Abstract
Adjuvant radiotherapy (RT) is an important part of breast cancer management but the dose and fractionation schedules used are variable. A total of 50 Gy in 25 daily fractions delivered over 5 weeks is often considered the “standard” adjuvant RT prescription. Hypofractionated regimes such as 42.5 Gy in 16 daily fractions or 40 Gy in 15 daily fractions following breast-conserving surgery have proven to be equally effective and achieve similar or better cosmetic and normal tissue outcomes for both invasive and in situ diseases and when treating the regional nodes. Hypofractionation is more convenient for patients and less costly. However, certain patients at higher risk of RT late effects may benefit from a less intense, even more extended fractionation schedule. This review describes the indications for whole breast hypofractionated adjuvant RT for patients with breast cancer following breast-conserving surgery and proposes that hypofractionation should be the new “standard” for adjuvant breast cancer RT.
Introduction
Adjuvant treatment of breast cancer is one of the most common indications for radiotherapy (RT) in western countries due to the high incidence of breast cancer and the multiple indications for RT in this disease.Citation1–Citation3 The meta-analyses of RT by Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) and surgery for early stage breast cancer have shown that breast-conserving surgery (BCS) followed by whole breast RT is equivalent to mastectomy and that BCS + RT is superior to BCS alone in terms of local control and survival.Citation4,Citation5 In randomized trials, the relative risk reductions from RT after BCS were independent of the dose/fractionation used. However, “standard” post-BCS fractionation has come to mean 5–6 weeks of daily treatments of 1.8–2 Gy/d, with or without a boost.Citation1,Citation6–Citation8 This is in part because 50 Gy in 25 daily fractions to the whole breast was used in the earliest published randomized trials that validated the use of BCS + RT.Citation9,Citation10
Over the past two decades, evidence has been accumulated from well-conducted, large, prospective randomized trials, comparing shorter RT courses to 50 Gy in 25 daily fractions.Citation11–Citation13 These trials and institutional series have confirmed that shorter courses of RT are equally effective compared to longer RT schedules for women with invasiveCitation11–Citation16 or in situ breast cancer,Citation17–Citation20 provided the total dose of RT is appropriately reduced. Shorter RT courses also result in improved quality of life,Citation21 convenience, and lower treatment delivery resource requirements. This has led to the suggestion that short fractionation should be the new standard following BCS for early stage breast cancer.Citation22
Whole breast RT schedules using 15–16 daily treatments following BCS have become widely accepted in parts of Canada and the UK. In Canada, 75%–85% of patientsCitation22–Citation24 and in the UK, 91% of patients in 2014 (I Locke, Lead for Clinical Oncology, Royal Marsden Hospital, UK, personal communication, April 29, 2015) receiving whole breast RT after BCS were treated with short fractionation but it has been adopted more slowly in the USA.Citation25–Citation27 This review discusses the safety and efficacy of short fractionation as compared to longer courses of adjuvant RT following BCS for invasive or in situ breast cancer and for locoregional RT for patients with node-positive disease following BCS or mastectomy. The role of accelerated partial breast irradiation is not addressed.
Hypofractionated RT following BCS is safe and effective
summarizes the long-term outcomes of four carefully conducted, randomized trials, involving 7,095 patients, which compared 13–16 fraction RT regimes to a 25-fraction schedule.Citation11–Citation13 With >10-year follow-up, the overall conclusion from the Standardization of Breast Radiotherapy (START) A trialCitation13 and the Canadian trialCitation12 was that 39 Gy in 13 daily fractions over 5 weeksCitation13 and 42.5 Gy in 16 daily fractions over 3.5 weeksCitation12 provided equivalent local control, survival, cosmetic outcome, and normal tissue toxicity compared to 50 Gy in 25 daily fractions. In contrast, 41.6 Gy in 13 daily fractions delivered over 5 weeks was somewhat more intense and 40 Gy in 15 daily fractions delivered over 3 weeks was somewhat less intense in terms of normal tissue toxicity.Citation13 Furthermore, patients randomized to 40 Gy in 15 daily fractions had significantly fewer locoregional recurrences and deaths compared to patients treated with 50 Gy in 25 daily fractions.Citation13 The biological effects of various RT schedules can be estimated using a linear quadratic formula based on the dose delivered each day, the number of treatments, the interval over which the treatment was delivered, and a tissue end point-specific constant called the α/β ratio.Citation28 The α/β ratios are lower for slowly responding tissues, including late fibrosis effects in normal tissues, whereas α/β ratios are higher for more rapidly proliferating tissues, including many, but not all, tumors. Two approaches to estimate the equivalence of different RT schedules have been proposed, the relative biological effective dose (BED) model and the equivalent dose at 2 Gy per fraction (EQD2) model.Citation28
Table 1 Characteristics and outcomes of randomized hypofractionation trials
and present the BEDs and the EQD2s, respectively, for adjuvant breast RT regimens across several estimates of the α/β ratio. At α/β=2, BED and EQD2 values are equivalent for regimens that have been demonstrated in randomized trials to have clinically equivalent normal tissue effects. For example, 42.5 Gy in 16 daily fractions and 50 Gy in 25 daily fractions have been shown to be clinically equivalent.Citation12 For those regimens, using α/β=2, the BEDs are 99 Gy and 100 Gy, and EQD2s are 49.5 Gy and 50 Gy, respectively. Previously, it has been assumed or calculated that normal tissue effects in the breast respond according to an α/β ratio of 3.4.Citation13,Citation29 However, there is greater discrepancy in the BED and EQD2 values when the earlier regimes are compared, assuming an α/β ratio of 3.4 or higher ( and ).
Table 2 BED of different hypofractionated regimes compared to standard at different α/β (time factor not included)
Concerns that hypofractionation may increase fibrosis and worsen cosmetic outcomes have limited its adoption. In the CanadianCitation12 and START trials,Citation13 normal tissue effects were not worse when compared to 50 Gy in 25 daily fractions. However, in the Randomized Trial of Accelerated Partial Breast Irradiation (RAPID) trial, 38.5 Gy in 10 fractions BID accelerated partial breast RT resulted in greater cosmetic deterioration.Citation30,Citation31 The excess adverse fibrosis and cosmetic effects may be explained by the BEDs and EQD2s of 38.5 Gy in 10 daily fractions which are 112.6 Gy and 56.3 Gy, respectively, compared to 100 Gy and 50 Gy, respectively, for 50 Gy in 25 daily fractions ( and ). The biological effect may have been even more intense due to the BID treatment used in the RAPID trial.Citation31 The radiobiological explanations for varying normal tissue and tumor responses to alterations in dose fractionation are an area of ongoing research.Citation32
Table 3 EQD2 of reported hypofractionation regimes compared to standard at different α/β
The long-term safety of short RT fractionation has been investigated using health service administrative data. Examining outcomes across many thousands of patients, it has been observed that adjuvant breast RT is associated with a small but statistically significant increased risk of cerebrovascular and cardiac hospitalizations or deaths,Citation33–Citation36 and second malignacies,Citation37 but that these risks were not higher among patients treated with hypofractionation (>2 Gy/d) as compared to ≤2 Gy/d RT schedules. One report suggested that severe hypofractionation (43 Gy in 10 daily fractions) may increase the risk of cardiac injury.Citation36 However, in the START A and B trials, the rate of confirmed ischemic heart disease in patients with left-sided breast cancer was not different between short and longer fractionation, although follow-up at 10 years, somewhat early for this end point.Citation13 To avoid cardiac injury, every effort should be made to exclude the heart from the therapeutic beam, no matter what fractionation is used.
There are limited data on the use of even shorter, four or five fraction RT regimens following BCS. A small trial from France reported comparable toxicity from 23 Gy in 4 daily fractions over 3 weeks and 45 Gy in 25 daily fractions over 5 weeks.Citation38 In the UK, regimens of whole breast RT, using 27 Gy in 5 daily fractions or 30 Gy in 5 daily fractions both delivered once per week over 5 weeks, were compared to 50 Gy in 25 daily fractions.Citation39 More acute normal tissue side effects were observed with 30 Gy in 5 daily fractions,Citation39 but 27 Gy in 5 daily fractions was tolerable and is being compared to 40 Gy in 15 daily fractions in a randomized trial.Citation40 An early report suggested that 27 Gy in 5 daily fractions results in low rates of acute skin reactions.Citation41
Providing whole breast RT in 15–16 treatment sessions is more convenient and preferred by patients compared to RT extending over 5–7 weeks and has been associated with more prompt recovery and improved quality of life compared to longer RT courses.Citation21 Shorter RT schedules significantly reduce resource utilization. Three patients can be treated with the same treatment delivery resources using hypofractionation (45–48 treatment visits for three patients) as would be used for two patients using a 25-fraction regimen (50 treatment visits for two patients). Shorter RT courses are beneficial to the capacity and sustainability of the health care system.Citation27 Several organizations have adopted short fractionation as preferred,Citation1 recommended,Citation2,Citation27 standard,Citation3 or acceptableCitation8 approach for whole breast RT following BCS. The Choosing Wisely campaign in the USA advocates: “Don’t initiate whole breast radiotherapy as a part of breast conservation therapy in women age ≥50 with early stage invasive breast cancer without considering shorter treatment schedules”.Citation42 This approach is entirely justified and is likely too conservative because it introduces caveats to restrict the use of shorter fractionation based on age, stage, and disease behavior. Such caveats are not evidence based as discussed in the following sections.
Hypofractionation appears to be equally effective in patients with breast ductal carcinoma in situ
Many patients with ductal carcinoma in situ (DCIS) are treated with BCS and whole breast RT. A number of institutions have reported that shorter RT schedules, generally 42.5 Gy in 16 daily fractions, achieved equivalent local control compared to longer fractionation.Citation17–Citation20 A meta-analysis of observational series found no difference in local recurrence rates between hypofractionated and 5-week or longer RT courses.Citation20 The efficacy and safety of hypofractionated RT for patients with DCIS are addressed in an Australian-led, randomized trial that accrued 1,608 patients.Citation43 However, there is no inherent reason that normal tissue side effects should be different following whole breast RT for patients with excised DCIS as compared to excised invasive cancer. A short RT schedule of 40 Gy in 15 daily fractions or 42.5 Gy in 16 daily fractions should be offered as an option to patients with DCIS.
Hypofractionation is effective for higher risk patients
An unplanned subset analysis within the Canadian hypofractionation trial suggested that patients with grade 3 histology had an increased risk of local recurrence when treated with 42.5 Gy in 16 daily fractions.Citation12 However, in the larger START trials, hypofractionation among patients with grade 3 histology was not associated with a higher risk of local recurrence.Citation13,Citation44 Furthermore, a comparative effectiveness evaluation of 1,335 patients with grade 3 histology treated with BCS and whole breast RT in British Columbia between 1989 and 1999, 81% of whom received short fractionation, showed identical local control and survival among patients treated with hypofractionated RT as compared to longer RT courses.Citation14 Short fractionation for whole breast RT should not be restricted to patients with lower grade histology, or by extension, other markers of an increased risk of local or distant relapse. The American Society for Radiation Oncology consensus statement that supports the use of shorter fractionation following BCS for women aged 50 and older with T1-2, pN0 breast cancer not receiving chemotherapy, is likely, overly cautious.Citation8
What boost dose should be used with hypofractionated whole breast RT?
Trials from the European Organization for Research and Treatment of Cancer (EORTC)Citation45 and Lyon, FranceCitation46 showed that a boost dose of RT directed to the primary site significantly improved local control compared to whole breast RT alone following BCS. The EORTC trial used 16 Gy in 8 daily fractions, whereas the French trial used 10 Gy in 5 daily fractions. The absolute differences in local recurrence varied between the trials and among subgroups with different pretreatment risks of local recurrence, but the relative risk reductions in the trials were overlapping.Citation45,Citation46
Common indications for a boost dose include close or focally positive margins and younger age.Citation1–Citation3,Citation7 It seems logical, if treating the whole breast in 15–16 treatments, to also use a shorter boost treatment of 10 Gy in 4–5 daily fractions rather than extending the treatment course by 50% to deliver 16 Gy in 8 daily fractions. We have found that a boost dose of 10 Gy in 4 daily fractions is tolerable (minimal fibrosis, pain, telangiectasia, or decrease in cosmesis) when delivered using a multibeam photon technique or a direct electron field restricted to 6–12 MeV energy and field sizes smaller than 8×8 cm2. Other researches have confirmed this observation.Citation47 We therefore recommend and use 10 Gy in 4 daily fractions if a patient has an indication for a primary site boost and is receiving 42.5 Gy in 16 daily fractions for whole breast RT following BCS.
Which patients should not have hypofractionation after BCS?
Even in jurisdictions where short fractionation for whole breast RT is commonly used, it is not recommended or used for all patients.Citation3,Citation23,Citation24 The primary concern with hypofractionation is that the larger dose per day may induce greater fibrosis or late normal tissue effects. A higher risk of late fibrosis after standard breast RT occurs with greater dose inhomogeneity,Citation28,Citation31,Citation48–Citation51 among current smokers,Citation31,Citation52 with implant reconstruction,Citation53,Citation54 or after postoperative infections.Citation31,Citation48,Citation50 The potential impact of dose inhomogeneities (areas of dose >107%) may be particularly severe with short fractionation.Citation28,Citation54 In addition, patients with significant postoperative breast edema have considerable amounts of protein-rich interstitial fluid in their breast. As that edema fluid resolves it leaves collagen behind and this translates to greater fibrosis over time.
Since 50 Gy in 25 daily fractions produces equivalent late fibrosis and cosmetic deterioration, it is not rational to use this fractionation for patients with an increased risk of later toxicity. A dose/fractionation that is biologically less intense for the whole breast such as 45 Gy in 25 daily fractions at 1.8 Gy/d should be utilized (). However, that lower dose may be insufficient to achieve optimal local control on its own so, a boost dose to the primary site in all patients needs to be added.Citation3,Citation6,Citation7,Citation55,Citation56
We therefore recommend 42.5 Gy in 16 daily fractions (or 40 Gy in 15 daily fractions) for most patients following BCS. If the patient has an indication for a boost, then 10 Gy in 4 daily fractions should be used. If the patient has a higher than average risk of late toxicity due to the factors listed above, 45 Gy in 25 daily fractions plus a boost of 10 Gy in 5 daily fractions is recommended. If the patient has predictors of a greater risk of late toxicity, plus an indication for a boost such as close margins or young age, the boost dose should be increased to 16 Gy in 8 daily fractions or 20 Gy in 10 daily fractions ().
Figure 1 Recommended breast dose/fractionation prescribing algorithm for patients treated with breast-conserving surgery and whole breast radiation therapy.
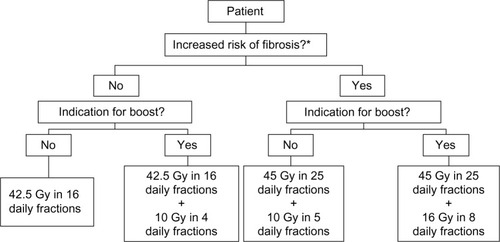
Table 4 BED and EQD2 of different fractionation used in regional nodal radiation compared to standard
Hypofractionation can be used for regional nodal RT after BCS or mastectomy
Institutions where short fractionation for whole breast RT is commonly used also use short fractionation when the regional nodes are part of the target volume.Citation3 There could be two concerns with such an approach: 1) short fractionation may be inadequate to achieve control in the regional nodes or 2) short fractionation may cause more pulmonary fibrosis, brachial plexopathy, or vessel injury, leading to cerebrovascular or cardiac morbidity.
Regarding efficacy, the British Columbia randomized trial of postmastectomy RT (PMRT) used a 16-fraction treatment schedule. This trial randomly allocated 318 premenopausal women with node-positive breast cancer treated with modified radical mastectomy, to full locoregional RT including the chest wall, axilla, supraclavicular fossa and a direct field over the internal mammary nodes, or no adjuvant RT.Citation57 Patients were treated from 1978 to 1986 and 20-year follow-up was reported in 2005.Citation58 Patients received a chest wall dose of 37.5 Gy in 16 daily fractions and the mid-axilla received 35 Gy in 16 daily fractions. These dose/fractionation schedules are biologically, substantially less intense compared to 45–50 Gy in 25 daily fractions (). In spite of this, the PMRT used in the British Columbia trial achieved similar reductions in the risk of locoregional recurrence, distant metastases, and death compared to the concurrently reported Danish trials that used a more conventional dose, 50 Gy in 25 daily fractions.Citation59,Citation60 These data demonstrate that a hypofractionated RT schedule is sufficient to achieve cancer control end points.
For many decades, the British Columbia Cancer Agency has used a PMRT prescription of 40 Gy in 16 daily fractions through a tangent pair with 0.5 cm bolus to the chest wall and dose of 37.5 Gy in 16 daily fractions to the mid-axilla.Citation4,Citation33–Citation35,Citation61 These doses are 7% higher than the doses shown to be effective in their randomized PMRT trial and are biologically less intense than 50 Gy in 25 daily fractions (). This PMRT prescription has also been used by others.Citation15 When combining regional RT with hypofractionated whole breast RT following BCS, the same nodal dose of 37.5 Gy in 16 daily fractions can be used.Citation3
Regarding safety, Powell et al reported that a higher dose/day fractionation schedule increased the brachial plexopathy rate from 1% to 6%.Citation62 This was based on a retrospective comparison of 45 Gy/15 fr and 54 Gy/30 fr, both delivered over 6 weeks. The 45 Gy/15 fr schedule has a much higher BED and EQD2 compared to 37.5 Gy/16 fr or 50 Gy/25 fr using a ratio of α/β=1 or α/β=2 (), which are commonly attributed to the brachial plexus.Citation63 Among patients treated in the START trials, 8%–14% of patients had nodal RT and no differences were noted in arm or shoulder function between the shorter and longer RT prescriptions.Citation13 A single case of brachial plexopathy (<0.1% of cases) was reported with the use of 41.6 Gy/13 fr in the START A trial.Citation13 Adjuvant RT irrespective of dose per fraction results in a small but statistically significant increase in cardiac and cerebrovascular toxicity as compared to no RT but is not increased with hypofractionation.Citation33–Citation36 Short fractionation for PMRT and for the regional nodal RT component after BCS is safe, provided the total dose is reduced sufficiently to avoid late normal tissue effects. Short fractionation does not compromise locoregional control.Citation58,Citation63
Summary
Two decades of observations from randomized trials and institutional series have demonstrated that following BCS, whole breast doses of 40 Gy/15 fr or 42.5 Gy/16 fr are as safe and effective as 50 Gy/25 fr. Evidence has been obtained from randomized trials and institutional series that hypofractionation is also effective and safe for adjuvant treatment of the regional lymph nodes. A shorter RT course should be the new standard and offered to most women because it is more convenient and cost-effective. However, short fractionation is not appropriate for all patients. Patients with postoperative complications, those with large breasts for whom a maximum dose of <107% is not achievable, or patients with implants for augmentation or reconstruction, have an increased risk for late fibrosis or cosmetic deterioration following RT. They should receive a whole breast or chest wall dose that is biologically less intense. For such patients, we recommend 45 Gy/25 fr to the whole breast and a primary site boost of at least 10 Gy/5 fr to achieve an equivalent antineoplastic effect at the primary site. For all others, a 15–16 treatment prescription is safe, effective, and recommended.
Disclosure
All authors declare that this is an original work and has not been submitted elsewhere for publication, and they report no conflicts of interest in this work.
References
- NCCN Clinical Practice Guidelines in Oncology: Breast Cancer, Version 2.2015National Comprehensive Cancer Network Available from: http://www.nccn.org/professionals/physician_gls/pdf/breast.pdfAccessed May 3, 2015
- NICE Clinical Guideline 80. National Institute for Health and Care Excellence2009 Available from: http://pathways.nice.org.uk/pathways/early-and-locally-advanced-breast-cancer#path=view%3A/pathways/early-and-locally-advanced-breast-cancer/early-and-locally-advanced-breast-cancer-adjuvant-therapy.xml&content=view-node%3Anodes-radiotherapyAccessed May 3, 2015
- BCCA Clinical Management Guidelines: Breast Cancer; Stage I and II Invasive Breast Cancer RT section2013 Available from: http://www.bccacncer.bc.ca/health-professionals/professional-recources/cancer-management-guidelines/breast/breast#ManagementAccessed May 3, 2015
- ClarkeMCollinsRDarbySEarly Breast Cancer Trialists’ Collaborative Group (EBCTCG)Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trialsLancet20053662087210616360786
- Early Breast Cancer Trialists’ Collaborative Group (EBCTCG)DarbySMcGalePEffect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trialsLancet20113781707171622019144
- MorrowMStromEABassettLWAmerican College of Radiology; American College of SurgeonsSociety of Surgical OncologyCollege of American PathologyStandard for breastconservation therapy in the management of invasive breast carcinomaCA Cancer J Clin20025227730012363326
- WhiteJRHalbergFERabinovitchRAmerican College of Radiology appropriateness criteria on conservative surgery and radiation: stages I and II breast carcinomaJ Am CollRadiol20085701713
- SmithBDBentzenSMCorreaCRFractionation for whole breast irradiation: an American Society for Radiation Oncology (ASTRO) evidence-based guidelineInt J Radiat Oncol Biol Phys201181596820638191
- VeronesiUSaccozziRDel VecchioMComparing radical mastectomy with quadrantectomy, axillary dissection, and radiotherapy in patients with small cancers of the breastN Engl J Med19813056117015141
- FisherBBauerMMargoleseRFive-year results of a randomized clinical trial comparing total mastectomy and segmental mastectomy with or without radiation in the treatment of breast cancerN Engl J Med19853126656733883167
- OwenJRAshtonABlissJMEffect of radiotherapy fraction size on tumour control in patients with early-stage breast cancer after local tumour excision: long-term results of a randomised trialLancet Oncol2006746747116750496
- WhelanTJPignolJPLevineMNLong-term results of hypofractionated radiation therapy for breast cancerN Engl J Med201036251352020147717
- HavilandJSOwenJRDewarJASTART Trialists’ GroupThe UK Standardisation of breast radiotherapy (START) trials of radiotherapy hypofractionation for treatment of early breast cancer: 10-year follow-up results of two randomised controlled trialsLancet Oncol2013141086109424055415
- HerbertCNicholAOlivottoIThe impact of hypofractionated whole breast radiotherapy on local relapse in patients with Grade 3 early breast cancer: a population-based cohort studyInt J Radiat OncolBiol Phys20128220862092
- KoDHNorrissAHarringtonCRRobinsonBAJamesMLHypofractionated radiation treatment following mastectomy in early breast cancer: the Christchurch experienceJ Med Imaging Radiat Oncol20155924324725287654
- ShelleyWBrundageMHayterCPaszatLZhouSMackillopWA shorter fractionation schedule for postlumpectomybreast cancer patientsInt J Radiat OncolBiol Phys20004712191228
- WaiESLesperanceMLAlexanderCSEffect of radiotherapy boost and hypofractionation on outcomes in ductal carcinoma in situCancer2011117546220803608
- LalaniNPaszatLSutradharRLong-term outcomes of hypofractionation versus conventional radiation therapy after breast-conserving surgery for ductal carcinoma in situ of the breastInt J Radiat OncolBiol Phys20149010171024
- HathoutLHijalTThébergeVHypofractionated radiation therapy for breast ductal carcinoma in situInt J Radiat OncolBiol Phys20138710581063
- NilssonCValachisAThe role of boost and hypofractionation as adjuvant radiotherapy in patients with DCIS: a meta-analysis of observational studiesRadiother Oncol2015114505525596912
- VersmessenHVinh-HungVVan ParijsHHealth-related quality of life in survivors of stage I-II breast cancer: randomized trial of post-operative conventional radiotherapy and hypofractionatedtomotherapyBMC Cancer20121249523098579
- HollowayCPanet-RaymondVOlivottoIAHypofractionation should be the new ‘standard’ for radiation therapy after breast conserving surgeryBreast20101916316720511064
- AshworthAKongWWhelanTMackillopWJA population-based study of the fractionation of post-lumpectomy breast radiation therapyInt J Radiat Oncol Biol Phys201386515723433799
- BerrangTSTruongPTTyldesleySOlivottoIAA population-based study of the fractionation of post-lumpectomy breast radiation therapy. In regard to Ashworth et alInt J Radiat Oncol Biol Phys20138763263324138908
- JagsiRFalchookADHendrixLHCurryHChenRCAdoption of hypofractionated radiation therapy for breast cancer after publication of randomized trialsInt J Radiat Oncol Biol Phys2014901001100925539365
- WangEHMougalianSSSoulosPRAdoption of hypofractionated whole-breast irradiation for early-stage breast cancer: a National Cancer Data Base analysisInt J Radiat Oncol Biol Phys201490993100025149661
- RajogopalanMSFlickingerJCHeronDEBeriwalSChanging practice patterns for breast cancer radiation therapy with clinical pathways: an analysis of hypofractionation in a large, integrated cancer centre networkPract Radiat Oncol20155636925748004
- JonesBDaleRGDeehanCHopkinsKIMorganDALThe role of biologically effective dose (BED) in clinical oncologyClin Oncol2001137181
- YarnoldJAshtonABlissJFractionation sensitivity and dose response of late adverse effects in the breast after radiotherapy for early breast cancer: long-term results of a randomised trialRadiother Oncol20057591715878095
- OlivottoIAWhelanTJParpiaSInterim cosmetic and toxicity results from RAPID: a randomized trial of accelerated partial breast irradiation using three-dimensional conformal external beam radiation therapyJ Clin Oncol2013314038404523835717
- PetersonDTruongPTParpiaSRAPID Trial InvestigatorsPredictors of adverse cosmetic outcome in the RAPID Trial: an exploratory analysisInt J Radiat Oncol Biol Phys20159196897625832689
- SomaiahNRothkammKYarnoldJWhere do we look for markers of radiotherapy fraction size sensitivity?Clin Oncol Epub2015621
- StokesELTyldesleySWoodsRWaiEOlivottoIAEffect of nodal irradiation and fraction size on cardiac and cerebrovascular mortality in women with breast cancer treated with local and loco-regional radiotherapyInt J Radiat Oncol Biol Phys20118040340920584587
- ChanEKWoodsRMcBrideMLAdjuvant hypo-fractionated versus conventional whole breast radiation therapy for early-stage breast cancer: long-term hospital-related morbidity from cardiac causesInt J Radiat Oncol Biol Phys20148878679224606848
- ChanEKWoodsRViraniSLong-term mortality from cardiac causes after adjuvant hypo-fractionated vs. conventional radiotherapy for localized left-sided breast cancerRadiother Oncol2015114737825227961
- TjessemKHJohansenSMalinenELong-term cardiac mortality after hypofractionated radiation therapy in breast cancerInt J Radiat Oncol Biol Phys20138733734323886416
- HamiltonSNTyldesleySLiDOlsonRMcBrideMSecond malignancies after adjuvant radiation therapy for early stage breast cancer: is there increased risk with addition of regional radiation to local radiation?Int J Radiat Oncol Biol Phys20159197798525832690
- BailletFHoussetMMaylinCThe use of a specific hypofractionated radiation therapy regimen versus classical fractionation in the treatment of breast cancer: a randomized study of 230 patientsInt J Radiat Oncol Biol Phys199019113111332254102
- FAST TRIALISTS GroupAgrawalRKAlhassoAFirst results of the randomised UK FAST Trial of radiotherapy hypofractionation for treatment of early breast cancer (CRUKE/04/015)Radiother Oncol20111009310021752481
- The Institute for Cancer Research, clinical trialsFAST-Forward2015 Available from: http://www.icr.ac.uk/our-research/our-research-centres/clinical-trials-and-statistics-unit/clinical-trials/fast_forward_pageAccessed April 25, 2015
- BruntAMYarnoldJWheatleyDAcute skin toxicity reported in the FAST-forward trial (HTA 09/01/47): a phase III randomized trial of 1-week whole breast radiotherapy compared to standard 3 weeks in patients with early breast cancerProceedings of the 10th National Cancer Research ConferenceNovember 2–5 2014Liverpool, UK
- American Society for Radiation OncologyChoose Wisely2013 Available from: http://www.choosingwisely.org/clinician-lists/american-society-radiation-oncology-whole-breast-radiotherapy/Accessed April 23, 2015
- Trans-Tasman Radiation Oncology Group (TROG)Radiation Doses and Fractionation Schedules in Non-Low Risk Ductal Carcinoma In Situ (DCIS) of the Breast Available from: https://clinicaltrials.gov/ct2/show/NCT00470236?term=ductal+carcinoma+in+situ&rank=24Accessed April 23, 2015 ClinicalTrials.gov identifier: NCT00470236
- HavilandJSYarnoldJRBentzenSMHypofractionated radiotherapy for breast cancerN Engl J Med2010362184320463347
- BartelinkHMaingonPPoortmansPEuropean Organisation for Research and Treatment of Cancer Radiation Oncology and Breast Cancer GroupsWhole-breast irradiation with or without a boost for patients treated with breast-conserving surgery for early breast cancer: 20-year follow-up of a randomised phase 3 trialLancet Oncol201516475625500422
- RomestaingPLehingueYCarrieCRole of a 10-Gy boost in the conservative treatment of early breast cancer: results of a randomized clinical trial in Lyon, FranceJ Clin Oncol1997159639689060534
- ChanEKTabarsiNTyldesleySPatient-reported long-term cosmetic outcomes following short fractionation whole breast radiotherapy with boostAm J Clin Oncol Epub2014
- VrielingCColletteLFourquetAThe influence of patient, tumor and treatment factors on the cosmetic results after breast-conserving therapy in the EORTC ‘boost vs no boost’ trial. EORTC Radiotherapy and Breast Cancer Cooperative GroupsRadiother Oncol20005521923210869738
- Van LimbergenERijndersAvan der SchuerenELerutTChristiaensRCosmetic evaluation of breast conserving treatment for mammary cancer. 2. A quantitative analysis of the influence of radiation dose, fractionation schedules and surgical treatment techniques on cosmetic resultsRadiother Oncol1989162532672616812
- BarnettGCWilkinsonJSMoodyAMThe Cambridge breast intensity-modulated radiotherapy trial: patient- and treatment-related factors that influence late toxicityClin Oncol201123662673
- CiammellaPPodgorniiAGaleandroMToxicity and cosmetic outcome of hypofractionated whole-breast radiotherapy: predictive clinical and dosimetric factorsRadiat Oncol201499724762173
- HoALBovillESMacadamSATyldesleySGiangJLennoxPAPostmastectomy radiation therapy after immediate two-stage tissue expander/implant breast reconstruction: a University of British Columbia perspectivePlast Reconstr Surg20141341e10e24622575
- SbitanyHWangFPeledAWImmediate implant-based breast reconstruction following total skin-sparing mastectomy: defining the risk of preoperative and postoperative radiation therapy for surgical outcomesPlast Reconstr Surg201413439640425158699
- YarnoldJBentzenSMColesCHavilandJHypofractionated whole-breast radiotherapy for women with early breast cancer: myths and realitiesInt J Radiat Oncol Biol Phys2011791920950960
- RoseMAOlivottoICadyBConservative surgery and radiation therapy for early breast cancer. Long-term cosmetic resultsArch Surg19891241531572916935
- ZissiadisYLanglandsAOBarracloughBBoyagesJBreastconservation: long-term results from Westmead HospitalAust N Z J Surg1997673133199193262
- RagazJJacksonSMLeNAdjuvant radiotherapy and chemotherapy in node-positive premenopausal women with breast cancerN Engl J Med19973379569629309100
- RagazJOlivottoIASpinelliJJLocoregional radiation therapy in patients with high-risk breast cancer receiving adjuvant chemotherapy: 20-year results of the British Columbia randomized trialJ Natl Cancer Inst20059711612615657341
- OvergaardMHansenPSOvergaardJPostoperative radiotherapy in high-risk premenopausal women with breast cancer who receive adjuvant chemotherapy. Danish Breast Cancer Cooperative Group 82b TrialN Engl J Med19973379499559395428
- OvergaardMJensenMBOvergaardJPostoperative radiotherapy in high-risk postmenopausal breast-cancer patients given adjuvant tamoxifen: Danish Breast Cancer Cooperative Group DBCG 82c randomised trialLancet19993531641164810335782
- WaiESLesperanceMSpeersCHIncreased use of regional radiotherapy is associated with improved outcome in a population-based cohort of women with breast cancer with 1–3 positive nodesRadiother Oncol20109730130620826030
- PowellSCookeJParsonsCRadiation-induced brachial plexus injury: follow-up of two different fractionation schedulesRadiother Oncol1990182132202217869
- BadiyanSNShahCArthurDHypofractionated regional nodal irradiation for breast cancer: examining the data and potential for future studiesRadiother Oncol2014110394424440047
