Abstract
Background and Objective
Nevus of Ota (NO), also known as “brownish-blue nevus of the palate of the eye”, is a benign dermal pigmentation that increases skin disease. The Q-switched ruby laser is a classic treatment for nevus of Ota in children, but the optimal age for treatment is still controversial. The aim of this study was to investigate the treatment effect of Q-switched ruby laser in children with nevus of Ota at different ages and the effect on psychological health status.
Materials and Methods
Children with nevus of Ota treated with Q-switched ruby laser in the Department of Dermatology of the Second Affiliated Hospital of Wenzhou Medical University from June 2015 to June 2019 were retrospectively analysed. And the mental health status was assessed using the CDI scale.
Results
In the preschool children group (0–7 year age), the significant efficacy rates was 93.1%, the average number of treatments was 3.6, and the overall incidence of adverse reactions was 4.7%. The significant efficacy rates in the school-age children group (7–14 year age) was 90.3%, the average number of treatments was 5.1, and the overall incidence of adverse reactions was 13.7%. The mean post-treatment CDI score in the preschool children group was 10.8, and 9.7% of children exceeding 19 points. The mean pre-treatment CDI score in the school-age children group was 17.3, and 24.6% of children exceeding 19 points. The mean post-treatment CDI score was 13.6 and 15.1% of children exceeded 19 points. The chi-square test for the significant efficacy rate of the two groups showed P>0.05, which was not statistically significant. The significant efficacy rate of the preschool group and that of the school-age children group. The t-test for the number of treatments in the two groups showed P<0.05, which was statistically significant. Adverse reactions in the two groups showed a statistically significant P<0.05. The mean CDI scores and the percentage of depressed individuals in the school-age children group were significantly lower after treatment than before treatment (p<0.05).
Conclusion
Q-switched ruby laser is safe and effective in treating nevus of Ota in children. Early treatment can reduce the number of treatments and the incidence of adverse reactions. In addition, early treatment can reduce children’s depression, which is beneficial to mental health.
Introduction
Nevus of Ota (NO), also known as “brownish-blue nevus of the palate”, is a benign dermal pigmentation disorder. Nevus of Ota is mostly seen in the area where the ophthalmic and maxillary branches of the trigeminal nerve are distributed, such as orbital, temporal, nasal, forehead and zygomatic areas,Citation1 with clinical manifestations of greyish-brown or bluish-grey patches, uneven colouring and unclear boundaries, and a large number of melanocytes can be seen in the papillary layer of the dermis and the upper part of the reticular layer. Most people with nevus of Ota develop it at birth, with another peak in adolescence. Nevus of Ota occurs in people of colour, such as Asians and Africans. The incidence of nevus of Ota is higher in females than in males, with a male-to-female ratio of about 1:4.8.Citation2 Nevus of Ota usually does not subside on its own, although it does not cause harm to the patient’s health, but it seriously affects the aesthetics and may bring a psychological burden to the patient and affect the patient’s daily life and work, so it needs to be actively treated. Traditional treatments include: CO2 laser, chemical peeling, skin dermabrasion, skin grafting surgery, freezing, etc. However, most of the treatments are unsatisfactory and are prone to cause pigment abnormalities, scarring and other adverse reactions, and are no longer used as a regular method of nevus of Ota treatment. Based on the theory of selective photothermal effect, selective laser has become the first choice of treatment for nevus of Ota patients.Citation3 The Q-switched ruby laser is the classic treatment for nevus of Ota.Citation4–6 However, it is still controversial when is the best age to treat nevus of Ota in children. Some scholars believe that early treatment of nevus of Ota in children is more effective and can avoid the psychological problems caused by nevus of Ota in children’s growth.Citation7,Citation8 However, some scholars believe that children patients usually do not cooperate in the treatment, and there may be some risks if general anaesthesia is chosen.Citation9 And if local anaesthesia is chosen, psychological trauma may be left due to pain during the treatment.
In order to study the impact of nevus of Ota on children’s mental health, we used the CDI scale for assessment. The CDI scale, known as the Child Depression Inventory (CDI), was adapted by Kovacs from the Beck’s Depression Inventory (BDI) for adults, and is used to measure depression in children and Adolescent Depressive Mood Scale. The scale is intended for children and adolescents between the ages of 7 and 17 years and is based on self-perceptions over a two-week period. The CDI consists of 27 questions and contains five factors: negative affect, interpersonal problems, inefficiency, lack of pleasure, and negative self-esteem. A scale of 0,1,2 for “occasionally”, “often”, and “always” was used to indicate the frequency of symptoms, with a total score of 54. A cut-off score of 19 was used to identify depressive symptoms based on the norm of the original scale.Citation10
This paper analyzes the clinical efficacy and safety of the Q-switched ruby laser on pediatric patients with nevus of Ota in different age groups through a retrospective study. The impact of nevus of Ota on children’s mental health status was also investigated by assessing children’s mental health status through Children’s Depression Inventory (CDI).
Materials and Methods
Retrospective analysis of patients with nevus of Ota who received Q-switched ruby laser treatment from June 2015 to June 2019 in the Department of Dermatology of the Second Affiliated Hospital of Wenzhou Medical University. Inclusion criteria: (1) Children with nevus of Ota aged 0–14 years old who recorded complete information; (2) did not receive other treatments; (3) lesions were located on the face and local anaesthesia was chosen. Exclusion criteria: (1) patients with scarring; (2) those with active local skin infections; (3) those suffering from coagulation disorders or other diseases unsuitable for laser treatment.
Procedures
This study was approved by the independent ethics committee of the Second Affiliated Hospital of Wenzhou Medical University and Yuying Children’s Hospital. The patient’s guardian had signed an informed consent form at the start of the treatment allowing images and data from the treatment period to be used for medical research. And agree to allow the use of images in the thesis as long as privacy is protected.
The treatment instrument was a Q-switched ruby laser produced by Asclepion Laser Company of Germany. The treatment parameters were set as follows: wavelength of 694 nm, pulse width of 10 ns, energy density of 5.5–7.5 J/cm2, and spot diameter of 4 mm. The risks associated with laser treatment, the expected effects of laser treatment, and the methods of postoperative care of laser treatment were described and explained to the patient’s family members prior to the treatment, and written informed consent was obtained from the patient’s family. Basic patient information (name, gender, age, etc.) was collected. Photographs were taken with a camera before each treatment for efficacy observation. Parameters were set according to the patient’s age, skin type, lesion site, and lesion colour. Lidocaine cream (5%) was applied externally and sealed for more than 1h before treatment, and the surface anaesthetic was removed and the treatment area was disinfected after the application. During the treatment, attention should be paid to the protection of the patient’s eyes. The operator should wear goggles and the patient should wear an eye mask. The laser treatment handpiece was perpendicular to the treatment area, without overlapping or missing, and the clinical endpoint was an immediate grey-white cream reaction. After laser treatment, cold compresses are applied for 15–30 minutes to reduce post-procedural pain and swelling. Fusidic acid cream was then applied topically for about 7 d to prevent infection, and sunlight was avoided after treatment. The interval between laser treatments is generally 3–6 months, depending on the condition. The occurrence of adverse reactions was followed up and recorded after treatment. Adverse reactions included erythema, oedema, blisters, crusting, scarring, abnormal pigmentation and hypopigmentation. Follow-up was performed until 6 months-2 years after the end of treatment.
Children’s mental health status was assessed by the Children’s Depression Inventory (CDI) Children with a CDI score of ≥19 were judged to have a depressed mood. The CDI was assessed pre-treatment and 3 years post-treatment in paediatric patients in the 7–14 year age group. Paediatric patients in the 0–7 year age group were assessed after 3 years of treatment for those who had reached the age of 7 years.
Assessment
The degree of skin lesion regression was evaluated by two physicians who were not involved in this study through pre-treatment and post-treatment photographs.
Level of efficacyI: pigmentation clearing <30%; Level of efficacyII: pigmentation clearing 30%~75%; Level of efficacy III: pigmentation clearing 75%~90%; Level of efficacy IV: pigmentation clearing ≥90%. Significant efficacy rates = (III+IV)/total number of treated cases×100%.
Statistical Analysis
Use SPSS Statistics (version 23.0; IBM Company, Armonk NY, USA) to analyze the data. And the P value <0.05 is considered statistically significant.
Results
A total of 159 paediatric patients with nevus of Ota, with an age range of 3 months to 14 years, were included in this study. According to the typology proposed by Tanino, 43 cases of type I nevus of Ota, 65 cases of type II nevus of Ota, and 23 cases of type III nevus of Ota were included in this study. We defined children from 3 months of age to 7 years of age as preschool children and children from 7 to 14 years of age as school-age children. The preschool group children group contained 86 child patients with nevus of Ota, 25 males and 61 females, with a mean age of 3.2 years. The school-age children group contained 73 child patients with nevus of Ota, 17 males and 56 females, with a mean age of 10.3 years ().
Table 1 Clinical Characteristics of Pediatric Patients with Nevus of Ota in the School-Age and Preschool Groups
After 1–7 treatments, 6 (6.9%) patients in the preschool children group achieved level of efficacy II, 48 (55.8%) patients achieved level of efficacy III, and 32 (37.2%) patients achieved level of efficacy IV, with a significant efficacy rate of 93.1%, and the average number of treatments was 3.6. In the group of school-age children, after 3–10 treatments, 7 (9.5%) patients achieved level of efficacy II, 44 (60.2%) patients achieved level of efficacy III, and 22 (30.1%) patients achieved level of efficacy IV, with a significant efficacy of 90.1%, and the average number of treatments was 5.1 times. The chi-square test for the significant efficacy rate of the two groups showed P>0.05, which was not statistically significant, indicating that there was no significant difference between the significant efficacy rate of the preschool group and that of the school-age children group. The t-test for the number of treatments in the two groups showed P<0.05, which was statistically significant, indicating that the number of treatments in the preschool children group was significantly smaller than that in the school-age children group ( and ). Common adverse reactions such as transient local erythema, oedema and crusting occurred in all patients after treatment. In the preschool children group, 3 cases (3.5%) developed hypopigmentation and 1 case (1.2%) developed hyperpigmentation, with an overall incidence of adverse reactions of 4.7%. Hypopigmentation was observed in 7 cases (9.6%) and hyperpigmentation in 3 cases (4.1%) in the school-age children group, with an overall incidence of adverse reactions of 13.7%. The chi-square test for the incidence of adverse reactions in the two groups showed a statistically significant P<0.05, indicating that the incidence of adverse reactions in the preschool children group was lower than that in the school-age children group.
Table 2 Significant Efficacy Rates and Average Number of Treatments for Nevus of Ota in Children
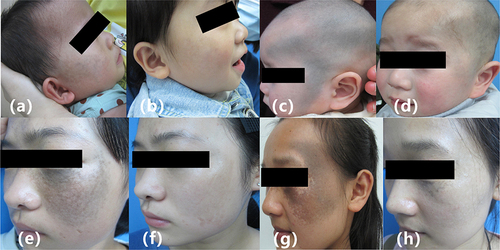
Figure 1 Nevus of Ota in Children Before and After Treatment. (a) 7-month-old child with type I nevus of Ota, before treatment. (b) 7-month-old child with type I nevus of Ota after 2 treatments. (c) 6-month-old child with type III nevus of Ota, before treatment. (d) 6-month-old child with type III nevus of Ota after 3 treatments. (e) 12-years-old child with typeIInevus of Ota, before treatment. (f) 12-years-old child with typeIInevus of Ota after 4 treatments. (g) 14-years-old child with type III nevus of Ota, before treatment. (h) 14-years-old child with type III nevus of Ota after 4 treatments.
The mean CDI score for the pre-treatment school-age children group was 17.3, and 18 children scored ≥19 (24.6%). The mean CDI score for the post-treatment school-age children group was 13.6, and 11 children scored ≥19 (15.1%). In the preschool children group, who reached the age of 7 years after three years of treatment, there were 31 children with a mean CDI score of 10.8, and 3 children (9.7%) scored ≥19 points ().
Table 3 CDI Scores of Children with Nevus of Ota Before and After Treatment
The mean CDI scores and the percentage of depressed individuals in the school-age children group were significantly lower after treatment than before treatment (p<0.05). It suggests that the treatment of children with nevus of Ota can improve the mental health status of children at school age. The mean CDI scores and the percentage of depressed individuals after treatment in the preschool children group were significantly lower than after treatment in the school-age group. This suggests that treating nevus of Ota in the preschool period can better improve the mental health status of children with nevus of Ota.
Discussion
Nevus of Ota is a benign dermal pigmentation disorder. Its pathogenesis is still unclear, and most scholars believe that it may be caused by abnormal apoptosis of melanocytes during embryonic development, which prevents melanocytes from migrating from the dermis to the epidermis, and Results in the production of activated melanin by melanocytes in the dermis.Citation11 In addition, sex hormones and ultraviolet rays are also important factors affecting the development of nevus of Ota. Nevus of Ota can seriously affect the patient’s appearance and may cause psychological disorders. Therefore, timely treatment is needed. Traditional treatments such as CO2 laser, chemical peeling, skin dermabrasion, skin grafting, freezing, etc. often cause scarring, pigmentation abnormalities and other adverse reactions, and are generally not used in clinical treatment. In 1994, Watanabe successfully treated 35 patients with nevus of Ota with Q-switched ruby laser based on the theory of selective photothermal effect.Citation4 As the Q-switched ruby laser can selectively destroy the pigment tissue particles of nevus of Ota and break them up, and then part of the broken pigment particles are removed through the shedding of scabs at the lesion site, and the other part is phagocytosed and removed by phagocytes of the body, with little damage to the surrounding normal tissues.Citation12 Therefore, these nanosecond lasers have the advantages of higher efficiency and less adverse reactions, and have become the treatment of choice for patients with nevus of Ota. Among them, Q-switched ruby laser is the classic method for treating nevus of Ota.Citation13 However, the effectiveness of clinical laser treatment for nevus of Ota is affected by many factors. For example, the starting age of the treatment, the number of treatments, the choice of energy, etc. will affect the efficacy of laser treatment of nevus of Ota. In the present study there was no significant difference between the apparent efficiency of the preschool children group and the school-age children group. However, the average number of treatments in the preschool children group was significantly smaller than that in the school-age children group. This suggests that early treatment can reduce the number of treatments when the same treatment effect is achieved. This may be due to the fact that nevus of Ota becomes progressively darker in colour as we grow older due to stimuli such as ultraviolet rays and sex hormones during life, and the efficacy of blue-green nevus of Ota, which has a darker rash, is usually not as good as that of brown nevus of Ota.Citation14 Therefore, treating nevus of Ota early before it becomes darker in colour may result in better outcomes. Another reason may be related to the histological depth of nevus of Ota. The histological depth of nevus of Ota was shallower in the preschool children group than in the school-age children group,Citation15 so the average number of treatments was lower in the preschool children group than in the school-age children group. In the current study, apart from transient adverse reactions such as local erythema, oedema and crusting, the most common adverse reactions were mainly hyperpigmentation and hypopigmentation, which is consistent with previous reports.Citation16 The incidence of adverse reactions was higher in the school-age children group than in the preschool children group. The possible reason for this is that the average number of treatments in the school-age children group was higher than that in the preschool children group. It has been suggested that the number of Q-switched laser treatments may be a risk factor for the occurrence of adverse reactions.Citation17 Early treatment may therefore not only reduce the number of treatments but also the risk of adverse effects. In addition, the energy setting of the laser is also very important, and choosing the right energy can effectively reduce the occurrence of pigmentation abnormalities and adverse reactions such as scars.Citation18 The theoretically optimal capacity is the lowest energy at which a therapeutic effect can be achieved, and the clinical endpoint of treatment is demonstrated by the grey cream response. In clinical practice, the appropriate energy should be selected according to the patient’s age, skin type and so on. Another important factor that affects the efficacy of treatment is the treatment interval. The Q-switched ruby laser destroys melanocytes in the dermis when treating nevus of Ota, and then macrophages will phagocytose and remove melanosomes and cellular debris.Citation18 If the interval between treatments is too short, the macrophages, which are still cleaning up, will be attacked as a target group because they have swallowed a large number of melanosomes, which will lead to the destruction of the macrophages themselves, so the interval between laser treatments needs to be 3–6 months. Therefore, the whole treatment cycle of nevus of Ota often takes 1 to 2 years, or even longer. Because nevus of Ota can seriously affect aesthetics, this may affect the patient’s social life or cause psychological disorders.Citation19 Therefore, some scholars believe that the treatment should be completed before school age, but the treatment cycle of nevus of Ota is long, so the treatment should be started as early as possible. However, there is still a need to consider the risks and benefits of having a child receive laser.Citation20 The psychological impact of nevus of Ota on paediatric patients has been mentioned in many articles, but most of them are theoretical speculations without concrete data. In this study, we used the CDI scale to quantify the mental health status of children with nevus of Ota. We found that school-aged patients with nevus of Ota were able to reduce their depression scores after receiving treatment. In addition, treatment at preschool age reduced depression scores compared to children treated at school age. Therefore, nevus of Ota in children should be treated early. Regarding the choice of anaesthesia. The guardians of the patients in this study were concerned that multiple general anaesthetics for the treatment process could adversely affect the development of the children’s brains, so local anaesthesia was chosen. However, there is also a view that the treatment process of local anaesthesia may cause psychological trauma due to fear and pain. We therefore surveyed 31 children in the preschool group who participated in the CDI Assessment. Twenty-two children reported having memories of the treatment sessions. Seventeen of these 22 children reported vague memories, and five reported definite pain memories. Maybe the trauma caused by the fear of pain during treatment is not as bad as we think it is. Early treatment brings perhaps even greater benefits. However, local anaesthesia requires a skilled team of laser operators. In addition, we usually allow parents to be present during the treatment. We believe that having a familiar face in an unfamiliar environment has a positive effect on the child.Citation21
Limitations
The limitations of this study are that it was a retrospective study, some variables could not be controlled for, and the sample size was not very large. A larger prospective study should be conducted. In addition, the CDI is only one of the scales used to assess children’s mental health status and cannot fully represent the mental health status of children. The CDI scale is applicable to children and adolescents from 7 to 17, so CDI could not be collected from patients before the age of 7. Moreover, the assessment of children’s CDI scale is also affected by other aspects, such as children’s families, academic pressure, etc.
Conclusions
Q-switched ruby laser is safe and effective in treating nevus of Ota in children. Early treatment can reduce the number of treatments and the incidence of adverse reactions. In addition, early treatment can reduce children’s depression, which is beneficial to mental health.
Ethics Statement
The patient’s guardian had signed an informed consent form at the start of the treatment allowing images and data from the treatment period to be used for medical research. And the use of images in papers is allowed and publication is permitted as long as privacy is protected.
Disclosure
The authors report no conflicts of interest in this work.
References
- Leung A, Kao C, Cho H, Siu M, Choi M, Sauve R. Scleral melanocytosis and oculodermal melanocytosis (nevus of Ota) in Chinese children. J Pediatr. 2000;137(4):581–584. doi:10.1067/mpd.2000.108208
- Hidano A, Kajima H, Ikeda S, Mizutani H, Miyasato H, Niimura M. Natural history of nevus of Ota. Arch Dermatol. 1967;95(2):187–195. doi:10.1001/archderm.1967.01600320043006
- Chan H, King W, Chan E, et al. In vivo trial comparing patients’ tolerance of Q-switched Alexandrite (QS Alex) and Q-switched neodymium: yttrium-aluminum-garnet (QS Nd:YAG) lasers in the treatment of nevus of Ota. Lasers Surg Med. 1999;24(1):24–28. doi:10.1002/(SICI)1096-9101(1999)24:1<24::AID-LSM5>3.0.CO;2-Z
- Watanabe S, Takahashi H. Treatment of nevus of Ota with the Q-switched ruby laser. New Engl J Med. 1994;331(26):1745–1750. doi:10.1056/NEJM199412293312604
- Zheng H, Xu A, Qiao G, Sun X, Deng J, Zhang Y. Results and Follow-Up of a Sequential Q-Switched Laser Therapy for Nevus of Ota in Infants. Clin Cosmet Invest Dermatol. 2024;17:339–347. doi:10.2147/CCID.S444410
- Yang C, Shih I, Huang Y, Hu S. Efficacy and safety of picosecond 755-nm alexandrite laser for treatment of nevus of Ota in Taiwanese children: a retrospective study. Lasers Surg Med. 2022;54(3):355–365. doi:10.1002/lsm.23488
- Belkin D, Jeon H, Weiss E, Brauer J, Geronemus R. Successful and safe use of Q-switched lasers in the treatment of nevus of Ota in children with phototypes IV-VI. Lasers Surg Med. 2018;50(1):56–60. doi:10.1002/lsm.22757
- Achavanuntakul P, Manuskiatti W, Wanitphakdeedecha R, Jantarakolica T. Early Treatment Initiation Improves Outcomes in Nevus of Ota: a 10-Year Retrospective Study. Am J Clin Dermatol. 2022;23(1):105–114. doi:10.1007/s40257-021-00637-0
- Andropoulos D, Greene M. Anesthesia and Developing Brains - Implications of the FDA Warning. New Engl J Med. 2017;376(10):905–907. doi:10.1056/NEJMp1700196
- Smucker M, Craighead W, Craighead L, Green B. Normative and reliability data for the Children’s Depression Inventory. J Abnorm Child Psychol. 1986;14(1):25–39. doi:10.1007/BF00917219
- Chang C, Kou C. Comparing the effectiveness of Q-switched Ruby laser treatment with that of Q-switched Nd:YAG laser for oculodermal melanosis (Nevus of Ota). J Plast Reconstruct Aesthetic Surg. 2011;64(3):339–345. doi:10.1016/j.bjps.2010.05.036
- Kono T, Chan H, Erçöçen A, et al. Use of Q-switched ruby laser in the treatment of nevus of ota in different age groups. Lasers Surg Med. 2003;32(5):391–395. doi:10.1002/lsm.10171
- Williams N, Gurnani P, Long J, et al. Comparing the efficacy and safety of Q-switched and picosecond lasers in the treatment of nevus of Ota: a systematic review and meta-analysis. Lasers Med Sci. 2021;36(4):723–733. doi:10.1007/s10103-020-03125-9
- Ueda S, Isoda M, Imayama S. Response of naevus of Ota to Q-switched ruby laser treatment according to lesion colour. Br J Dermatol. 2000;142(1):77–83. doi:10.1046/j.1365-2133.2000.03264.x
- K W, L E, C GS. Treatment of Ota’s nevus by Q-switched alexandrite laser: therapeutic outcome in relation to clinical and histopathological findings. Eur J Dermatol. 1999;9(8):639–643.
- Kono T, Nozaki M, Chan H, Mikashima Y. A retrospective study looking at the long-term complications of Q-switched ruby laser in the treatment of nevus of Ota. Lasers Surg Med. 2001;29(2):156–159. doi:10.1002/lsm.1103
- Chan H, Leung R, Ying S, et al. A retrospective analysis of complications in the treatment of nevus of Ota with the Q-switched alexandrite and Q-switched Nd:YAG lasers. Dermatologic Surg. 2000;26(11):1000–1006.
- Wanner M, Sakamoto F, Avram M, Anderson R. Immediate skin responses to laser and light treatments: warning endpoints: how to avoid side effects. J Am Acad Dermatol. 2016;74(5):807–819; quiz 819–820. doi:10.1016/j.jaad.2015.06.025
- Strauss R, Resnick S. Pulsed dye laser therapy for port-wine stains in children: psychosocial and ethical issues. J Pediatr. 1993;122(4):505–510. doi:10.1016/S0022-3476(05)83527-9
- Shahriari M, Makkar H, Finch J. Laser therapy in dermatology: kids are not just little people. Clin Dermatol. 2015;33(6):681–686. doi:10.1016/j.clindermatol.2015.09.010
- Alegre-Sánchez A, Pérez-García B, Boixeda P. Pulsed-dye laser treatment of port-wine stains in children: useful tips to avoid general anesthesia. Pediatr Dermatol. 2017;34(5):619–621. doi:10.1111/pde.13207
