Abstract
Previous studies have suggested a benefit for patients with plaque psoriasis when omega-3 fatty acids are added to topical treatment. This study evaluated the efficacy of a nutritional complement rich in omega-3 fatty acids in patients with mild or moderate plaque psoriasis. Thirty patients were recruited, 15 of whom were given topical treatment with tacalcitol, forming the control group. The remaining 15 patients were given topical tacalcitol and 2 capsules of Oravex® daily. Three visits, the baseline, intermediate (week 4), and final (week 8), were held over an 8-week period. The main efficacy endpoints were the Psoriasis Area and Severity Index (PASI), Nail Psoriasis Severity Index (NAPSI) and Dermatological Life Quality Index (DLQI). A clear and significant improvement was observed in all the efficacy endpoints in both groups between the baseline visit and the end visit. This improvement was significantly greater in the group treated additionally with Oravex® than in the control group. Supplementary treatment with omega-3 fatty acids complements topical treatment in psoriasis, and makes a significant contribution to reducing PASI and NAPSI and improving DLQI; and to reducing scalp lesion and pruritus, erythema, scaling, and infiltration of the treated areas.
Introduction
Psoriasis is a chronic skin disease which shows a course with outbreaks and presents variable clinical findings.Citation1 Nowadays, psoriasis is regarded as an immunologically based disease which combines dermal inflammation with secondary epidermal hyperplasia.Citation2
In recent years, the so-called metabolic syndrome has been described, and defined as the ensemble of cardiovascular risk factors, including central obesity, atherogenic dyslipidemia, hypertension, and glucose intolerance, affected by lifestyle, genetic predisposition, and the environment. The presence of metabolic syndrome triples a patient’s risk of developing type 2 diabetes mellitus and doubles the risk of developing cardiovascular disease.Citation3
It has been described that patients diagnosed with psoriasis have a high prevalence of metabolic disorders such as diabetes, hypertension, obesity, and hyperlipidemia, as well as a high frequency of tobacco consumption, and also an increased morbidity and mortality risk.Citation4–Citation6
Like psoriasis, metabolic syndrome is characterized by a fundamentally TH1 inflammatory response, which points to the hypothesis that psoriasis is associated with metabolic syndrome due to a shared inflammation mechanism. Another possible explanation for predisposition to the development of metabolic syndrome by patients with psoriasis lies in behavioral habits or in the psychological impact of the disease. Another hypothesis is that it is the actual metabolic syndrome that promotes development of psoriasis.
In relation to the foregoing, several studies have demonstrated an increase in C-reactive protein in patients with psoriasis due to an elevation in the serum concentration of IL-6 and MRP8 and MRP14 proteins, which presents proatherogenic action.Citation4 Recent studies confirm that Th17, Th22, and Th1 cells are detected in psoriatic skin lesions and implicated in psoriasis pathogenesis.Citation7
In recent years, the topical treatment of psoriasis has made major progress.Citation8–Citation10 Vitamin D derivatives are one of the pillars of topical treatment of psoriasis.Citation11–Citation15 In Spain 3 vitamin D derivatives are used: calcipotriol, tacalcitol, and calcitriol. In combination with other treatments, vitamin D derivatives constitute the ideal maintenance treatment, since their application may be maintained over time.
Omega-3 fatty acids, eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), reduce symptoms in many inflammatory skin diseases, limiting the spreading of the inflammatory process.Citation16,Citation17 In the skin, the main route for the synthesis of leukotrienes is 15-lipoxygenase, giving rise to 15-hydroxyeicosatetraenoic acid. Moreover, the epidermis can convert the leukotriene A4 (produced by the polymorphonuclear leukocytes) into leukotriene B4, one of the main inflammation mediators.
The intake of EPA and DHA leads to the formation of hydroxylated metabolites through 15-lipoxygenase, 15-hydroxyeicosapentaenoic acid, and 15-hydroxydocosahexaenoic acid. Both substances are potent inhibitors of the 5-lipoxygenase of mononuclear cells, thus limiting the synthesis of proinflammatory leukotrienes LTB4, LTC4, and LTD4.
To date, several studies have been performed to evaluate the efficacy of the daily supplementation of EPA and DHA in patients with psoriasis,Citation17–Citation20 with an improvement observed in their mean Psoriasis Area and Severity Index (PASI) score, as well as in clinical symptoms, particularly in pruritus.
Objective
The study endpoint is to evaluate the efficacy of the intake of omega-3 fatty acids in patients with mild or moderate plaque psoriasis by means of the addition of Oravex® (Thea Laboratories, Barcelona, Spain [280 mg of eicosapentaenoic acid, 40 mg of docosahexaenoic acid, 50 mg of thyme extract, 50 mg of olive leaf extract, 20 mg of green tea extract, 7.5 mg of zinc, 27.5 μg of selenium per capsule]), as a nutritional complement rich in omega-3 fatty acids, increases the efficacy of topical treatment of plaque psoriasis.
Methodology
This was a prospective, open, single-center, controlled observational study with a 2-month follow-up.
Fifteen patients were selected during October and November 2007 and began treatment with tacalcitol, forming group B. In turn, a further 15 patients were selected who, besides treatment with tacalcitol, took 2 daily capsules of Oravex®, forming group A. There was no placebo in the study, so the study was not blinded to either the patient or to the observer. Both groups were homogenous for sex, age, and body mass index (BMI). The dosage of EPA and DHA was 640 mg daily (the World Health Organization recommends a minimum daily intake of 0.3 to 0.5 g of EPA and DHA in the general population).
The inclusion criteria were age between 18 and 70 years, and stable mild (PASI < 3) or moderate (PASI 3–10) plaque psoriasis. The exclusion criteria were receiving topical therapy in the previous 2 weeks and phototerapy, systemic, or biological therapy in the previous 4 weeks. Also we excluded pregnant or breastfeeding women, and patients with liver disease and neuropathies.
The main efficacy endpoints were PASI, Nail Psoriasis Severity Index (NAPSI), and Dermatology Life Quality Index (DLQI).
Secondary endpoints were the values pertaining to the presence of pruritus (yes/no), scalp psoriasis (0, no; 1, mild; 2, moderate; 3, severe) and clinical evolution of the target plaque according to erythema, infiltration, and scaling (scored on a scale of 0, none to 5, serious).
Blood analyses were performed on the patients at the baseline and end visits.
Results
Data were collected from the 30 patients at the baseline visit and weeks 4 and 8 (). No patient dropped out or was withdrawn from the study.
Table 1 Results of primary and secondary endpoints
The mean age was 58.97 ± 15.1 years, 63.3% were men, and mean BMI was 26.85 ± 3.3 kg/m2; 30.0% of the patients had a normal BMI, 53.3% were overweight, and the remaining 16.7% were considered obese.
The safety endpoints, particularly in blood control, presented no deterioration in patient state rendering withdrawal from the study advisable.
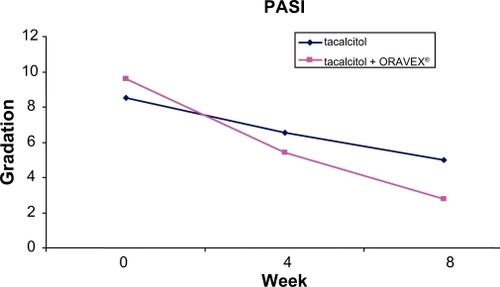
The PASI presented an improvement of 6.8 points in the Oravex® group, whereas in the control group it was only 3.5 points (). This difference was highly significant (P < 0.0001).
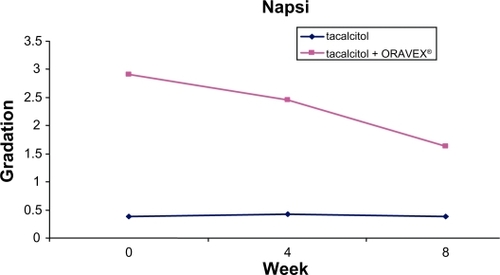
A reduction was observed in the NAPSI in the group treated with Oravex®, from 2.91 at the baseline visit to 1.68 in the visit after 8 weeks. The control group did not improve in this endpoint, although this endpoint was initially very low and different to that of group A ().
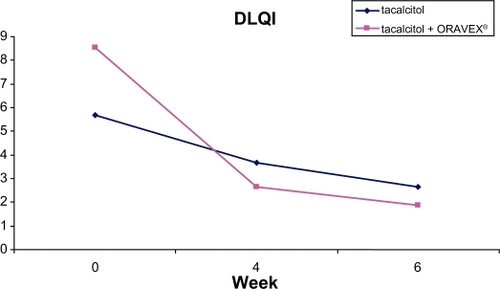
DLQI was also greater in the group treated with Oravex®, with an improvement of 6.67 points versus 3.03 in the control group ().
In all the secondary endpoints studied (scalp lesion, lesion of target plaque-erythema, infiltration, and scaling) a significant improvement was observed in the group treated with Oravex® compared with the control group after 8 weeks of treatment.
The evolution of some of the patients of the group treated with Oravex® plus tacalcitol is shown in and .
Discussion
The present study was conducted to evaluate the efficacy of the addition of a nutritional supplement rich in omega-3 fatty acids in the treatment of psoriasis. Previous studies have demonstrated the possible effect of the diet on the evolution of the disease. Dietary omega-3 (n-3) fatty acids have a variety of anti-inflammatory and immune-modulating effects that may be of relevance to atherosclerosis and its clinical manifestations of myocardial infarction, sudden death, and stroke. A variety of biologic effects of EPA and DHA have been demonstrated from feeding studies with fish or fish oil supplements in humans and animals. These include effects on triglycerides, high-density lipoprotein cholesterol, platelet function, endothelial and vascular function, blood pressure, cardiac excitability, measures of oxidative stress, pro- and anti-inflammatory cytokines, and immune function. Clinically important anti-inflammatory effects in man are further suggested by trials demonstrating benefits of fatty acids in psoriasis, among others.Citation21
After 8 weeks of treatment, there was a clear improvement in all the study endpoints in the group with Oravex® added to the treatment with tacalcitol versus the control group, treated exclusively with tacalcitol.
Despite the low number of patients recruited to the study, the statistical significance of the differences between groups clearly indicates that a global improvement is achieved with the addition of Oravex® to the treatment with tacalcitol.
Conclusion
Supplementary treatment with omega-3 fatty acids complements topical treatment in psoriasis, and makes a significant contribution to reducing PASI and NAPSI, and improving DLQI; and in reducing scalp lesion and pruritus, erythema, scaling, and infiltration of the treated areas.
Disclosure
The authors declare no conflicts of interest.
References
- FerrándizCDermatosis eritematoescamosas (I) Psoriasis EritrodermiasFerrándizCDermatología ClínicaMadridMosby1996149156
- CasanovaJMMartíRMInmunopatogénesis de la psoriasisPiel19937486495
- Puig SanzLPsoriasis, a systemic disease?Actas Dermosifiliog200798396402
- LoveTJQureshiAAKarlsonEWGelfandJMChoiHKPrevalence of the Metabolic Syndrome in Psoriasis: Results From the National Health and Nutrition Examination Survey, 2003–2006Arch Dermatol20101220 [Epub ahead of print].
- PreySPaulCBronsardVCardiovascular risk factors in patients with plaque psoriasis: a systematic review of epidemiological studiesJ Eur Acad Dermatol Venereol201024Suppl 2233020443997
- MallbrisLRitchinCTStahleMMetabolic disorders in patients with psoriasis and psoriatic arthritisCurrent Rheumatol Rev2006835563
- KagamiSRizzoHLLeeJJKoguchiYBlauveltACirculating Th17, Th22, and Th1 cells are increased in psoriasisJ Invest Dermatol20101301373138320032993
- CasanovaJMDiagnóstico y tratamiento de la psoriasisPiel19872416424
- De PabloGuerraATratamiento de la psoriasis en pacientes ambulatoriosPiel19938388396
- GraavesMVWeinsteinGDTreatment of psoriasisN Engl J Med19953325815877838193
- KragballeKVitamin D3 analoguesDermatol Clin1995138358398785887
- LebwohlMGThe evolution of vitamin D analogues for the treatment of psoriasisArch Dermatol1995131132313247503579
- OhtaTOkabeKAzumaYKiyokiMIn vivo microautoradiography of tacalcitol following topical application to normal rats in vitro metabolism in human keratinocitesArch Dermatol Res19962881881968967791
- SatoHSugimotoIMatsunagaTTsuchimotoMOhtaTUnoHTacalcitol inhibits phorbol esterinduced epidermal proliferation and cutaneous inflammation, and induces epidermal differenciation in miceArch Dermatol Res19962886566638931867
- ScarpaCTacalcitol Pomada: Un tratamiento eficaz y bien tolerado de la psoriasisJ Eur Acad Dermatol Venereol19966142146
- WoltersMDiet and psoriasis: experimental data and clinical evidenceBr J Dermatol200515370671416181450
- WoltersMThe significance of diet and associated factors in psoriasisHautartz2006579991004
- KragballeKFoghKA low-fat diet supplemented with dietary fish oil (Max-EPA) results in improvement of psoriasis and in formation of leukotriene B5Acta Derm Venereol19896923282563604
- KojimaTTeranoTTanabeEOkamotoSTamuraYYoshidaSLong-term administration of highly purified eicosapentaenoic acid provides improvement of psoriasisDermatologica19911822252301884857
- LassusADahlgrenALHalpernMJSantalahtiJHapponenHPEffects of dietary supplementation with polyunsaturated ethyl ester lipids (Angiosan) in patients with psoriasis and psoriatic arthritisJ Int Med Res19901868732139859
- MoriTABeilinLJOmega-3 fatty acids and inflammationCurr Atheroscler Rep2004646146715485592