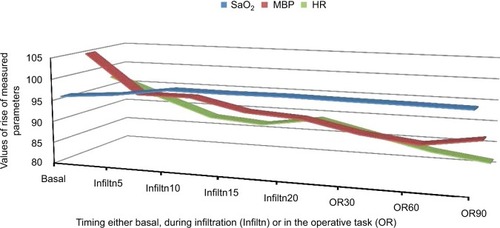
Clinical signs suggesting insufficient analgesia (pain, movement, or rise in blood pressure or heart rate >20% of the basal) were managed if necessary by fentanyl 25 μg increments, extra infiltration, propofol increments of 50 mg, or midazolam 1–2 mg, dexmedetomidine 1 μg/kg IV bolus over 10 minutes followed by infusion 0.2–0.5 μg/kg/h as required. Most of the patients requested this with axillary dissection. In the presence of excessive pain, movements, hemodynamic instability, or difficult ventilation, the technique was considered as failed and general anesthesia was conducted, airway was maintained by a suitable sized laryngeal mask (LMA) with sevoflurane inhalation. The mean blood pressure, heart rate, and oxygen saturation were recorded during the procedure ().
Total intraoperative requirements of propofol, fentanyl and midazolam, and dexmedetomidine were recorded, together with the conversion rate to general anesthesia.
Accordingly the tumescent anesthesia index was calculated as: The number of episodic adding propofol, fentanyl, midazolam, dexmedetomidine, and extra infiltration/duration of surgery in hours.
Infiltration time, the operative time, and the amount of blood loss were recorded.
All cases were operated by a single surgeon and surgeon satisfaction score from 0–10 was recorded.
Toxicity signs of local anesthetics or epinephrine side effects were assessed and managed according to ASRA recommendations (American Society of Regional Anesthesia).Citation14 The pulse, blood pressure, and oxygen saturation were recorded initially, then every 5 minutes during infiltration, then every 30 minutes. Hypotension was managed by boluses of ephedrine 5 mg and additional IV fluids. Hypertension was managed by increments of 25 μg fentanyl, dexmedetomidine 1 μg/kg over 10 min, and nitroglycrine 0.5–10 μg/kg/minute. Bradycardia was managed by 0.5 mg atropine, while tachycardia was managed as hypertension plus propranolol 1 mg if required. Other dysrhythmias were managed according to their specific types. Myocardial ischemia was assessed intraoperatively by ECG and postoperatively by ECG for all patients within 24 hours or in those with with clinical symptoms.
Postoperative management
The following parameters were recorded.
The total mean of postoperative vital signs (mean blood pressure, heart rate, and respiratory rate) in the first 24 hours.
ECG after 24 hours or in those with appearance of ischemic symptoms.
Pain assessment every 4 hours using the 10 points visual analog score (VAS).
The time till the first request for analgesia.
Postoperative analgesia, which was given on patient request or at VAS ≥4 as ketoralc 30 mg and paracetamol 1 g, and if pain was not controlled, nalbuphine 5 mg increments were given until VAS is ≤2.
Total analgesic requirements.
Rate of anesthetic complications as hypo or hypertension, dysrhythmia, or hypoxia.
The amount of drain output every day for 3 days.
Hematoma, seroma, flap necrosis, wound infection, and wound dehiscence.
The length of hospital stay.
Patient satisfaction on a score of 0–10.
Results
Patient demographic and clinical data are shown in . The operative data are shown in and . Postoperative outcomes are demonstrated in and . There was no reported complaint of chest pain, and there were no ECG changes after 24 hours. The mean postoperative VAS did not exceed 4 within the first 24 hours measurement (). There were 6 cases of postoperative mild seroma (30%) that were managed successfully with repeated aspiration. Simple hematoma occurred in three patients (15%), and all passed smoothly with conservative measures. There was one case of partial flap necrosis of less than 15%, which was treated by simple debridement at the outpatient clinic, and there was one case of minor wound gap that was treated by secondary closure after 2 weeks. shows a postoperative photo of one of the cases that was operated with the technique.
Figure 3 Four days postoperative view of a patient who underwent total mastectomy and axillary clearance by the tumescent technique.

Table 1 Demographic and clinical data (n=20)
Table 2 Operative data (n=20)
Table 3 Postoperative outcomes (n=20)
Discussion
Tumescent anesthesia is not a new technique, but it gained popularity through its wide use in liposuction techniques.Citation2,Citation15 In the field of breast surgery, it was popularized by WorlandCitation16 in 1996, when he observed its successful use in abdominoplasties, but it was reserved for elderly patients and those with poor anesthetic risk, especially those with ASA score III or IV.Citation5 Although epidural anesthesia, intercostal block, and paravertebral block are used in these situations, all are technically demanding, not free of complications, and still have a failure rate.Citation15 The tumescent technique depends on blockade of the noxious stimuli from nerve endings at the site of incision through infiltration of tissues around the nerve endings.Citation17 The most commonly used drug is lidocaine;Citation5 however, some authors add bupivacaine to prolong the analgesic effect.Citation18 To avoid the systemic toxicity of lidocaine absorption, two options were undertaken: the first was epinephrine that was added to constrict the blood vessels, and the second option was the hydrostatic pressure of the tumescent diluting saline which further compress vessels. By this technique, a very high concentration of lidocaine, up to 55 mg/kg, was used safely without significant complications.Citation19 There was a theoretical risk of epinephrine toxicity due to about 15 minutes delay of onset of vessels’ constriction with risk of elevated blood pressure, tachycardia, or arrhythmias.Citation20 Actually this was not recorded, partly due to the saline diluting effect and partly due to the compressed and constricted vessels by the tumescent fluid mechanical effect, which leads to slow absorption of epinephrine. Another advantage of the vasoconstrictive mechanism partly due to epinephrine and partly due to the hydrostatic pressure is the significantly minimized blood loss with nearly bloodless field () ().Citation21,Citation22 The use of propofol in this study was not for anesthetic purpose but it was as a sedative to enable the process of tumescent fluid infiltration. In our study, we used combined flaps infiltration and anatomically based regional local nerve infiltration. This is to ensure total analgesia, but it was very important to wait for nearly 15 minutes for the cocktail to work before starting the incision.Citation3 Actually, the time consumed in infiltration was compensated by the ease of mastectomy and the minimal blood loss (). Although, we described the use of local nerve blocks in this study, this does not mean a mastectomy with a field block; however, during tumescent infiltration, we focused on the regions of the sensory cutaneous nerves such as the infraclavicular and intercostal nerves. The tumescent technique is not just a nerve blockade, but it entails use of a cocktail that minimizes bleeding and blocks the sensory stimuli from every point along the mastectomy incision. In most of our cases, aid was provided with analgesic medications (), but there was no conversion to general anesthesia in any case. There was a high surgeon and patient satisfaction score, and this reflects the degree of success of the technique. In this study, most of patients were hemodynamically stable throughout the procedure with accepted vitals (), the same was recorded in the postoperative period with noticeable dramatic analgesic postoperative effect, which was reflected as the minimal requirement of postoperative analgesia (). In the literature, there is an argument about the impact of this technique on the incidence of post-mastectomy complications; some showed an increased rate of complications in the tumescent group,Citation21,Citation23 while others showed an increase of the native breast envelop necrosis.Citation24 However, other studies showed that the technique did not pose any additive effect to these complications.Citation25,Citation26 One of the interesting findings in a study by Johnson and his coworkersCitation27 that was reported in 2008 found lidocaine to provide a dose-dependent inhibition of bacterial growth, with growth of gram-negative organisms being inhibited more than gram-positive organisms. In our study, there were few postoperative complications that passed smoothly with conservative treatment (), and most of patients were discharged after the average hospital stay period. Some of the learned surgical tips are: infiltration under propofol sedation markedly alleviates patient apprehension and improves patient trust and confidence, it is very important to infiltrate the axilla well as this area is a common source of intraoperative painful stimuli. The cocktail decreases need for diathermy use, which is a source of painful stimuli or muscle contractions that irritates the patient. This technique can serve well for patients who would otherwise be canceled from operation and avoids the hazards and cost of general anesthesia and opioids that are commonly used for pain control in postmastectomy settings.
Conclusion
We can consider tumescent mastectomy in well-selected patients a safe alternative for mastectomy when general anesthesia is hazardous, with minimal blood loss and long lasting postoperative analgesia without an additive effect on the operative time, hospital stay, and intraoperative and postoperative complications.
Disclosure
The authors report no conflicts of interest in this work.
References
- Beck-SchimmerBPaschTTumescent technique for local anesthesiaAnasthesiol Intensivmed Notfallmed Schmerzther2002372848811865385
- ConroyPHO’RourkeJTumescent anaesthesiaSurgeon201311421022123375489
- KleinJAThe tumescent technique. Anesthesia and modified liposuction techniqueDermatol Clin1990834254372199105
- KleinJATumescent technique for regional anesthesia permits lidocaine doses of 35 mg/kg for liposuctionJ Dermatol Surg Oncol19901632482632179348
- CarlsonGWTotal mastectomy under local anesthesia: the tumescent techniqueBreast J200511210010215730454
- LynchEPWelchKJCarabuenaJMEberleinTJThoracic epidural anesthesia improves outcome after breast surgeryAnn Surg199522256637487214
- AtanassoffPGAlonEWeissBMIntercostal nerve block for lumpectomy: superior postoperative pain relief with bupivacaineJ Clin Anesth19946147518142099
- TerheggenMAWilleFBorel RinkesIHIonescuTIKnapeJTParavertebral blockade for minor breast surgeryAnesth Analg200294235535911812698
- DaabissMAmerican Society of Anaesthesiologists physical status classificationIndian J Anaesth201155211111521712864
- NovoaJCTumescent Anesthetic Breast Surgery (TABS): breast augmentation surgery in an office-based surgical centerMugeaTTShiffmanMAAesth Surg BreastBerlin HeildelbergSpringer2015107119
- El-OteifyMMegeedHAAhmedBEl-ShazlyMAssessment of the breast volume by a new simple formulaIndian J Plast Surg200639113
- JabsDRichardsBGRichardsFDQuantitative effects of tumescent infiltration and bupivicaine injection in decreasing postoperative pain in submuscular breast augmentationAesth Surg J2008285528533
- SwansonEProspective study of lidocaine, bupivacaine, and epinephrine levels and blood loss in patients undergoing liposuction and abdominoplastyPlast Reconstr Surg2012130370272222929254
- NealJMMulroyMFWeinbergGLAmerican Society of Regional Anesthesia and Pain MedicineAmerican Society of Regional Anesthesia and Pain Medicine checklist for managing local anesthetic systemic toxicity: 2012 versionReg Anesth Pain Med2012371161822189574
- BatraRKKrishnanKAgarwalAParavertebral blockJ Anaesthesiol Clin Pharmacol201127151121804697
- WorlandRGExpanded utilization of the tumescent technique for mastectomyPlast Reconstr Surg19969871321
- ScottNBWound infiltration for surgeryAnesthesia2010656775
- PaikAMDanialiLNLeeESHsiaHCLocal anesthetic use in tumescent liposuction: an American Society of Plastic Surgeons surveyAnn Plast Surg201574214515125590254
- OstadAKageyamaNMoyRLTumescent anesthesia with a lidocaine dose of 55 mg/kg is safe for liposuctionDermatol Surg199622119219279063507
- KleinJAAnesthetic formulation of tumescent solutionsDermatol Clin199917475175910526707
- AbbottAMMillerBTTuttleTMOutcomes after tumescence technique versus electrocautery mastectomyAnn Surg Oncol20121982607261122402814
- JosephAYBlochRYeeSSimple anesthesia for simple mastectomiesBreast Cancer Res Treat20037718919112602918
- SethAKHirschEMFineNAAdditive risk of tumescent technique in patients undergoing mastectomy with immediate reconstructionAnn Surg Oncol201118113041304621947584
- ChunYSVermaKRosenHUse of tumescent mastectomy technique as a risk factor for native breast skin flap necrosis following immediate breast reconstructionAm J Surg2011201216016520409522
- KhavaninNFineNABethkeKPTumescent technique does not increase the risk of complication following mastectomy with immediate reconstructionAnn Surg Oncol201421238438824121881
- VargasCRKoolenPGHoOATumescent mastectomy technique in autologous breast reconstructionJ Surg Res2015198252552925891675
- JohnsonSMSaint JohnBEDineAPLocal anaesthetics as antimicrobial agents: a reviewSurg Infect20089205213