Abstract
Granular parakeratosis is an uncommon acquired keratinization disorder that occurs in the armpit, groin, and other parts of the body. It may be related to stimulation by detergents and antiperspirants. This article reports a case of granular parakeratosis in the groin. The patient was a young man with no predisposing factors. The clinical manifestations included symmetrical bilateral inguinal erythema, dryness, and a small amount of bran-like desquamation. After histopathological examination, the final diagnosis was granular parakeratosis, which was cured by topical application of glucocorticoid cream and silicone oil cream. Granular parakeratosis is a rare skin disease of unknown etiology. Clinicians need to pay attention to this disease and differentiate it from various diseases to avoid misdiagnosis.
Introduction
Granular parakeratosis (GP) is a rare keratotic skin disorder. It was first reported by Northcutt et al in 1991. The lesions of the four adult patients in their study were all axillary, and histopathological examination of the skin lesions showed epidermal parakeratosis and basophilic transparent keratin granule deposition. The authors referred to this phenomenon as GP and proposed a diagnosis of axillary GP.Citation1 In 1998, Mehregan first reported GP in the non-axillary region.Citation2 Since then, GPs that occur in the groin, perianal, intermammary, and lower breast regions have been reported, and the disease can occur in children.Citation3–Citation6 This article reports a case of GP in the groin of a young man who was misdiagnosed with eczema. The GP was aggravated by use of compound flumetasone ointment (a two-compound ointment with 0.2 mg/g flumetasone and 30 mg/g salicylic acid). This report aims to draw the attention of dermatological clinicians to this possibility and to prevent misdiagnoses.
Case Presentation
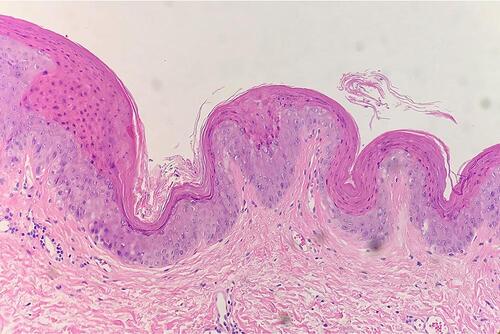
The patient was a 29-year-old man with scrotal and groin erythema for one month. He developed erythema in the scrotum and groin, which gradually expanded without significant aggravation on February 16, 2022. Half a month later, the patient visited a school hospital and was diagnosed with eczema. The erythema worsened and the skin lesions increased after topical application of flumethasone salicylic acid ointment. At first visit, no obvious abnormality was found in the examination of the systemic organs. Dermatological examination revealed well-demarcated erythema in the scrotum and bilateral groin with central hyperpigmentation and peripheral dry skin, with a small number of bran-like scales (). There was no obvious abnormality on the skin of the patient’s axilla or perianal folds. Histological analysis revealed increased hyperkeratosis (thickened stratum corneum) and parakeratosis (retention of nuclei in cornified cells), with numerous clear keratin granules in the stratum corneum. There was mild hyperplasia and hypertrophy of the spinous layer, no intercellular oedema, and normal morphology of basal layer cells. In the superficial layer of the dermis, the blood vessels were also noted to be dilated and congested. Mild perivascular lymphocyte-dominated infiltration (). Fungal culture and microscopic examination did not reveal any abnormalities.
Figure 1 Clinical manifestation of GP. In the groin and scrotum, red macules and patches are seen, with well-defined borders, dry surfaces, and overlying desquamation.

Figure 2 The histopathological finding of GP. Histological changes are mainly located in the stratum corneum of the epidermis. It reveals hyperkeratosis, parakeratosis, numerous transparent keratin granules in the stratum corneum (H&E staining, ×200).
The patient was healthy and denied any history of trauma or infectious diseases. He also denied using antiperspirants and deodorants and had never been exposed to mercury and various metals. Based on the clinical manifestations and histopathological findings, the final diagnosis was GP. The skin lesions disappeared after 2 weeks of topical glucocorticoid and silicone oil cream. There was no recurrence after 3 months of follow-up.
Discussion
GP often occurs in the folds and is characterized by erythema, with varying degrees of hyperpigmentation, and it may be accompanied by significant pruritus in some patients. The etiology of this disease is unclear. Some studies have shown that patients develop symptoms after exposure to zinc oxide, deodorants, antiperspirants, benzalkonium chloride, and drugs for the treatment of melasma.Citation7,Citation8 Therefore, it is speculated that the disease may be a form of contact dermatitis. However, this hypothesis cannot explain the phenomenon of unilateral disease in patients with bilateral irritant exposure who do not have a previous history of irritant exposure. In recent years, some researchers have successfully induced GP in mice using aluminum chloride. They found that impaired filaggrin processing leads to the production of basophilic granules.Citation9 GP usually occurs in areas vulnerable to friction, and some patients experience exacerbation in summer and remission in winter.Citation10 Therefore, some researchers believe that local sweating, humidity, friction, mechanical stimulation, and obesity may be predisposing factors for GP.Citation11,Citation12 In addition, local dermatophyte infections, bacterial infections, and other reports related to GP have been published.Citation13,Citation14 GP may also be a manifestation of other dermatological or systemic diseases such as GP combined with ichthyosis, atopic dermatitis, dermatomyositis myositis, or tumor-related GP.Citation7,Citation8,Citation15,Citation16 Therefore, physical examination of the entire body cannot be ignored in the clinical evaluation of GP.
There are various clinical types of GP. A previous case report summarized GP into intertriginous GP (axillary GP), GP of the eccrine ostium, follicular GP, granular parakeratotic acanthoma, incidental GP.Citation8 GP is a rare clinical condition with diverse clinical manifestations. Thus, a differential diagnosis is required for an accurate diagnosis. Differential diagnoses may mainly include eczema, contact dermatitis, jock itch, reverse psoriasis, and chronic familial benign pemphigus. Because of the typical histopathological features, histopathological examination is of great value for rashes of intertriginous sites with unclear diagnosis and suboptimal treatment. But it should be emphasized that GP can also be a pathological non-specific change. Histopathological changes similar to GP are also seen in molluscum contagiosum, dermatophytosis, actinic keratosis, basal cell carcinoma, and squamous cell carcinoma. Therefore, pathologists need to combine the comprehensive analysis of cell morphology and atypia, viral inclusion bodies, fungal hyphae and spores to make a correct pathological diagnosis.
GP has a favorable prognosis and several treatment options, and its effect varies widely. Some patients recover spontaneously after discontinuing the stimulant, and there are also reports that oral isotretinoin and antibacterial drugs, topical glucocorticoids, tretinoin, and vitamin D3 derivatives are effective.Citation17–Citation20 There have also been cases of successful treatment with freezing, botulinum toxin injection, and Nd: YAG combined with CO2 fractional laser therapy.Citation1,Citation21,Citation22 In this patient, GP occurred in the groin without an identifiable cause. However, the skin lesions were aggravated with the use of salicylic acid glucocorticoid ointment. Thus, salicylic acid stimulation may be the reason for the aggravation. After the stimulating drugs were discontinued, the patient was administered topical hydrocortisone butyrate cream and silicone oil cream, and the skin lesions disappeared.
Conclusion
GP is a rare, acquired, keratotic skin disorder that often presents with erythema in the folds. The cause of GP is unknown and may be related to exposure to irritants. Clinically, it needs to be differentiated from other skin diseases in the folds, and histopathological examination can help to confirm the diagnosis. GP has various treatment options and a favorable prognosis.
Consent Statement
The patient had given written informed consent for the publication of his clinical details and accompanying images. Institutional approval is not required for this case study.
Disclosure
Qingxia Lin and Dong Zhang are co-first authors for this study. The authors have no conflicts of interest to declare.
Additional information
Funding
References
- Northcutt AD, Nelson DM, Tschen JA. Axillary granular parakeratosis. J Am Acad Dermatol. 1991;24(4):541–544. doi:10.1016/0190-9622(91)70078-G
- Mehregan DA, Thomas JE, Mehregan DR. Intertriginous granular parakeratosis. J Am Acad Dermatol. 1998;39(3):495–496. doi:10.1016/S0190-9622(98)70333-0
- Wohlrab J, Luftl M, Wolter M, Marsch WC. Submammary granular parakeratosis: an acquired punctate hyperkeratosis of exogenic origin. J Am Acad Dermatol. 1999;40(5 Pt 2):813–814.
- Trowers AB, Assaf R, Jaworsky C. Granular parakeratosis in a child. Pediatr Dermatol. 2002;19(2):146–147. doi:10.1046/j.1525-1470.2002.00044.x
- Patrizi A, Neri I, Misciali C, Fanti PA. Granular parakeratosis: four paediatric cases. Br J Dermatol. 2002;147(5):1003–1006. doi:10.1046/j.1365-2133.2002.04953.x
- Akkaya AD, Oram Y, Aydin O. Infantile granular parakeratosis: cytologic examination of superficial scrapings as an aid to diagnosis. Pediatr Dermatol. 2015;32(3):392–396. doi:10.1111/pde.12444
- Robinson AJ, Foster RS, Halbert AR, King E, Orchard D. Granular parakeratosis induced by benzalkonium chloride exposure from laundry rinse aids. Australas J Dermatol. 2017;58(3):e138–e140. doi:10.1111/ajd.12551
- Chirasuthat P, Chirasuthat S, Suchonwanit P. Follicular granular parakeratosis: a case report, literature review, and proposed classification. Skin Appendage Disord. 2021;7(2):144–148. doi:10.1159/000512950
- Fujii M, Kishibe M, Honma M, Anan T, Ishida-Yamamoto A. Aluminum chloride-induced apoptosis leads to keratinization arrest and granular parakeratosis. Am J Dermatopathol. 2020;42(10):756–761. doi:10.1097/DAD.0000000000001513
- Kossard S, White A. Axillary granular parakeratosis. Australas J Dermatol. 1998;39(3):186–187. doi:10.1111/j.1440-0960.1998.tb01280.x
- Ding CY, Liu H, Khachemoune A. Granular parakeratosis: a comprehensive review and a critical reappraisal. Am J Clin Dermatol. 2015;16(6):495–500. doi:10.1007/s40257-015-0148-2
- Nelson G, Lien MH, Messina JL, Ranjit S, Fenske NA. Submammary granular parakeratosis treated with mastopexy. J Drugs Dermatol. 2017;16(8):810–812.
- Resnik KS, Kantor GR, DiLeonardo M. Dermatophyte-related granular parakeratosis. Am J Dermatopathol. 2004;26(1):70–71. doi:10.1097/00000372-200402000-00011
- Kumarasinghe SPW, Chandran V, Raby E, Wood B. Hyperkeratotic flexural erythema responding to amoxicillin-clavulanic acid therapy: report of four cases. Australas J Dermatol. 2019;60(4):311–314. doi:10.1111/ajd.13069
- Resnik KS, DiLeonardo M. Incidental granular parakeratotic cornification in carcinomas. Am J Dermatopathol. 2007;29(3):264–269. doi:10.1097/DAD.0b013e3180465860
- Pock L, Hercogova J. Incidental granular parakeratosis associated with dermatomyositis. Am J Dermatopathol. 2006;28(2):147–149. doi:10.1097/01.dad.0000171604.71057.3e
- Webster CG, Resnik KS, Webster GF. Axillary granular parakeratosis: response to isotretinoin. J Am Acad Dermatol. 1997;37(5 Pt 1):789–790. doi:10.1016/S0190-9622(97)70119-1
- Chamberlain AJ, Tam MM. Intertriginous granular parakeratosis responsive to potent topical corticosteroids. Clin Exp Dermatol. 2003;28(1):50–52. doi:10.1046/j.1365-2230.2003.01159.x
- Brown SK, Heilman ER. Granular parakeratosis: resolution with topical tretinoin. J Am Acad Dermatol. 2002;47(5 Suppl):S279–280. doi:10.1067/mjd.2002.109252
- Contreras ME, Gottfried LC, Bang RH, Palmer CH. Axillary intertriginous granular parakeratosis responsive to topical calcipotriene and ammonium lactate. Int J Dermatol. 2003;42(5):382–383. doi:10.1046/j.1365-4362.2003.01722.x
- Ravitskiy L, Heymann WR. Botulinum toxin-induced resolution of axillary granular parakeratosis. Skinmed. 2005;4(2):118–120. doi:10.1111/j.1540-9740.2005.03700.x
- Laimer M, Emberger M, Brunasso AM, Ahlgrimm-Siess V, Massone C. Laser for the treatment of granular parakeratosis. Dermatol Surg. 2009;35(2):297–300. doi:10.1111/j.1524-4725.2008.01052.x
