Abstract
Hair loss is a very common complaint. Patients may describe increased shedding and diffuse or localized alopecia. The differential diagnosis of hair loss includes a number of disorders causing cicatricial or noncicatricial alopecias. This paper describes the clinical approaches and diagnostic tests that are useful in the evaluation of patients presenting with alopecia. It also reviews treatments for noncicatricial alopecias, including androgenetic alopecia, alopecia areata, and telogen effluvium, as well as cicatricial alopecias, including lichen planopilaris, its clinical variant frontal fibrosing alopecia, and discoid lupus erythematosus.
Keywords:
Background
There are many resources available for the assessment of patients who present with hair loss. Evaluations can be categorized as invasive (eg, scalp biopsies), semi-invasive (eg, trichogram), or noninvasive (eg, hair counts, microscopic evaluation, trichoscopy). Each of the following approaches, when interpreted with the comprehensive clinical picture, can provide valuable insights into patient diagnosis, treatment, and monitoring.Citation1 This paper reviews the clinical approaches and diagnostic tests that are useful in the evaluation of patients presenting with alopecia. We reviewed the PubMed literature for evaluative methods and therapeutic interventions for noncicatricial alopecias, including androgenetic alopecia, alopecia areata, and telogen effluvium, and cicatricial alopecias, including lichen planopilaris, its clinical variant of frontal fibrosing alopecia, and discoid lupus erythematosus.
A careful clinical history is essential. In patients complaining of increased hair shedding, clinicians should investigate for potential triggers from the 3 months before the development of hair loss, including drug intake, systemic illness, or weight loss. Gynecologic history is very important in women, and hormonal evaluation is indicated in women with androgenetic alopecia and a history of irregular menses. Further, a family history of hair loss is characteristic in androgenetic alopecia and alopecia areata. Laboratory tests should evaluate iron and vitamin D levels and thyroid function.Citation2
Clinical evaluation should establish if hair density is normal or decreased and if the scalp shows diffuse or patchy alopecia. The severity of hair shedding should be assessed by a pull test. The pull test begins with gentle traction on a group of hairs (approximately 40–60) on three separate areas of the scalp.Citation3 The hairs extracted by this gentle traction are examined microscopically and quantified. A normal or negative pull test extracts three or fewer hairs and a positive pull test extracts six or more hairs from a single area.Citation3 Microscopically, the hair roots should be identified as being in the telogen or anagen phase and checked for dystrophy. The telogen roots, which have a club-shaped bulb and an absence of an inner root sheath, are the most commonly seen in a variety of hair disorders.Citation1 Dystrophic, broken hairs are seen in diseases that interrupt the mitotic activity of anagen follicles, including alopecia areata and systemic chemotherapy.Citation4 Anagen roots, which are darkly pigmented and triangular or delta-shaped, are typically seen in lymphocytic cicatricial alopecia.Citation4
The wash test is a valuable tool in which the patient collects hairs shed during standardized shampooing.Citation5 In one study, hair was washed and all shed hairs were counted and divided into groups of 5 cm or longer, intermediate length (3–5 cm), and 3 cm or shorter (considered telogen vellus hairs). Patients who had at least 10% telogen vellus hairs were classified as having androgenetic alopecia.Citation6 The modified wash test permits evaluation of the whole scalp. One recent study found that dystrophic, anagen hairs were present among the shed telogen hairs in patients with presumed telogen effluvium, who may in fact have alopecia areata incognita.Citation7
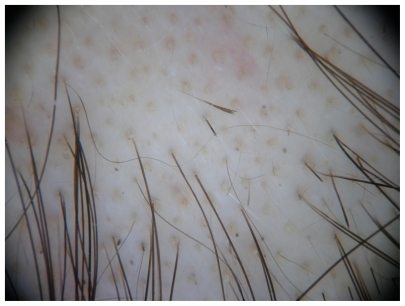
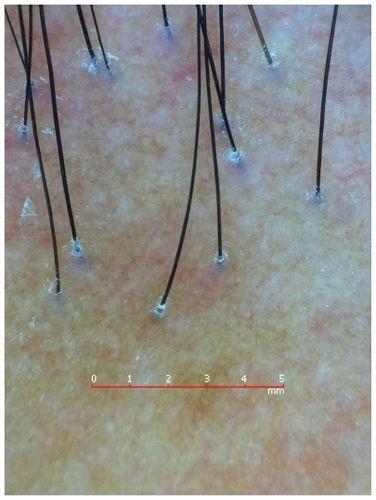
Trichoscopy, or dermoscopy and videodermoscopy of the scalp, may reveal features of a specific type of hair loss. As an example, in the case of alopecia areata, a characteristic “yellow dot” pattern is often seen, as well as micro-exclamation hairs and black cadaverized hairs or “black dots” ().Citation8,Citation9 Dermoscopy in androgenetic alopecia reveals greater than 20% diversity in the hair diameter ().Citation10 A brown, depressed halo at the follicular opening can be observed in early androgenetic alopecia and yellow dots can be seen in advanced cases. Further, a honeycomb-pigmented appearance can be appreciated in sun-exposed regions of the scalp.Citation11 Dermoscopy of active lesions of tinea capitis reveals comma hairs, which are slightly curved, fractured hair shafts.Citation9
Dermoscopy of primary and secondary cicatricial alopecia reveals decreased hair density and loss of follicular openings ().Citation11 In the case of lichen planopilaris and its clinical variant, frontal fibrosing alopecia, hyperkeratotic, perifollicular white scales with variable perifollicular erythema and peripilar white dots can be observed,Citation10 along with blue-gray dots with a target distribution around the follicle.Citation12 In the case of discoid lupus erythematosus of the scalp, mottled dyschromia, follicular plugs, telangiectasias, white central plaques, and irregularly distributed blue-gray dots in a speckled pattern between the hair follicles may be seen.Citation11 Red dots can help distinguish discoid lupus erythematosus of the scalp from lichen planopilaris. Red dots appear as erythematous, polycyclic, concentric structures, regularly distributed around the follicular opening. Citation13 In folliculitis decalvans tufted hairs and perifollicular pustules can be appreciated.Citation11
A scalp biopsy (the gold standard is a 4 mm punch biopsy) can be used for a more definitive diagnosis.Citation14 Scalp biopsies can be vertically or horizontally oriented. Vertical or longitudinal punch biopsy is appropriate for the assessment of alopecias associated with interface changes, lichenoid infiltrates, and subcutaneous pathology.Citation15 Only portions of a small number of follicular units (2–3) are seen in a given tissue section due to biopsy tangentially interrupting the characteristic angle of hair follicle growth.Citation16 Thus, only 10% of the follicles present in the specimen will be visualized. Citation17 Horizontal or transverse biopsy is best taken by a 4 mm punch biopsy 1–1.5 mm below the epidermal–dermal junction and yields follicular pathology and a quantitative approach to diagnosis.Citation16 Horizontal biopsy also allows complete evaluation of the hair follicles throughout their entire length.Citation17
Scalp biopsy is a useful tool for the evaluation of most cases of cicatricial alopecia and some cases of noncicatricial alopecia. The ideal location for biopsy depends on the presumed diagnosis. For example, in noncicatricial alopecia, a punch in the center of the lesion is appropriate; in cicatricial alopecia, the punch should be taken from areas of inflammation.Citation1
Androgenetic alopecia
Androgenetic alopecia, or patterned alopecia, is the most common form of hair loss in both men and women and is characterized by a progressive loss of hair diameter, length, and pigmentation. The genetic inheritance of androgenetic alopecia is well known, although the causative genes have yet to be elucidated. Androgenetic alopecia is often precipitated and exacerbated by conditions that can induce telogen effluvium, including drugs, acute stressors, weight loss, and partum. For example, drugs with androgenetic effects, including contraceptives containing androgenic progestins and hormonal treatments for menopause, may induce or worsen androgenetic alopecia.Citation18,Citation19 Due to the progressive nature of androgenetic alopecia, treatments should be started early and extended to maintain efficacy.
Medical treatments approved by the US Food and Drug Administration (FDA) for androgenetic alopecia include topical minoxidil 2% for women and topical minoxidil 5% and the oral type II 5-α-reductase inhibitor finasteride (1 mg/day) for men.Citation20 Many authors advocate the use of minoxidil 5% for women, but this is not approved by the FDA.Citation21 The oral type I and II 5-α-reductase inhibitor, dutasteride, is also effective at the dosage of 0.5 mg/day but is not approved for this indication.Citation22 Topical minoxidil should be applied twice daily and used for at least 12 months before making a decision regarding efficacy.Citation2
Hair transplantation, which is a surgical method of hair restoration, is an option for male and female patients over the age of 25 years with substantial hair loss. The degree and type of hair loss should be considered, because ideal candidates for hair transplantation are those with frontal and midfrontal hair loss.Citation20 Follicular unit hair transplantation is the gold standard, because it preserves the natural architecture of the hair units and gives natural results.Citation23
The loss of progenitor cells, but not stem cells, is evident in bald vs non-bald scalp areas in patients with androgenetic alopecia. These findings reported by Garza et al support the hypothesis that a defect in conversion of hair follicle stem cells to progenitor cells plays a role in the pathogenesis of androgenetic alopecia.Citation24 This breakthrough could implicate a novel model for future treatments.
Alopecia areata
Alopecia areata is a noncicatricial loss of hair in any area of the body, with a multifactorial autoimmune pathogenesis and an unknown etiology.Citation25 This disease affects up to 2% of the population and presents with a wide range of clinical heterogeneity.Citation26 Patients with alopecia areata may present with a very sudden and dramatic loss of hair. Clinically, one or more well circumscribed, smooth, scarless, hair-less patches that enlarge in a centrifugal pattern can be observed. Severe forms involve the whole scalp (alopecia areata totalis) or all body hair (alopecia areata universalis). Alopecia areata can be associated with other autoimmune diseases, including thyroid disease, celiac disease, vitiligo, and atopy.Citation27
The first episode of alopecia areata can often resolve spontaneously without any medical intervention.Citation27,Citation28 The severity of the first episode of alopecia areata is an important prognostic factor. Further, response to topical immunotherapy may be associated with a better prognosis. In children, the prognosis is worse. Finally, it has been shown that alopecia areata worsens over time.Citation29
Most cases of alopecia areata resolve spontaneously within 1 year, but up to 25% of patients develop severe forms with total loss of scalp hair (alopecia totalis) or of all body hair (alopecia universalis) that often persist indefinitely.Citation27,Citation28 One study showed in adults that the more severe the disease at onset, the more severe the prognosis. In children, the evolution is difficult to predict, because patients with mild alopecia areata also tend to progress to severe forms.Citation29
Available treatments may induce hair regrowth but have never been proven to change the course of the disease. These include pulsed high doses of oral or intravenous steroids, topical high potency steroids under occlusion, photochemotherapy, and topical immunotherapy. Efficacy of treatments in patients with alopecia totalis and alopecia universalis is poor, with long-term complete regrowth in less than 20% of patients.Citation29
Intralesional steroids (triamcinolone acetonide 5 mg/mL) are probably the most utilized treatments for patchy alopecia areata, although there are no controlled studies that confirm efficacy.Citation28 Systemic steroids, which have been used in daily, weekly, and monthly pulse regimens with variable success, are effective in inducing regrowth and arresting hair loss in acute disease.Citation28,Citation30–Citation32 However, the use of systemic steroids is limited by the frequent occurrence of relapses after treatment tapering or interruption.Citation28 High potency topical corticosteroids under occlusion are also effective in alopecia areata totalis and universalis, with long-term benefit in approximately 15% of patients.Citation29
Topical immunotherapy with diphenylcyclopropenone or squaric acid dibutylester is a good option in severe alopecia, including alopecia totalis and universalis.Citation33 The goal of treatment is to induce a mild contact dermatitis of the scalp. The efficacy of diphenylcyclopropenone has been proven by studies that demonstrated hair regrowth limited to the treated half side of the scalp.Citation28,Citation34–Citation36 Unfortunately, only a few therapies for alopecia areata have been comprehensively evaluated in randomized controlled trials.Citation37
Telogen effluvium
Telogen effluvium is the loss of telogen hair due to abnormal hair cycling.Citation38 Excessive daily shedding of approximately 100–200 telogen hairs is typically seen. If hair loss is present for less than 6 months, it is labeled acute telogen effluvium. However, if hair loss is present for more than 6 months, it is labeled chronic telogen effluvium.Citation2 Acute telogen effluvium does not usually produce visible alopecia, because approximately 50% of hair is usually lost before there is an apparent reduction of hair density. Possible causes of acute telogen effluvium include systemic disease, drugs, fever, psychoemotional stress, weight loss, delivery, iron and Vitamin D deficiency, inflammatory scalp disorders, interruption of oral contraceptives, and iron deficiency.Citation2 Treatment for telogen effluvium should be focused on the cause. For example, most dermatologists prescribe iron supplementation when the ferritin level is below 30 ng/mL. However, a recent study showed no statistically significant increase in the incidence of iron deficiency in premenopausal or postmenopausal women with androgenetic alopecia or chronic telogen effluvium vs control subjects.Citation39
Cicatricial alopecia
Cicatricial alopecia includes a group of conditions characterized by inflammation and subsequent destruction of the hair follicle, resulting in irreversible hair loss. Cicatricial alopecia can be primary or secondary. Diseases that primarily affect the hair follicle cause primary cicatricial alopecia, which is classified as lymphocytic or neutrophilic, based on the type of inflammatory cell that predominates. Examples of lymphocytic cicatricial alopecia include lichen planopilaris, its clinical variant frontal fibrosing alopecia, and discoid lupus erythematosus.Citation40 Secondary cicatricial alopecia is caused by more systemic disorders, including scleroderma, granulomatous inflammation, such as sarcoidosis, or neoplastic disease. The diagnosis of cicatricial alopecia requires pathological evaluation. Early diagnosis of cicatricial alopecia is essential because the goal of treatment is to slow progression of the condition.Citation41
First-line treatments for discoid lupus erythematosus of the scalp and lichen planopilaris are potent topical corticosteroids, including fluocinonide 0.025%–0.05% and clobetasol lotion or cream,Citation42–Citation45 and intralesional triamcinolone acetonide (4–5 mg/mL and 10 mg/mL).Citation46–Citation48 Oral corticosteroids (1 mg/kg/day or 25 or 50 mg/day for 1 month) can be particularly helpful in the case of rapidly progressive disease and can be tapered over 2–4 months.Citation48–Citation50
Other useful therapeutic options include topical (1.5%) and oral cyclosporine (4 and 5 mg/kg/day for 3–5 months).Citation41,Citation44 Hydroxychloroquine was proven effective in arresting progression of lichen planopilaris, frontal fibrosing alopecia, and discoid lupus erythematosus of the scalp.Citation51–Citation53 Also, mycophenolate mofetil has been shown to be efficacious in treating lichen planopilaris.Citation54,Citation55 Finally, doxycycline has shown some efficacy in the treatment of lichen planopilaris.Citation51
A promising new treatment focus for lichen planopilaris is the abnormal peroxisome proliferator-activated receptor pathways, which leads to aberrant lipid metabolism in the sebaceous gland, a toxic buildup of lipids, and an inflammatory response.Citation56 Improvement of lichen planopilaris following treatment with the oral peroxisome proliferator-activated receptor-γ agonist, pioglitazone hydrochloride at 15 mg/day was recently reported.Citation57
Overall, an aggressive multiple modality therapeutic approach is often necessary for the treatment of cicatricial alopecia. Unfortunately, treatment failure is common and none of the available agents clearly halt the progression of cicatricial alopecia.Citation58–Citation60
Conclusion
Overall, there are many useful evaluative approaches to aid in the diagnosis of both cicatricial and noncicatricial alopecias. These include scalp biopsies, microscopic evaluation, trichoscopy, or hair counts, just to name a few. Following diagnosis, a variety of treatments are available. Further, promising new treatment modalities are being considered, including those that target hair follicle stem cells for the treatment of androgenetic alopecia or the peroxisome proliferator-activated receptor pathways for the treatment of lichen planopilaris. Continued advances will aid the clinician in effectively treating both cicatricial and noncicatricial alopecias in the future.
Disclosure
The authors report no conflicts of interest in this work.
References
- DhuratRSaraogiPHair evaluation methods: merits and demeritsInt J Trichology20091210811920927232
- TostiAPiracciniBMSistiADuque-EstradaBHair loss in womenMinerva Ginecol200961544545219749676
- HillmannKBlume-PeytaviUDiagnosis of hair disordersSemin Cutan Med Surg2009281333819341940
- WhitingDAHistopathology of alopecia areata in horizontal sections of scalp biopsiesJ Invest Dermatol1995104Suppl 526S27S7738382
- WhitingDAChronic telogen effluvium: increased scalp hair shedding in middle-aged womenJ Am Acad Dermatol19963568999068959948
- ReboraAGuarreraMBaldariMVecchioFDistinguishing androgenetic alopecia from chronic telogen effluvium when associated in the same patient: a simple noninvasive methodArch Dermatol2005141101243124516230561
- QuercetaniRReboraAFediMPatients with profuse hair shedding may reveal anagen hair dystrophy: a diagnostic clue of alopecia areata incognitaJ Eur Acad Dermatol Venereol201125780881020946585
- ArdigoMTostiACameliNVincenziCMiscialiCBerardescaEReflectance confocal microscopy of the yellow dot pattern in alopecia areataArch Dermatol20111471616421242396
- RudnickaLOlszewskaMRakowskaAKowalska-OledzkaESlowinskaMTrichoscopy: a new method for diagnosing hair lossJ Drugs Dermatol20087765165418664157
- RossEKVincenziCTostiAVideodermoscopy in the evaluation of hair and scalp disordersJ Am Acad Dermatol200655579980617052485
- TostiATorresFDermoscopy in the diagnosis of hair and scalp disordersActas Dermosifiliogr2009100Suppl 111411920096205
- Duque-EstradaBTamlerCSodreCTBarcauiCBPereiraFBDermoscopy patterns of cicatricial alopecia resulting from discoid lupus erythematosus and lichen planopilarisAn Bras Dermatol201085217918320520933
- TostiATorresFMiscialiCFollicular red dots: a novel dermoscopic pattern observed in scalp discoid lupus erythematosusArch Dermatol2009145121406140920026850
- TostiAGrayJAssessment of hair and scalp disordersJ Investig Dermatol Symp Proc20071222327
- FrishbergDPSperlingLCGuthrieVMTransverse scalp sections: a proposed method for laboratory processingJ Am Acad Dermatol1996352 Pt 12202228708025
- WhitingDADiagnostic and predictive value of horizontal sections of scalp biopsy specimens in male pattern androgenetic alopeciaJ Am Acad Dermatol1993285 Pt 17557638496421
- StefanatoCMHistopathology of alopecia: a clinicopathological approach to diagnosisHistopathology2010561243820055903
- [No authors listed]Hair loss and contraceptivesBr Med J1973258654995004736624
- BracheVFaundesAAlvarezFCochonLNonmenstrual adverse events during use of implantable contraceptives for women: data from clinical trialsContraception2002651637411861056
- OlsenEAMessengerAGShapiroJEvaluation and treatment of male and female pattern hair lossJ Am Acad Dermatol200552230131115692478
- HoedemakerCvan EgmondSSinclairRTreatment of female pattern hair loss with a combination of spironolactone and minoxidilAustralas J Dermatol2007481434517222303
- RathnayakeDSinclairRMale androgenetic alopeciaExpert Opin Pharmacother20101181295130420426708
- PatwardhanNMysoreVIADVL Dermatosurgery Task Force. Hair transplantation: standard guidelines of careIndian J Dermatol Venereol Leprol2008Suppl 74S465318688103
- GarzaLAYangCCZhaoTBald scalp in men with androgenetic alopecia retains hair follicle stem cells but lacks CD200-rich and CD34-positive hair follicle progenitor cellsJ Clin Invest2011121261362221206086
- TruebRMSystematic approach to hair loss in womenJ Dtsch Dermatol Ges201084284298 German20105246
- KosLConlonJAn update on alopecia areataCurr Opin Pediatr200921447548019502982
- MacDonald HullSPWoodMLHutchinsonPESladdenMMessengerAGBritish Association of Dermatologists. Guidelines for the management of alopecia areataBr J Dermatol2003149469269914616359
- AlkhalifahAAlsantaliAWangEMcElweeKJShapiroJAlopecia areata update: part II. TreatmentJ Am Acad Dermatol201062219120220115946
- TostiABellavistaSIorizzoMAlopecia areata: a long term follow-up study of 191 patientsJ Am Acad Dermatol200655343844116908349
- FriedliALabartheMPEngelhardtEFeldmannRSalomonDSauratJHPulse methylprednisolone therapy for severe alopecia areata: an open prospective study of 45 patientsJ Am Acad Dermatol1998394 Pt 15976029777767
- KarBRHandaSDograSKumarBPlacebo-controlled oral pulse prednisolone therapy in alopecia areataJ Am Acad Dermatol200552228729015692475
- SharmaVKPulsed administration of corticosteroids in the treatment of alopecia areataInt J Dermatol19963521331368850047
- SinghGLavanyaMTopical immunotherapy in alopecia areataInt J Trichology201021363921188022
- CotellessaCPerisKCaraccioloEMordentiCChimentiSThe use of topical diphenylcyclopropenone for the treatment of extensive alopecia areataJ Am Acad Dermatol2001441737611148480
- OrecchiaGPerfettiLAlopecia areata and topical sensitizers: allergic response is necessary but irritation is notBr J Dermatol199112455092039735
- Dall’oglioFNascaMRMusumeciMLTopical immunomodulator therapy with squaric acid dibutylester (SADBE) is effective treatment for severe alopecia areata (AA): results of an open-label, paired-comparison, clinical trialJ Dermatolog Treat2005161101415897160
- DelamereFMSladdenMMDobbinsHMLeonardi-BeeJInterventions for alopecia areataCochrane Database Syst Rev20082CD00441318425901
- HarrisonSSinclairRTelogen effluviumClin Exp Dermatol2002275385389
- OlsenEAReedKBCacchioPBCaudillLIron deficiency in female pattern hair loss, chronic telogen effluvium, and control groupsJ Am Acad Dermatol201063699199920947203
- HarriesMJPausRThe pathogenesis of primary cicatricial alopeciasAm J Pathol201017752152216220889564
- MirmiraniPWilleyAPriceVHShort course of oral cyclosporine in lichen planopilarisJ Am Acad Dermatol200349466767114512914
- RoenigkHHJrMartinJSEichornPGilliamJNDiscoid lupus erythematosus. Diagnostic features and evaluation of topical corticosteroid therapyCutis19802532812856987043
- BjornbergAHellgrenLTreatment of chronic discoid lupus erythematosus with fluocinolone acetonide ointmentBr J Dermatol19637515616013971327
- ChieregatoCZiniABarbaAMagnaniniMRosinaPLichen planopilaris: report of 30 cases and review of the literatureInt J Dermatol200342534234512755968
- KangHAlzolibaniAAOtbergNShapiroJLichen planopilarisDermatol Ther200821424925618715294
- CallenJPChronic cutaneous lupus erythematosus. Clinical, laboratory, therapeutic, and prognostic examination of 62 patientsArch Dermatol198211864124167092253
- NewtonRCHebertAAFreeseTWSolomonARScarring alopeciaDermatol Clin1987536036183301117
- RossEKTanEShapiroJUpdate on primary cicatricial alopeciasJ Am Acad Dermatol200553113715965418
- KossardSLeeMSWilkinsonBPostmenopausal frontal fibrosing alopecia: a frontal variant of lichen planopilarisJ Am Acad Dermatol199736159668996262
- WisemanMCShapiroJScarring alopeciaJ Cutan Med Surg19993Suppl 3S45S4811749890
- SamraoAChewALPriceVFrontal fibrosing alopecia: a clinical review of 36 patientsBr J Dermatol201016361296130020698851
- KraakJHVan KetelWPrakkenJRVan ZwetWThe value of hydroxychloroquine (Plaquenil) for the treatment of chronic discoid lupus erythematosus; a double blind trialDermatologica196513029330514333636
- ChiangCSahDChoBKOchoaBEPriceVHHydroxychloroquine and lichen planopilaris: efficacy and introduction of Lichen Planopilaris Activity Index scoring systemJ Am Acad Dermatol201062338739220061052
- ChoBKSahDChwalekJEfficacy and safety of mycophenolate mofetil for lichen planopilarisJ Am Acad Dermatol201062339339720061053
- TursenUApiHKayaTIkizogluGTreatment of lichen planopilaris with mycophenolate mofetilDermatol Online J20041012415347506
- KarnikPTekesteZMcCormickTSHair follicle stem cell-specific PPAR gamma deletion causes scarring alopeciaJ Invest Dermatol200912951243125719052558
- MirmiraniPKarnikPLichen planopilaris treated with a peroxisome proliferator-activated receptor gamma agonistArch Dermatol2009145121363136620026843
- TostiADuque-EstradaBTreatment strategies for alopeciaExpert Opin Pharmacother20091061017102619364249
- TanEMartinkaMBallNShapiroJPrimary cicatricial alopecias: clinicopathology of 112 casesJ Am Acad Dermatol2004501253214699361
- Moreno-RamirezDFerrandizLCamachoFMDiagnostic and therapeutic assessment of frontal fibrosing alopeciaActas Dermosifiliogr200798959460217961448