Abstract
Postmenopausal women have an increased risk of osteopenia and osteoporosis due to loss of the bone-protective effects of estrogen. Disease-related processes may also contribute to the risk of bone loss in postmenopausal women with breast cancer. One of the most common and severe safety issues associated with cancer therapy for patients with breast cancer is bone loss and the associated increase in risk of fractures. This paper reviews the recent literature pertaining to aromatase inhibitor (AI)-associated bone loss, and discusses suggested management and preventative approaches that may help patients remain on therapy to derive maximum clinical benefit. A case study is presented to illustrate the discussion. We observed that AIs are in widespread use for women with hormone receptor-positive breast cancer and are now recommended as adjuvant therapy, either as primary therapy or sequential to tamoxifen, for postmenopausal women. AIs target the estrogen biosynthetic pathway and deprive tumor cells of the growth-promoting effects of estrogen, and AI therapies provide benefits to patients in terms of improved disease-free survival. However, there is a concern regarding the increased risk of bone loss with prolonged AI therapy, which can be managed in many cases with the use of bisphosphonates and other interventions (eg, calcium, vitamin D supplementation, exercise).
Introduction
Aromatase inhibitors (AIs) are increasingly used as adjuvant endocrine therapy, in addition to tamoxifen, for postmenopausal women with hormone-sensitive breast cancer.Citation1 The estrogen receptor is expressed in a large proportion of breast cancer tumors and has growth-promoting effects on tumor cells.Citation2 In about two thirds of all cases, breast cancer tumors are estrogen-sensitive.Citation3 Accordingly, many treatment strategies have focused on hormonal ablation, antagonism of estrogen receptor signaling, and suppression of estrogen synthesis.Citation2
AIs prevent estrogen synthesis by inhibiting the aromatase enzyme, which is responsible for the conversion of androgens to estrogen.Citation4 Adjuvant therapy with third-generation AIs is now an accepted standard for adjuvant endocrine treatment in addition to tamoxifen.Citation5,Citation6 Third-generation AIs include the nonsteroidal formulations, letrozole and anastrozole, and the steroidal formulation, exemestane.Citation4,Citation7 Nearly complete suppression of plasma estrogen levels has been demonstrated consistently with all third-generation AIs.Citation8–Citation13 A greater degree of estrogen suppression has been demonstrated with letrozole when compared with anastrozole in a similar study.Citation9 Greater suppression of each tissue estrogen fraction was observed with letrozole in blood plasma as well as in tumor tissues.Citation9 The clinical significance of these differences remains uncertain.
A recent update from the American Society of Clinical Oncology (ASCO) clinical practice guidelines re-emphasized the recommendation that AI therapy should be considered for all postmenopausal women with hormone receptor-positive (HR+) breast cancers.Citation14 In addition, St Gallen international expert consensus guidelines also suggest that AIs should be a preferred initial adjuvant endocrine therapy.Citation15 Nowadays, AIs are used routinely in three different postsurgical treatment approaches for patients with breast cancer, ie, upfront monotherapy (5 years of initial treatment with an AI), sequential adjuvant therapy (tamoxifen followed by an AI for a total of 5 years), and the extended adjuvant setting (using an AI after 5 years of tamoxifen).Citation6 If an extended strategy is used, the ASCO guidelines update recommends 5 years of tamoxifen followed by 3–5 years of an AI.Citation14 Superior clinical efficacy has been shown with all AIs compared with tamoxifen alone in each of these settings.Citation16–Citation23 While there is clear evidence that inclusion of an AI in the treatment strategy, whether upfront or switching after tamoxifen, is superior to 5 years of tamoxifen alone, the optimal strategy for AI use remains unclear.Citation24 However, only upfront use of an AI addresses the early peak of recurrence.
Following breast cancer surgery, there is a long-term risk of recurrence.Citation25 The first peak of recurrence occurs 1–2 years postsurgery.Citation25 The most common type of recurrence seen during this early peak is distant metastasis, while locoregional and contralateral recurrences occur at a much lower rate.Citation26 This is important because distant metastasis is associated with increased mortality.Citation27 Therefore, therapies that reduce distant metastasis during this early peak of recurrence may have the potential to improve survival.Citation27
All AI therapies, both as initial and as sequential therapy, have improved disease-free survival in patients with breast cancer; however, the effect on distant metastasis has not been uniform among AIs.Citation16–Citation19,Citation21,Citation22,Citation28–Citation32 The Breast International Group (BIG) 1-98 Arimidex, Tamoxifen Alone or in Combination (ATAC) and Tamoxifen Exemestane Adjuvant Multinational (TEAM) trials examined initial AI therapy compared with tamoxifen. The BIG 1-98 trial investigated the following adjuvant treatments in HR+ postmenopausal women following breast surgery: upfront initial letrozole for 5 years, upfront initial tamoxifen for 5 years, 2 years of letrozole followed by 3 years of tamoxifen, or 2 years of tamoxifen followed by 3 years of letrozole.Citation17 The initial results of the BIG 1-98 trial (n = 8010) at a median follow-up of 25.8 months demonstrated the superiority of letrozole over tamoxifen in significantly prolonging disease-free survival (hazard ratio [HR] = 0.81; P = 0.003).Citation17 In addition, letrozole-treated patients had a significant (P = 0.001) early benefit in time to distant recurrence, with a 27% reduction in risk of distant metastasis at this early time point.Citation17 Based on the results demonstrating the superiority of letrozole, the tamoxifen monotherapy arm was unblinded and patients were permitted to cross over to letrozole. The significant benefits of letrozole on disease-free survival (HR = 0.88; P = 0.03) and distant metastasis (HR = 0.85; P = 0.05) were maintained at a median follow-up of 76 months (monotherapy arms, n = 4922), despite crossover of 25.2% of patients.Citation19 In addition, there was a trend (HR = 0.87; P = 0.08) in the intent-to-treat population suggesting an overall survival benefit with letrozole. Because the crossover complicated the results, the inverse probability of a censored weighting method was utilized. Using this method a 17% (95% confidence interval [CI], 0.71–0.97) improvement in overall survival was seen with letrozole compared with tamoxifen. Similar to the BIG 1-98 trial, the ATAC trial (N = 9366 overall; n = 5216 HR+ patients), which compared anastrozole with tamoxifen monotherapy in HR+ and HR-unknown postmenopausal women following breast cancer surgery, demonstrated a significant (HR = 0.83; P = 0.005) disease-free survival benefit with anastrozole over tamoxifen at 68 months’ median follow-up in HR+ patients.Citation16 However, anastrozole did not provide a significant (HR = 0.84; P = 0.06) reduction in distant metastasis at this time point, nor was there any overall survival benefit (HR = 0.97; P = 0.7). Only at 100 months’ follow-up was there a significant (HR = 0.84; P = 0.022) distant metastasis benefit, along with maintenance of a significant benefit in disease-free survival (HR = 0.85; P = 0.003), but there was still no overall survival improvement (HR = 0.97; P = 0.7).Citation31 The TEAM trial (n = 9766) was originally designed to compare adjuvant therapy with 5 years of exemestane versus 5 years of tamoxifen in postmenopausal women with HR+ breast cancer.Citation23 However, it was modified to include sequential therapy with tamoxifen for 2.5–3.0 years followed by exemestane. The first coprimary endpoint at 2.75 years analyzed patients randomized to initial therapy with exemestane or tamoxifen, and found no significant improvement in disease-free survival with exemestane compared with tamoxifen (HR = 0.89; P = 0.12). The second coprimary endpoint at 5 years, comparing exemestane monotherapy versus sequential therapy (tamoxifen to exemestane), also showed no difference in disease-free survival (HR = 0.97; P = 0.604).Citation33
Switch studies differ from initial adjuvant trials in that patients are randomized after completing 2–3 years of tamoxifen, and they exclude patients with disease recurrence (including patients with early distant metastases) during this prerandomization period. The Intergroup Exemestane Study (IES) examined estrogen receptor-positive (ER+) or ER-unknown patients (n = 4742) receiving tamoxifen followed by exemestane versus patients receiving tamoxifen monotherapy.Citation22 In hormone-responsive patients at a median follow-up of 56 months, the IES showed a significant improvement in disease-free survival in patients who switched to exemestane after 2–3 years of tamoxifen treatment (HR = 0.75; P = 0.0001).Citation22 The results of this study also demonstrated significant improvement in overall survival in this patient population (HR = 0.83; P = 0.05). The Austrian Breast and Colorectal Cancer Study Group (ABCSG) 8 trial compared tamoxifen followed by anastrozole versus tamoxifen monotherapy in hormone-sensitive patients with breast cancer (n = 2566 switch population).Citation30 At 30 months’ median follow-up, event-free survival favored sequential therapy (HR = 0.68; P = 0.02). However, switch trials do not include distant metastasis occurring during the early periods following surgery and only examine patients who respond to therapy. Initial adjuvant AI therapy has demonstrated superior efficacy compared with tamoxifen, but only letrozole significantly reduced early distant metastasis, possibly resulting in a long-term survival advantage.
Even though AI therapy has clear benefits for patients with breast cancer, AIs can also have detrimental long-term effects on bone health.Citation34–Citation36 Bone loss is a predictable consequence of estrogen deprivation.Citation37 Estrogen has a negative regulatory effect on bone resorption; therefore, any therapy that depletes estrogen has the potential to cause bone loss, impacting bone integrity and putting the patient at risk for fractures. Postmenopausal patients with breast cancer are already at an increased risk of osteoporosis due to age-related failure of ovarian function, a corresponding decline in estrogen levels, and possible disease-related bone loss. Potential treatment-related bone loss may be an added risk factor.Citation2,Citation38–Citation40 Cancer treatment-induced bone loss may be accentuated in women with breast cancer who are receiving multiple forms of anticancer treatment (eg, chemotherapy, endocrine therapy).Citation41
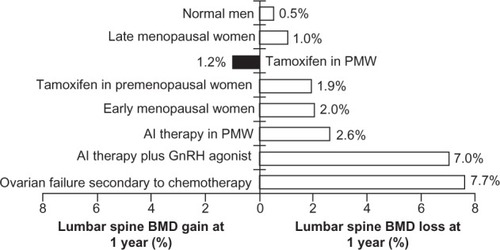
For example, average lumbar spine bone mineral loss at one year has been reported to be 1%–2% in early and late menopausal women, compared with 7.7% in women with ovarian failure secondary to chemotherapy (). AI-induced bone loss with endocrine therapy is associated with rapid bone loss and an increased fracture risk that is distinctly different from that observed in postmenopausal osteoporosis ().Citation2 One of the most common side effects of AI use is skeletal bone loss leading to thinning of the bone (osteopenia) and/or an increased risk of bone fractures.Citation6,Citation42,Citation43 When combined with other treatments, this risk may be significantly enhanced (). Eastell et al reported a 2.6% loss in lumbar spine bone mineral density in postmenopausal women with breast cancer receiving AI treatment.Citation44 In comparison, a 7% loss was reported in women receiving AI therapy combined with a gonadotropin-releasing hormone agonist.Citation45
Figure 1 Cancer treatment-induced bone loss.Citation44,Citation45,Citation88–Citation90
The bone loss seen during AI treatment appears to be similar from one agent to another within this class, although there is a paucity of data from direct comparator trials.Citation21,Citation46 A randomized investigation of healthy volunteers (Letrozole, Exemestane, and Anastrozole Pharmacodynamic trial) demonstrated that all AIs (steroidal or nonsteroidal) have a similar effect on bone and are associated with increased bone turnover.Citation47 Recently, there has been greater recognition of the increased fracture rates and bone loss seen in studies of patients undergoing AI therapy,Citation48,Citation49 and also of the need for appropriate management and intervention to reduce bone loss and prevent fragility fractures.Citation34,Citation42,Citation50,Citation51 This paper reviews the recent literature pertaining to the risk of fractures and the premature or accelerated development of bone loss in patients treated with adjuvant AI therapy. A case study is described for a patient who demonstrated decreasing bone mineral density while undergoing treatment with endocrine therapy. Suggested management approaches are also discussed.
AI-associated bone loss
Bone tissue undergoes a continuous resorption/formation process. Small amounts of bone mineral that are removed by osteoclasts (resorption) are balanced by equal deposition of new mineral by osteoblasts (formation), preserving bone strength.Citation52 Estrogen is one of the crucial modulators of bone formation. In postmenopausal women, low estrogen levels are associated with increased bone turnover, which may result in net bone loss,Citation53–Citation55 a decrease in bone strength, and an increased fracture risk.Citation37,Citation55–Citation58 Adjuvant endocrine therapy is designed to deprive tumor cells of the growth-promoting effects of estrogen.Citation59 AIs prevent estrogen synthesis by inhibiting the aromatase enzyme, which is responsible for the conversion of androgens to estrogen.Citation4 Therefore, estrogen deprivation during AI therapy in postmenopausal women may increase bone turnover and induce bone loss, which is observed at sites rich in trabecular bone, at an average rate of 1%–3% annually. This leads to an increase in fracture incidence compared with that seen during tamoxifen therapy.Citation60 Although the mechanism of action between the steroidal (binding irreversibly to aromatase, eg, exemestane) and nonsteroidal (competitive inhibitors that bind to the heme moiety of the aromatase cytochrome P450 complex, eg, anastrozole, letrozole)Citation61 AIs is somewhat different, adverse effects on bone health have been observed with all currently used AIs ().
Table 1 Bone-related and fracture-related adverse events from aromatase inhibitor (AI) trialsCitation5,Citation18,Citation22,Citation31,Citation62
Anastrozole
The ATAC trial compared the efficacy and safety of anastrozole with that of tamoxifen in the initial adjuvant setting in postmenopausal women with early breast cancer.Citation16,Citation28 After a median follow-up of 68 months, the fracture rate was 11% for patients treated with anastrozole (n = 3092) versus 7.7% in patients treated with tamoxifen (n = 3094).Citation16
Letrozole
The BIG 1-98 trial is the largest ongoing trial comparing letrozole with tamoxifen in the initial adjuvant setting. A slight but significant (P < 0.001) difference in fracture rate was observed between the letrozole arm (5.7%) and the tamoxifen arm (4.0%) at 25.8 months of median follow-up.Citation17 At 51 months of follow-up, letrozole (n = 2448) was associated with an 8.6% versus 5.8% fracture rate with tamoxifen (n = 2447) (P < 0.001).Citation18 At 5 years of follow-up, the incidence of bone fractures remained higher among patients treated with letrozole (9.3% versus tamoxifen 6.5%; no P value reported).Citation62 The wrist was found to be the most common site of fracture in each treatment group.
Exemestane
In the IES, patients were randomized to either 5 years of tamoxifen (n = 2372) or a switch to exemestane following 2–3 years of tamoxifen treatment (n = 2352) for a total of 5 years. Within 6 months of switching to exemestane, bone mineral density was lowered by 2.7% at the lumbar spine and 1.4% at the hip compared with baseline values (P < 0.0001 at both sites).Citation63 All in all, 162 patients (7%) in the exemestane arm and 115 (5%) in the tamoxifen arm had fractures at a mean follow-up of 58 months (P = 0.01). In the TEAM trial, tamoxifen treatment resulted in a 0.5% increase from baseline in bone mineral density at the spine, which was maintained at the 12-month assessment (n = 83). In contrast, exemestane treatment resulted in an increase in bone loss at 6 months (2.6% decrease in spine bone mineral density) and a further decrease of 0.2% at 12 months (n = 78).Citation36 In a recent subanalysis of the TEAM trial, exemestane resulted in increases from baseline in all bone turnover markers (eg, bone-specific alkaline phosphatase, amino terminal propeptide type I, procollagen, osteocalcin) at all time points.Citation64 In contrast, levels of all bone turnover markers decreased with tamoxifen treatment.
Case report
A 62-year-old postmenopausal female presented with ER+, progesterone receptor-positive, human epidermal growth factor receptor 2-negative breast cancer. The patient’s age of menopausal onset was 51 years and she received hormone replacement therapy until her diagnosis of breast cancer. She did not have any family history relevant to osteoporosis, and there was no history of prevalent fractures, glucocorticoid therapy, chemotherapy, or smoking.
The patient was diagnosed to have invasive ductal breast cancer on the left side. Upon diagnosis, she underwent the standard procedure in Germany which included chest radiography, liver ultrasound, and scintigraphy, and all tests revealed no sign of metastasis. Breast-conserving surgery (including sentinel lymphadenectomy) was performed. One month later, skeleton scintigraphy showed no sign of bone metastasis and the patient was placed on AI therapy (letrozole 2.5 mg/day, orally). The patient also received adjuvant radiation therapy to the left breast. Her bone mineral density was measured by dual-energy x-ray absorptiometry at two locations, ie, the femur and lumbar spine (initial, 12-month, and 24-month data are presented in – [A, B, and C, respectively] and ). Quantitative ultrasound assessments of bone were also made at the initial, 12, and 24-month time points (). The patient’s bone scans showed decreasing bone mineral density over time while on letrozole treatment.
Figure 2 Left femur bone mass density over time. (A) At baseline, (B) at 12 months, and (C) at 24 months.
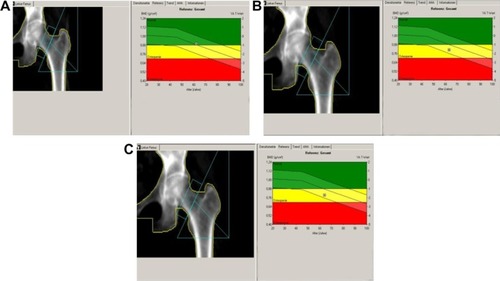
Figure 3 Right femur bone mass density over time. (A) At baseline, (B) at 12 months, and (C) at 24 months.
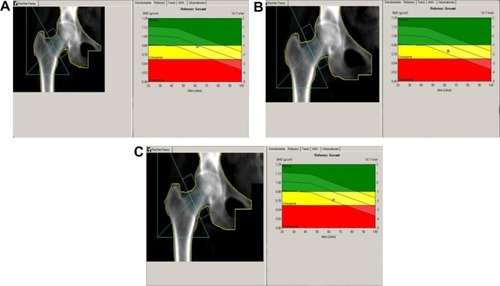
Figure 4 Lumbar spine bone mass density over time. (A) At baseline, (B) at 12 months, and (C) at 24 months.
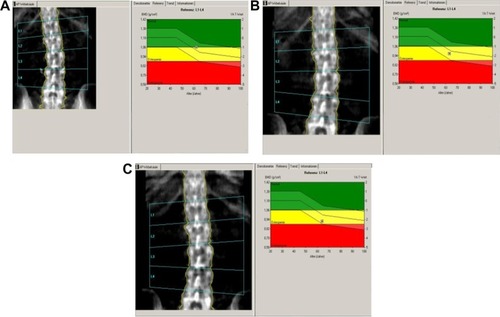
Table 2 Dual-energy X-ray absorptiometry (DXA) and quantitative ultrasound (QUS) results
Guidelines for bone loss management
Osteoporosis screening and treatment are standard components of health maintenance in postmenopausal women; however, current treatment and preventative guidelines are inadequate for averting fractures in osteopenic women with breast cancer, especially those receiving AI therapy.Citation65,Citation66 A more complete understanding of clinically relevant risk factors for fracture will help to assess overall fracture risk and provide practical guidance for the prevention and treatment of bone loss in this population.Citation34,Citation65,Citation66
In order to place bone mineral density assessments and other risk factors within the context of identifying women with breast cancer who are at increased risk of fracture, and who are likely candidates for preventative therapy, a panel of experts recently evaluated data from large clinical trials in postmenopausal women and women with breast cancer to develop international consensus guidelines for using clinical risk factors for fracture along with bone mineral density measurements.Citation67 Eight risk factors were validated in women with breast cancer, including AI therapy, t score <−1.5, age >65 years, low body mass index (<20 kg/m2), family history of hip fracture, personal history of fragility fracture after the age of 50 years, oral corticosteroid use >6 months, and smoking.Citation34,Citation68 These current guidelines underscore the importance of comprehensive fracture risk assessment and advocate bone mineral density measurement in all patients taking AIs with selective use of antiresorptive therapy in osteoporotic (t score <−2.5) women.Citation68,Citation69 Evaluating both bone mineral density and clinical risk factors may allow for the most effective identification of patients with breast cancer who have an increased risk of fracture as well as the appropriate use of preventative therapies.Citation70
Zometa-Femara Adjuvant Synergy Trials
Mounting evidence now suggests that treatment with bisphosphonates (eg, zoledronic acid) may help manage and potentially prevent AI-associated bone loss.Citation2,Citation24,Citation50,Citation68,Citation71,Citation72 Because of the increased bone loss associated with use of AIs, three randomized international studies, ie, the Zometa-Femara Adjuvant Synergy Trials (Z-FAST, ZO-FAST, and E-ZO-FAST), were performed to evaluate the bone-protective effects of zoledronic acid during endocrine treatment with letrozole. The primary endpoint of these companion trials was to determine the impact of upfront or delayed (if t score < −2.0 or in the presence of a fracture) zoledronic acid on bone mineral density at the lumbar spine at 12 months in postmenopausal women (n = 2194) with hormone-sensitive breast cancer receiving letrozole. Secondary endpoints included fracture rate, disease-free survival, and disease recurrence. These studies have all shown that the bone mineral density loss associated with AI therapy can be prevented effectively by adjuvant treatment with zoledronic acid. Current management guidelines now recommend that any patient initiating or receiving AI therapy with any two identified risk factors should receive bisphosphonate therapy.Citation34
The results of the Z-FAST study demonstrate a continuous annual bone mineral density increase at both the lumbar spine and total hip in patients who were receiving upfront zoledronic acid (n = 301) versus delayed treatment (n = 301).Citation72 Long-term 5-year follow-up data confirm that compared with a delayed start, upfront zoledronic acid (4 mg intravenously every 6 months) effectively prevents/treats bone loss in postmenopausal women, regardless of baseline t score, chemotherapy status, or number of osteoporotic risk factors.Citation72 The results show a progressive and significantly increased lumbar spine and total hip bone mineral density over 5 years with upfront zoledronic acid treatment (percent change in lumbar spine and total hip bone mineral density from baseline at 61 months: 6.19% and 2.57%, respectively, P < 0.0001).Citation72 Similarly, in the ZO-FAST study (n = 1065), there were significant increases in bone mineral density in favor of upfront zoledronic acid compared with delayed zoledronic acid at the 5-year final follow-up (lumbar spine 10%, P < 0.0001).Citation73 However, it should be noted that there was no difference observed in fracture rates between the two treatment groups (upfront or delayed).Citation73 Over the 5-year study duration, osteonecrosis of the jaw was found in 4/669 patients who received zoledronic acid (0.6%).Citation73 Other adverse events were consistent with the known safety profile of zoledronic acid.
Potential anticancer activity of bisphosphonates
The principal biologic effect of bisphosphonates is to inhibit osteoclastic bone resorption; these agents may impede both the development of bone metastases and the survival of dormant cancer cells in the bone marrow microenvironment.Citation74–Citation76 In addition to their primary effect upon bone mineral density, bisphosphonates also may confer additional anticancer benefits. Several direct and indirect mechanisms may contribute to this anticancer activity, including cancer cell apoptosis, inhibition of proliferation and migration, reduction in angiogenesis, activation of the immune system against cancer cells, and synergistic effects with other cancer treatments such as endocrine and chemotherapies.Citation76,Citation77 Therefore, bisphosphonates may provide further clinical benefit to patients with breast cancer by reducing the risk of distant and bone metastasis and increasing overall survival and disease-free survival.Citation78
Given the potential anticancer activity of the bisphosphonates, the Zometa-Femara Adjuvant Synergy Trials included disease-free survival as a secondary endpoint, although the studies were insufficiently powered to detect differences between treatment arms for this variable, and the findings should be interpreted with caution (). In the recent analysis at 5-year follow-up of the ZO-FAST study, upfront zoledronic acid was associated with a significant 34% reduction in risk of recurrence compared with use of delayed zoledronic acid (P = 0.034).Citation73,Citation79 However, recently published data from the AZURE trial that examined adjuvant use of bisphosphonates in reducing rates of recurrence and death in patients with early-stage breast cancer found no significant between-group difference in disease-free survival (primary endpoint of this study) in patients on standard adjuvant systemic therapy either with or without zoledronic acid.Citation80
Table 3 Disease-free survival (DFS) events and deathsTable Footnotea
Discussion
Use of emerging international guidelines to initiate bisphosphonate therapy as an early intervention strategy may help to prevent a large percentage of all potential fractures in postmenopausal patients with breast cancer receiving AI therapy.Citation34,Citation70 The case study discussed herein represents one potential illustrative example. The patient concerned would not have been eligible for zoledronic acid treatment based on her scans at 12 months because the t score was more than −2 and there was an absence of other risk factors, eg, family history. Nevertheless, extended treatment with letrozole and the latest scan in 2009 demonstrated that the patient would be a potential candidate for zoledronic acid treatment.
Given its significant benefit in breast cancer treatment, eg, reduction in distant metastases, AI therapy should be maintained with effective management of adverse events in order to maximize patient benefit. The benefits of superior disease control should always be considered along with effective management of adverse events. Effective management of bone loss with adjuvant bisphosphonate therapy has been demonstrated while maintaining AI therapy.Citation81 The bone mineral density loss seen in the patient described in the present case report may have been mitigated with early intervention with adjuvant zoledronic acid therapy. Other strategies may also be combined with bisphosphonate therapy for the effective management of AI-associated bone loss. These strategies may include various lifestyle adjustments, such as muscle-strengthening exercises, reduced alcohol consumption, cessation of smoking, and dietary supplementation with calcium and vitamin D.Citation82–Citation86
Conclusion
Adjuvant AI treatment of HR+ breast cancer in postmenopausal women has now become the standard of care due to superior disease-free survival results and a more favorable side effect profile compared with tamoxifen. However, due to the profound estrogen depletion that occurs with AI therapy, negative effects on bone health may also be observed. Screening and medical management for bone complications in patients with breast cancer being treated with AIs is therefore an important area for clinical intervention. The presence of risk factors (eg, age, t score, body mass index, family and personal history, smoking) may be used for appropriate patient stratification and determination of an optimal treatment plan to preserve bone integrity. Several studies have demonstrated the efficacy of antiresorptive agents (eg, bisphosphonates) for prevention of the bone mineral density loss associated with breast cancer therapy. Although no treatments are approved specifically for AI-associated bone loss, patients at high risk of rapid bone loss may benefit from early and sustained intravenous bisphosphonate therapy. Adequate calcium and vitamin D supplementation and a healthy lifestyle may also positively impact long-term bone health. In the case study presented herein, eligibility for bisphosphonate therapy according to the 2006 consensus guidelines would not have been met due to the lack of risk factors and bone mineral density being above the guideline threshold values. However, according to the revised 2009 guidelines, eligibility criteria would have been met. In addition to the positive effects on bone health, there is now some evidence supporting the potential anticancer benefits of bisphosphonate therapy. Therefore, patients may potentially derive dual benefit from both improvement in bone health and anticancer activity.
Disclosure
Financial support for the medical editorial assistance of Maria Soushko was provided by Novartis Pharmaceuticals.
References
- MortimerJEManaging the toxicities of the aromatase inhibitorsCurr Opin Obstet Gynecol201022566020019610
- HadjiPAromatase inhibitor-associated bone loss in breast cancer patients is distinct from postmenopausal osteoporosisCrit Rev Oncol Hematol200969738218757208
- FolkestadLBjarnasonNHBjerregaardJKBrixenKThe effect of aromatase inhibitors on bone metabolismBasic Clin Pharmacol Toxicol200810431019152547
- MillerWRBartlettJBrodieAMAromatase inhibitors: are there differences between steroidal and nonsteroidal aromatase inhibitors and do they matter?Oncologist20081382983718695261
- JanniWHeppPAdjuvant aromatase inhibitor therapy: outcomes and safetyCancer Treat Rev20103624926120133065
- ContePFrassoldatiAAromatase inhibitors in the adjuvant treatment of postmenopausal women with early breast cancer: putting safety into perspectiveBreast J200713283517214790
- OzairSIqbalSEfficacy and safety of aromatase inhibitors in early breast cancerExpert Opin Drug Saf2008754755818759707
- MacedoLFSabnisGBrodieAAromatase inhibitors and breast cancerAnn N Y Acad Sci2009115516217319250202
- GeislerJAromatase inhibitors: from bench to bedside and backBreast Cancer200815172618224389
- GeislerJKingNDowsettMInfluence of anastrozole (Arimidex), a selective, non-steroidal aromatase inhibitor, on in vivo aromatisation and plasma oestrogen levels in postmenopausal women with breast cancerBr J Cancer199674128612918883419
- GeislerJKingNAnkerGIn vivo inhibition of aromatization by exemestane, a novel irreversible aromatase inhibitor, in postmenopausal breast cancer patientsClin Cancer Res19984208920939748124
- GeislerJHaynesBAnkerGDowsettMLonningPEInfluence of letrozole and anastrozole on total body aromatization and plasma estrogen levels in postmenopausal breast cancer patients evaluated in a randomized, cross-over studyJ Clin Oncol20022075175711821457
- DowsettMJonesAJohnstonSRJacobsSTrunetPSmithIEIn vivo measurement of aromatase inhibition by letrozole (CGS 20267) in postmenopausal patients with breast cancerClin Cancer Res19951151115159815951
- BursteinHJGriggsJJPrestrudAATeminSAmerican Society of Clinical Oncology clinical practice guidelines: update on adjuvant endocrine therapy for women with hormone receptor-positive breast cancerJ Clin Oncol2010283784379620625130
- GoldhirschAIngleJNGelberRDThresholds for therapies: highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2009Ann Oncol2009201319132919535820
- HowellACuzickJBaumMResults of the ATAC (Arimidex, Tamoxifen, Alone or in Combination) trial after completion of 5 years’ adjuvant treatment for breast cancerLancet2005365606215639680
- ThürlimannBKeshaviahACoatesASA comparison of letrozole and tamoxifen in postmenopausal women with early breast cancerN Engl J Med20053532747275716382061
- CoatesASKeshaviahAThürlimannBFive years of letrozole compared with tamoxifen as initial adjuvant therapy for postmenopausal women with endocrine-responsive early breast cancer: update of study BIG1-98J Clin Oncol20072548649217200148
- MouridsenHGiobbie-HurderAGoldhirschALetrozole therapy alone or in sequence with tamoxifen in women with breast cancerN Engl J Med200736176677619692688
- BoccardoFRubagottiAPuntoniMSwitching to anastrozole versus continued tamoxifen treatment of early breast cancer: preliminary results of the Italian Tamoxifen Anastrozole TrialJ Clin Oncol2005235138514716009955
- CoombesRCHallEGibsonLJA randomized trial of exemestane after two to three years of tamoxifen therapy in postmenopausal women with primary breast cancerN Engl J Med20043501081109215014181 Erratum in:New Engl J Med20043512461
- CoombesRCKilburnLSSnowdonCFSurvival and safety of exemestane versus tamoxifen after 2–3 years’ tamoxifen treatment (Intergroup Exemestane Study): a randomised controlled trialLancet200736955957017307102 Erratum in:Lancet200736990617368151
- JonesSESeynaeveCHasenburgAResults of the first planned analysis of the TEAM (tamoxifen exemestane adjuvant multinational) prospective randomized phase III trial in hormone sensitive postmenopausal early breast cancerCancer Res200969Suppl 267S Abstract 15
- ChlebowskiRCuzickJAmakyeDClinical perspectives on the utility of aromatase inhibitors for the adjuvant treatment of breast cancerBreast200918Suppl 2S1S1119712865
- SaphnerTTormeyDCGrayRAnnual hazard rates of recurrence for breast cancer after primary therapyJ Clin Oncol199614273827468874335
- MansellJMonypennyIJSkeneAIPatterns and predictors of early recurrence in postmenopausal women with estrogen receptor-positive early breast cancerBreast Cancer Res Treat2009117919819112615
- LameratoLHavstadSGandhiSJonesDChlebowskiRBreast cancer recurrence and related mortality in US pts with early breast cancerJ Clin Oncol200523Suppl 1662S Abstract 738
- BaumMBuzdarACuzickJAnastrozole alone or in combination with tamoxifen versus tamoxifen alone for adjuvant treatment of postmenopausal women with early-stage breast cancer: results of the ATAC (Arimidex, Tamoxifen Alone or in Combination) trial efficacy and safety update analysesCancer2003981802181014584060
- GossPEIngleJNMartinoSRandomised trial of letrozole following tamoxifen as extended adjuvant therapy in receptor-positive breast cancer: updated findings from NCIC CTG MA.17J Natl Cancer Inst2005971262127116145047
- JakeszRJonatWGnantMSwitching of postmenopausal women with endocrine-responsive early breast cancer to anastrozole after 2 years’ adjuvant tamoxifen: combined results of ABCSG trial 8 and ARNO 95 trialLancet200536645546216084253
- ForbesJFCuzickJBuzdarAEffect of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: 100-month analysis of the ATAC trialLancet Oncol20089455318083636
- JonatWHilpertFKaufmannMAromatase inhibitors: a safety comparisonExpert Opin Drug Saf2007616517417367262
- ReaDHasenburgASeynaeveCFive years of exemestane as initial therapy compared to tamoxifen followed by exemestane for five years: the TEAM trial, a prospective, randomized, phase iii trial in postmenopausal women with hormone-sensitive early breast cancerCancer Res200969SupplS24
- HadjiPAaproMSBodyJJPractical guidance for the management of aromatase inhibitor-associated bone lossAnn Oncol2008191407141618448451
- ClunieGPClarkAMortimerCJEvaluating bone health in women with oestrogen receptor positive breast cancer (ERBC) starting aromatase inhibitorsEur J Surg Oncol20093547548018950981
- HadjiPZillerMKiebackDGEffects of exemestane and tamoxifen on bone health within the Tamoxifen Exemestane Adjuvant Multicentre (TEAM) trial: results of a German, 12-month, prospective, randomised substudyAnn Oncol2009201203120919218306
- DelaneyMFStrategies for the prevention and treatment of osteoporosis during early postmenopauseAm J Obstet Gynecol2006194Suppl 2S12S2316448872
- GibsonKO’BryantCLScreening and management of osteoporosis in breast cancer patients on aromatase inhibitorsJ Oncol Pharm Pract20081413914518719068
- GralowJRBiermannJSFarookiANCCN Task Force Report: Bone Health in Cancer CareJ Natl Compr Canc Netw20097Suppl 3S1S32S33S3519555589
- GeislerJLonningPEImpact of aromatase inhibitors on bone health in breast cancer patientsJ Steroid Biochem Mol Biol201011829429919833206
- BertoldoFPancheriSZenariSBoldiniSEmerging drugs for the management of cancer treatment induced bone lossExpert Opin Emerg Drugs20101532334220377485
- YamamotoDSVialePHUpdate on identifying and managing osteoporosis in women with breast cancerClin J Oncol Nurs200913E18E2919793700
- RugoHSThe breast cancer continuum in hormone-receptor-positive breast cancer in postmenopausal women: evolving management options focusing on aromatase inhibitorsAnn Oncol200819162717693420
- EastellRHannonRACuzickJClackGAdamsJEEffect of anastrozole on bone density and bone turn over: results of the ‘Arimidex’ (anastrozole), Tamoxifen, Alone or in Combination (ATAC) studyJ Bone Miner Res200217Suppl 1S165
- GnantMHausmaningerHSamoniggHChanges in bone mineral density caused by anastrozole or tamoxifen in combination with goserelin (+/− zoledronate as adjuvant treatment for hormone receptor-positive premenopausal breast cancer: results of a randomized multicenter trialBreast Cancer Res Treat200276Suppl 1S31 Abstract 12
- McCaigFMRenshawLWilliamsLA randomised study of the effects of anastrozole (A), letrozole (L) and exemestane (E) on bone turnoverBreast Cancer Res Treat200911964365119941160
- McCloskeyEHannonRLaknerGClackGMiyamotoAEastellRInteraction between body mass index and bone turnover during aromatase inhibition: evidence from the letrozole (L), exemestane (E), and anastrozole (A) pharmacodynamics (LEAP) trialJ Clin Oncol200725Suppl 1817S Abstract 560
- ReidDMPrevention of osteoporosis after breast cancerMaturitas2009644819709826
- ColemanREBodyJJGralowJRLiptonABone loss in patients with breast cancer receiving aromatase inhibitors and associated treatment strategiesCancer Treat Rev200834Suppl 1S31S4218486346
- BundredNJCampbellIDDavidsonNEffective inhibition of aromatase inhibitor-associated bone loss by zoledronic acid in postmenopausal women with early breast cancer receiving adjuvant letrozole: ZO-FAST Study resultsCancer20081121001101018205185
- AbdulhaqHGeyerCSafety of adjuvant endocrine therapy in postmenopausal women with breast cancerAm J Clin Oncol20083159560519060594
- SaadFAdachiJDBrownJPCancer treatment-induced bone loss in breast and prostate cancerJ Clin Oncol2008265465547618955443
- ChapurlatRDBauerDCCummingsSRAssociation between endogenous hormones and sex hormone-binding globulin and bone turnover in older women: study of osteoporotic fracturesBone20012938138711595622
- GarneroPSornay-RenduEClaustratBDelmasPDBiochemical markers of bone turnover, endogenous hormones and the risk of fractures in postmenopausal women: the OFELY studyJ Bone Miner Res2000151526153610934651
- RogersASalehGHannonRAGreenfieldDEastellRCirculating estradiol and osteoprotegerin as determinants of bone turnover and bone density in postmenopausal womenJ Clin Endocrinol Metab2002874470447512364420
- EttingerBPressmanASklarinPBauerDCCauleyJACummingsSRAssociations between low levels of serum estradiol, bone density, and fractures among elderly women: the study of osteoporotic fracturesJ Clin Endocrinol Metab199883223922439661589
- CummingsSRBrownerWSBauerDEndogenous hormones and the risk of hip and vertebral fractures among older women. Study of Osteoporotic Fractures Research GroupN Engl J Med19983397337389731089
- ChapurlatRDGarneroPBreartGMeunierPJDelmasPDSerum estradiol and sex hormone-binding globulin and the risk of hip fracture in elderly women: the EPIDOS studyJ Bone Miner Res2000151835184110977003
- PerezEASafety profiles of tamoxifen and the aromatase inhibitors in adjuvant therapy of hormone-responsive early breast cancerAnn Oncol200718Suppl 8viii26viii3517890211
- EastellRHannonRACuzickJEffect of an aromatase inhibitor on BMD and bone turnover markers: 2-year results of the Anastrozole, Tamoxifen, Alone or in Combination (ATAC) trial (182332030)J Bone Miner Res2006211215122316869719
- BerryJAre all aromatase inhibitors the same? A review of controlled clinical trials in breast cancerClin Ther2005271671168416368441
- RabaglioMSunZPriceKNBone fractures among postmenopausal patients with endocrine-responsive early breast cancer treated with 5 years of letrozole or tamoxifen in the BIG 1-98 trialAnn Oncol2009201489149819474112
- ColemanREBanksLMGirgisSISkeletal effects of exemestane on bone-mineral density, bone biomarkers, and fracture incidence in postmenopausal women with early breast cancer participating in the Intergroup Exemestane Study (IES): a randomized controlled studyLancet Oncol2007811912717267326
- HadjiPZillerMKiebackDGThe effect of exemestane or tamoxifen on markers of bone turnover: results of a German sub-study of the Tamoxifen Exemestane Adjuvant Multicentre (TEAM) trialBreast20091815916419364653
- PantSShapiroCLAromatase inhibitor-associated bone loss: clinical considerationsDrugs2008682591260019093701
- YamamotoYIwaseHSafety profiles of aromatase inhibitors and selective estrogen-receptor modulators in the treatment of early breast cancerInt J Clin Oncol20081338439418946748
- HadjiPAaproMSBodyJJManagement of aromatase inhibitor-associated bone loss in postmenopausal women with breast cancer: practical guidance for prevention and treatmentAnn Oncol2011222546255521415233
- BundredNJAromatase inhibitors and bone healthCurr Opin Obstet Gynecol200921606719125005
- AaproMAbrahamssonPABodyJJGuidance on the use of bisphosphonates in solid tumours: recommendations of an international expert panelAnn Oncol20081942043217906299
- HadjiPZillerMAlbertUSKalderMAssessment of fracture risk in women with breast cancer using current vs emerging guidelinesBr J Cancer201010264565020087347
- BrufskyAMBossermanLDCaradonnaRRZoledronic acid effectively prevents aromatase inhibitor-associated bone loss in postmenopausal women with early breast cancer receiving adjuvant letrozole: Z-FAST study 36-month follow-up resultsClin Breast Cancer20099778519433387
- BrufskyAHarkerWGBeckJTThe effect of zoledronic acid on aromatase inhibitor-associated bone loss in postmenopausal women with early breast cancer receiving adjuvant letrozole: the Z-FAST study 5-year final follow upPresented at the 32nd Annual San Antonio Breast Cancer Symposium (SABCS)San Antonio, TXDecember 9–132009 Abstract 4083
- DeBoerRBundredNEidtmannHThe effect of zoledronic acid on aromatase inhibitor associated bone loss in postmenopausal women with early breast cancer receiving adjuvant letrozole: the ZO-FAST study 5-year final follow-ppPresented at the 33rd Annual San Antonio Breast Cancer Symposium (SABCS)San Antonio, TXDecember 8–122010 Abstract P5-11-01
- ColemanRGnantMNew results from the use of bisphosphonates in cancer patientsCurr Opin Support Palliat Care2009321321819561507
- JohnstonSRDowsettMAromatase inhibitors for breast cancer: lessons from the laboratoryNat Rev Cancer2003382183114668813
- GnantMClézardinPDirect and indirect anticancer activity of bisphosphonates: a brief review of published literatureCancer Treat Rev10 72011 [Epub ahead of print.]
- GnantMEidtmannHThe anti-tumour effect of bisphosphonates ABCSG-12, ZO-FAST and more…Crit Rev Oncol Hematol201074Suppl 1S2S620427029
- CartenìGBordonaroRGiottaFEfficacy and safety of zoledronic acid in patients with breast cancer metastatic to bone: a multicenter clinical trialOncologist20061184184816880243
- AbrahamJZoledronic acid improves disease-free survival in hormone-responsive early breast cancerCommunity Oncol200961113
- ColemanREMarshallHCameronDAZURE InvestigatorsBreast-cancer adjuvant therapy with zoledronic acidN Engl J Med20113651396140521995387
- ColemanRBundredNde BoerRImpact of zoledronic acid in postmenopausal women with early breast cancer receiving adjuvant letrozole: Z-FAST, ZO-FAST, and E-ZO-FASTPresented at the 32nd Annual San Antonio Breast Cancer Symposium (SABCS)San Antonio, TXDecember 9–132009 Abstract 4082
- HinesSLSloanJAAthertonPJZoledronic acid for treatment of osteopenia and osteoporosis in women with primary breast cancer undergoing adjuvant aromatase inhibitor therapyBreast201019929620079640
- NievesJWBarrett-ConnorESirisESCalcium and vitamin D intake influence bone mass, but not short-term fracture risk, in Caucasian postmenopausal women from the National Osteoporosis Risk Assessment (NORA) studyOsteoporosis Int200819673679
- BoonenSLipsPBouillonRBischoff-FerrariHAVanderschuerenDHaentjensPNeed for additional calcium to reduce the risk of hip fracture with vitamin D supplementation: evidence from a comparative metaanalysis of randomized controlled trialsJ Clin Endocrinol Metabol20079214151423
- JacksonRDLaCroixAZGassMCalcium plus vitamin D supplementation and the risk of fracturesN Engl J Med200635466968316481635 Erratum in:N Engl J Med20093541102
- KemmlerWEngelkeKvon StengelSWeineckJLauberDKalenderWALong-term four-year exercise has a positive effect on menopausal risk factors: the Erlangen Fitness Osteoporosis Prevention StudyJ Strength Cond Res20072123223917313298
- LipsPBouillonRvan SchoorNMReducing fracture risk with calcium and vitamin DClin Endocrinol (Oxford)200973277285
- KanisJADiagnosis of osteoporosisOsteoporosis Int19977Suppl 3S108S116
- ShapiroCLManolaJLeboffMOvarian failure after adjuvant chemotherapy is associated with rapid bone loss in women with early-stage breast cancerJ Clin Oncol2001193306331111454877
- PowlesTJHickishTKanisJATidyAAshleySEffect of tamoxifen on bone mineral density measured by dual-energy x-ray absorptiometry in healthy premenopausal and postmenopausal womenJ Clin Oncol19961478848558225