Abstract
Bullous pemphigoid (BP) is an autoimmune blistering disease mainly affecting elderly individuals. Comorbidities are common in patients with BP and have been found to complicate the management and prognosis. We describe a patient with multiple comorbidities who was successfully treated with omalizumab and suggest omalizumab as a good alternative therapy for BP to prevent treatment-related complications in elderly patients with a poor general condition.
Introduction
Bullous pemphigoid (BP) is an autoimmune disorder that mainly affects those over 70 years of age, with a rising incidence in the past decade.Citation1 Studies have revealed an association between BP and other major chronic conditions affecting elderly individuals, such as neuropsychiatric disorders, hypertension, diabetes mellitus, and chronic kidney disease.Citation2,Citation3 These comorbid conditions make the traditional immunosuppressive therapy of BP with systemic corticosteroids relatively contraindicated. Thus, alternative treatment with a favorable safety profile is of great benefit for this group of BP patients. The underlying pathophysiological mechanism of BP is thought to be IgG class autoantibodies against autoantigens BP 180 and BP230 at the basement membrane zone. IgE anti-BP180 autoantibodies were also found to be pathogenic in recent studies.Citation4 Omalizumab, a humanized monoclonal antibody directed against IgE, has been found to be useful in the treatment of BP.Citation5 Here, we report a patient with multiple comorbidities and uncontrolled blood glucose who was recalcitrant to systemic corticosteroid therapy and successfully treated with omalizumab.
Case Report
A 76-year-old male was admitted to our department with a 1-month history of severely itchy erythema, papules, blistering, and scratching. The rash initially appeared on the torso, with subsequent progression to the extremities and face and gradually with blister formation, despite ongoing treatment with oral antihistamines, thalidomide, compound glycyrrhizin tablets, and super potent topical corticosteroids.
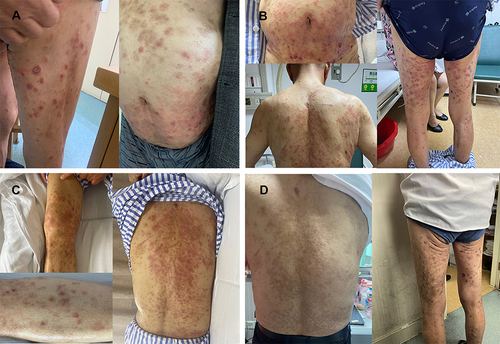
On admission, the patient was afebrile with urticarial erythema and papules on the face, trunk, and extremities. Isolated tense blisters and bullae could be observed on the abdomen and bilateral thighs (). The Nikolsky sign was negative. There was no erosion or ulceration of the mucosa.
Figure 1 (A) On admission, urticarial erythema and papules on the trunk and extremities. Isolated tense blisters and bullae on the abdomen and bilateral thighs (B and C) erythema on the back and lower limbs progressed, with more new vesicles continuing to appear on the legs. (D) Erythema transformed into hyperpigmentation.
In addition, the patient had multiple comorbidities, including hypertension and type 2 diabetes mellitus (T2DM) for over 20 years, diabetic nephropathy for more than 4 years, and a history of “sudden deafness” for more than 5 years. He also had a surgical history of percutaneous coronary intervention (PCI) of anterior descending and circumflex branches for 10 years. He was under a regimen of several drugs for his comorbidities, but he denied taking any new medications during recent months.
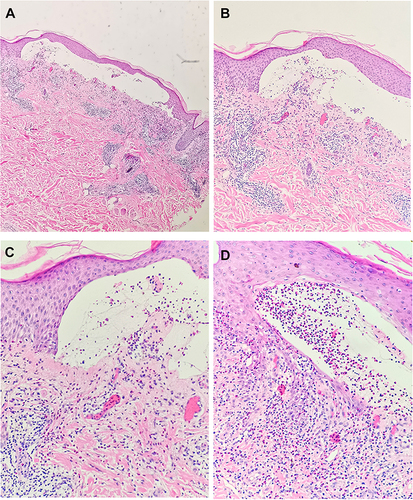
The laboratory tests revealed significantly increased IgE levels (>2000.00 kIU/L) and eosinophilia (0.76*10^9/L), elevated HbA1c (7.60%), creatinine (141 μmol/L) and uric acid (601 μmol/L), and decreased total protein (56.1 g/L) and albumin (33.8 g/L). Serum BP230 IgG antibodies were positive. Urine routine analysis showed urine glucose++++, urine microalbumin +++. Histopathological examination from a skin biopsy of the left thigh demonstrated subepidermal blister formation with eosinophilic infiltrate, dermal vascular proliferation with lymphocytes, and eosinophil infiltration ().
Figure 2 Pathology of skin biopsy from the lesions on the left thigh showed subepidermal blister formation with eosinophilic infiltrate, dermal vascular proliferation with lymphocytes, and eosinophil infiltration. (A) Magnification ×40, (B) magnification × 100, (C) magnification × 200, (D) magnification × 200.
A diagnosis of bullous pemphigoid was made based on the classical clinical and histopathological findings and positive serum BP230 antibody. Thus, intravenous methylprednisolone 60 mg per day was given along with compound glycyrrhizin injection, oral antihistamines, thalidomide, and super potent topical corticosteroids. However, the regimen failed to control the disease. Erythema on the back and lower limbs progressed, with more new vesicles continuing to appear on the legs (). His pruritus also deteriorated. While his skin lesions and pruritus resisted responding to systemic steroid therapy, the side effects of the treatment were very prominent, exacerbating his type 2 diabetes mellitus. His fasting and postprandial blood glucose was exceedingly high even though endocrinologists were consulted frequently to adjust his diabetes medications. Considering that his diabetic nephropathy and other diabetic complications might deteriorate and based on the available reports, omalizumab was initiated at a dose of 300 mg subcutaneously every 4 weeks to taper systemic steroids. The pruritus was alleviated, and new blisters stopped appearing after 3 days. The dose of systemic steroid was gradually tapered without any flare. One month after the initiation of omalizumab, the patient’s blood eosinophils returned to normal, but his serum IgE level remained high (>2000.00 kIU/L). On the 2nd dose of omalizumab, the patient only had slight itching, and the erythema transformed into hyperpigmentation (). He had 3 injections of omalizumab in total, and systemic steroids were gradually tapered to a daily dose of 4 mg of methylprednisolone. On recent follow-up, 8 months after discontinuation of omalizumab injection, he remained on a maintenance dose of 4 mg of methylprednisolone and remained in clinical remission. Lab tests showed normal eosinophils and decreased IgE levels (782.00 kIU/L).
Discussion
BP is the most common autoimmune blistering disease that typically affects the elderly individuals. The global incidence of bullous pemphigoid is 0.0419 per 1000 person-years.Citation6 BP has been reported to be significantly associated with mortality, with 1-year mortality rates ranging from 6% to 41%.Citation7 Two studies based on Chinese hospitals reported 1-year mortality rates of 12.9% and 23.4%, respectively.Citation8,Citation9
BP has been demonstrated to have an association with comorbid health conditions such as neuropsychiatric disorders, hypertension, diabetes mellitus, chronic kidney disease, and end-stage renal disease.Citation2,Citation3 These comorbidities have been found to complicate the management and prognosis.Citation10 BP in patients with comorbid T2DM have a significantly greater medical comorbidity and complication burden and are more challenging to manage.Citation10 BP has also been found to be associated with a 5-fold higher risk of cardiovascular disease mortality.Citation11 Our patient had a long history of cardiovascular disease (CVD), T2-DM, and diabetic nephropathy. As a potential risk factor for complications and mortality, his multiple comorbidities called for more urgent and prompt control of his skin condition.
The systemic treatment with the highest level of evidence for BP is glucocorticoids.Citation12 As many of these comorbidities might be worsened by glucocorticoids, steroid-sparing strategies are often necessary for these patients. The traditional steroid-sparing strategies mainly include immunosuppressive therapy, such as methotrexate (MTX), azathioprine, and cyclosporin A. The application of these therapies is restricted in the elderly because of their potential severe adverse effects. In recent years, biologics such as rituximab, omalizumab, and dupilumab have been shown to be effective in BP treatments with a favorable safety profile.Citation13–15 Our patient was recalcitrant to traditional systemic glucocorticoid therapy and had exceedingly high blood glucose levels after treatment. His renal function may have been further impaired if traditional immunosuppressive drugs, such as MTX and cyclosporine A, were used. Considering the risk of traditional therapy on his multiple comorbidities, omalizumab was added in an attempt to rapidly control disease progression and accelerate the tapering of glucocorticoids. The application of omalizumab in our patient successfully resulted in rapid resolution.
The laboratory tests of our patient revealed significantly elevated IgE levels and eosinophilia. It has been reported that 50% to 60% of BP patients have peripheral eosinophilia, and 70% to 85% of BP patients have elevated total IgE serum levels.Citation16 A study found that IgE antibodies against the 16th noncollagenous domain of BP180 (BP180 NC16A) paralleled disease activity. This finding supports the notion that anti-BP180 IgE is of pathogenic relevance.Citation17 A study also suggested a putative relationship between disease severity and peripheral eosinophilia.Citation18 In our patient, peripheral eosinophilia indicated disease severity, and elevated IgE levels were consistent with the symptoms of severe itching and urticarial erythema.
Omalizumab is a recombinant humanized IgG1 monoclonal antibody against human IgE.Citation19 Omalizumab effectively treats BP either as a monotherapy or in combination with other drugs.Citation5 The mechanism of action of omalizumab on BP is not fully understood. A study showed that the efficacy of omalizumab might be related to a reduction in FcepsilonRI and IgE expression in lesional skin of BP.Citation20 Thus, serum IgE levels might be associated with the response to omalizumab treatment in BP. Although it has been proven in chronic spontaneous urticaria that the clinical response to omalizumab is linked to and predicted by IgE levels and their change, the data on omalizumab in BP treatment are not sufficient to obtain a similar conclusion.Citation5,Citation21 However, a systematic review of existing evidence on omalizumab treatment of BP showed a marginal association between baseline eosinophilia and complete remission.Citation5 Due to the limited sample size, the role of IgE and eosinophilia in predicting the BP response to omalizumab requires further investigation.
Conclusion
In this case, we report a 76-year-old patient with multiple comorbidities who was relatively contraindicated for immunosuppressive therapy. Initiation with omalizumab showed a rapid response with a good safety profile. Our case suggests omalizumab as a good alternative therapy for BP to prevent treatment-related complications in a vulnerable, elderly population. Further research, especially randomized controlled trials, is required to investigate the role of omalizumab in the treatment of BP, especially in elderly patients with multiple comorbidities.
Data Sharing Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Ethics Statement
Written informed consent was obtained from the individual for the publication of any potentially identifiable images or data included in this article. Institutional approval was not required for this case details.
Approval and Consent to Participate
All authors have approved to this submission to your esteemed journal. Its publication is also approved tacitly by the responsible authorities where the work was carried out.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to give sincere thanks to the patient and his family for understanding and supporting the publication of the case.
References
- Schmidt E, Zillikens D. Pemphigoid diseases. Lancet. 2013;381(9863):320–332. doi:10.1016/S0140-6736(12)61140-4
- Lee S, Rastogi S, Hsu DY, Nardone B, Silverberg JI. Association of bullous pemphigoid and comorbid health conditions: a case-control study. Arch Dermatol Res. 2021;313(5):327–332. doi:10.1007/s00403-020-02100-2
- Ren Z, Hsu DY, Brieva J, Silverberg NB, Langan SM, Silverberg JI. Hospitalization, inpatient burden and comorbidities associated with bullous pemphigoid in the U.S.A. Br J Dermatol. 2017;176(1):87–99. doi:10.1111/bjd.14821
- Hashimoto T, Ohzono A, Teye K, et al. Detection of IgE autoantibodies to BP180 and BP230 and their relationship to clinical features in bullous pemphigoid. Br J Dermatol. 2017;177(1):141–151. doi:10.1111/bjd.15114
- D’Aguanno K, Gabrielli S, Ouchene L, et al. Omalizumab for the treatment of bullous pemphigoid: a systematic review of efficacy and safety. J Cutan Med Surg. 2022:12034754221089267. doi:10.1177/12034754221089267.
- Lu L, Chen L, Xu Y, Liu A. Global incidence and prevalence of bullous pemphigoid: a systematic review and meta-analysis. J Cosmet Dermatol. 2022. doi:10.1111/jocd.14797
- Lee JH, Kim SC. Mortality of patients with bullous pemphigoid in Korea. J Am Acad Dermatol. 2014;71(4):676–683. doi:10.1016/j.jaad.2014.05.006
- Li J, Zuo YG, Zheng HY. Mortality of bullous pemphigoid in China. JAMA Dermatol. 2013;149(1):106–108. doi:10.1001/archdermatol.2012.2994
- Zhang LM, Wu J, Xiao T, et al. Treatment and mortality rate of bullous pemphigoid in China: a hospital-based study. Eur J Dermatol. 2013;23(1):94–98. doi:10.1684/ejd.2012.1906
- Patel S, Ahsanuddin S, Cadwell JB, Lambert WC. The impact of diabetes mellitus on medical complication and mortality rates among inpatients with bullous pemphigoid. Ir J Med Sci. 2021. doi:10.1007/s11845-021-02726-9
- Shen WC, Chiang HY, Chen PS, Lin YT, Kuo CC, Wu PY. Risk of all-cause mortality, cardiovascular disease mortality, and cancer mortality in patients with bullous pemphigoid. JAMA Dermatol. 2021. doi:10.1001/jamadermatol.2021.5125
- Kibsgaard L, Bay B, Deleuran M, Vestergaard C. A retrospective consecutive case-series study on the effect of systemic treatment, length of admission time, and co-morbidities in 98 bullous pemphigoid patients admitted to a tertiary centre. Acta Derm Venereol. 2015;95(3):307–311. doi:10.2340/00015555-1925
- Yoo DS, Lee JH, Kim SC, Kim JH. Mortality and clinical response of patients with bullous pemphigoid treated with rituximab. Br J Dermatol. 2021;185(1):210–212. doi:10.1111/bjd.19890
- Kremer N, Snast I, Cohen ES, et al. Rituximab and omalizumab for the treatment of bullous pemphigoid: a systematic review of the literature. Am J Clin Dermatol. 2019;20(2):209–216. doi:10.1007/s40257-018-0401-6
- Zhang Y, Xu Q, Chen L, et al. Efficacy and safety of dupilumab in moderate-to-severe bullous pemphigoid. Front Immunol. 2021;12:738907. doi:10.3389/fimmu.2021.738907
- van Beek N, Schulze FS, Zillikens D, Schmidt E. IgE-mediated mechanisms in bullous pemphigoid and other autoimmune bullous diseases. Expert Rev Clin Immunol. 2016;12(3):267–277. doi:10.1586/1744666X.2016.1123092
- van Beek N, Luttmann N, Huebner F, et al. Correlation of serum levels of IgE autoantibodies against BP180 with bullous pemphigoid disease activity. JAMA Dermatol. 2017;153(1):30–38. doi:10.1001/jamadermatol.2016.3357
- Kridin K. Peripheral eosinophilia in bullous pemphigoid: prevalence and influence on the clinical manifestation. Br J Dermatol. 2018;179(5):1141–1147. doi:10.1111/bjd.16679
- Gonul MZ, Keseroglu HO, Ergin C, Ozcan I, Erdem O. Bullous pemphigoid successfully treated with omalizumab. Indian J Dermatol Venereol Leprol. 2016;82(5):577–579. doi:10.4103/0378-6323.183628
- Seyed Jafari SM, Gadaldi K, Feldmeyer L, Yawalkar N, Borradori L, Schlapbach C. Effects of omalizumab on FcepsilonRI and IgE expression in lesional skin of bullous pemphigoid. Front Immunol. 2019;10:1919. doi:10.3389/fimmu.2019.01919
- Ertas R, Ozyurt K, Atasoy M, Hawro T, Maurer M. The clinical response to omalizumab in chronic spontaneous urticaria patients is linked to and predicted by IgE levels and their change. Allergy. 2018;73(3):705–712. doi:10.1111/all.13345
