Abstract
Papular elastorrhexis (PE) is a rare disorder of dermal elastic fibers, which presents as firm, hypopigmented papules, commonly distributed on the trunk and extremities. The facial area is rarely involved. We report the case of a 47-year-old woman with multiple asymptomatic, soft, skin-colored facial papules whose histopathological features are compatible with PE. Facial PE may be a variant of PE, and special staining in showing changes in both elastic and collagen fibers may be of great value in diagnosis.
Introduction
Papular elastorrhexis (PE) is a rare acquired elastolytic disorder that usually occurs within the first or second decade of life and is characterized by asymptomatic, firm, discrete, nonfollicular, and hypopigmented papules. The lesions usually localize on the trunk and extremities.Citation1 To date, only 2 cases with facial involvement have been reported.Citation2,Citation3 The histopathologic features of PE are fragmentation and focal absence of elastic fibers, while the changes of collagen fibers are inconsistencies.Citation1,Citation4 In this report, we would like to present the first case of facial PE in China and to demonstrate, for the first time, changes in collagen fibers in PE lesions using Masson staining.
Case Report
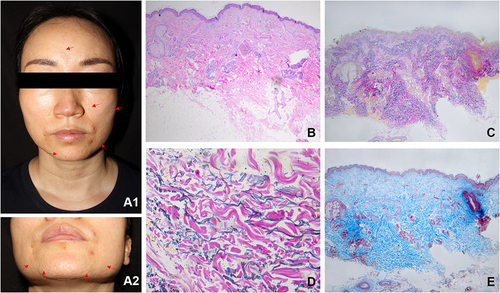
A 47-year-old woman presented with asymptomatic papules on her face for 10 years, no significant medical history indicated. There was no previous inflammation, long-term sunlight exposure or trauma, except for the occasional pimples around the mouth. No family history of similar dermatosis was noted. Dermatological examination revealed multiple, nonfollicular, skin-colored, discrete papules on the mandibular regions, nose, cheeks, and forehead ( and ). The papules were soft, with no sense of cystic sensation on palpation. The skin between the papules was normal, and no same eruptions were found on her neck or axillae. Skin biopsy revealed unremarkable changes in epidermis and slight fibrosis in the dermis on hematoxylin and eosin staining (). Elastin staining (Verhoeff-Van Gieson) revealed patchy loss and prominent fragmentation of elastic fibers throughout the dermis ( and ). Focal collagen hyperplasia was found on Masson staining (). The diagnosis of PE was made, and the patient received no treatment. There were no significant changes on a 1-year follow-up.
Figure 1 Multiple, skin-colored papules on face (The red arrows mark several of these typical papules). Near the left corner of the mouth, there are 2 red follicular papules (diagnosed as acne) (A1 and A2). Normal epidermis with slight fibrosis in the dermis (B) (H&E, 40×). Patchy loss of elastic fibers throughout the dermis with no correlation to hair follicles (C) (Verhoeff-Van Gieson, 40×). Prominent elastic fragmentation (D) (Verhoeff-Van Gieson, 400×). Focal hyperplasia of collagen bundles in the mid-dermis (E) (Masson staining, 40×).
Discussion
PE is a rare acquired elastolytic skin disorder with a skeptical etiopathogenesis.Citation1 It is mostly considered to be a non-familial disorder, while an isolated case of familial clustering has been reported.Citation1,Citation5 Therefore, both acquired and familial forms of PE were believed to be existed.Citation6 No systemic involvement has been reported.Citation1,Citation5 For slow-appearing lesions on sun-exposed area such as face, we should first consider whether it is related to sunlight exposure. No history of long-term sun exposure or signs of solar damage were found in the pathological findings of the facial PE cases, suggesting that ultraviolet radiation may play a minor role in the pathogenesis of facial PE.
PE is characterized by asymptomatic, nonfollicular, firm papules on the trunk and extremities. Facial involvement is rare. Şahin et alCitation2 reported a 30-year-old male patient with lesions on face, scalp, and retroauricular region, which developed in an eruptive fashion. Santonja et alCitation3 reported another case of facial PE, whose clinical presentations were exactly the same with our patient— gradually appearing, soft, skin-colored papules on face, except that the patient was much older, and the papules were more numerous and more widespread on face. Although not mentioned in Şahin et al’s case,Citation2 these facial papules were likely to be soft, which was different from conventional PE.
The diagnostic pathological manifestations of PE are focal absence and prominent fragmentation of elastic fibers.Citation1,Citation6 Changes in collagen fibers vary, and no detailed description has been documented.Citation6 We found marked focal collagen hyperplasia by using Masson staining, while only slight fibrosis in a diffused manner could be seen in H&E staining. This reminded us that Masson staining might be a great tool in the diagnosis of facial PE.
The differential diagnosis of multiple, noninflammatory papules on the face includes tumors of epithelial origin (such as syringoma), and cystic lesions (such as milia), all of which can be differentiated easily by histopathologic findings. Other papular dermatoses with fragmentation or diminution of elastic fibers such as anetoderma, pseudoxanthoma elasticum-like papillary dermal elastolysis (PXE-PDE), mid-dermal elastolysis (MDE) and pseudoxanthoma elasticum (PXE) should also be differentiated.Citation1,Citation6 These diseases can be distinguished from PE by their specific clinical and pathological manifestations. For example, the papules of anetoderma have a cystic sensation on palpation, while PE has not, and the lesions of papular acne scars are perifollicular, while PE are nonfollicular. The diagnostic characteristic for PXE-PDE shows nearly complete loss of elastic tissue in the papillary dermis, and for MDE, it appears a band-like loss of elastic fibers in the mid-dermis, which can be differentiated with PE.Citation1,Citation6,Citation7 The papules of PXE have the tendency to coalesce into plaques with cobblestone appearance. Histopathology reveals fragmented, curled, thickened mineralized elastic fibers in mid and deep reticular dermis, which can be seen on H&E staining, while the fragmentation of elastic fibers of PE can only be seen on elastic staining.Citation1,Citation8
There is no reliable curative treatment for PE, and it has no tendency for spontaneous resolution.Citation1 Reassure the patients with the benign nature of PE is the most important.
Conclusion
PE is a benign disease with only cosmetic concerns. It is important to distinguish PE from other papular dermatoses that need to rule out systemic involvement, such as anetoderma, MDE and PXE. What is more, clinicians should be aware that facial PE may be another variant of PE. When it comes to histologic diagnosis, we would like to stress the importance of special staining in showing changes in both elastic and collagen fibers.
Consent Statement
Written informed consent was provided to the patient to have the case details and associated images published. Institutional approval was not required to publish the case details.
Disclosure
The authors report no conflicts of interest in this work.
Additional information
Funding
References
- Sezer E, Durmaz EÖ, Şahin S. Papular elastorrhexis: clinical perspectives. Clin Cosmet Investig Dermatol. 2018;11:541–544. doi:10.2147/CCID.S151020
- Şahin S, Durmaz EÖ, Sezer E, Çetin ED. Eruptive papular elastorrhexis of the face and scalp. J Am Acad Dermatol. 2013;69(5):251–252. doi:10.1016/j.jaad.2013.05.027
- Santonja C, Salinas S, Requena L, Kutzner H, Valverde R. Late-onset facial papular elastorrhexis. Am J Dermatopathol. 2018;40(12):930–932. doi:10.1097/DAD.0000000000001215
- Lee SH, Sung NH. The importance of collagen tissue in papular elastorrhexis, eruptive collagenoma, and nevus anelasticus. Ann Dermatol. 2016;28(2):210–215. doi:10.5021/ad.2016.28.2.210
- Schirren H, Schirren CG, Stolz W, Kind P, Plewig G. Papular elastorrhexis: a variant of dermatofibrosis lenticularis disseminata (Buschke-Ollendorff syndrome)? Dermatology. 1994;189(4):368–372. doi:10.1159/000246881
- Lewis KG, Bercovitch L, Dill SW, Robinson-Bostom L. Acquired disorders of elastic tissue: part II. Decreased elastic tissue. J Am Acad Dermatol. 2004;51(2):165–185. doi:10.1016/j.jaad.2004.03.016
- Zemheri E, Subasi B, Zindanci I, Ozkanli S, Zenginkinet T, Karadag AS. Mid-dermal elastolysis on face, unusual localization: a case report. J Med Cases. 2014;5(16):334–336. doi:10.14740/jmc1771w
- Andrés-Ramos I, Alegría-Landa V, Gimeno I, et al. Cutaneous elastic tissue anomalies. Am J Dermatopathol. 2019;41(2):85–117. doi:10.1097/DAD.0000000000001275
