Abstract
Background
Atopic dermatitis (AD) is a chronic inflammatory, non-communicable, and relapsing skin disease that affects all age groups. There is a dearth of literature that reports the disease burden, and epidemiology and highlights unmet needs in the diagnosis and management of AD in India.
Methods
A total of ten specialists including dermatologists, pediatric dermatologists, and pediatricians with more than ten years of experience and practicing in different parts of India served as the expert panel during the virtual meet conducted on January 24, 2021. A questionnaire comprising 32 questions on different aspects of AD management was categorized among different sections: burden of disease (five questions), age of onset and prevalence (five questions), etiology and pathogenesis (six questions), diagnosis and severity of the disease (seven questions), and treatment (nine questions). Consensus was defined when agreement was provided by ≥90% of the experts.
Results
Considering the profound impact AD has on the quality of life (QoL) of patients, the expert panel recommended patient counseling while moderate to severe cases of AD need a prompt referral to a specialist. The panel did not recommend any specific diagnostic and severity criteria as a standard due to the inherent limitations associated with every criterion. The role of environment and changing lifestyle in addition to genetic and familial risk factors for AD was also considered. The panel unanimously recommended to conduct a countrywide, multicenter survey/study to estimate the true prevalence of AD in India. Further, the experts recommended to follow proper treatment protocols and to perform longitudinal monitoring for understanding corticosteroid treatment associated side effects.
Conclusion
This guidance focuses on identifying the unmet gaps and provides practical recommendations for improving QoL, diagnosis, prognosis, and overall management of patients with AD in India.
Introduction
Atopic dermatitis (AD) is a chronic inflammatory, non-communicable, and relapsing skin disease that most often develops during early infancy and childhood.Citation1 AD developed during childhood is characterized by eczematous lesions on the flexural areas, nape of the neck, dorsum of the feet and hands; whereas, lichenified/exudative flexural dermatitis alone or associated with head/neck, and hand eczema, and the prurigo nodularis (PN)-like AD are commonly observed in adult patients with AD.Citation2–Citation4 Owing to these manifestations, patients with AD may experience itching, sleep disturbances, poor performance at school/work, and disturbed social, mental, and emotional functioning.Citation1,Citation5 Furthermore, childhood AD has also shown a negative impact on the quality of life (QoL) of the patient’s family and caregivers.Citation5,Citation6 AD is also associated with several “other atopic diseases” including asthma, allergic rhinitis, food allergies, and hay fever, whose prevalence vary by age;Citation7 AD also increases the risk of other non-allergic comorbidities including mental health disorders and other autoimmune- or immune-mediated diseases.Citation1
The Global Burden of Skin Disease study (2010) estimated that AD affects up to 230 million people worldwide with a higher prevalence in females and lower prevalence in older age groups.Citation8,Citation9 The Global Burden of Disease study reported that the prevalence of AD and disability-adjusted life years (DALYs) in adults have remained stable since 1990 till 2017.Citation10 As per the International Study of Asthma and Allergies in Childhood (ISAAC), prevalence of AD in India (6–7 years: 2.7% and 13–14 years: 3.6%) was lower compared to the global estimates.Citation11
A number of hospital-based or region-specific studies have assessed the prevalence of AD in India;Citation12–Citation15 while region-specific-differences in prevalence are likely due to the different climatic conditions.Citation16,Citation17 In this regard, nationwide, systematic studies identifying the disease burden, epidemiology, and challenges in the diagnosis and management of AD in India are lacking.
The primary objective of this consensus meeting was to identify the need gaps and to provide practical guidance to understand the prevalence, diagnosis, and management of AD in India.
Methods
To understand the region-specific differences in terms of prevalence, diagnosis, and management of AD, the expert panel included ten specialists including dermatologists, pediatric dermatologists, and pediatricians with more than ten years of experience and practicing in different parts of India was convened. Dr. Amod Tilak and Dr. Charles Adhav coordinated with the expert panel, analyzed the results, and were responsible for the overall organizational and logistic aspects of the project. The expert discussion was moderated by Dr. Murlidhar Rajagopalan. The expert panel consisted of Dr. Ram Gulati, Dr. Nidhi Sharma, Dr. Amarjeet Chitkara, Dr. Abhishek De, Dr. Sharad Mutalik, Dr. Prakash Vaidya, Dr. Samir Dalwai, Dr. Shrutakirthi Shenoi, and Dr. Samipa Mukherjee.
The ethical committee approval was not applicable, as this article is based on previously conducted studies and does not contain involvement with human participants or animals.
Questionnaire and Compilation of Tentative Consensus
A rapid review of global and regional data on the management of AD was conducted. The panel members decided to include questions on different aspects of the disease including humanistic and economic burden, prevalence, diagnosis, severity, and treatment of AD. The questionnaire was developed and curated by the Chairperson; further, he consulted other panel members during the meeting to add/modify certain questions.
A questionnaire comprising 32 questions (Supplementary Table 1) on different aspects of AD management was categorized among different sections: burden of disease (five questions), age of onset and prevalence (five questions), etiology and pathogenesis (six questions), diagnosis and severity of the disease (seven questions), and treatment (nine questions). Majority of the questions were formulated such that the experts could provide response from the options “Agree,” “Disagree,” and “Partially Agree.” However, a few open-ended questions had specific options to initiate further discussion. “Consensus” was defined when agreement was provided by ≥90% of the experts.
All the panel members were allowed to share their personal experiences and answer the clinical questions enlisted under each topic. The virtual meet was conducted on January 24, 2021. This manuscript is the outcome of the expert panel discussion and consensus arrived during the meeting.
Results and Discussion
Burden of Disease
Adult patients with AD experience substantially impaired health-related QoL as a result of itching and scratching, mood and sleep disorders, negative emotions compared with the general population and patients with other chronic diseases such as diabetes mellitus and hypertension.Citation6 Furthermore, AD is also associated with high levels of stigmatization, societal rejection, anxiety, depression, and suicidal ideation.Citation18 School-going children (aged >8 years) can experience bullying and avoidance resulting in lack of self-esteem, social withdrawal, and rejection.Citation5,Citation6
As per Handa et al over a 6-month period, the cost of AD treatment was Rs. 6235.00 ± 3514.00; the mean total costs increased significantly with the severity and ranged approximately between Rs. 3500 and 8990 (mild AD: Rs. 3579.00 ± 948.00, moderate AD: Rs. 6806.00 ± 3676.00 and severe AD: Rs. 8991.00 ± 3129.00) in an outpatient hospital setting. Caregiver cost constituted half of the total cost, followed by indirect cost (31.7%), and provider cost (18.1%).Citation19 It is important to note that the direct comparison of total treatment cost of AD with other chronic diseases is difficult considering the duration, severity, and nature of the disease, and patient- and caregiver-specific characteristics (location: rural/urban, age, education, annual income, community/tertiary care hospitals, outpatient clinics, specialty and so on).
The experts echoed with the published literature on the burden of the disease (). In addition to busy outpatient clinic, lack of training on patient communication and counseling, and inadequate knowledge of patients were considered as the major deterrents. The direct costs (cost of medication and hospitalization) contribute more toward the total costs of mild-to-moderate AD, whereas direct and indirect costs contribute equally in moderate-to-severe AD. The panel suggested that a prompt referral to a specialist may reduce the symptomatic and economic burden in patients with AD; however, it depends on the area of practice (rural/urban setting) in India.
Table 1 Consensus Statements
Diagnosis
The clinical diagnosis of AD is mainly based on the physical examination and personal/family history of atopy and not on a definitive laboratory test.Citation20,Citation21 Commonly used diagnostic criteria include Hanifin-Rajka (HR), the United Kingdom (UK) Working Party, and the modified American Academy of Dermatology (AAD) criteria; however each criteria is associated with inherent limitations.Citation20,Citation22 A systematic review of randomized controlled trials (RCT; N = 212) conducted between 2007 and 2016, including adult and pediatric patients with AD, reported that among 10 different diagnostic criteria, HR criteria (41.0%) was the most commonly used followed by the UK refinement of the HR criteria (9.0%) and AAD criteria (3.8%).Citation23 Although the most common clinical features associated with AD are pruritus, lichenification, and xerosis, inconsistency or deviation from the classical pattern especially in adult patients can often make it the diagnosis of exclusion.Citation24
About 44% of experts recommended HR followed by UK working party (33%), and AAD revised of UK Working Party criteria (22%) for diagnosis of AD. However, considering practical limitations associated with every diagnostic criterion, the expert panel did not reach consensus on recommending a standard criterion for diagnosis of AD.
Severity of the Disease
A simplified severity assessment of AD includes (): (a) measuring the area involved in percentage of body surface; (b) establishing acute, subacute, or chronic changes; and (c) determining the impact on patient’s QoL.Citation25 The severity of dermatitis can be measured and monitored in several ways including the adequately validated and user-friendly scales such as: Scoring Atopic Dermatitis (SCORAD), Objective Severity Assessment of Atopic dermatitis (OSAAD), The Eczema Area and Severity Index (EASI), and Patient-Oriented Eczema Measure (POEM); however, there is no standard measure yet to understand the disease severity in clinical practice.Citation22,Citation25
Figure 1 Classification of AD based on severity. Data fromCitation25,Citation47.
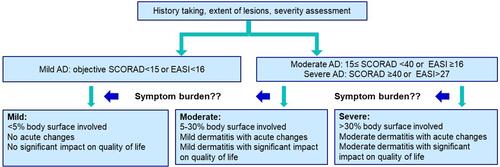
An equal proportion (25%) of experts recommended EASI and POEM, whereas 37% recommended Investigator’s Static Global Assessment for determining severity of AD; regardless of scoring system, the experts highlighted to consider Dermatology Life Quality Index in routine management.
Age of Onset of Atopic Dermatitis
In about 80% of patients, AD is developed before six years of age.Citation1 AD is less persistent when developed before two years of age, whereas onset at a later stage can result in greater severity and more persistent AD.Citation26
A study conducted in the eastern part of India reported that the mean age of onset in the “infantile AD” group, and in the “childhood AD” group was 5.2 months and 3.47 years, respectively.Citation12 Other studies including children aged 2 to 12 years reported mean age of onset as 3.63 years and 4.58 years.Citation13,Citation27
Although majority of experts (70%) responded that the mean age of onset in India for infantile AD is between 3 and 6 months and childhood AD is between 3 and 5 years, exact estimation is challenging due to: (a) lack of simple and consistent definition; (b) challenges in interpreting the clinical symptoms in infants due to lack of awareness and inaccurate history provided by the parents/caregivers; (c) diagnosis of exclusion due to common presentations including infantile rash (nappy rash), fungal infection, and contact dermatitis.
Prevalence of Atopic Dermatitis
A number of previously published region-specific studies have reported variation in terms of prevalence of AD in India (). In this regard, the expert panel unanimously agreed to conduct a countrywide, multicenter survey/study that would estimate the true prevalence of AD in India ().
Table 2 Studies Determining Prevalence of AD in India
A great variation was also observed in terms of gender-specific risk of AD. A study conducted among school-going children reported male to female ratio of 1:1.73 including 42.2% boys and 57.8% girls.Citation15 Conversely, studies by Kumar et al and Dhar et al reported male predominance in infant and childhood groups.Citation12,Citation27 More than half of the experts (60%) agreed that male and female are at equal risk of developing AD. However, preponderance of male patients could be observed due to sociocultural biases (gender disparity, taboo associated with skin diseases), and protective role of estrogen in females.
Etiology of Atopic Dermatitis
AD, a multifactorial disease, is due to the interaction between genetic, immunological, and environmental factors ().Citation28,Citation29 In addition to filaggrin, there are other genes that could be responsible for skin barrier impairment. The majority of panel members (70%) did not recommend performing gene profiling routinely, due to cost constraints and inadequate resources; however, its potential in the near future was not denied. A few experts (30%) specified that gene profiling may avoid unnecessary exposure to steroids and other topical/systemic drugs and may reduce multiple treatments in patients with AD. The expert panel indicated temperature, humidity, air pollution, tobacco smoke, urban versus rural living, family size, and antibiotics as some of the environmental risk factors for AD that are aligned with those published in the literature ().Citation1 The panel did not consider diet as one of the major trigger factors, as the dietary habits (wheat-based, dairy products) have been relatively consistent over the centuries. However, recent changes in the lifestyle and adoption of western diet can be considered as one of the trigger factors for AD in India.
Table 3 Etiology of AD
Pathogenesis of Atopic Dermatitis
Pathogenesis of AD is multifactorial and complex in nature, which includes skin barrier dysfunction, immunological (cutaneous and systemic) dysregulation, and dysbiosis of resident microbiota ().Citation28,Citation29
Figure 2 Pathogenesis of AD. Data from Citation1,Citation29,Citation48.
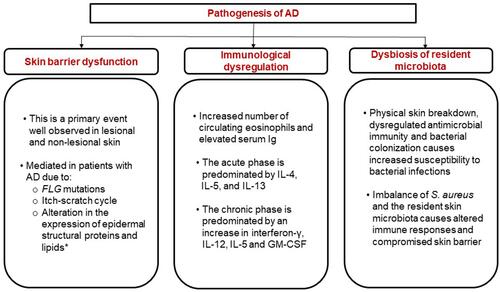
It is important to note that not all microbial infections are protective against AD. Specifically, colonization of S aureus was observed in 70% lesional skin, 39% non-lesional skin, and 62% nose of patients with AD.Citation30 In a cross-sectional study conducted in southern India, S. aureus was present on the lesional and non-lesional skin of 92.4% of children aged <12 years with AD.Citation31 About 60% of experts agreed that patients with moderate-to-severe AD are susceptible to S aureus infection likely due to itching, disruption of skin barrier, and poor hand hygiene. The majority of experts who agreed and responded partial applicability of hygiene hypothesis were 40% and 50%, respectively. The panel recommended to conduct a high-powered systematic study in urban and rural settings for a better understanding of the role of hygiene hypothesis in India.
Treatment of Atopic Dermatitis
Due to chronic nature of the disease, the ideal long-term management of AD includes managing cutaneous and systemic inflammation. In most cases, AD is managed by controlling exacerbation factors, good general skin care, and topical treatments. Good skin care routine,Citation21,Citation32 and patient and caregiver education on treatment doses together with skin-care techniquesCitation21,Citation32,Citation33 are some of the important aspects of overall self-management of AD. Additionally, psychological interventions such as brief dynamic psychotherapy, cognitive-behavioral therapy, biofeedback, relaxation training, hypnosis, distraction, and habit reversal could be used to reduce itch intensity, disease severity, and scratching in adult patients with AD.Citation18,Citation33 Distraction and redirection to hands-on activities can be recommended to pediatric patients.Citation33
First-Line Therapy
Topical Corticosteroids
Topical corticosteroids (TCS) are used as the first-line treatment in the management of acute AD flare-ups by decreasing the inflammatory immune response resulting in rapid relief.Citation34 A scoping systematic review of nine RCTs reported that a large proportion of participants responded to TCS treatment compared to placebo and proactive treatment (16 weeks) prevented flare-ups during the treatment period.Citation35 There is a little consensus on the frequency of application (once daily/twice daily or more frequent use) due to similar efficacy.Citation35,Citation36 Possible adverse effects of TCS include skin atrophy, purpura, telangiectasia, striae, hypopigmentation, and acneiform eruption.Citation34,Citation37
Systemic Corticosteroids
According to the International Eczema Council, systemic corticosteroids (SCS) are not recommended for routine use and may be used only in specific circumstances for the treatment of severe AD. However, the treatment duration of SCS should be limited to short duration as a bridge to steroid-sparing therapies.Citation38 Noted adverse events include rebound AD flares, adrenal suppression, growth retardation, hypertension, and weight gain.Citation39 The most recent AAD guidelines recommend tapered schedule during the use of SCS to decrease the risk of adrenal suppression.Citation40
About 66% of experts responded that glaucoma, cataract, and adrenal insufficiency are rarely observed in Indian patients with AD, while the majority of experts reported that skin atrophy, acneiform eruption, and hypopigmentation are commonly reported as TCS-associated side effects. The panel was divided into two groups on reporting “steroid addiction” that is associated with prolonged self-medication. Conversely, majority of experts expressed non-compliance to TCS treatment () owing to various factors such as: (a) patient–physician relationship; (b) lack of communication; (c) corticosteroid phobia or fear of side effects. More than half of the experts (57%) indicated that Indian patients following SCS treatment report hypertension, weight gain, behavioral changes, and opportunistic infections. The panel emphasized that treatment-associated side effects do exist and hence clinicians should follow proper treatment protocols and perform longitudinal monitoring.
Second-Line Therapy
Phototherapy is recommended as a second-line treatment either as a monotherapy or as an adjuvant to emollients and steroids in patients with moderate-to-severe AD.Citation40 Commonly reported side effects associated with phototherapy include xerosis cutis, treatment-induced erythema, and burning of skin. Long-term adverse effects particularly due to high dosage of UVA1 include photodamage, skin carcinogenesis, and melanoma induction.Citation32,Citation41
Systemic immunomodulating agents are recommended for the treatment of adult and pediatric patients with moderate-to-severe AD when topical regimens and/or phototherapy fail or when QoL is substantially impacted.Citation40 Effective off-label systemic treatment options include cyclosporine, azathioprine, methotrexate, and mycophenolate mofetil.Citation40
Summary
AD, a multifactorial disease, disproportionately affects health-related QoL and social, mental, and emotional functioning in both, patients and parents/caregivers. To understand the unmet need in the overall management of AD, the expert panel including dermatologists across India proactively discussed, shared their experiences, and provided recommendations () in terms of estimating prevalence, etiopathogenesis, diagnosis, and severity of the disease, and treatment of AD. These consensus statements aim to provide a practical guidance to dermatologists, pediatricians, and primary care physicians while treating patients with AD in India.
Table 4 Expert Panel Recommendations on the Management of AD in India
The panel acknowledged the burden AD has on patients and suggested focused training on patient communication and counseling. Lack of simple and uniform definition of AD, varied clinical presentation, cultural biases, and inadequate knowledge about the disease makes estimation of prevalence, gender ratio, and age of onset difficult in the clinical practice. There was no consensus on using a specific diagnostic criteria and severity scoring as standard due to inherent drawbacks associated with every criterion or tool. However, experts recommended to consider QoL and symptom burden while determining the severity of the disease. Furthermore, the panel acknowledged the occurrence of commonly reported side effects following TCS or SCS or systemic therapy among Indian patients. In this regard, it is important to consider that treatment-associated side effects do exist and hence, clinicians should follow proper treatment protocols and should perform longitudinal monitoring.
This guidance focuses on identifying the unmet gaps and provides practical recommendations for improved QoL, diagnosis, prognosis, and overall management of patients with AD in India.
Acknowledgments
Medical writing support was provided by Ashwini Atre, PhD and Sumedha Kulkarni, M. Pharm of Indegene Pvt. Ltd. Bangalore, India and that was funded by Pfizer India Ltd.
Disclosure
Dr. Sharad Mutalik is on the advisory board of Novartis, Pfizer, Dr Reddy Labs and Sanofi and receives remuneration for the same. Dr. Shrutakirthi Shenoi reports personal fees from Pfizer India Ltd, during the conduct of the study. Dr. Amod and Dr. Charles are employees of Pfizer ltd. The authors report no other conflicts of interest in this work.
Additional information
Funding
References
- Weidinger S, Beck LA, Bieber T, Kabashima K, Irvine AD. Atopic dermatitis. Nat Rev Dis Prim. 2018;4(1). doi:10.1038/s41572-018-0001-z
- Nettis E, Ortoncelli M, Pellacani G, et al. A multicenter study on the prevalence of clinical patterns and clinical phenotypes in adult atopic dermatitis. J Investig Allergol Clin Immunol. 2020;30(6):448–472. doi:10.18176/jiaci.0519
- Silverberg JI, Vakharia PP, Chopra R, et al. Phenotypical differences of childhood- and adult-onset atopic dermatitis. J Allergy Clin Immunol Pract. 2018;6(4):1306–1312. doi:10.1016/j.jaip.2017.10.005
- Ozkaya E. Adult-onset atopic dermatitis. J Am Acad Dermatol. 2005;52(4):579–582. doi:10.1016/j.jaad.2004.11.037
- Lifschitz C. The impact of atopic dermatitis on quality of life. Ann Nutr Metab. 2015;66(suppl 1):34–40. doi:10.1159/000370226
- Blome C, Radtke MA, Eissing L, Augustin M. Quality of life in patients with atopic dermatitis: disease burden, measurement, and treatment benefit. Am J Clin Dermatol. 2016;17(2):163–169. doi:10.1007/s40257-015-0171-3
- Chiesa Fuxench ZC. Atopic dermatitis: disease background and risk factors. Adv Exp Med Biol. 2017;1027:11–19. doi:10.1007/978-3-319-64804-0_2
- Barbarot S, Auziere S, Gadkari A, et al. Epidemiology of atopic dermatitis in adults: results from an international survey. Allergy Eur J Allergy Clin Immunol. 2018;73(6):1284–1293. doi:10.1111/all.13401
- Hay RJ, Johns NE, Williams HC, et al. The global burden of skin disease in 2010: an analysis of the prevalence and impact of skin conditions. J Invest Dermatol. 2014;134(6):1527–1534. doi:10.1038/jid.2013.446
- Laughter MR, Maymone MBC, Mashayekhi S, et al. The global burden of atopic dermatitis: lessons from the Global Burden of Disease Study 1990–2017*. Br J Dermatol. 2021;184(2):304–309. doi:10.1111/bjd.19580
- Odhiambo JA, Williams HC, Clayton TO, Robertson CF, Asher MI; ISAAC Phase Three Study Group. Global variations in prevalence of eczema symptoms in children from ISAAC Phase Three. J Allergy Clin Immunol. 2009;124(6):1251–1258.e23. doi:10.1016/j.jaci.2009.10.009
- Kumar MK, Singh PK, Tahir MMA. The clinico-epidemiological profile and the risk factors associated with the severity of atopic dermatitis (AD) in eastern Indian children. J Clin Diagnostic Res. 2012;6(7 SUPPL):1162–1166.
- Sehgal V, Srivastava G, Aggarwal A, Saxena D, Chatterjee K, Khurana A. Atopic dermatitis: a cross-sectional (descriptive) study of 100 cases. Indian J Dermatol. 2015;60(5):519. doi:10.4103/0019-5154.164412
- Jawade SA, Chugh VS, Gohil SK, Mistry AS, Umrigar DD. A clinico-etiological study of dermatoses in pediatric age group in tertiary health care center in South Gujarat region. Indian J Dermatol. 2015;60(6):635. doi:10.4103/0019-5154.169147
- Upendra Y, Keswani N, Sendur S, Pallava A. The clinico-epidemiological profile of atopic dermatitis in residential school children: a study from South Chhattisgarh, India. Indian J Paediatr Dermatol. 2017;18(4):281. doi:10.4103/ijpd.ijpd_52_17
- Tsai TF, Rajagopalan M, Chu CY, et al. Burden of atopic dermatitis in Asia. J Dermatol. 2019;46(10):825–834. doi:10.1111/1346-8138.15048
- Kanwar A, De D. Epidemiology and clinical features of atopic dermatitis in India. Indian J Dermatol. 2011;56(5):471. doi:10.4103/0019-5154.87112
- Senra MS, Wollenberg A. Psychodermatological aspects of atopic dermatitis. Br J Dermatol. 2014;170(SUPPL. 1):38–43. doi:10.1111/bjd.13084
- Handa S, Jain N, Narang T. Cost of care of atopic dermatitis in India. Indian J Dermatol. 2015;60(2):213. doi:10.4103/0019-5154.152573
- Rajagopalan M, De A, Godse K, et al. Guidelines on management of atopic dermatitis in India: an evidence-based review and an expert consensus. Indian J Dermatol. 2019;64(3):166. doi:10.4103/ijd.IJD_683_18
- Sathishkumar D, Gupta A, Saini K. Atopic dermatitis in children: an update for pediatricians. Curr Med Issues. 2020;18(4):317. doi:10.4103/cmi.cmi_81_20
- Eichenfield LF, Tom WL, Chamlin SL, et al. Guidelines of care for the management of atopic dermatitis: section 1. Diagnosis and assessment of atopic dermatitis Work Group. J Am Acad Dermatol. 2014;70(2):338–351. doi:10.1016/j.jaad.2013.10.010
- Vakharia PP, Chopra R, Silverberg JI. Systematic review of diagnostic criteria used in atopic dermatitis randomized controlled trials. Am J Clin Dermatol. 2018;19(1):15–22. doi:10.1007/s40257-017-0299-4
- Silvestre Salvador J, Romero-Pérez D, Encabo-Durán B. Atopic dermatitis in adults: a diagnostic challenge. J Investig Allergol Clin Immunol. 2017;27(2):78–88. doi:10.18176/jiaci.0138
- Sinclair W, Aboobaker J, Green RJ, Levin ME. Diagnosis of atopic dermatitis: from bedside to laboratory. South African Med J. 2014;104(10):711. doi:10.7196/SAMJ.8850
- Kim JP, Chao LX, Simpson EL, Silverberg JI. Persistence of atopic dermatitis (AD): a systematic review and meta-analysis. J Am Acad Dermatol. 2016;75(4):681–687.e11. doi:10.1016/j.jaad.2016.05.028
- Dhar S, Bisweswar Mandal AG. Epidemiology and clinical pattern of atopic dermatitis in 100 children seen in a city hospital. Indian J Dermatol. 2002;47(4):202–204.
- Yang G, Seok JK, Kang HC, Cho YY, Lee HS, Lee JY. Skin barrier abnormalities and immune dysfunction in atopic dermatitis. Int J Mol Sci. 2020;21(8):1–14. doi:10.3390/ijms21082867
- Magnifico I, Petronio GP, Venditti N, et al. Atopic dermatitis as a multifactorial skin disorder. Can the analysis of pathophysiological targets represent the winning therapeutic strategy? Pharmaceuticals. 2020;13(11):1–18. doi:10.3390/ph13110411
- Totte JEE, van der Feltz WT, Hennekam M, van Belkum A, van Zuuren EJ, Pasmans SGMA. Prevalence and odds of S taphylococcus aureus carriage in atopic dermatitis: a systematic review and meta-analysis. Br J Dermatol. 2016;175(4):687–695. doi:10.1111/bjd.14566
- Kurien G, Divakaran MV, Sadanandan SM, Sobhanakumari K, Sarin A, Jagadeesan S. Methicillin-resistant Staphylococcus aureus colonization and disease severity in atopic dermatitis: a cross-sectional study from South India. Indian J Dermatol, Venereol Leprol. 2014;80(3):229–234. doi:10.4103/0378-6323.132250
- Langan SM, Irvine AD, Weidinger S. Atopic dermatitis. Lancet. 2020;396(10247):345–360. doi:10.1016/S0140-6736(20)31286-1
- LeBovidge JS, Elverson W, Timmons KG, et al. Multidisciplinary interventions in the management of atopic dermatitis. J Allergy Clin Immunol. 2016;138(2):325–334. doi:10.1016/j.jaci.2016.04.003
- Frazier W, Bhardwaj N. Atopic dermatitis: diagnosis and treatment. Am Fam Physician. 2020;101(10):590–598.
- Nankervis H, Thomas KS, Delamere FM, Barbarot S, Rogers NK, Williams HC. Scoping systematic review of treatments for eczema. Program Grants Appl Res. 2016;4(7):1–480. doi:10.3310/pgfar04070
- Green C, Colquitt JL, Kirby J, Davidson P. Topical corticosteroids for atopic eczema: clinical and cost effectiveness of once-daily vs. more frequent use. Br J Dermatol. 2005;152(1):130–141. doi:10.1111/j.1365-2133.2005.06410.x
- Berke R, Singh A, Guralnick M. Atopic dermatitis: an overview. Am Fam Physician. 2012;86(1):35–42.
- Drucker AM, Eyerich K, de Bruin-Weller MS, et al. Use of systemic corticosteroids for atopic dermatitis: international Eczema Council consensus statement. Br J Dermatol. 2018;178(3):768–775. doi:10.1111/bjd.15928
- Yu SH, Drucker AM, Lebwohl M, Silverberg JI. A systematic review of the safety and efficacy of systemic corticosteroids in atopic dermatitis. J Am Acad Dermatol. 2018;78(4):733–740.e11. doi:10.1016/j.jaad.2017.09.074
- Sidbury R, Davis DM, Cohen DE, et al. Guidelines of care for the management of atopic dermatitis: section 3. Management and treatment with phototherapy and systemic agents. J Am Acad Dermatol. 2014;71(2):327–349. doi:10.1016/j.jaad.2014.03.030
- Garritsen FM, Brouwer MWD, Limpens J, Spuls PI. Photo(chemo)therapy in the management of atopic dermatitis: an updated systematic review with implications for practice and research. Br J Dermatol. 2014;170(3):501–513. doi:10.1111/bjd.12645
- Rashmi Sarkar AJK. Clinico-epidemiological profile and factors affecting severity of atopic dermatitis in north Indian children. Indian J Dermatol. 2004;49(3):117–122.
- Karthikeyan K, Thappa DM, Jeevankumar B. Pattern of pediatric dermatoses in a referral center in South India. Indian Pediatr. 2004;41(4):373–377.
- Handa S, Khullar G, Pal A, Kamboj P, De D. Filaggrin gene mutations in hand eczema patients in the Indian subcontinent: a prospective case-control study. Contact Dermatitis. 2019;80(6):359–364. doi:10.1111/cod.13233
- Jain C, Das S, Ramachandran VG, Saha R, Bhattacharya SN, Dar S. Malassezia yeast and cytokine gene polymorphism in atopic dermatitis. J Clin Diagnostic Res. 2017;11(3):DC01–DC05. doi:10.7860/JCDR/2017/23948.9474
- Dhar S, Kanwar AJ. Epidemiology and clinical pattern of atopic dermatitis in a north Indian pediatric population. Pediatr Dermatol. 1998;15(5):347–351. doi:10.1046/j.1525-1470.1998.1998015347.x
- Kim JE, Kim HJ, Lew BL, et al. Consensus guidelines for the treatment of atopic dermatitis in Korea (part II): systemic treatment. Ann Dermatol. 2015;27(5):578–592. doi:10.5021/ad.2015.27.5.578
- Fujii M. Current understanding of pathophysiological mechanisms of atopic dermatitis: interactions among skin barrier dysfunction, immune abnormalities and pruritus. Biol Pharm Bull. 2020;43(1):12–19. doi:10.1248/bpb.b19-00088
