Abstract
Dermal filler treatments require constant reassessment for improving and safeguarding the rapidly evolving aesthetic field. Suboptimal injection technique, patient selection and product knowledge have touted a concerning increase in filler complications, with new challenges such as the COVID-19 pandemic leading to new paradigms in the understanding, prevention, diagnosis and treatment of complications. The updated 10-point plan has been developed to curtail complications through consideration of causative factors, categorized as patient, product, and procedure-related. Patient-related factors include a preprocedural consultation with careful elucidation of skin conditions (acne, rosacea, dermatitis), systemic disease (allergies, autoimmune disease, underlying bacterial and viral disease (herpes simplex virus, COVID-19 infection), medications (antineoplastic drugs, recreational drugs) and previous cosmetic procedures (including fillers and energy-based devices). Patient assessment should include standardized photography and also evaluate the role of social media, ethnicity, gender, generational, and LGBTQ+ needs. Specified informed consent for both adverse events and their treatment is essential due to the increase in vascular complications, including the risk of blindness. Product-related factors include the powerful advantage of reversibility when using hyaluronic acid (HA) products. Product characteristics such as molecular weight and filler degradation should be understood. Product layering over late or minimally degradable fillers is still inadvisable due to the initial filler being teased into reactivity. Procedural factors such as consistent photographic documentation, procedural planning, aseptic non-touch technique (ANTT), knowledge of topographical anatomy and angiosomes, and technical dexterity including pinch anatomy and needle skills are of pivotal importance. The final section is dedicated to algorithms and checklists for managing and treating complications such as allergic hypersensitivity reactions, vascular events, infection, edema and late-onset adverse events (LOAEs). The updated 10-point plan is a methodical strategy aimed at further minimising the risk of dermal filler complications.
Introduction
The exponential increase in the use of injectable fillers has heralded unique safety requirements, mandating ongoing reappraisal of both procedural method and complication management.
As with the initial 10-point plan for avoiding hyaluronic acid dermal filler-related complications during facial aesthetic procedures and algorithms for management,Citation1 this updated plan aims to establish a simple, user-friendly checklist for optimising patient factors, practical product knowledge and safer technique. Updated treatment and safety algorithms have been added in a visual format (, Figure 21, 22, 23).
Table 1 A 10-Point Plan for Avoiding Filler Complications
Patient-Related Factors
History and Selection
Frequently queried selection criteria include the following:
The Neoplastic Process and Antineoplastic Drugs
Filler safety is frequently queried in patients with cancer or on antineoplastics, cytotoxics, biologicals, or immunotherapy (). Conversely, the influence of fillers on the incidence, behavior, or aggravation of malignant tumors has been questioned, with the rapidly evolving field of onco-immunology raising awareness around immunity, chronic inflammation, carcinogenesis, and the effects of antineoplastic therapy.Citation2
Table 2 Selection Criteria
Physicians should, however, consider the cumulative psychological burden of altered physical appearance, loss of identity, helplessness to change, and subsequent impact on immunity. Oncologic patients are often concerned about their appearance and fear pitying remarks from outsiders regarding their overall physiognomy. Wearing a cap or a headscarf to hide chemotherapy induced alopecia is an example of the former. Often patients are strongly insistent on maintaining regular aesthetic treatments in order to avoid the perception of suffering or losing their attractiveness. Therefore, the psychological benefits of aesthetic treatments often transcend their potential fear.Citation3 Importantly, risks should be consented upfront.
Active chemotherapy is an accepted contraindication to fillers, with significantly delayed long-term immune changes documented 12 months post-treatment and at least 6–10 months after completing adjuvant therapy for breast cancer.Citation4 Early recovery phases are prone to viral reactivation, with increased bacterial infections during later stages and slower recovery in smokers.Citation5
Increasingly, antineoplastic immunotherapy is causing a unique spectrum of immune-related adverse events. Immune checkpoint inhibitors (ICI)Citation6 remove the brake on activated T-lymphocytes, enabling T-cell attack on normal cells. LOAEs are documented after ipilimumabCitation7,Citation8 and cetuximab,Citation9 and facial swelling and granulomatous reactions with protein-tyrosine kinase inhibitors. However, uneventful HA filler treatment has been described after treatment with imatinib mesylate.Citation10
Carboxymethylcellulose-polycaprolactone, and polylactic acid fillers may induce LOAEs mimicking tumors after nivolumab (ICI), causing staging difficulties on PET-CT scans.Citation11,Citation12
During immunotherapy, filler treatments should preferably be postponed, with vigilant follow-up in patients insisting on psychologically motivated treatments. Standard antibiotic and intralesional steroid treatment of LOAEs is permissible, while oral steroids are contraindicated due to potential interruption of immunotherapy.
The immunological effects of radiotherapy and paradoxical effects of immune stimulation or suppression vary with individual regimes.Citation13 Although no discrete guidelines exist, it is advisable to consider post-radiotherapy patients as being immunosuppressed and to delay fillers for at least 6–12 months.
Physician discretion and vigilant follow-up are advocated in situations where fillers may offer much-needed psychological support after treatment of neoplastic disease.Citation3
In contrast to a 2010 study inferring chronic inflammatory or neoplastic changes due to the pro-inflammatory properties of “low molecular” HA molecules, other reports have queried the actual presence of HA fragments and highlighted varying definitions of “low molecular weight” fragments. (Table 7).Citation14,Citation15
A single anecdotal case has posed a hypothetical correlation between a cutaneous metaplastic synovial cyst and facial HA injections.Citation16 However, large long-term cohort studies demonstrating extensive pharmaco-vigilance have failed to correlate neoplasia with either single or repeated facial HA filler injections.
Autoimmune Collagen Disease: Lupus, Morphea and Systemic Sclerosis
Previous recommendation has been for filler avoidance during active phases of collagen disease, whilst stable or burnt-out disease phases may be treated with relative safety.
Two recent literature reviews state that patients with autoimmune conditions may be safely treated with a variety of fillers.Citation17,Citation18 During active disease stages, we still advise against filler treatments.
Recreational Drugs
Nicotine and recreational drugs such as marijuana, cocaine, and opiates not only alter neuropsychological and pathophysiological responses but also inhibit immune function through direct and indirect mechanisms enhancing susceptibility to infections ().Citation19
The potential effect on tissue response, healing, and onset of adverse events should not be overlooked. The negative effect of smoking on cancer rehabilitation is well documented.Citation20
Drug Interactions
LOAE protocols may recommend antibiotics or anti-inflammatories prone to drug interactions involving especially hepatic cytochrome P-related medications (eg, clarithromycin, erythromycin, celecoxib, diclofenac) necessitating careful documentation of prior drug intake.
Genetic Predisposition to Immune-Mediated Adverse Reactions, and Genes Within the Major Histocompatibility Complex
Upfront screening for a propensity to LOAEs, although not currently feasible, would be ideal. In addition to speculation around HLA B*08 and DRB1*03 – subtypes in immune-mediated disorders affecting women with silicone breast implants, Decates et al also examined the major histocompatibility haplotypes in 211 patients where 129/211 demonstrated LOAEs after fillers. A significant correlation was demonstrated between the combined presence of HLA B*08/DRB1*03 and inflammation, with an almost 4-fold increase in immune-mediated adverse events (odds ratio = 3.79, 95% CI 1.25–11.48).Citation18
HLA subtyping poses future possibilities for pre-identifying individuals at risk of delayed reactions.
Our recommendation is for avoidance of fillers in patients with this specific combination of HLA subtypes (B*08 and DRB1*03).
Pregnancy and Lactation
Medicolegally, insufficient procedural or drug-related safety data mandate against use during pregnancy, intended pregnancy, or breastfeeding. Due to the paucity of data and unpredictability of complications and their management, fillers are deemed inadvisable during pregnancy or lactation.Citation21 Should a patient fall pregnant shortly after treatment, no specific action other than routine follow-up is needed.
Previous LOAEs
The safety and timing of re-treatment after previous LOAEs is often questioned. Importantly, previous triggers such as acne, dental procedures, sinusitis, gastroenteritis, flu-like illness, vaccinations or causes of compromised skin barrier should be managed upfront. A recent review cites the majority of patients re-treated with a similar filler product having an uneventful course.Citation22
The authors suggest at least one month between full clearance of LOAE and re-treatment to exclude transient clearance on steroids or antibiotics. For medicolegal purposes, an intradermal test with 0.1ml of the intended product may be performed and checked after 1 and 3 months ( and ).
Energy-Based Devices (EBD)
EBD treatments are best avoided in areas overlying LOAEs as they invariably impact skin barrier function and may act as external trauma triggers or induce infection in predisposed patients. Radiofrequency treatment (RF) has been documented to result in statistically significant increases in inflammatory, foreign body, and fibrotic responses associated with fillers despite histological absence of immediate thermal effect following RF ().Citation23 The use of microneedle RF over recently placed filler should be approached with caution.Citation24
Skin Barrier Function, Infection, and Treatment Timing
Importantly, skin barrier function may be altered for 3–4 weeks after apparent clearing of conditions such as dermatitis.
Active rosacea implies increased vascularity, impeded barrier function, and antimicrobial peptides, generally taking 12 weeks to stabilize.Citation25 Perioral dermatitis should be pre-treated to full clearance, generally necessitating 6 weeks.
Patients with underlying Staphylococcus aureus carrier status may be treated topically with intranasal mupirocin bd x 5 days, alternatively topical neomycin and bacitracin, chlorhexidine, or bleach baths.Citation26
Herpes simplex (HSV) lesions are infective until disappearance of the last crust. To prevent eczema herpeticum, particularly in patients with a history of or active atopic dermatitis, HSV is best treated prophylactically for 5 days starting one day pre-treatment, particularly when injecting close to HSV areas. Acyclovir (ACV) and related nucleoside analogs (valacyclovir or famciclovir) have long been a gold standard. However, the rapid emergence of ACV-resistant HSV, combined with increasing transplant and cancer patient numbers, mandates a careful treatment history despite this not representing the usual injectable patient cohort.Citation27
Covid Infection
LOAEs following influenza-like viral illnesses are documented after treatment with various HA filler brands. The current global COVID-19 SARS 2 pandemic has led to similar reaction patterns, with several publications detailing LOAEs after HA fillers.Citation28–Citation30
The COVID-19 SARS-2 spike protein interacts with dermal angiotensin-converting enzyme receptors (ACE2) which normally regulate the homeostasis between angiotensin 2 (pro-inflammatory) and angiotensin 1 (anti-inflammatory). This induces a pro-inflammatory, loco-regional TH1 cascade thought to promote a CD8+T cell-mediated reaction to incipient granulomas previously formed around residual HA particles.Citation29
Covid Vaccinations
As seen in the ASIA (Autoimmune/inflammatory syndrome induced by adjuvants) syndrome, vaccinations may trigger immunological hypersensitivity cascades with subsequent LOAEs.Citation31 Not surprisingly, LOAEs have indeed been reported after various COVID-19 SARS 2 vaccine brands.Citation29 Multiple clinical manifestations ranging from edema, erythema, swelling and tenderness to subsequent painful, indurated plaques and nodules have been documented in patients with fillers placed from weeks to years before either a first or second Covid vaccination.Citation30
Evolving COVID-19 vaccination protocols may well become one of the most common triggers of subsequent HA filler-associated LOAE, with the triad of increasing filler use, escalating COVID-SARS-2 infection rates and progressive vaccine roll-out recently cited as potentially portending a perfect storm.Citation29
Interestingly, ACE inhibitors such as lisinopril have anecdotally been found beneficial in reducing vaccination-induced LOAEs, with lisinopril proposed as pre-vaccination medication in patients prone to LOAEs after HA fillers, or having developed LOAEs following first vaccinations.Citation32 Currently, no controlled study is available to prove either large-scale benefit or the benefit following non-HA fillers. As cited in recent publications, oral corticosteroids constitute initial one-month therapy for Covid vaccination-related LOAE therapy for Covid vaccination-related LOAE.Citation29,Citation30
Patient Expectations and Psychological Screening
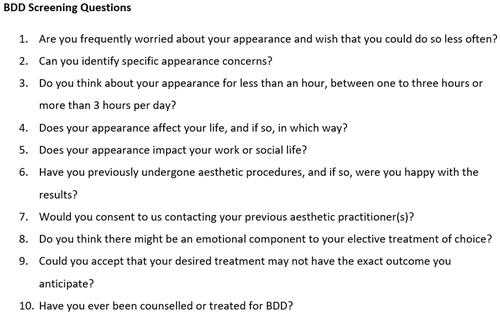
Body dysmorphic disorder (BDD) often presents with cosmetic complaints and higher pre-procedural expectations (). Psychopathology or unrealistic expectations regarding enhanced quality of life (QOL), self-esteem, social interactions or facial beauty should be excluded upfront due to decreased procedural satisfaction.Citation33
Table 3 Body Dysmorphic Disorder (BDD)
Patient questionnaires may serve as valuable screening tools. Concerning answers to the questions in Figure 5 merit completion of a more extensive BDD questionnaire or referral for psychological evaluation ().Citation34
Figure 5 Valuable BDD screening questions. Note: Data adapted from Krebs et al.Citation34
Assessment
Generation
Baby boomers (in their 60s) and Gen Zs (born 1994-) currently comprise the largest aesthetic market segments, mandating an understanding of specific needs.Citation35 Aesthetic education of younger generations also bears long-term implications for future patient loyalty. The expert injector’s role lies in communicating insightful facial analysis despite the increasing challenge of selfies, photographic distortion and social media pressure. A systematic analysis of all facial angles, both in repose and animation, helps to establish expertise through irrefutable clinical logic.
Social Media and Aesthetic Self-Perception
Obsessive selfie-taking, classified by the American Psychiatric Association as a mental disorder associated with low self-esteem, is ascribed to social competition, attention-seeking, mood modification, self-confidence and social conformity, consequently initiating the development of a psychometric Selfitis Behavior Scale (SBS).Citation36
Selfie-filters may encourage unrealistic expectations through complexion enhancement and altered features such as erased nasolabial folds, tighter jawlines, and bigger lips. Furthermore, normalization of pouting poses has blurred the boundaries between resting and dynamic lip proportions, complicating realistic volume expectations. Only 60–65% of real-world images are differentiated from manipulated images, further encouraging manipulation.Citation37
Importantly, social media has significantly altered the concept of patient confidentiality, with patients increasingly keen to publicize treatment experiences.
The current COVID-SARS2 pandemic has fuelled further perceptual change as remote living and working have forced individuals to view themselves on-screen, unedited, in motion and at the mercy of short focal length webcams. The resulting “zoom face” inevitably depicts a more rounded face, wider set eyes and broader nose, creating a flawed representation of reality which patients struggle to process.Citation38
Ethnicity
Asian and African beauty concepts may differ fascinatingly from Caucasian ideals, with perceptions increasingly influenced by the advent of social media and “beauty influencers” ().Citation39 Whilst the traditional African beauty concept has shifted to more Westernized ideals, with an increasing desire for lower body mass and paler, yellowish skin tone, Chinese aesthetic patients demonstrate a strong desire for retained ethnic identity. A Singaporean study comparing Caucasian and Chinese aesthetic patients demonstrated that Chinese patients were younger and more likely to seek correction or more obvious changes than Caucasian patients. On multivariate analyses, powerful predictors for proceeding with non-invasive facial treatments included rejuvenation rather than correction as a goal, an expectation of an immediate result, and prior aesthetic treatments.Citation40
Table 4 Ethnicities: Features and Management
The expert injector should understand not only universal, cross-cultural beauty ideals, but grasp applicable ethnic nuances.
Asian
Asian faces have unique facial proportions, beauty concepts, aging stigmata, and cosmetic demands.Citation40 The frequent need for centro-facial treatment with higher injection volumes merits highly specialized skills and carries a higher risk of intravascular embolic events.
Indian
The Indian face is particularly prone to developing early periorbital hyperpigmentation and infraorbital hollowing, with tear trough deficiency the most common filler request between 20 and 40 years.Citation41 Malar volume loss and jowling are common in older individuals, with excess medial soft tissue on a relatively smaller midface mandating initial treatment of lateral vectors to create adequate lift without excess medial volume. The shorter, wider lower face requires 3-dimensional correction and chin augmentation to achieve optimal facial height and the desired oval shape.
African
Despite escalating demand, few discrete guidelines exist for African phenotypes. Key considerations include a tendency to scarring, keloids or post-inflammatory hyperpigmentation (PIHP).Citation39 Mild and transient hyperpigmentation after nasolabial fold HA fillers in Fitzpatrick Skin Types (FST) IV–Vl is cited in 2–17% of patients (6% of injection sites). Serial punctures, superficial injection depth and fast injection speed predispose to PIHP. Whilst a 27G needle should pose no significant risk of PIHP or keloid formation, a test area with a small 31/33-gauge needle is suggested when in doubt. Keloid tendency is linked to chromosome band 7p11 and the EGFR gene.Citation42
LGBTQ+ Population
When performed with a clear understanding of male and female features and desired outcomes, facial procedures may greatly enhance overall QOL. Hormonal therapy, especially whilst transitioning from female to male, may induce acne which should be optimally treated before attempting fillers.Citation43
Clinic staff should be trained in using preferred pronouns and identifiers when addressing transgender patients, whilst intake forms should request “gender” rather than “sex” and include a write-in option for “other.”
Facial Dynamics
Insightful understanding of functional anatomy, synergistic and antagonistic muscle balance and both the direct and indirect effects of fillers are essential for natural dynamic outcomes. These principles also underlie the rehabilitation of facial palsy through injectables.Citation44,Citation45
Filler placement may modify muscle behaviour through:
Stretching muscles to improve tensile strength.
Expanding the submuscular aponeurotic system (SMAS).
Providing a mechanical block via intramuscular injection.
Inducing resistance or support through differential placement above or below the muscle.
Consent
Although rare, the potential for allergic reactions, infection, vascular incidents, visual loss, and LOAEs must be stipulated on consent forms and explicitly discussed with the patient.Citation46 Particular care should be exercised when consenting patients with cancer, on antineoplastic treatment or BDD. Importantly, to circumvent treatment delays, upfront consent should be obtained for managing potential complications. Additionally, in certain countries, the aesthetic use of hyaluronidase is off-label and should be clarified.Citation47
The Covid-era has necessitated a new subset of regulations, as well as the initiation of conversation around potential vaccination sequelae. As cutaneous implications of both COVID-19 infection and vaccination emerge, cosmetic patients may benefit from a discussion around COVID-19 vaccine-related planning as a part of pre-procedure counselling for dermal fillers. In the absence of final data, we provisionally suggest waiting 2 to 4 weeks between filler injections and vaccination, with an even longer window in patients with a higher risk profile for developing reactions.Citation32
Upfront financial consent remains mandatory.
Product
Reversibility
The widespread use of HA fillers is driven by the unparalleled advantage of reversibility through hyaluronidase (). Despite a consensus paper advocating hyaluronidase for calcium hydroxylapatite (CaHa)-induced vascular occlusion due to its anti-edematous and anti-inflammatory properties, it does not dissolve the culprit. While a recent proof-of-concept study has demonstrated potential reversibility of CaHA through intralesional sodium thiosulfate (STS),Citation48 optimal injection concentration, treatment ratio, time to onset, ability to pass through intact vessels, and treatment efficacy for established nodules are still unknown.Citation49,Citation50
Table 5 Hyaluronidase Safety Aspects
A human cadaver study has demonstrated a very limited in vitro potential of STS to dissolve intraarterial CaHa after submerging CaHa-filled arterial segments in varying concentrations of STS.Citation50
Hyaluronidase: Practical Aspects
A 3-fold difference has been cited in the required number of hyaluronidase units per HA volume, with dissolution times varying from 2 to 16 minutes per 0.1 mL aliquot. This underscores the need for knowledge regarding the efficacy of locally available hyaluronidase on preferentially used HA products ().Citation51
Table 6 Hyaluronidase Practical Aspects
Product Characteristics
Molecular Weight, Inflammatory Response and Autoimmunity
Although HA has been cited as a potential trigger factor for the ASIA syndrome, recent publications maintain that carbohydrates induce poor antibody responses due to their antigenic incapacity to stimulate T cell responses (). Carbohydrates preferentially bind to membrane receptors such as immunoglobulins to induce clustering and primary B cell activation, stimulating production of low affinity, short-living IgM, and no induction of memory effect in the absence of T cells.Citation52,Citation53
Table 7 Definitions
Conversely, bacteria act as potent activators of the TLRs (1,4,5,7,9) to induce inflammation, innate immunity, and non-agent-specific autoimmunity (). This underlines the critical importance of aseptic technique in avoiding late-onset inflammatory and immune sequelae.Citation31,Citation54 In genetically predisposed patients or specific HLA types, inflammasomes are triggered, possibly through an adjuvant role of ionized molecules.
Table 8 HA Filler Degradation
Importantly, acne is present in 10% of the population. Cutibacterium acnes (C.acnes) has a strong immunostimulatory capacity, is found in all stages of acne, and binds to the cytoplasmic nucleoside-binding oligomerization domain-like (NOD-like) receptors to induce inflammasomes and opportunistic infections, thus stimulating both innate and adaptive immune responses.Citation55,Citation56 The “safe injection distance” from individual acne lesions is currently unknown and adequate pre-treatment is mandatory.
Product Layering
Whilst Alijotas-Reig et al initially posed the increased risk of immune-mediated adverse reactions after consecutive injection of different fillers, a subsequent review of 260 cases found no increased risk of local or systemic reactions after repeated injections of different fillers in the same or different sites. When occurring, however, they were more likely to become chronic, systemic, and severe.Citation31
Layering fillers over late or minimally biodegradable products is still deemed inadvisable due to the initial filler being teased into reactivity, which may be histologically proven.Citation57,Citation58
In cases of unknown previous fillers, and to determine the precise nature of fillers, ultrasound may offer a valuable diagnostic tool.Citation59,Citation60
Injection Depth and Immunological Response
Despite questions posed around the differential immunological response with filler depth and subsequent impact on immunologically induced LOAEs in the Covid-era, no data is currently available for risk stratification of intradermal vs deep tissue injections.
Procedure
Photography
Consistent Positioning
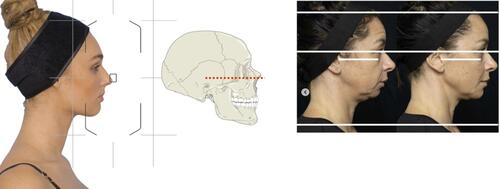
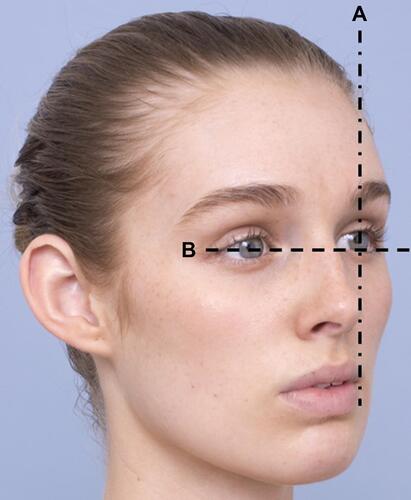
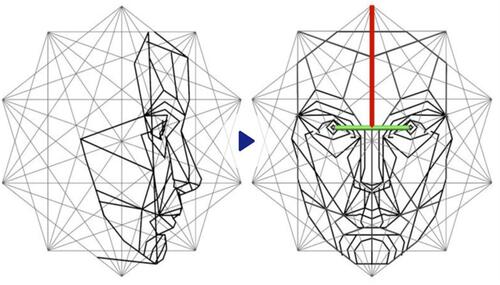
Accurate clinical photography, at rest and in animation, is vital for facial analysis, learning curves, and medicolegal purposes. Common consistency pitfalls include inaccurate positioning in the lateral and oblique views, which are avoidable by adhering to basic tenets. Position accurately for lateral views by using the Frankfort Line, thus also facilitating correct angulation for oblique views, in which all 4 canthi should be visible (–).
Figure 6 Frankfort horizontal plane vs natural head position.
Photographic Distortion
Due to photographic distortion, mobile photos are inadequate for clinical use.
Selfies taken from a distance of 12 inches increase nasal size by 30% in males and 29% in females, with distortion of the perceived ratio of nasal breadth to bizygomatic width and inaccurate 3-dimensional appearance. Images taken at standard portrait distance render accurate proportions ().Citation61
Figure 9 Selfie distortion: the effect of focal length, illustrating wide angle (28mm) distortion as seen with mobile photography. Note: Image courtesy of Dr Heydenrych.
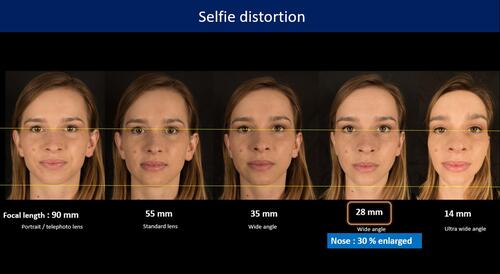
Further studies are needed to establish the role of frequent selfies in increased patient dissatisfaction, and the impact of selfie distortion on future medical decisions.Citation62 Recently, the COVID-SARS −2 pandemic has provoked a surge in patients citing their appearance on virtual platforms as the reason for seeking care, particularly concerning acne and wrinkles.Citation38 The patient is now also the viewer!
When available, computerized photography systems may add additional consistency and finesse to accurate and academic documentation.
Procedural Planning and Aseptic Technique
Aseptic Non Touch Technique (ANTT)
Vigilant aseptic technique is critical in the light of normal non-sterile office circumstances. Most sterility breaches have been proven to occur during the initial procedural phase, mandating pre-planning of product, volumes, and instruments of choice.Citation47,Citation63
Mucosal Cleansing Agents
Whilst chlorhexidine has previously been widely regarded as a good oral antiseptic, the Covid-era has raised new challenges. Preferred alternatives include Na hypochlorite, 1% peroxide, povidone-iodine, cyclodextrin, and succinic acid, with routine oral rinses (2 × 30 seconds) before fillers to decrease viral load.Citation64,Citation65
Anatomy
Intravascular injections, with consequences ranging from tissue necrosis to blindness, constitute the most feared injectable complications. Whilst topographical vessel course is varied (“x and y” axes in graph analogy), vessel depth (“z” vector) is far more predictable, thus bearing great significance in avoiding filler embolism. “Injection anatomy” commonly refers to surface markings in relation to the depth of underlying vital structures.
For effective localization of adjacent vasculature, topographical points are best marked with the patient in the upright position. Important pre-procedural markings may be seen in – and discussed in .
Figure 10 Topographical markings of foramina in anterior view. Note: Image courtesy of Dr Heydenrych.
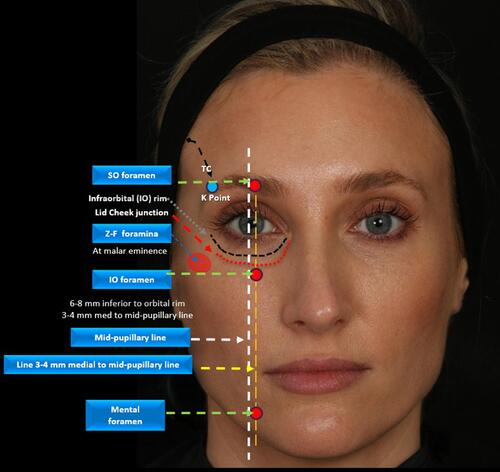
Figure 11 Oblique view illustrating topographical markings of bony landmarks and adjacent danger areas. Note: Image courtesy of Dr Heydenrych.
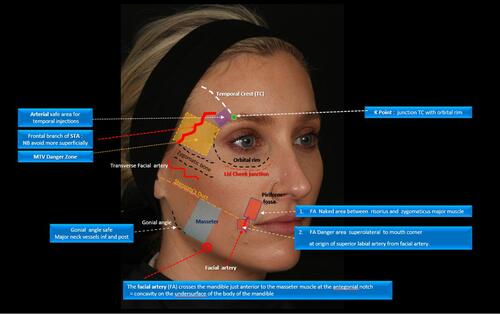
Figure 12 Temporal venous danger zone delineated by the upper margin of the zygomatic bone and a parallel horizontal line running from the K Point, at the junction of temporal crest (TC) and lateral orbital rim.
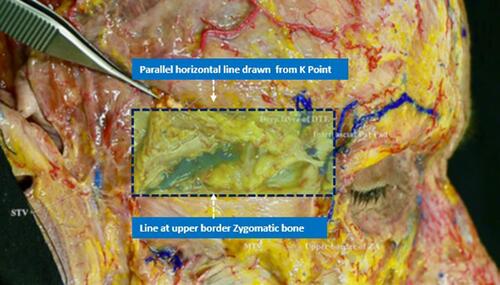
Table 9 Ten Topographical Tracings
Facial Artery Course
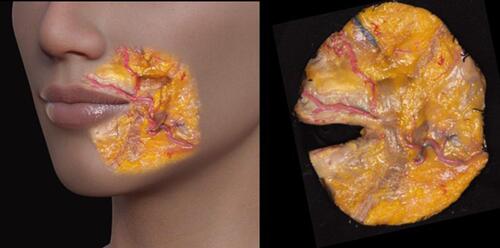
The facial artery (FA) crosses the mandible at the antegonial notch just anterior to the anterior border of the masseter, before traveling superomedially, lateral to the modiolus, towards the piriform fossa. Between the risorius and zygomaticus major, it lies coiled and unprotected by muscle cover (“naked”), meriting injection caution. A second naked area lies superolateral from the mouth corner, medial to levator anguli oris (LAO), where the superior labial artery arises from the facial artery. The FA more frequently runs medial to the NLF, starting 1.7 mm medial in the lower portion, crossing beneath the fold at a depth of 5 mm at the superior third, and eventually reaching a point 3.2 mm lateral to the nasal ala ().
Figure 13 Naked areas of facial artery. Notes: Reproduced with permission from Pirayesh A, Bertossi D, Heydenrych I, editors. Aesthetic Facial Anatomy Essentials for Injections. Boca Raton: CRC Press; 2020.Citation66 Copyright 2020 Taylor & Francis.
Pinch Anatomy
Pinching with the non-dominant hand may serve as injection guide for avoiding inadvertent intravascular placement during temporal fossa injections through altering the tissue layer ().Citation67
Table 10 Differences Between “Gentle Pinch” and “Deep Pinch” with Non-Dominant Hand During Temporal Injection
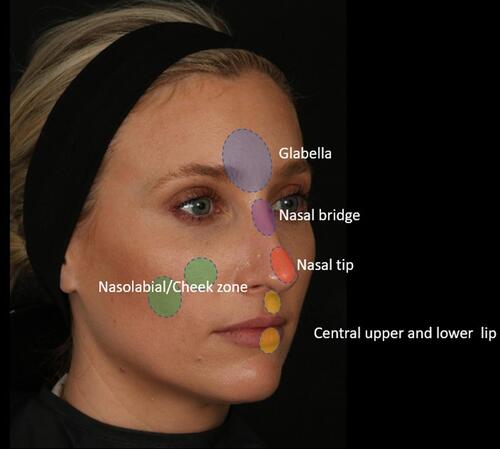
Functional Vascular Anatomy (Angiosomes)
The skin’s three-dimensional functional angiosomes are supplied by a single source vessel and bordered by an anastomotic perimeter of either true or choke anastomoses.Citation68 Whilst extravascular HA is well tolerated, intravascular placement induces severe vessel wall inflammation, predisposing to embolism. Pain may be a warning symptom even in the absence of cutaneous blanching but is not always present. Choke vessels respond with spasm to control or prevent flow across angiosome boundaries, impacting HA spread and necrosis of adjacent angiosomes. Vascular complication sites fall within five specific choke angiosome territories of the facial, ophthalmic, maxillary, and superficial temporal arteries and may sometimes be remote from the primary injection site ( and ).Citation69 These sites are the:
Glabella
Nasal bridge
Nasal tip
Central upper/lower lips
Nasolabial/cheek zone
Figure 15 Vascular occlusion illustrating choke anastomotic distributions. Note: Images courtesy of Dr K De Boulle.

Figure 16 Vascular obstruction: 60 IU hyaluronidase under ultrasound guidance (A) pre-Rx (B) 2h post -Rx (C) 1-week post- Rx. Yellow circle denotes injection area. Note: Images courtesy of Dr Stefania Roberts.

Scant upper facial and periorbital venous valves may cause arteriovenous shunting after choke vessel spasm, with resultant embolization to the ophthalmic vein, cavernous sinus, and brain.
True anastomoses, in contrast, link adjacent territories without caliber loss to potentially allow unimpeded embolic passage to remote or contralateral facial sites.Citation69 Three common true anastomotic connections are:
Angular artery with dorsal nasal or supratrochlear artery
Across nasal tip
Across upper or lower lips
When injection pressure is lower than systemic arterial pressure, anterograde vascular occlusion causes downstream flow to vascular tributaries, resulting in predominantly skin surface changes. Displacement against arterial blood flow causes retrograde vascular occlusion, with emboli traversing back to a vascular bifurcation to cause anterograde occlusion in more posterior locations upon stabilization of arterial pressure, effecting more distal capillary non-perfusion.Citation70
Nitroglycerin Paste During Vascular Occlusion
A recent overview advocates the adjuvant use of nitroglycerin in pending vascular occlusion.Citation71 However, choke vessel spasm is deemed a major determinant for the location and extent of tissue necrosis and because nitroglycerin paste may induce choke vessel dilation to alleviate flow-limiting spasm, allowing expansion of the number of affected angiosomes and increasing the area of tissue necrosis, the use of nitroglycerin paste is discouraged.Citation69
The Use of Diagnostic Ultrasound
Although technically intricate, accurately performed and interpreted ultrasound may offer a valuable risk reduction tool during blinded injection procedures ( and ).Citation59
Uses include:
Upfront vessel localization for prevention of intravascular injection:Citation54
Localization and treatment of acute vascular occlusion:
The amount, location, and depth of injected HA fillers may be identified, enabling targeted delivery of hyaluronidase.
3. Product identification during late-onset events.Citation59
It is advisable to align with an expert referral center in this regard.
Figure 17 Ultrasound-guided Hyaluronidase treatment illustrating resolution of obstruction over 2 minutes (60 IU) Hyaluronidase. Note: Ultrasound images courtesy of Dr Stefania Roberts.
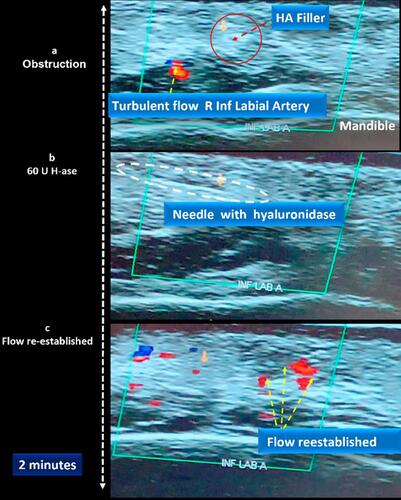
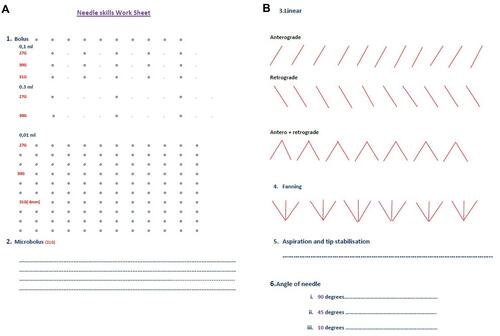
Figure 18 Needle Skills Worksheet. A laminated copy is used for regular extrusion practice utilizing sonar gel/expired products. Proprioceptive memory regarding volume control, needle resistance, and positional angulation may be refined. (A) Refining of volume control (B) refinement of needle course stability and angle.
Technical Knowledge
Unlimited online access to procedural techniques may blur the boundaries between possibilities and capabilities. It is important to grasp that acquiring motor hand skills involves both cognitive spatio-temporal and motoric learning components. Especially during initial learning phases, cognitive representation accrues more rapidly than muscle-specific representations which develop only after extensive practice.Citation72 Attempting injection procedures after online instruction only thus carries inherent risks. Considering the potentially grave sequelae of incorrect placement through minute variations in needle positioning, angulation and plunger control, it has never been more relevant to develop methods for gauging inherent hand skills. Needle skills training forms an integral component of the author’s teaching practice and is useful in refining differential dexterity for controlling factors such as needle position, angle, volume and injection speed ().
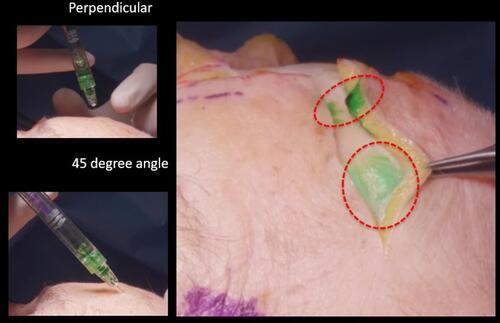
Figure 19 For upper forehead injections, the avascular subgaleal plane may be accessed with needle at 45 degrees to bone. Perpendicular injection may cause bevel height to extend to the vascular supragaleal plane.
Volume and Speed
Dexterous hand control, slow injection speed, and constant vigilance for undue pain which may portend intravascular placement are vital. Watershed perfusion areas such as the glabella or nasal tip should be constantly observed for fleeting blanching, mandating immediate cessation of injection. Blindness has been reported with volumes as low as 0.2 mL of HA filler, whilst 0.085 mL may fill the supratrochlear artery from skin to orbit.Citation73 Large boluses carry a higher risk for biofilm, with recommendation being for bolus size of less than 0.2–0.3 mL.
The Aspiration Controversy
Although the real-time clinical utility of pre-injection aspiration is controversial,Citation74–Citation80 all injectors are ultimately aligned in avoidance of intravascular incidents. No single method guarantees safety, despite individual preference for aspiration or constant needle movement, thus the following should be borne in mind.
Negative aspiration does not guarantee safe injection – slow, careful, low-volume injection is mandatory.
Adequate aspiration time should be allowed (5 −7 seconds).
Waiting times for visualizing flashback may be affected by physiochemical and rheological properties, with some products requiring longer negative pressure.
Not all injectors are equally able to maintain a steady needle position on bone.
Awareness of bevel angle (eg, 45 degrees vs perpendicular) in relation to tissue plane and vascularity is vital.
With the needle in perpendicular position, the bevel tip still may be in a dangerous vascular plane despite a stable needle tip on bone as in the forehead or temple (aSTA).
Intravascular placement is possible with a cannula, especially with < 25G, and in the presence of underlying fibrosis or skin tethering.
Insightful knowledge of vascular anatomy is mandatory, especially pertaining to “z-axis” or vessel depth.
Constant vigilance of watershed areas such as nasal tip and glabella is mandatory as these areas often demonstrate early, fleeting blanching.
Pain is not invariably present with intravascular injection.
Injection Angles vs Placement Depth (Needle/Cannula)
Angulation dictates injection depth and safety, mandating constant awareness (, ).
Table 11 Angles vs Depth (Needle or Cannula)
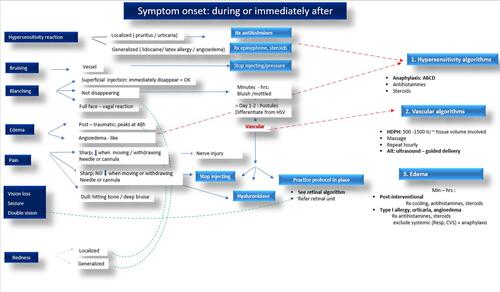
Algorithms and Checklists
A thorough pre- and post-procedural history, with careful clinical examination, should elucidate predisposing factors and facilitate categorization of adverse events. After accurate diagnosis, the majority of problems may be managed through algorithms for:
Allergic hypersensitivity reactions
Vascular events
Edema
Late-onset adverse events (LOAEs)
Early occurring symptoms and algorithms include factors as illustrated in and :
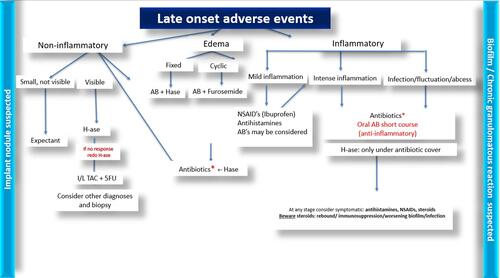
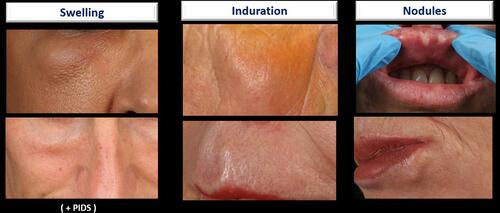
Late occurring adverse events may be classified according to symptoms as non-inflammatory, inflammatory or edema, and treated according to algorithms as shown in . Anatomical factors, such as decreased muscle tonus of the orbicularis oculi, can cause symptoms such as the shelving illustrated in . Edema may have a variable clinical presentation as demonstrated in and be classified according to temporal onset as seen in . Post-procedural swelling () should be clinically differentiated from type 1 hypersensitivity reactions (). Importantly, sterile abscesses may occur either as early or late-onset events, mandating targeted antibiotic therapy with incision and drainage in order to avoid tissue necrosis (). The differential diagnosis of skin discoloration after fillers is varied (). It is critically important to recognize the mottled or livedoid pattern of early vascular occlusion and not to confuse subsequent pustulation with herpes simplex infection.
Figure 21 Late-occurring symptoms of LOAEs.
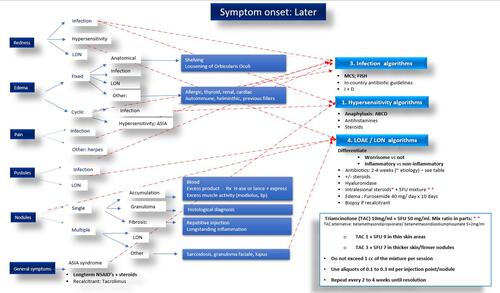
Figure 24 Differential diagnosis of swelling. 1 = edema; 2 = malar edema; 3 = late inflammatory response syndrome; 4 = late onset nodules (LON); 5 = persistent intermittent delayed swelling. Notes: Adapted with permission from Pirayesh A, Bertossi D, Heydenrych I, editors. Aesthetic Facial Anatomy Essentials for Injections. Boca Raton: CRC Press; 2020.Citation66 Copyright 2020 Taylor & Francis.

Figure 25 Temporal onset of post-procedural swelling. Notes: Reproduced with permission from Pirayesh A, Bertossi D, Heydenrych I, editors. Aesthetic Facial Anatomy Essentials for Injections. Boca Raton: CRC Press; 2020.66 Copyright 2020 Taylor & Francis.

Figure 26 Patient demonstrating postprocedural swelling. Note: Image courtesy of Dr De Boulle.

Figure 28 Evolution of a sterile abscess during the first-week post -filler. Rx: targeted antibiotic therapy, with incision and drainage, is vital to prevent tissue necrosis. This presentation may also occur as a late-onset event. Note: Image courtesy of Dr Heydenrych.

Figure 29 Differential diagnosis of skin discoloration: 1. Hematoma; 2. Ecchymosis; 3. Neovascularization; 4. Hyperpigmentation; 5. The Tyndall effect; 6. Ischaemia. Notes: Adapted with permission from Pirayesh A, Bertossi D, Heydenrych I, editors. Aesthetic Facial Anatomy Essentials for Injections. Boca Raton: CRC Press; 2020.Citation66 Copyright 2020 Taylor & Francis.
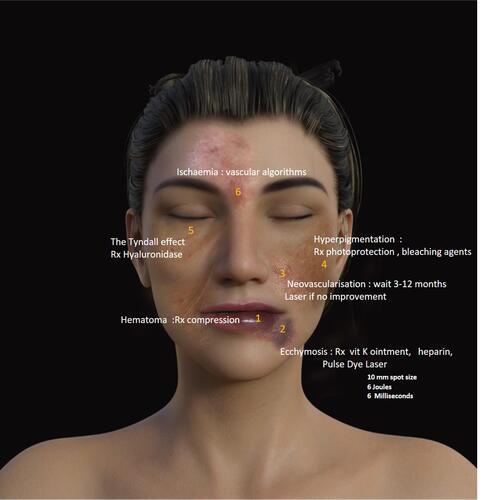
Figure 30 The clinical spectrum of LOAEs includes inflammatory or non-inflammatory manifestations, including swelling, induration, and nodules. Onset is usually after > 4 weeks.
Pre-Treatment Checklist
Country-specific Covid guidelines should be adhered to.Citation81
Post-Treatment Checklist
Patient adherence to the factors as noted in should be encouraged.
Table 12 Suggested Inclusions for Post-Procedure Checklist
Hypersensitivity
Aesthetic practices should be geared for efficient management of hypersensitivity events, albeit rare ().Citation82 Computer reminders are suggested for emergency drug expiry dates.
Table 13 Management of Anaphylaxis with Emergency Crash Cart
Vascular Events
Sufficient hyaluronidase should be available for the management of intravascular events, with high-dose pulse hyaluronidase (HDPH) currently deemed the gold standard (see ). Dosage is according to tissue volume or areas involved. At least 5×1500 IU (or equivalent dosage in other format vials) should be available in-clinic. Check expiry dates.
Table 14 High-Dose Pulse Hyaluronidase (HDPH) for Intravascular Events.
Hyaluronidase treatment for intravascular placement should be instituted as soon as possible, with cut-off time regarded as 4 days. Later treatment options include anti-inflammatory medications, antibiotics, hyperbaric oxygen, and standard wound care.
Visual Complications
There is a paucity of local management guidelines for visual complications after dermal fillers. A recent study cited widespread unawareness of existing protocols despite awareness of the complication in 75% of respondents, underscoring the urgent need for multidisciplinary collaboration and structured protocols.Citation83
In contrast to previous studies, a recent systematic review detailing HA fillers only showed no cases after lower face treatment, with 32/44 events occurring after injection of the glabella and nose.Citation84 Blindness has been reported with volumes as low as 0.2 mL of HA filler, whilst 0.085 mL may fill the supratrochlear artery from skin to orbit.Citation73
Visual loss is often instantaneous and may be painless. Early, accurate documentation of visual signs is mandatory for subsequent decisions in the retinal referral centre ().
Table 15 Prognosis
Treatment
There is currently a lack of indisputable evidence for reversal of injection-related visual compromise (IRVC), with conflicting reports regarding the merits of retrobulbar, supraorbital, and supratrochlear hyaluronidase and an urgent need for multidisciplinary collaboration.Citation85
Many studies are flawed by incomplete documentation. It is imperative that vision is documented upfront in order to establish prognosis.
Neurologic Assessment
Given the 24% incidence of concomitant cerebral involvement, the exact mechanism of which still needs elucidation, a multi-speciality approach including neurological and neurosurgical examination is vital.
Practice Protocol for Injection-Related Visual Compromise (IRVC)
Although no universal protocol exists, factors as noted in should be considered and documented. Upfront medico-legal advice may be advisable.
Table 16 A Suggested Practice Protocol for Managing Ophthalmic Incidents in the Aesthetic Practice
Late-Onset Adverse Events
LOAEs may present clinically as swelling, induration, nodules, or intermittent swelling (persistent intermittent delayed swelling = PIDS) (–).
Figure 31 Patient with LOAE (nodule). Despite lack of improvement on long-term antibiotics, total resolution was affected with colchicine.

Figure 32 Patient with PIDS successfully treated with 0.1 mL of hyaluronidase. Note: Image courtesy of Dr A De Almeida.

The ASIA Syndrome (Autoimmune/Inflammatory Syndrome Induced by Adjuvants)
In genetically predisposed hosts such as HLA B8 or HLA DRB1*- positive individuals, biomaterials may trigger delayed immune responses, eventually progressing to granulomatous or autoimmune disorders falling into the ASIA diagnostic complex ().Citation31 Two or more stimuli increase the risk of abnormal immune responses and include:
Local trauma
Infections
Filler injections
Vaccines
Dental amalgams
Menstrual exacerbations
Table 17 ASIA Syndrome: Summary
HA is thought to trigger the immune system via adjuvant effect rather than primary antigenic immune response, being cited as potential trigger in 340/350 patients with previous filler treatments where filler removal effected improvement in 60% of cases. The adjuvant effect of microbial molecules may determine a limited autoimmune response vs evolution to full-blown disease.
Infection
Ciprofloxacin now carries an FDA black box warning and should not be prescribed for longer than 60 days (British National Formulary). Potential quinolone side-effects, including colitis and prolonged QT interval, merit recommendation as third-line agents in case of intolerance, allergy, or contraindication to macrolides and tetracyclines. Dual antibiotic therapy should continue for four weeks, followed by patient re-assessment ().Citation86
Table 18 Antibiotic Choice by Infection Origin (Adhere to Country-Specific Microbiotic Guidelines)
Conclusion
Facial filler treatment is a constantly evolving field mandating continuous reassessment and improvement. New challenges (eg, the COVID 19 SARS 2 pandemic) prompt new insights, with resultant evolution in the understanding, prevention, diagnosis and therapeutic approaches to filler complications.
The updated 10-point plan aims to empower aesthetic physicians to perform optimally through prudent patient selection, knowledgeable product choice, and attentive procedural planning. The most dreaded adverse events are vascular complications and filler-induced blindness. However, with a systematic approach, in-depth knowledge of facial anatomy, and appropriate algorithms, the majority of adverse events are avoidable or manageable.
This updated version of our former publication attempts to illuminate salient background knowledge, whilst still embodying a practical reference guide to the cosmetic health-care practitioner. Hopefully, an increased understanding of safety factors may serve to protect not only our patients but also the future of aesthetic medicine.
Consent
Written informed consent for publication of their clinical details and/or clinical images was obtained from the patients. No ethical concerns were raised in this paper.
Acknowledgment
The authors would like to express deep gratitude to PhD candidate, Elizabeth Rademan, Centre for Research on Evaluation, Science and Technology (CREST), Stellenbosch University, South Africa, for the invaluable writing and editing assistance serving to significantly improve the manuscript.
Disclosure
Dr Izolda Heydenrych reports honoraria for advisory boards and lecturing from Allergan, outside the submitted work; and being a consultant for Allergan/AbbVie, LÓreal, LaRochePosay, SkinCeuticals, Genop Healthcare. Dr Koenraad De Boulle reports grants and personal fees from Allergan and Genévrier, outside the submitted work. The authors report no other potential conflicts of interest in this work.
References
- Heydenrych I, Kapoor KM, De Boulle K, Goodman G, Swift A, Kumar N. A 10-point plan for avoiding hyaluronic acid dermal filler-related complications during facial aesthetic procedures and algorithms for management. Clin Cosmet Investig Dermatol. 2018;11:603–611. doi:10.2147/CCID.S180904
- Gonzalez H, Hagerling C, Werb Z. Roles of the immune system in cancer: from tumor initiation to metastatic progression. Genes Dev. 2018;32(19–20):1267–1284. doi:10.1101/GAD.314617.118
- Brierley ME, Sansom‐Daly UM, Baenziger J, McGill B, Wakefield CE. Impact of physical appearance changes reported by adolescent and young adult cancer survivors: a qualitative analysis. Eur J Cancer Care (Engl). 2019;28(4):e13052. doi:10.1111/ecc.13052
- Kang DH, Weaver MT, Park NJ, Smith B, McArdle T, Carpenter J. Significant impairment in immune recovery following cancer treatment Duck-Hee. Nurs Res. 2009;58(2):105–114. doi:10.1097/NNR.0b013e31818fcecd.
- Verma R, Foster RE, Horgan K, et al. Lymphocyte depletion and repopulation after chemotherapy for primary breast cancer. Breast Cancer Res. 2016;18(1):1–12. doi:10.1186/s13058-015-0669-x
- Naidoo J, Page DB, Li BT, et al. Toxicities of the anti-PD-1 and anti-PD-L1 immune checkpoint antibodies. Ann Oncol. 2015;26(12):2375–2391. doi:10.1093/annonc/mdv383
- Bisschop C, Bruijn MS, Stenekes MW, Diercks GFH, Hospers GAP. Foreign body reaction triggered by cytotoxic T lymphocyte‐associated protein 4 blockade 25 years after dermal filler injection. Br J Dermatol. 2016;175(6):1351–1353. doi:10.1111/bjd.14674
- De Boulle K. A sting in the tail: filler nodules after monoclonal antibody treatment. Br J Dermatol. 2016;175(6):1149. doi:10.1111/bjd.15117
- Pathmanathan S, Dzienis M. Cetuximab associated dermal filler reaction. BMJ Case Reports CP. 2019;12(8):e228882. doi:10.1136/bcr-2018-228882
- Hibler BP, Yan BY, Marchetti MA, Momtahen S, Busam KJ, Rossi AM. Facial swelling and foreign body granulomatous reaction to hyaluronic acid filler in the setting of tyrosine kinase inhibitor therapy. J Eur Acad Dermatol Venereol. 2018;32(6):e225. doi:10.1111/jdv.14749
- Syunyaeva Z, Kahnert K, Kauffmann-Guerrero D, Huber RM, Tufman A. Dermal filler injections mimic tumor activity during immune checkpoint inhibition. Respiration. 2018;95(5):362–363. doi:10.1159/000487601
- Dwivedi K, Prabhu IS, Bradley KM. Fluorodeoxyglucose activity associated with a cosmetic poly-L-lactide filler: a potential confounder on positron emission tomography and computed tomography. Br J Oral Maxillofac Surg. 2018;56(2):148–150. doi:10.1016/j.bjoms.2017.09.011
- Carvalho HDA, Villar RC. Radiotherapy and immune response: the systemic effects of a local treatment. Clinics. 2018;73(1):1–11. doi:10.6061/clinics/2018/e557s
- Lyle DB, Breger JC, Baeva LF, et al. Low molecular weight hyaluronic acid effects on murine macrophage nitric oxide production. J Biomed Mater Res Part A. 2010;94(3):893–904.
- Scheibner KA, Lutz MA, Boodoo S, Fenton MJ, Powell JD, Horton MR. Hyaluronan fragments act as an endogenous danger signal by engaging TLR2. J Immunol. 2006;177(2):1272–1281. doi:10.4049/jimmunol.177.2.1272
- Inchingolo F, Tatullo M, Abenavoli FM, et al. A hypothetical correlation between hyaluronic acid gel and development of cutaneous metaplastic synovial cyst. Head Face Med. 2010;6(1):13. doi:10.1186/1746-160X-6-13
- Creadore A, Watchmaker J, Maymone MBC, Pappas L, Vashi NA, Lam C. Cosmetic treatment in patients with autoimmune connective tissue diseases: best practices for patients with lupus erythematosus. J Am Acad Dermatol. 2020;83(2):343–363. doi:10.1016/j.jaad.2020.03.123
- Decates TS, Velthuis PJ, Schelke LW, et al. Increased risk of late-onset, immune-mediated, adverse reactions related to dermal fillers in patients bearing HLA-B*08 and DRB1*03 haplotypes. Dermatol Ther. 2020:1–6. doi:10.1111/dth.14644
- Friedman H, Newton C, Klein TW. Microbial infections, immunomodulation, and drugs of abuse. Clin Microbiol Rev. 2003;16(2):209–219.
- Warren GW, Alberg A. Smoking cessation after a cancer diagnosis and survival in cancer patients. Am Soc Clin Oncol. 2018;36(15):1561. doi:10.1200/JCO.2018.36.15_suppl.1561
- Trivedi MK, Kroumpouzos G, Murase JE. A review of the safety of cosmetic procedures during pregnancy and lactation. Int J Womens Dermatol. 2017;3(1):6–10. doi:10.1016/j.ijwd.2017.01.005
- Humphrey S, Jones DH, Carruthers J, et al. Retrospective review of delayed adverse events secondary to treatment with a smooth, cohesive. J Am Acad Dermatol. 2020. doi:10.1016/j.jaad.2020.01.066
- Shumaker PR, England LJ, Dover JS, et al. Effect of monopolar radiofrequency treatment over soft‐tissue fillers in an animal model: part 2. Lasers Surg Med. 2006;38(3):211–217.
- Hsu SH, Chung HJ, Weiss RA. Histologic effects of fractional laser and radiofrequency devices on hyaluronic acid filler. Dermatologic Surg. 2019;45(4):552–556. doi:10.1097/DSS.0000000000001716
- Del Rosso JQ, Tanghetti E, Webster G, Gold LS, Thiboutot D, Gallo RL. Update on the management of rosacea from the American Acne & Rosacea Society (AARS). J Clin Aesthet Dermatol. 2019;12(6):17.
- Kuraitis D, Williams L. Decolonization of Staphylococcus aureus in Healthcare: a Dermatology Perspective. J Healthc Eng. 2018;2018:1–8. doi:10.1155/2018/2382050
- Jiang Y-C, Feng H, Lin Y-C, Guo X-R. New strategies against drug resistance to herpes simplex virus. Int J Oral Sci. 2016;8(1):1–6. doi:10.1038/ijos.2016.3
- Rowland‐Warmann MJ. Hypersensitivity reaction to hyaluronic acid dermal filler following novel coronavirus infection–a case report. J Cosmet Dermatol. 2021;20(5):1557–1562. doi:10.1111/jocd.14074
- Munavalli GG, Knutsen-Larson S, Lupo MP, Geronemus RG. Oral angiotensin converting enzyme inhibitors for the treatment of delayed inflammatory reaction of dermal hyaluronic acid fillers following COVID-19 vaccination–a model for inhibition of angiotensin ii-induced cutaneous inflammation. JAAD Case Rep. 2021;10:63–68. doi:10.1016/j.jdcr.2021.02.018
- Munavalli GG, Guthridge R, Knutsen-Larson S, Brodsky A, Matthew E, Landau M. COVID-19/SARS-CoV-2 virus spike protein-related delayed inflammatory reaction to hyaluronic acid dermal fillers: a challenging clinical conundrum in diagnosis and treatment. Arch Dermatol Res. 2021;1–15. doi:10.1007/s00403-020-02094-x
- Alijotas-Reig J, Esteve-Valverde E, Gil-Aliberas N, Garcia-Gimenez V. Autoimmune/inflammatory syndrome induced by adjuvants—ASIA—related to biomaterials: analysis of 45 cases and comprehensive review of the literature. Immunol Res. 2018;66(1):120–140. doi:10.1007/s12026-017-8980-5
- Rice SM, Ferree SD, Mesinkovska NA, Kourosh AS. The art of prevention: COVID-19 vaccine preparedness for the dermatologist. Int J Womens Dermatol. 2021;7(2):209–212. doi:10.1016/j.ijwd.2021.01.007
- Naraghi M, Atari M. Development and validation of the expectations of aesthetic rhinoplasty scale. Arch Plast Surg. 2016;43(4):365. doi:10.5999/aps.2016.43.4.365
- Krebs G, de la Cruz LF, Mataix-Cols D. Recent advances in understanding and managing body dysmorphic disorder. Evid Based Ment Health. 2017;20(3):71–75. doi:10.1136/eb-2017-102702
- Focus D Deep focus’ Cassandra report: Gen Z uncovers massive attitude shifts toward money, work and communication preferences. Market Wired; 2015.
- Balakrishnan J, Griffiths MD. An exploratory study of “Selfitis” and the development of the Selfitis Behavior Scale. Int J Ment Health Addict. 2018;16(3):722–736. doi:10.1007/s11469-017-9844-x
- Nightingale SJ, Wade KA, Watson DG. Can people identify original and manipulated photos of real-world scenes? Cogn Res Princ Implic. 2017;2(1):30. doi:10.1186/s41235-017-0067-2
- Rice SM, Graber E, Kourosh AS. A pandemic of dysmorphia:“Zooming” into the perception of our appearance. Facial Plast Surg Aesthetic Med. 2020;22(6):401–402. doi:10.1089/fpsam.2020.0454
- Heydenrych I, Siolo E, Dlova NC, Avelar LE. Skin and structural aging in patients of African ethnicity. Features, management and the role of regenerative surgery. In: Kalaaji A, editor. Plastic and Aesthetic Regenerative Surgery and Fat Grafting: Clinical Application and Operative Techniques. Springer; 2021.
- Samizadeh S, Wu W. Ideals of facial beauty amongst the Chinese population: results from a large national survey. Aesthetic Plast Surg. 2018;42(6):1540–1550. doi:10.1007/s00266-018-1188-9
- Kapoor KM, Chatrath V, Anand C, et al. Consensus recommendations for treatment strategies in Indians using botulinum toxin and hyaluronic acid fillers. Plast Reconstr Surg Glob Open. 2017;5(12):e1574. doi:10.1097/GOX.0000000000001574
- Glass DA. Current Understanding of the Genetic Causes of Keloid Formation. J Investig Dermatol Symp Proc. 2017;18(2):S50–S53. doi:10.1016/j.jisp.2016.10.024
- Ginsberg BA. Dermatologic care of the transgender patient. Int J Womens Dermatol. 2017;3(1):65–67. doi:10.1016/j.ijwd.2016.11.007
- De Maio M, Heydenrych I. Myomodulation. In: Pirayesh A, Bertossi D, Heydenrych I, editors. Aesthetic Facial Anatomy Essentials for Injections. CRC Press; 2020.
- Belhaouari L, Lopez-Tomasety M, Quinodoz P, De Boulle K. Myomodulation and hyaluronic acid. Prime J. 2020:57–61.
- Joganathan V, Shah-Desai S. Awareness of management of hyaluronic acid induced visual loss: a British National Survey. Eye. 2020;10–13. doi:10.1038/s41433-020-0810-7
- Goodman GJ, Liew S, Callan P, Hart S. Facial aesthetic injections in clinical practice: pretreatment and posttreatment consensus recommendations to minimise adverse outcomes. Australas J Dermatol. 2020.
- Robinson DM. In vitro analysis of the degradation of calcium hydroxylapatite dermal filler: a Proof-of-Concept Study. Dermatol Surg. 2018;44:5–9. doi:10.1097/DSS.0000000000001683
- van Loghem J, Funt D, Pavicic T, et al. Managing intravascular complications following treatment with calcium hydroxylapatite: an expert consensus. J Cosmet Dermatol. 2020;19(11):2845–2858. doi:10.1111/jocd.13353
- Yankova M, Pavicic T, Frank K, et al. Intraarterial degradation of calcium hydroxylapatite using sodium thiosulfate–an in vitro and Cadaveric Study. Aesthetic Surg J. 2021;41(5):NP226–NP236. doi:10.1093/asj/sjaa350
- Casabona G, Marchese PB, Montes JR, Hornfeldt CS. Durability, behavior, and tolerability of 5 hyaluronidase products. Dermatologic Surg. 2018;44(11):42–50. doi:10.1097/DSS.0000000000001562
- Pifferi C, Berthet N, Renaudet O. Cyclopeptide scaffolds in carbohydrate-based synthetic vaccines. Biomater Sci. 2017;5(5):953–965. doi:10.1039/C7BM00072C
- Reinholz M, Clanner‐Engelshofen BM, Heppt MV, et al. Dermal fillers do not induce upregulation of NLRP3 inflammasomes or expression of inflammatory cytokines in granulomas. J Cosmet Dermatol. 2020;19(11):2838–2844. doi:10.1111/jocd.13341
- Buhren BA, Schrumpf H, Bölke E, Kammers K, Gerber PA. Standardized in vitro analysis of the degradability of hyaluronic acid fillers by hyaluronidase. Eur J Med Res. 2018;23(1):1–6. doi:10.1186/s40001-018-0334-9
- Beylot C, Auffret N, Poli F, et al. Propionibacterium acnes: an update on its role in the pathogenesis of acne. J Eur Acad Dermatol Venereol. 2014;28(3):271–278. doi:10.1111/jdv.12224
- McLaughlin J, Watterson S, Layton AM, Bjourson AJ, Barnard E, McDowell A. Propionibacterium acnes and acne vulgaris: new insights from the integration of population genetic, multi-omic, biochemical and host-microbe studies. Microorganisms. 2019;7(5):128. doi:10.3390/microorganisms7050128
- De Boulle K. Management of complications after implantation of fillers. J Cosmet Dermatol. 2004;3(1):2–15. doi:10.1111/j.1473-2130.2004.00058.x
- De Boulle K. Critical reflections on ArteFill, a permanent injectable product for soft tissue augmentation: mechanism of action and injection techniques, indications, and applications. Aesthetic Plast Surg. 2010;34(3):287–289. doi:10.1007/s00266-010-9521-y
- Schelke LW, Decates TS, Velthuis PJ. Ultrasound to improve the safety of hyaluronic acid filler treatments. J Cosmet Dermatol. 2018;17(6):1019–1024. doi:10.1111/jocd.12726
- Urdiales‐Gálvez F, De cabo‐Francés FM, Bové I. Ultrasound patterns of different dermal filler materials used in Aesthetics. J Cosmet Dermatol. 2021;20(5):1541–1548. doi:10.1111/jocd.14032
- Ward B, Ward M, Fried O, Paskhover B. Nasal distortion in short-distance photographs: the selfie effect. JAMA Facial Plast Surg. 2018;20(4):333–335. doi:10.1001/jamafacial.2018.0009
- Diefenbach S, Christoforakos L. The selfie paradox: nobody seems to like them yet everyone has reasons to take them. An exploration of psychological functions of selfies in self-presentation. Front Psychol. 2017;8:7. doi:10.3389/fpsyg.2017.00007
- Clare S, Rowley S. Implementing the Aseptic Non Touch Technique (ANTT®) clinical practice framework for aseptic technique: a pragmatic evaluation using a mixed methods approach in two London hospitals. J Infect Prev. 2018;19(1):6–15. doi:10.1177/1757177417720996
- Kirk-Bayley J, Challacombe S, Sunkaraneni S, Combes J The use of povidone iodine nasal spray and mouthwash during the current COVID-19 pandemic may protect healthcare workers and reduce cross infection. Available SSRN 3563092; 2020.
- Peng X, Xu X, Li Y, Cheng L, Zhou X, Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12(1):1–6. doi:10.1038/s41368-020-0075-9
- Pirayesh A, Bertossi D, Heydenrych I, editors. Aesthetic Facial Anatomy Essentials for Injections. Boca Raton: CRC Press; 2020.
- Kapoor KM, Chatrath V, Li CQ, Bertossi D. Pinch anatomy: an injection guide for temple filler injections. Dermatol Ther. 2020;33(6). doi:10.1111/dth.13983
- Chubb DP, Taylor GI, Ashton MW. True and “choke” anastomoses between perforator angiosomes: part ii. dynamic thermographic identification. Plast Reconstr Surg. 2013;132(6):1457–1464. doi:10.1097/01.prs.0000434407.73390.82
- Ashton MW, Taylor GI, Corlett RJ. The role of anastomotic vessels in controlling tissue viability and defining tissue necrosis with special reference to complications following injection of hyaluronic acid fillers. Plast Reconstr Surg. 2018;141(6):818e–830e. doi:10.1097/PRS.0000000000004287
- Khan TT, Colon-Acevedo B, Mettu P, DeLorenzi C, Woodward JA. An anatomical analysis of the supratrochlear artery: considerations in facial filler injections and preventing vision loss. Aesthetic Surg J. 2017;37(2):203–208. doi:10.1093/asj/sjw132
- Carley SK, Kraus CN, Cohen JL. Nitroglycerin, or not, when treating impending filler necrosis. Dermatologic Surg. 2020;46(1):31–40. doi:10.1097/DSS.0000000000002030
- Sobierajewicz J, Naskręcki R, Jaśkowski W, Van der Lubbe RHJ. Do musicians learn a fine sequential hand motor skill differently than non-musicians? PLoS One. 2018;13(11):1–23. doi:10.1371/journal.pone.0207449
- Kapoor K, Kapoor P, Heydenrych I, Bertossi D. Vision loss associated with hyaluronic acid fillers: a systematic review of literature. Aesthetic Plast Surg. 2020;44(3):929–944. doi:10.1007/s00266-019-01562-8
- Albornoz CA, Jhawar N, Durso TA, Hazan E, Wang JV, Saedi N. Preinjection aspiration for injectable fillers in aesthetic dermatology: trust or bust? J Cosmet Dermatol. 2020;19(5):1063–1064. doi:10.1111/jocd.13377
- Wang JV, Hazan E, Hattier G, Torbeck RL, Khorasani H, Saedi N. Utility of preinjection aspiration for hyaluronic fillers: a novel in vivo human evaluation. J Cutan Med Surg. 2020;24(4):1203475420921387. doi:10.1177/1203475420921387
- Kogan I, Korolik P, Cartier H, Adhoute H, Liberzon A. In vitro evaluation of aspiration of hyaluronic acid filler with a new saline flashing method. J Cosmet Dermatol. 2020;19(10):2513–2518. doi:10.1111/jocd.13651
- Goodman GJ, Magnusson MR, Callan P, et al. Neither positive nor negative aspiration before filler injection should be relied upon as a safety maneuver. Aesthetic Surg J. 2021;41(4):NP134–NP136. doi:10.1093/asj/sjaa215
- Casabona G. Blood aspiration test for cosmetic fillers to prevent accidental intravascular injection in the face. Dermatologic Surg. 2015;41(7):841–847. doi:10.1097/DSS.0000000000000395
- Carey W, Weinkle S. Retraction of the plunger on a syringe of hyaluronic acid before injection: are we safe? Dermatol Surg. 2015;41:S340–S346. doi:10.1097/DSS.0000000000000557
- Goodman GJ, Magnusson MR, Callan P, et al. Aspiration before tissue filler—an exercise in futility and unsafe practice. Aesthetic Surg J. 2021. doi:10.1093/asj/sjab036
- Goodman GJ, Liew S, Callan P, et al. Re Facial aesthetic injections in clinical practice: pretreatment and post-treatment consensus recommendations to minimise adverse outcome Region-specific changes in line with the Covid-19 pandemic. Australas J Dermatol. 2020. doi:10.1111/ajd.13374
- Alvarez-Perea A, Tanno LK, Baeza ML. How to manage anaphylaxis in primary care. Clin Transl Allergy. 2017;7(1):1–10. doi:10.1186/s13601-017-0182-7
- Humzah MD, Ataullah S, Chiang CA, Malhotra R, Goldberg R. The treatment of hyaluronic acid aesthetic interventional induced visual loss (AIIVL): a consensus on practical guidance. J Cosmet Dermatol. 2019;18(1):71–76. doi:10.1111/jocd.12672
- Goodman GJ, Magnusson MR, Callan P, et al. A consensus on minimizing the risk of hyaluronic acid embolic visual loss and suggestions for immediate bedside management. Aesthetic Surg J. 2019.
- Paap MK, Milman T, Ugradar S, Goldberg R, Silkiss RZ. Examining the role of retrobulbar hyaluronidase in reversing filler-induced blindness: a systematic review. Ophthalmic Plast Reconstr Surg. 2019. doi:10.1097/PRS.0000000000005806
- King M, Bassett S, Davies E, King S. Management of delayed onset nodules. J Clin Aesthet Dermatol. 2016;9(11):1–5.
- Liew S. Ethnic and gender considerations in the use of facial injectables: Asian patients. Plast Reconstr Surg. 2015;136(5):22–27. doi:10.1097/PRS.0000000000001728
- Cavallini M, Papagni M, Trocchi G. Sensitivity of hyaluronic acid fillers to hyaluronidase: an in vitro analysis. J Clin Exp Dermatol Res. 2020;11(517).
- King M, Convery C, Davies E. The use of hyaluronidase in aesthetic practice the use of hyaluronidase in aesthetic practice. Aesthetic Complicat Expert Gr. 2019;2.4:1–12.
- Rauso R, Zerbinati N, Fragola R, Nicoletti GF, Tartaro G. Transvascular hydrolysis of hyaluronic acid filler with hyaluronidase. Dermatologic Surg. 2020;47(3):370–372. doi:10.1097/dss.0000000000002773
- Rauso R, Zerbinati N, Franco R, et al. Cross-linked hyaluronic acid filler hydrolysis with hyaluronidase: different settings to reproduce different clinical scenarios. Dermatol Ther. 2020;33(2):1–5. doi:10.1111/dth.13269
- De Boulle K, Glogau R, Kono T, et al. A review of the metabolism of 1, 4‐Butanediol Diglycidyl ether–crosslinked hyaluronic acid dermal fillers. Dermatologic Surg. 2013;39(12):1758–1766. doi:10.1111/dsu.12301
- Kumar N, Swift A, Rahman E. Development of “Core Syllabus” for facial anatomy teaching to aesthetic physicians: a Delphi consensus. Plast Reconstr Surg Glob Open. 2018;6(3):1–7. doi:10.1097/GOX.0000000000001687
- Sindel A, Özalp O, Yıldırımyan N, Oğuz N, Sindel M, Llankovan V. Evaluation of the course of the marginal mandibular branch of the facial nerve: a fresh cadaveric study. Br J Oral Maxillofac Surg. 2021;59(2):179–183. doi:10.1016/j.bjoms.2020.08.020
- Delorenzi C. New high dose pulsed hyaluronidase protocol for hyaluronic acid filler vascular adverse events. Aesthetic Surg J. 2017;37(7):814–825. doi:10.1093/asj/sjw251
- Mackern-Oberti JP, Jara EL, Riedel CA, Kalergis AM. Hormonal modulation of dendritic cells differentiation, maturation and function: implications for the initiation and progress of systemic autoimmunity. Arch Immunol Ther Exp (Warsz). 2017;65(2):123–136. doi:10.1007/s00005-016-0418-6