Abstract
Background
Metabolic syndrome (MBS) has been reported as a frequent comorbidity in psoriatic patients. The main pathogenesis is considered to be inflammation in this association. MBS has been investigated in eating disorders as well. While psoriasis has some psychiatric comorbidities, the link between psoriasis, MBS, and eating disorders (EDs) is unknown.
Methods
The study was designed as a cross-sectional, randomized, and controlled trial. A total of 100 patients with psoriasis were included in the study. Sociodemographic data, clinical subtype of psoriasis, Psoriasis Area and Severity Index (PASI) scores, and associated diseases were registered for each patient. The criteria for diagnosis of MBS developed by the International Diabetes Foundation (IDF) was used. These are central obesity (waist circumference ≥94 cm in men or ≥80 cm in women), plus two of the following: elevated triglycerides (≥150 mg/dL), reduced high-desity lipoprotein cholesterol (>40 mg/dL for men; >50 mg/dL for women), elevated blood pressure (≥130 mmHg systolic or ≥85 mmHg diastolic), and elevated fasting blood glucose (≥100 mg/dL). Additionally, the Eating Attitude Test (EAT), Beck Depression Inventory (BDI), and Beck Anxiety Inventory (BAI), and psychiatric interview were performed for all patients.
Results
There were 45 female and 55 male patients, aged between 18 and 85 years old (median 41.12 ± 16.01). MBS was present in 31% of the patients with psoriasis. There was no correlation between the severity of psoriasis and MBS. EAT scores were ≥30 in 7/100 patients. Four out of 31 patients with MBS (12.9%) had ED and 3/69 patients were without MBS (4.3%). Mean ED scores were compared statistically and the difference was significant (EAT = 17.9 ± 9.558 and 11.5 ± 7.204, P < 0.001).
Conclusion
Defining risk factors leading to comorbidities is important in psoriasis. EDs seem to have an impact on the development of MBS in psoriasis. Establishment and treatment of EDs in patients with psoriasis may prevent the onset of MBS and other comorbidities due to MBS.
Introduction
Psoriasis is a chronic inflammatory skin disease. Variable immunological and inflammatory processes play a role in pathogenesis and also contribute to occurrence of comorbidities. While the more common concomitant disorders are psoriatic arthritis and depression/anxiety, research papers of comorbidities due to metabolic disregulation and resultant metabolic syndrome (MBS) gradually increase.Citation1–Citation8 MBS is particularly important, because it includes a cluster of risk factors such as central obesity, hypertension, abnormal glucose intolerance, and dyslipidemia, all of which are strong predictors of cardiovascular disease, diabetes mellitus, and stroke.Citation9–Citation11 All these comorbidities are complex and are supposed to share common pathogenetic pathways and cytokine profiles with psoriasis. Moreover, it is also important to be aware of some predisposing factors, such as sedentary life style, smoking, and alcoholism, which have been previously considered to be facilitating factors for the development of MBS in patients with psoriasis.Citation12
Eating disorders (EDs) are characterized by clinically significant disturbances in eating behavior. They are often accompanied by another psychiatric disorder such as depression and anxiety. Particularly, binge-eating disorder (BED) may be associated with obesity and MBS.Citation12,Citation13 Hence, it is logical to consider that EDs are psychogenic cofactors which may contribute to the development of MBS in psoriatic patients who are also prone to various psychiatric comorbidites; for example, depression and anxiety.Citation14–Citation16
While a few studies demonstrate a link between MBS and EDs,Citation17–Citation19 there are also some studies implicating a relationship between EDs and anxiety.Citation20–Citation22 If there is a relationship between EDs and psoriasis, diagnosing any ED would be useful for suggesting a change in eating behavior of a psoriatic patient with MBS and thus improve resultant MBS.
Materials and methods
The study was designed as a cross-sectional, randomized, and controlled trial. A total of 100 patients with psoriasis (55 males, 45 females, age range 18–85, mean age 41.12 ± 16.01) were included in the study. Sociodemographical data including sex, age, marital status and educational status, clinical subtype of psoriasis, psoriasis area severity index (PASI) scores, and other systemic diseases were registered for each patient. Additionally, Eating attitudes Test (EAT), Beck Depression Inventory (BDI), and Beck Anxiety Inventory (BAI) were performed on all patients.
EAT-26 is a widely used self-report measure of EDs, and although it was developed by Garner and Garfinkel in 1979Citation23 to measure symptoms of anorexia nervosa (AN), it has been used in nonclinical samples as a general screening measure for disordered eating attitudes. EAT-26 is based on EAT-40 and was adapted to Turkish by Erol and Savasir in 1989.Citation24 Total scores on EAT-26 are derived as a sum of the composite items, ranging from 0 to 53, with a score of 20 used as the cutoff.Citation24 The Turkish version of EAT consists of 40 questions, the answers to which are evaluated with a six-point Likert scale, from “always” to “never.” The resulting scores range between 0 and 120 points, and individuals scoring ≥30 points are considered as at high risk of EDs.Citation24 The Turkish versions of BDI and BAI, reliability and validity studies of which had been previously performed in the Turkish population, were used.Citation25–Citation28
All patients were evaluated for the presence of MBS. The criteria developed by the International Diabetes Foundation for diagnosis of MBS was used. These criteria are central obesity (waist circumference ≥94 cm in men or ≥80 cm in women), plus two of the following: triglycerides ≥150 mg/dL; high-desity lipoprotein cholesterol <40 mg/dL for men or <50 mg/dL for women; blood pressure ≥130 mmHg systolic or ≥85 mmHg diastolic; and fasting blood glucose ≥100 mg/dL. Two study groups were formed according to these criteria. Group 1 consisted of the patients who met MBS criteria, and Group 2 consisted of the patients who did not meet MBS criteria. These two groups were compared statistically in terms of sociodemographical factors and the presence of MBS, EDs, depression, and anxiety. The patients who had an ED according to EAT were also evaluated by a psychiatrist, and the ED was confirmed by psychiatric examination and Diagnostics and Statistical Manual of Mental Disorders, 4th edition criteria.Citation29
Patients who were found to have an ED were assessed according to EAT, and a psychiatric interview was done by a psychiatrist. The patients were classified as having AN, bulimia nervosa (BN), BED, or an ED not otherwise specified (ED-NOS). Independent samples t-test, Mann–Whitney U-test, chi-square test, Fisher’s exact test, and SPSS Statistics 11.5 (IBM Corporation, Somers, NY) software for Windows® were used for statistical assessments. P < 0.05 was considered statistically significant.
Results
Group 1 consisted of 31 patients with MBS (31%, mean age 48.5 ± 13.4), and Group 2 consisted of 69 patients (69%, mean age 37.7 ± 16.0). When the two groups were compared, all parameters including sex, marital status, educational status, disease duration, type of psoriasis according to onset age (type I and type 2), and disease severity determined by PASI values except for age were statistically insignificant (). EAT scores were ≥30 in 7 out of 100 patients. Four out of 31 patients with MBS (12.9%) and 3 out of 69 patients without MBS (4.3%) had an ED. However, statistical evaluation was impossible because of low numbers of patients; therefore, mean ED scores were evaluated and a statistically significant difference was found (EAT = 17.9 ± 9.558 and 11.5 ± 7.204, P < 0.001) (). In psychiatric evaluation, three out of four patients (75%) had BED and one (25%) had ED-NOS in Group 1. Two out of three patients (67%) had BED, and one (33%) had ED-NOS. No patients had AN or BN.
Figure 1 Mean scores of EAT in patients with MBS and patients without MBS (EAT = 17.900 ± 9.558 and 11.500 ± 7.204, P < 0.001).
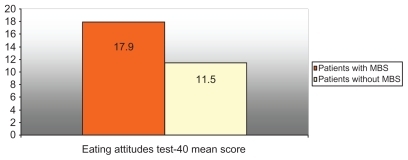
Table 1 Demographic and clinical characteristics of psoriatic patients with MBS and without MBS
When the relationship between EDs and depression/anxiety scores was considered, mean BAI scores of the patients with an ED were higher than those without an ED, and the statistical difference was significant (P = 0.004) (). In addition, when the presence of anxiety is considered, the difference between the patients with an ED and those without an ED was statistically significant (P = 0.002). BDI did not show any correlation with ED scores; thus, the existence of depression was not related to an ED.
Table 2 Beck anxiety and Beck depression mean scores in psoriatic patients with EDs and without EDs (Mann–Whitney U-test; 95% confidence interval)
The relationship between PASI and other parameters (criteria of MBS, anxiety, and depression) was evaluated statistically. Only the presence of depression revealed a significant difference (P = 0.031).
Discussion
Psoriasis is a chronic, immunologically based, inflammatory disease associated with many comorbidities related to immune-mediated inflammation and metabolic dysregulation. In particular, recent studies have focused on the MBS and its components such as atherogenesis, hypertension, and insulin resistance. It is hypothesized that proinflammatory cytokines and pathomechanisms in inflammation are shared in both psoriasis and MBS.Citation1,Citation4 In fact, this association alone was proven; it was not considered a causality. Hence, a new problem has emerged with additional risk factors such as cigarette smoking, excessive alcohol consumption, and obesity, which predispose psoriatic patients to develop MBS.Citation4,Citation14–Citation16 This hypothesis was reinforced by Alsufyani et al.Citation4 They suggested that speculation exists as to whether this association is causative or whether it is the result of other habits seen in psoriasis patients, such as increased rates of smoking, alcohol consumption, and sedentary lifestyle, which add to the complexity of the association between psoriasis and MBS.
Some authors proposed that abnormal eating behavior associated with a sedentary lifestyle may contribute to the development of obesity.Citation14 This was previously demonstrated in some studies, in particular for BED, short-term overeating, and ED-NOS.Citation30–Citation32 BED is characterized by recurrent episodes of binge eating. In fact, binge eating behaviour which is also seen in many cases of AN and BN is the main characteristic of ED. Although little is known about MBS in obese patients with BED, laboratory studies have shown that eating behaviors frequently found in BED patients may increase the risk of metabolic abnormalities. For example, in one study, increased eating rate has been demonstrated to be associated with central obesity, elevated serum lipids, and fatty liver.Citation32 The results of a longitudinal study conducted by Hudson et al showed that BED may increase the risk of components of MBS independent of the risk conferred by obesity alone.Citation18 Interestingly, metabolic abnormalities have even been observed in healthy lean women following laboratory-based binge-like episodes.Citation33 The fact that the mean ED score was higher in psoriatic patients with MBS than in those without MBS is in accordance with literature data implicating a link between MBS and ED.Citation32,Citation34 However, the number of patients was inadequate for statistical comparison for EDs. This may be a limitation of this present study. More reliable or indicative results are likely with a larger number of psoriasis patients. When considering the prevalence of EDs, there are different studies in different populations. Women, children, adolescents, and the obese have been the principal subjects for prevalence studies.Citation32,Citation35–Citation37 In a largescale prevalence study including six European countries, AN 0.48%, BN 0.51%, and BED 1.12% were found.Citation38 Therefore, working with larger numbers of patients would probably be more indicative because of the small percentage of real EDs in the general population.
These data raise another question as to why psoriatic patients have EDs. The explanation comes from increased psychiatric comorbidity, in particular depression and anxiety, in psoriatic patients.Citation14,Citation15 There are some reports that indicate a link between ED and stress factors including anxiety and depression.Citation20–Citation22,Citation35 This means that, in particular, anxiety associated with psoriasis may cause abnormal eating habits and resultant MBS in psoriasis. In a study conducted by Herron et al obesity was suggested as a consequence of psoriasis and not a risk factor for onset of disease.Citation14 Accordingly, the authors of this present paper suggest that the interaction between psoriasis, psychiatric symptoms, and EDs may lead to obesity or MBS over time; that these current results showed higher mean age in MBS may reinforce this speculation.
According to this study’s findings, clinical severity of psoriasis measured by PASI seems to be an independent variable in the relationship between EDs, MBS, and anxiety.
Conclusion
In conclusion, it appears that it is not adequate to establish the presence of comorbidities alone; defining risk factors leading to comorbidities is also important in patients with psoriasis. If causative factors are detected, controlling them by a multidisciplinary approach will prevent the onset of comorbidities and also provide both cost-effective and satisfactory management of psoriasis.
Disclosure
The authors report no conflicts of interest in this work.
References
- NickoloffBJThe immunologic and genetic basis of psoriasisArch Dermatol19991351104111010490116
- SommerDMJenischSSuchanMIncreased prevalence of the metabolic syndrome in patients with moderate to severe psoriasisArch Dermatol Res200629832132817021763
- GisondiPTessariGContiAPrevalence of metabolic syndrome in patients with psoriasis: a hospital-based case-control studyBr J Dermatol2007157687317553036
- AlsufyaniMAGolantAKLebwohlMPsoriasis and the metabolic syndromeDermatol Ther20102313714320415820
- Al-MutairiNAl-FaraqSAl-MutainComorbidities with psoriasis: an experience from the Middle EastJ Dermatol20103714615520175849
- ChristophersEComorbidities in psoriasisClin Dermatol20072552953418021889
- KimNThrashBMenterAComorbidities in psoriasis patientsSemin Cutan Med Surg201029101520430302
- GuenterLGulliwerWPsoriasis comorbiditiesJ Cutan Med Surg200913877887
- WilsonPWD’AgostinoRBPariseHMetabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitusCirculation20051123066307216275870
- EckelRHAlbertiKGGrundySMThe metabolic syndromeLancet201037518118320109902
- WannametheeSGShaperAGLennonLMetabolic syndrome vs Framingham Risk Score for prediction of coronary heart disease, stroke and type 2 diabetes mellitusArch Intern Med20051652644265016344423
- RoehringMMashepMRWhiteMAGriloMCThe metabolic syndrome and behavioral correlates in obese patients with binge disordersObesity20091748148619219063
- GuerdjikovaAIMcElroySLKotwalRKeckPEJrComparison of obese men and women with binge eating disorder seeking weight managementEat Weight Disord2007121923
- HerronMDHinckleyMHoffmanMSImpact of obesity and smoking on psoriasis presentation and managementArch Dermatol20051411527153416365253
- HavesJKooJPsoriasis: depression, anxiety, smoking and drinking habitsDermatol Ther20102317418020415825
- KurdSKTroxelABCrits-ChristophPThe risk of depression, anxiety and suicidality in patients with psoriasis: a population-based cohort studyArch Dermatol201014689189520713823
- VaagABrønsCApelJSMetabolic consequences of overeatingUgeskr Laeger200616818318716403347
- HudsonJILalondeJKCoitCELongitudinal study of the diagnosis of components of the metabolic syndrome in individuals with binge-eating disorderAm J Clin Nutr2010911568157320427731
- HerpetzSAlbusCWagenerRComorbidity of diabetes and eating disorders. Does diabetes control reflect disturbed eating behavior?Diabetes Care199821111011169653604
- BulikCMSullivanPFFearJLEating disorders and antecedent anxiety disorders: a controlled studyActa Psychiatr Scand1997961011079272193
- GodartNFlamentMCurtFAre anxiety disorders more frequent in subjects with eating disorders?Ann Med Interne2003154209218
- BlinderBJCumellaEJSanatharaVAPsychiatric comorbidities of female inpatients with eating disordersPsychosom Med20066945446216738079
- GarnerDMGarfinkelPEThe eating attitudes test: an index of the symptoms of anorexia nervosaPyschol Med19799273279
- ErolNSavaşırIEating attitude test: index of anorexia nervosa symptomsTurkish Journal of Psychology198923132136 [In Turkish, English abstract.]
- BeckATWardCHMendelsonMAn inventory for measuring depressionArch Gen Psychiatry1961456157113688369
- HisliNReliability and validity study of Turkish version of Beck depression inventoryTurkish Psychol J19886118122
- BeckATEpsteinNBrownGAn inventory for measuring clinical anxiety: psychometric propertiesJ Consult Clin Psychol1988568938973204199
- UlusoyMErkmenHşahinNTurkish version of the Beck anxiety inventory: psychometric propertiesJ Cogn Psychother199812163172
- American Psychiatric AssociationDiagnostic Statistical and Manual of Mental Disorders4th edWashington, DCAmerican Psychiatric Association1994
- HudsonJILalondeJKBerryJMBinge-eating disorder as a distinct familial phenotype in obese individualsArch Gen Psychiatry20066331331916520437
- DanielssonAFagerholmSOstAShort-term overeating induces insulin resistance in fat cells in lean human subjectsMol Med20091522823419593406
- VillagomezLCortesJBarreraEComorbidity of obesity and eating behaviour disordersRev Invest Clin20035553554514968475
- TaylorAEHubbardJAndersenEJImpact of binge eating on metabolic and leptin dynamics in normal young womenJ Clin Endocrinol Metab19998442843410022396
- KralJGBuckleyMCKissileffHRMetabolic correlates of eating behavior in severe obesityInt J Obes Relat Metab Disord20012525826411410829
- SwansonCACrowSJLe GrangeDPrevalence and correlates of eating disorders in adolescents: results from the national comorbidity survey replication adolescent supplementArch Gen Psychiatry20116871472321383252
- MondJMArrighiAGender differences in perceptions of the severity and prevalence of eating disordersEarly Interv Psychiatry20115414921272274
- MammenPRussellSRussellPSPrevalence of eating disorders and psychiatric comorbidity among children and adolescentsIndian Pediatr20074435735917536137
- PretiGGirolamoGVilagutGThe epidemiology of eating disorders in six European countries: results of the ESEM Ed-WMH projectJ Psychiatr Res2009431125113219427647