Abstract
Introduction
Shared decision making (SDM) is a collaborative process involving both healthcare providers and patients in making medical decisions, which gains increasing prominence in healthcare practice. But evidence on the level of SDM in medical practice and barriers as well as stimulus during the SDM implementation among aesthetic dermatologists is limited in China.
Methods
From July to August 2023, 1938 dermatologists were recruited online in China. Data were collected through an electronic questionnaire covering: (1) demographic features; (2) SDM questionnaire physician version (SDM-Q-Doc); and (3) stimulus and barriers in SDM implementation. Logistic regression was applied to explore factors associated with SDM practice, barriers, and stimulus of SDM implementation, respectively.
Results
The 1938 dermatologists included 1329 females (68.6%), with an average age of 35 years. The total SDM score ranged from 0 to 45, with a median value of 40 (IQR: 35–44), and the median stimulus score and barriers scores were 28 (IQR: 24–32) and 19 (IQR: 13–26), respectively. The prevalence of good SDM was 27.2%, logistic regression indicated that female dermatologists (odds ratio, OR=1.21, 95% confidence interval, CI: 0.96–1.51), and dermatologists with more years of aesthetic practice had a higher proportion of good SDM practice (OR was 1.44 for 5–9 years, 1.58 for 10–15 years and 1.77 for over 15 years). Moreover, female dermatologists and dermatologists with higher education level and serviced in private settings had lower barrier scores; female dermatologists and dermatologists with more years of aesthetic practice had higher stimulus scores.
Conclusion
Chinese aesthetic dermatologists appear to implement SDM at an active level, with more stimulus and less barriers in SDM implementation. The integration of SDM into clinical practice among dermatologists is beneficial both for patients and dermatologists. Moreover, SDM practice should be strongly promoted and enhanced during medical aesthetics, especially among male dermatologists, dermatologists with less working experience, and those who work at public institutions.
Introduction
Shared decision making (SDM) has gained increasing prominence in healthcare practice with the rising recognition of patient-centered care in past decades.Citation1–3 It involves a collaborative process where healthcare providers and patients make a medical decision together.Citation4 The clinician provides information on treatment options, benefits, and risks, while the patient provides information about their preference and treatment goals. Besides achieving an agreement aligned with patient’s value, SDM is also equally critical to offer comfort and support to the family or surrogate as an essential aspect of shared decision making.Citation5 Constantly, patients highlight the communication with the healthcare providers as being one of their most important concerns, with the majority of the patient’s family members or surrogates expressing a desire for both themselves and physicians to be actively involved in the medical decision-making process.Citation6,Citation7 SDM implementation could increase patients’ quality of life, and patients who experience higher levels of SDM participation have better reported health outcomes and decreased healthcare utilization.Citation7
Medical aesthetics has been experiencing substantial growth in China since the 1980s due to the cultural attitudes toward beauty, societal pressures, and the growing demand for cosmetic procedures, with a Compound Annual Growth Rate (CAGR) ranging from 17% to 23% in the past 5 years.Citation8 The overall medical aesthetic market is expected to reach a valuation of $50 billion by 2026. It is worth noting that medical aesthetic industry in China comprises more than 10,000 facilities, including hospitals, outpatient centers, and clinics, all regulated by the China Healthcare Commission. The aim of medical aesthetic intervention is to enhance an individual’s overall appearance and well-being, with procedures typically driven by the patient’s desires rather than medical necessity, and the subjective nature of beauty standards, potential psychological implications of aesthetic procedures, and ethical considerations could also influence the decision-making dynamics, all of which demonstrates the significant value of SDM for the selection of treatment options in medical aesthetics.Citation9–11 However, evidence demonstrating whether SDM is universally applied or not is not yet understood and studied in China.Citation12,Citation13
Previous studies indicated that Chinese physicians perceived SDM with high willingness (78.38%) based on the discrete-choice experiment (DCE) survey and the SDM questionnaire physician version (SDM-Q-Doc) survey.Citation14 However, studies focusing on SDM in the areas of medicine aesthetic or aesthetic surgery are still lacking, especially with the rising medical aesthetic demands in China. Moreover, Koyama et alCitation4 stated that factors that promote or hinder SDM implementation might be modified by the specific type of hospital where the physicians work. In China, the three main types of clinical institutions are distinctly regulated by various healthcare regulations, they exhibit distinctions at various aspects, encompassing service scope, level of service complexity, area size and service room setting, and number and specialty of healthcare providers. Besides, dermatologists working in public or private institutions encounter distinct leadership dynamics, organizational cultures, revenue structure, and patient expectations. Such differences may strengthen or weaken the SDM implementation upon the institution type. Unfortunately, there is a notable absence of the level of SDM in medical practice among aesthetic dermatologists, and also the comparative studies focusing on the aforementioned research line in China.
In this study, we implemented a cross-sectional survey to investigate the medical decision-making practice, the barriers, and stimulus during medical encounters among aesthetic dermatologists. Besides, to further explore the potential influencing factors associated with a good SDM practice among Chinese aesthetic dermatologists.
Methods
Study Design
During July and August 2023, we conducted this cross-sectional survey among Chinese dermatologists online at Umer Doctor APP (Shanghai Maise Information Technology Co., Ltd). Sample size was calculated based on the formula for the cross-sectional study, we set the proportion of aesthetic dermatologists with good SDM practice (those achieving over 80% of SDM scores) as 50%, α=0.05, δ=5% of p, and a non-response rate of 15%, so a total of 1767 aesthetic dermatologists should be recruited. In this study, the aesthetic dermatologist was a convenience sample selected online at Umer Doctor APP, and data for SDM were collected from the spontaneous response among dermatologists with digital informed consent. In this study, 1938 aesthetic dermatologists whose practice license is active in China mainland and practices medical aesthetics with no less than 12 months experience completed the interview and are included in the final data analysis. This study was reviewed and approved by the Institutional Review Board of Shanghai Skin Diseases Hospital, Medical School, Tongji University (2022–31), and was in line with the Helsinki Declaration.
Data Collection
In this study, data were collected through electronic questionnaire on Umer Doctor APP. The online questionnaire covered four parts: (1) demographic features including age, sex, education, professional qualification, institution type, private or public institutions, and years of practice in medical aesthetics; (2) SDM-Q-Doc,Citation14 which consists of nine questions, and the response to each items was assessed through a six-point Likert scale with 0=completely disagree, 1=strongly disagree, 2=somewhat disagree, 3=somewhat agree, 4=strongly agree, and 5=completely agree – the total SDM score is the aggregation of responses to the 9 questions, which ranges from 0 to 45 with a higher score indicating the most active level of SDM implementation in medical encounters; (3) barriers for SDM implementation includes eight questions, the response to each items was assessed through a five-point Likert scale with 1=completely disagree and 5= completely agree – the total score of barriers is an aggregation of responses to the 8 questions, which ranges from 0 to 40 with a higher score indicating more barriers in SDM implementation; and (4) stimulus for SDM implementation consists of seven questions, and the response to each item was also assessed through a five-point Likert scale with 1= completely disagree and 5=completely agree – the total score of stimulus ranges from 0 to 35 with a higher score indicating more stimulus in SDM implementation.
Index Definition
In this study, good SDM practice among aesthetic dermatologists is defined as those who achieved ≥44 score out of the total 45 score based on SDM-Q-Doc, which was the 75th percentile value of SDM score. Similarly, we define a higher barrier score as those who achieved ≥26 score out of the total 50 score based on their responses to barriers in SDM implementation, and define a higher stimulus score as those who achieved ≥32 score out of the total 35 score based on their responses to stimulus in SDM implementation. In this study, age is classified into <30 years, 30–39 years, 40–49 years and >50 years. Education splits into four groups of college and lower, graduate, master's, and doctor/post-doctor. Professional qualification consists of resident, attending physician, associated chief physician, and chief physician. Institution type refers to the groups of general hospital, specialized hospital, outpatient center, and clinics. Years of aesthetic practice is divided into <5 years, 5–9 years, 10–15 years, and >15 years. Healthcare setting is classified into public institutions and private institutions.
Data Analysis
In this study, SAS 9.4 was employed for data analysis. Quantitative variables are presented as the mean and standard deviation (SD) or median and interquartile range (IQR) as appropriate. We applied Student’s t-test or Mann–Whitney U-tests to examine the difference between groups for quantitative variables. Qualitative variables were described as frequency counts and proportion (%), and the chi-square test was used for statistical significance testing between groups. The odds ratio (OR) and 95% confidence interval (95% CI) were calculated to explore factors associated with good SDM practice, barriers of SDM implementation, and stimulus of SDM implementation, respectively. The box plot was produced to show the distribution of the SDM practice score, the barrier score, and the stimulus score of SDM implementation, and the scatter plot was produced to show the correlation between them. Moreover, the forest tree plot was produced to show potential influencing factors associated with the good SDM practice, barriers of SDM implementation, and stimulus of SDM implementation based on logistic regression, respectively. In this study, we set a P value less than 0.05 as statistically significant.
Results
In this study, the median age of the 1938 aesthetic dermatologists was 35 years (IQR: 30–40 years). Approximately 68% of dermatologists were female and 42% of them had master's and above education. In this study, fewer than 20% of the dermatologists were chief physician or associated chief physician, 59% of them worked in the general hospital, and fewer than 40% of the dermatologists worked in the private institutions. The median years of aesthetic practice was 5 years (IQR: 3–10 years). indicates that male dermatologists were older than female dermatologists, had a higher proportion of master's and above education, had a higher proportion of being chief physician or associated chief physician, with longer years of aesthetic practice, but a lower proportion of servicing in a general hospital than female dermatologists; the differences were all statistically significant (P<0.05) (.
Table 1 Demographic Features of 1938 Dermatologists Who Practice Medical Aesthetics in China
SDM Scores and Scores for Barrier and Stimulus in SDM Implementation
In this study, SDM implementation among aesthetic dermatologists was evaluated based on the SDM-Q-Doc with 9 questions. indicates that the proportion of completely agree (score 5) responses among dermatologists ranged from 40.3% to 57.2%, and the proportion of completely disagree (score 0) responses ranged from 0.1% to 0.4%. The total SDM score ranged from 0 to 45, with a median value of 40 score (IQR: 35–44) (, .
Table 2 The Total Shared Decision Making (SDM) Score Based on SDM-Q-Doc Among the 1938 Dermatologists Who Practice Medical Aesthetics in China
Figure 1 The score of shared decision making (SDM), score of barriers for SDM implementation, and score of stimulus for SDM implementation among 1938 dermatologists who practice medical aesthetics in China.
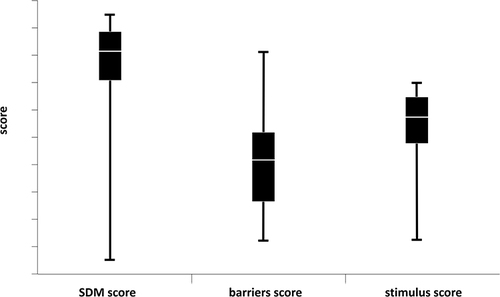
indicates the scores for barriers in SDM implementation. The proportion of completely disagree (score 1) responses to the eight questions ranged from 22.9% to 52.1%, and the proportion of completely agree (score 5) ranged from 10.3% to 16.1%. The total score of barriers in SDM implementation ranged from 7 to 40, with a median value of 19 score (IQR: 13–26). also indicates the scores for stimulus in SDM implementation. The proportion of completely disagree (score 1) responses to the seven questions ranged from 1.1% to 15.9%, and the proportion of completely agree (score 5) ranged from 28.6% to 47.6%. The total score of stimulus in SDM implementation ranged from 7 to 35, with a median value of 28 score (IQR: 24–32) (, .
Table 3 The Barriers and Stimulus for Shared Decision Making (SDM) Implementation Among the 1938 Dermatologists Who Practice Medical Aesthetics in China
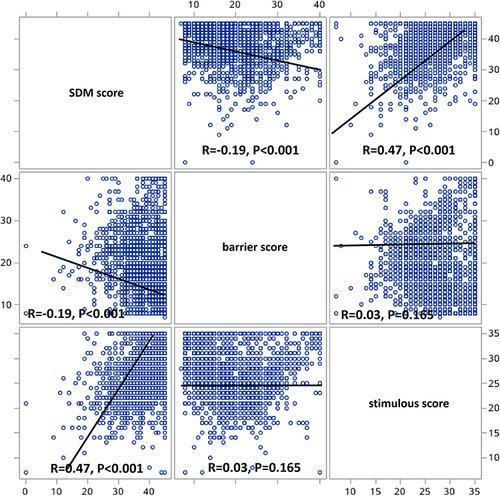
depicts the correlation between SDM score and score of barrier as well as scores of stimulus during SDM implementation. The SDM score of dermatologists was positively correlated with their stimulus score (r=0.47, P<0.001), and was negatively correlated with their barrier score (r=−0.19, P<0.001). Whereas the correlation between the barrier score and the stimulus score among dermatologists was not statistically significant (r=0.03, P=0.165) (.
Factors Associated with Good SDM Practice
In this study, 528 out of 1938 dermatologists achieved ≥44 scores based on the SDM-Q-Doc, the proportion of good SDM practice was 27.2% (95% CI: 25.3–29.3%). The chi-square test indicated that aesthetic dermatologists with older age had a higher proportion of good SDM practice, and the proportion of good SDM practice was higher among dermatologists with higher professional qualification, with more years of aesthetic practice, and those serving in private institutions and working in ambulatory centers and clinics (.
Table 4 The Influencing Factors for Those Achieved Higher Shared Decision Making (SDM) Score, Score of Barriers for SDM Implementation, and Score of Stimulus for SDM Implementation Among 1938 Dermatologists Who Practice Medical Aesthetics in China
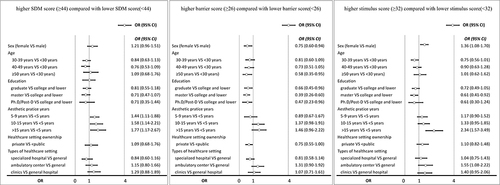
The logistic regression indicated that female dermatologists had higher proportion of good SDM practice (OR=1.21, 95% CI: 0.96–1.51) than male dermatologists. Dermatologists with more years of aesthetic practice had higher proportion of good SDM practice, the OR was 1.44 (95% CI: 1.11–1.88) for those with 5–9 years, 1.58 (95% CI: 1.14–2.21) for those with 10–15 years, and 1.77 (95% CI: 1.17–2.67) for those with over 15 years, in comparison with those with less than 5 years of aesthetic practice. Dermatologists serviced in ambulatory center (OR=1.15, 95%: 0.80–1.66) and clinics (OR=1.29, 95%: 0.88–1.89) also tended to have higher proportion of good SDM practice, but without statistical significance (.
Figure 3 The influencing factors for those who achieved higher score of shared decision making (SDM), score of barriers for SDM implementation, and score of stimulus for SDM implementation among the 1938 dermatologists who practice medical aesthetics in China, an analysis based on multivariate logistic regression (MLR).
Factors Associated with the Barriers During SDM Implementation
In this study, 488 dermatologists achieved ≥26 scores in the evaluation of barriers in SDM implementation, the proportion of dermatologists with higher barrier score was 25.2% (95% CI: 23.3%-27.1%). Chi-square test indicated that female dermatologists had lower proportion of having a higher barrier score than male dermatologists. Moreover, dermatologists with higher education or with less aesthetic practice years were prone to have a lower proportion of achieving higher barrier score (.
Logistic regression indicated that female dermatologists had lower proportion of achieving higher barrier score (OR=0.75, 95% CI: 0.60–0.94) than male dermatologists. Dermatologists with older age and less aesthetic practice years tended to have lower barrier scores, but without statistical significance. In comparison with dermatologists with college and lower education, dermatologists with higher education level tended to have lower proportion of achieving higher barrier scores, the OR was 0.66 (95% CI: 0.45–0.96) for those with graduate, 0.39 (95% CI: 0.26–0.60) for those with master's, and 0.47 (95% CI: 0.23–0.96) for those with Ph.D/Post-D education. Moreover, dermatologists serviced in private settings (OR=0.75, 95%: 0.55–1.00) also had lower proportion of achieving higher barrier scores (.
Factors Associated with the Stimulus in SDM Implementation
In this study, 543 dermatologists achieved ≥32 scores in the evaluation of stimulus in SDM implementation, the proportion was 28.0% (95% CI: 26.1–30.0%). Chi-square test indicated that dermatologists with older age had higher proportion of achieving a higher stimulus score, and the proportion of higher stimulus score was higher among dermatologists with more years of aesthetic practice, those serving in private institutions and working in clinics, ambulatory centers, and specialized hospital (.
Logistic regression indicated that female dermatologists had higher proportion of achieving higher stimulus score (OR=1.36, 95% CI: 1.08–1.70) than male dermatologists. Dermatologists with more aesthetic practice years also had higher stimulus score; the OR was 1.17 (95% CI: 0.90–1.52) for those with 5–9 years, 1.33 (95% CI: 0.95–1.85) for those with 10–15 years, and 2.34 (95% CI: 1.57–3.49) for those with over 15 years, in comparison with those with less than 5 years of aesthetic practice (.
Discussion
To our knowledge, this is the first study in China to explore the SDM implementation among aesthetic dermatologists and its associated barriers and stimulus in SDM practice. The findings indicated that Chinese dermatologists had high perception on SDM during their aesthetic practice, and female dermatologists, dermatologists with longer aesthetic practice years, and serving in ambulatory centers and clinics had higher SDM scores. In addition, the SDM scores was positive associated with the stimulus score, but negatively associated with the barrier score. The gender, education level, and aesthetic practice years were associated with the stimulus score as well as the barrier score among the aesthetic dermatologists.
The SDM-Q-Doc is primarily developed as a psychometrically tested instrument to evaluate the SDM process among physicians.Citation15 Considering its broadly tested psychometrics and multiple language availability, the SDM-Q-Doc appears to be the prioritized approach to measure the decision-making process from physician perspective. Therefore, the SDM implementation among dermatologists was assessed through the 9-item SDM-Q-Doc in this study, which covered: (1) recognizing the need for a decision; (2) establishing an equal partnership; (3) outlining treatment alternatives; (4) providing details on the advantages and drawbacks of options; (5) assessing the patient’s comprehension and expectations; (6) pinpointing preferences of both parties; (7) engaging in negotiation; (8) achieving a mutual decision; and (9) organizing follow-up procedures.Citation16–18
In this study, most of the dermatologists reported to have a high-level implementation of SDM during the clinical practice. The median SDM sum score was 88.9 after standardizing the raw score (median value was 40) by a linear transformation to convert the score into a scale ranging from 0 to 100, which demonstrates Chinese dermatologists situate a decent level in implementing SDM, and the finding was in line with previous studies.Citation4,Citation14 A cross-sectional study implemented in Japan showed that the mean SDM score was 76.9 among 129 physicians who worked at university hospital and municipal hospitals.Citation4 Another Chinese SDM study regarding lung cancer treatment also indicated that the mean SDM score was 85.4 among 185 physicians.Citation14,Citation19 Meanwhile, It is also worth noting that the high level of self-reported SDM implementation could be partially due to the overestimation of SDM competencies among aesthetic dermatologists in this study. The reasoning is supported by a review which indicated that the actual decision-making behavior appeared to be rather paternalistic, although most physicians had positive attitudes toward SDM.Citation20
Apparently, the extent to which physicians use SDM in practice is influenced by individual factors.Citation21 In this study, we noticed that female dermatologists tend to have higher SDM score than male dermatologists during their SDM practices. Meanwhile, the stimulus scores during SDM implementation were also higher among female dermatologists. The finding regarding sex aligns with previous research indicating that female dermatologists exhibit more favorable SDM behavior compared to their male counterparts.Citation22 In instances where SDM was more effectively employed by female dermatologists, it encompassed aspects such as assisting patients in comprehending technical information, elucidating the benefits and risks of treatment options, and engaging in a comprehensive evaluation before collectively deciding on the preferred treatment option.
Apart from sex, the results for age suggested consistency with the previous studies stressing that age is a vital factor for SDM practice.Citation23 In this study, dermatologists with older age tended to have higher SDM scores and stimulus scores, but lower barriers scores. Compared to dermatologists older than 50 years who showed strong preference on SDM implementation, the findings indicated that the preferences of SDM implementation were similarly lower among dermatologists aged 30–39, 40–49, and below 30 years. The findings further confirmed that aesthetic dermatologists below age 50 years hold same preferences to implement SDM; this was partially aligned with a study that demonstrating age was an essential factor for SDM practice,Citation24 and this might due to the fact that younger dermatologists had more workloads than older dermatologists in China, and they had limited time to implement SDM in their clinical practice. So it worth further research with rigorous design like a prospective cohort to evaluate the effect of age on SDM implementation.
Regarding the years of aesthetic practice, working experience plays an essential role in the career. In this study, aesthetic dermatologists practicing 5 years and more would behave better in SDM and had higher stimulus score during SDM implementation compared to those practicing less than 5 years, and the group with aesthetic practice over 15 years have the strongest preferences. The results held the same points with a study which demonstrated that years of working experience positively relates to the behavioral change outcomes.Citation25 Rooting the current situation in China, the reason could be that dermatologists with aesthetic practice more than 15 years normally enjoy a great reputation in the industry and are easier to gain trust from patient to adopt shared decision-making practice. For younger physicians, they have less experience and are motivated to serve more patients to build their reputation and trust with the patients, so younger dermatologists have lower participation in SDM practice even with strong willingness. Interestingly, dermatologists with longer years of aesthetic practice in this study also reported more barriers in SDM implementation than those with less aesthetic practice years, and this might be due to that dermatologists with longer aesthetic practice years had higher expectation in SDM implementation to provide better service for their patients. But the true reason needs to be explored by in-depth interview in the future.
Previous studies indicate that the intention to engage in SDM among physicians varies between settings and disciplines.Citation26,Citation27 In this study, dermatologists who served at private healthcare settings had higher SDM sore and stimulus score, but had lower barrier score in SDM implementation than those who served at public healthcare settings. The results for institution type are in alignment with the previous studies that the type of care provided by different institutions would influence the extent to which dermatologists and patients actually participate in decision-making.Citation28,Citation29 For medical aesthetic practice in China, dermatologists who work at private institutions have more time to encounter each patient, as they see less number of patients per day than those from public institutions due to very different patient daily traffic; moreover, dermatologists in private institutions mainly see patients who seek aesthetics treatment only, while public dermatologists see patients with higher complexity but less proportion of aesthetics, and this helps understand the ground of why private practice adopts SDM more.
In this study, the Chinese aesthetic dermatologists implement SDM at an active level, with more stimulus and less barriers in SDM implementation. Whereas dermatologists still reported some barriers in SDM practice, which including the limited ability to participate among patients, the extra time need for SDM, and noisy and busy hospital settings. As depicted in a review study by Gravel et al,Citation30 the most important obstacles to implementing SDM were time constraints, features of patients, and clinical settings, which was in line with the findings in this study. Therefore, stakeholders and dermatologists as well should provide assistance for patients to improve their involvement in SDM practice.Citation31 Moreover, the incorporation of SDM into health policy objectives and instruments is also important for SDM implementation, and SDM could be promoted by training programs or educational initiatives focused on SDM skills resource development and funding streams, and providing techniques could also help standardize and improve SDM practice across diverse demographic and practice related groups.Citation32
This study has some limitations. First, data were collected through spontaneous response among dermatologists through online investigation, which is regarded as convenience sampling, and may weaken the representativeness of this study and could not represent all aesthetic dermatologists in China. Also, dermatologists who are more positive to SDM maybe prone to respond to this survey, while those who do not know or are negative to SDM may not respond. Second, this study missed the patient component; previous studies showed that the involvement of patients’ interaction provides a holistic understanding of SDM practice. But most of these studies were conducted in a small sample size, including a 50-physician survey conducted in DubaiCitation33 and a 66-provider survey conducted in Canada.Citation34 Given the sample size is approximately 2000 in this study, it is difficult to enroll the same number of patients to explore the interaction which is an inevitable challenge. Third, this study had information bias such as over-reporting; we measure the SDM implementation through self-reported questionnaires by the SDM-Q-DOC scale, and this may raise the possibility of respondents over-reporting their SDM implementation. Fourth, SDM implementation involves multiple stakeholders in healthcare systems, so it is important to consider the barriers and facilitators from multiple stakeholder perspectives to optimize the implementation effect. Whereas this study was only focused on the dermatologist’s perspective, which is another limitation. So the incorporation of some improvement such as face-to-face interview, multiple stakeholders, and a patient component in future study could ensure the in-depth understanding of SDM practice in China.
Conclusions
The integration of SDM into clinical practice among aesthetic dermatologists across various health disciplines worldwide is beneficial both for patients and dermatologists. Chinese aesthetics dermatologists appear to implement SDM at an active level, with more stimulus and less barriers in SDM implementation. Moreover, SDM practice should be strongly promoted and enhanced during medical aesthetics, especially among male dermatologists, junior dermatologists with less working experience, and among dermatologists who work at public institutions.
Abbreviations
SDM, Shared Decision Making; CAGR, Compound Annual Growth Rate; DCE, Discrete-Choice Experiment; SDM-Q-Doc, SDM Questionnaire Doctor Version; SD, Standard Deviation; CI, Confidence Interval; OR, Odds Ratio.
Ethics Approval and Consent to Participate
The study was reviewed and approved by the Review Board of Shanghai Skin Diseases Hospital of Tongji University (2022-31). Informed consent was signed online by each participant before the questionnaire interview.
Author Contributions
All authors in this paper made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgment
We would like to thank the Umer Doctor APP for providing the platform for data collection, all aesthetic dermatologists for participation, and Professor Michael Engelgau from US CDC for giving suggestions and comments for this manuscript.
Data Sharing Statement
Data in this study can be made available upon request to the corresponding author.
Additional information
Funding
References
- Willman AS. Shared decision making and remote consultation. BMJ Military Health. 2023;169(3):290–291. doi:10.1136/bmjmilitary-2022-002096
- Barry MJ, Susan EL. Shared decision making- pinnacle of patient-centered care. New Engl J Med. 2012;366(9):780–781. doi:10.1056/NEJMp1109283
- Vasudeva A, Sheikh NA. Shared decision making in health care. J Fam Med Prim Care. 2023;12(8):1737. doi:10.4103/jfmpc.jfmpc_2304_22
- Koyama T, Nawa N, Itsui Y, Okada E, Fujiwara T. Facilitators and barriers to implementing shared decision making: a cross-sectional study of physicians in Japan. Patient Educ Couns. 2022;105(7):2546–2556. doi:10.1016/j.pec.2022.01.016
- Entwistle VA, Watt IS. Patient involvement in treatment decision-making: the case for a broader conceptual framework. Patient Educ Couns. 2006;63(3):268–278. doi:10.1016/j.pec.2006.05.002
- Elwyn G, Frosch D, Thomson R, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27(10):1361–1367. doi:10.1007/s11606-012-2077-6
- Hughes TM, Merath K, Chen Q, et al. Association of shared decision-making on patient reported health outcomes and healthcare utilization. Am J Surg. 2018;216(1):7–12. doi:10.1016/j.amjsurg.2018.01.011
- China National Health Commission. Medical Aesthetics Service Regulation 2016. Available from: http://www.nhc.gov.cn/wjw/. Accessed May 7, 2024.
- Cranley LA, Slaughter SE, Caspar S, et al. Strategies to facilitate shared decision making in long term care. Int J Older People. 2020;15(3):e12314. doi:10.1111/opn.12314
- Kim DE, Kim MJ. Factors influencing shared decision making in long term care facilities. BMC Geriatr. 2023;23(1):577. doi:10.1186/s12877-023-04301-6
- Ubbink DT, Santema TB, Lapid O. Shared decision-making in cosmetic medicine and aesthetic surgery. Aesthetic Surg J. 2016;36(1):NP14–19. doi:10.1093/asj/sjv107
- Knops AM, Ubbink DT, Legenate DA, Dehaes JC, Goossens A. Information communicated with patients in decision making about their abdominal aortic aneurysm. Eur J Vasc Endovasc Surg. 2010;39(6):708–713. doi:10.1016/j.ejvs.2010.02.012
- Braddock CH, Edwards KA, Hasenberg NM, Laidley TL, Levinson W. Informed decision making in outpatient practice: time to get back to basics. JAMA. 1999;282(24):2313–2320. doi:10.1001/jama.282.24.2313
- Yan J, Wei Y, Teng Y, et al. Physician preferences and shared-decision making for the traditional Chinese medicine treatment of lung cancer: a discrete-choice experiment study in China. Patient Prefer Adherence. 2022;16:1487–1497. doi:10.2147/PPA.S365109
- Scholl I, Kriston L, Dirmaier J, Buchholz A, Harter M. Development and psychometric properties of the shared decision making questionnaire -physician version (SDM-Q-Doc). Patient Educ Couns. 2012;88(2):284–290. doi:10.1016/j.pec.2012.03.005
- Kriston L, Scholl I, Holzel L, Simon D, Loh A, Harter M. The 9-item Shared Decision Making Questionnaire (SDM-Q-9). Development and psychometric properties in a primary care sample. Patient Educ Couns. 2010;80(1):94–99. doi:10.1016/j.pec.2009.09.034
- Goto Y, Miura H, Son D, et al. Psychometric evaluation of the Japanese 9-Item shared decision-making questionnaire and its association with decision conflict and patient factors in Japanese primary care. JMA J. 2020;3(3):208–215.
- Nakayama K, Osaka W, Matsubara N, et al. Shared decision making, physicians’ explanations, and treatment satisfaction: a cross-sectional survey of prostate cancer patients. BMC Med Inf Decis Making. 2020;20:1–10. doi:10.1186/s12911-020-01355-z
- Chen ZR, Zhang L, Chen YW, et al. Correlation analysis between physicians’ evaluations of doctor-patient relationship and their preferences for shared decision-making in China. Front Psychiatry. 2022;13:946383. doi:10.3389/fpsyt.2022.946383
- Pollard S, Bansback N, Bryan S. Physician attitudes toward shared decision making: a systematic review. Patient Educ Couns. 2015;98(9):1046–1057. doi:10.1016/j.pec.2015.05.004
- Alguera LV, Dowsey MM, Ride J, Kinder S, Castle D. Shared decision making in mental health: the importance for current clinical practice. Australas Psychiatr. 2017;25(6):578–582. doi:10.1177/1039856217734711
- Alameddine M, Otaki F, Boukarroum K, et al. Patients’ and physicians’ gender and perspective on shared decision-making: a cross-sectional study from Dubai. PLoS One. 2022;17(9):e0270700. doi:10.1371/journal.pone.0270700
- Marphatia AA, Ambale GS, Reid AM. Women’s marriage age matters for public health: a review of the broader health and social implications in South Asia. Front Public Health. 2017;5:269–273. doi:10.3389/fpubh.2017.00269
- Zimmermann A, Bernuit D, Gerlinger C, Schaefers M, Geppert K. Prevalence, symptoms and management of uterine fibroids: an international internet-based survey of 21,746 women. BMC Women's Health. 2012;12(1):6–10. doi:10.1186/1472-6874-12-6
- Klassen RM, Chiu MM. Effects on teachers’ self-efficacy and job satisfaction: teacher gender, years of experience, and job stress. J Educ Psychol. 2010;102(3):741–745.
- Jeroen KJB, Trudy VDW, Erick WD, Heyligers IC. Experienced barriers in shared decision making behavior of orthopaedic surgery residents compared with orthopaedic surgeons. Musculosket Care. 2019;17:198–205.
- Farrelly S, Lester H, Rose D, et al. Barriers to shared decision making in mental health care: qualitative study of the joint crisis plan for psychosis. Health Expect. 2016;19(2):448–458. doi:10.1111/hex.12368
- Van-Den BMA, Spreeuwenberg P, Rijken M. Preferences and experiences of chronically ill and disabled patients regarding shared decision-making: does the type of care to be decided upon matter? Patient Educ Couns. 2011;84(1):111–117. doi:10.1016/j.pec.2010.07.032
- Mousazadeh Y, Jannati A, Jabbari BH, Asgharijafarabadi M, Ebadi A. Advantages and disadvantages of different methods of hospitals’ downsizing: a narrative systematic review. Health Promotion Perspect. 2013;3(2):276–287. doi:10.5681/hpp.2013.032
- Gravel K, Legare F, Graham ID. Barriers and facilitators to implementing shared decision making in clinical practice: a systematic review of health professionals’ perceptions. Implement Sci. 2006;1(6):1–16. doi:10.1186/1748-5908-1-16
- Alex W, Alyse L, Gerri S, Peter B. Barriers and facilitators to shared decision making in hospitals from policy to practice: a systematic review. Implement Sci. 2021;16:74. doi:10.1186/s13012-021-01142-y
- Legare F, Stacey D, Forest PG, et al. Shared decision making in Canada: update on integration of evidence in health decisions and patient-centered care government mandates. Z Evid Fortbild Qual Gesundhwes. 2022;171:22–29. doi:10.1016/j.zefq.2022.04.006
- Alameddine M, Algurg R, Otaki F, Alsheikh-Ali AA. Physicians’ perspective on shared decision-making in Dubai: a cross-sectional study. Hum Resour Health. 2020;18(1):33. doi:10.1186/s12960-020-00475-x
- Manhas KP, Olson K, Churchill K, et al. Measuring shared decision making and collaborative goal setting in community rehabilitation: a focused ethnography using cross-sectional surveys in Canada. BMJ Open. 2020;10(8):e034745. doi:10.1136/bmjopen-2019-034745