Abstract
Erosive pustular dermatosis is a rare noninfectious disease of the scalp or legs. Clinical findings are nonspecific, with crusts, atrophy, and pustules. A later complication of erosive pustular dermatosis is secondary cicatrical alopecia. The list of possible differential diagnoses is long, and includes infectious, inflammatory, and neoplastic dermatoses. Treatment is challenging. Topical drug therapy may improve the condition, but rarely results in a complete resolution. Surgery has been linked to exacerbation in some patients. In our hands, it achieved complete remission in male patients.
Introduction
Erosive pustular dermatosis (EPD) is a noninfectious inflammatory disorder that was described first in 1979 by Pye et al.Citation1 The disorder occurs in two types: on the scalp and on the leg. We will review available data on the disease. Here, we present an update on this unusual dermatosis, with a special focus on treatment.
Epidemiology
EPD is a rarely reported entity, but the condition might be underrecognized, and its true frequency might be higher than previously thought. About 100 cases have been reported in the literature so far.Citation2 Patton et al challenged the established concept of extreme rarity by finding eleven cases in a small region over a period of 3 years. They suggested that a focused search for the diagnosis and reconsideration of its main features, including the commonly seen lack of pustules, could lead to an increased rate of diagnosing EPD.Citation3
EPD most commonly develops in the elderly. Rare cases of EPD in younger patients have also been reported.Citation3 An infantile EPD in association with Klippel–Feil syndrome was observed in a 6-month old baby-girl.Citation4 Although initially considered a female disease, EPD is encountered in both sexes, with a female predominance of approximately 2:1.Citation1,Citation3 Specific geographical or racial distribution has not been demonstrated.
Clinical presentation
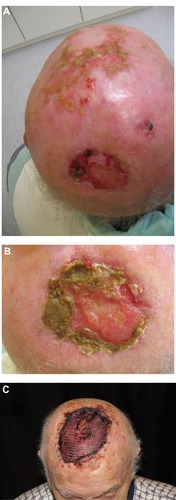
The typical clinical picture of EPD is a mixture of superficial erosions with crusts and pustules on atrophic skin ( and ). The number of pustules can vary remarkably, and sometimes they are absent. They often developed over several months or even years without improvement. Secondarily, cicatrical alopecia may develop. The lesions are not painful. Pruritus is uncommon. The course is progressive. No spontaneous remissions occur.Citation1,Citation3
Figure 1 (A–C) Chronic eosinophilic dermatosis of the scalp in a 76 year-old male. (A) Overview. (B) Detail of crusted and erosive lesion with overgranulation. No signs of reepithelialization. (C) Excision and split-skin transplant. Ten days after transplantation, a stable transplant without recurrence is seen.
On the leg, usually single lesions are found closely resembling chronic vegetating pyoderma. Scarring is a lesser problem than on the scalp. Edema and varicose veins are associated instead of skin atrophy.
Histopathology
Histopathology is uncharacteristic and not very helpful in confirming the diagnosis. However, a biopsy is important to exclude some of the differential diagnoses that may need different treatment or run another course. Histopathology shows subcorneal pustules, epidermal hypertrophy, or atrophy and erosions. The pustules, when present, are not of the follicular type, an important difference to bacterial folliculitis. These findings can be accompanied by a polymorphous dermal inflammatory infiltrate composed of neutrophil leukocytes, lymphocytes, and some plasma cells. In the neighborhood of erosions and ulcerations, a minimal leukocytoclastic vasculitis might be present. Microbial and mycological investigations remain negative.Citation1
Differential diagnosis ()
Tinea capitis or kerion celsi may resemble EPD, and mycological investigations are necessary in diagnostics.Citation5 Other scalp disorders that need consideration include Gram-negative folliculitis, folliculitis decalvans, folliculitis et perifolliculitis abscedens et suffodiens, chronic vegetating pyoderma, superficial pyoderma gangrenosum, and others.Citation6
Table 1 Differential diagnosis of erosive pustular dermatitis of the scalp (EPDS)
A Tzanck smear test seems to be helpful in differential diagnoses to autoimmune vesiculobullous diseases like pemphigus.Citation7 Other types of cicatrical alopecia caused by lichen planopilaris or lupus erythematosus need to be differentiated. Histological examination is most helpful.Citation3
In scalp EPD, field cancerization and squamous cell carcinoma are differential diagnoses ().Citation8 A number of elderly EPD patients had previously squamous cell carcinomas of the skin.Citation9
Figure 2 A 57-year-old patient with chronic actinic damage, multiple actinic keratoses and a T2 squamous cell carcinoma on the scalp. Field cancerization is an important differential diagnosis to erosive pustular dermatosis of the scalp.

Targeted therapies of cancer may induce EPD-like disease. Toda et al reported EPD-like lesions on the scalp during anti-epidermal growth-factor receptor gefitinib therapy. In their paper, a total of 11 cases were discussed.Citation10
Pathogenesis
The etiology and exact pathogenesis of EPD remain unclear, which impedes proper categorization. Some authors consider EPD a disease in the spectrum of inflammatory dermatoses, whilst others claim immunological dysfunction as the main pathogenetic mechanism. Underlying factors include trauma and tissue damage, chronic inflammation, and neutrophilic dysfunction.Citation3
Leg lesions most commonly develop in patients with venous stasis and edematous skin changes.Citation11 EPD on the legs has also been reported in patients with paraplegia or quadriplegia.Citation3,Citation12
Trauma and tissue damage play a triggering role in EPD.Citation13 Preceding herpes zoster,Citation14 cochlear implant positioning,Citation15 and iatrogenic injury caused by cryotherapy, topical chemotherapy, excisional surgery, imiquimod,Citation16 grafting after surgery of nonmelanoma skin cancer,Citation17 topical methyl aminolevulinate photodynamic therapy,Citation18 and carbon dioxide laser therapyCitation19 have all been reported in association with EPD.
Chronic ongoing inflammation is a feature of EPD. Neutrophils are commonly present, but do not predominate as in the specific neutrophilic dermatoses.Citation3,Citation20 Autoimmune diseases have been reported in association with EPD, although a direct pathogenetic link is difficult to establish.Citation3,Citation21,Citation22 Positive antinuclear antibody testing was found in one study in four of eleven patients.Citation3
Delayed wound healing is characteristic for EPD. The lack of hair bulge stem cells, estrogen deprivation, poor restorative capacity of aged keratinocytes, and chronic inflammation may be implicated in delayed healing.Citation3,Citation23
Treatment ()
EPD is a chronic condition that requires long-term management. Multiple therapeutic modalities have been tried, with high-potency topical corticosteroids being the mainstay of treatment. Topical and systemic antibiotics have been tried, with little or no response.Citation1,Citation18
Table 2 Therapeutic opportunities in erosive pustular dermatosis of scalp and leg
The rarity of EPD and the scarce literature data impede the establishment of a treatment algorithm for the disease. Based on the available knowledge, it could currently be recommended that topical agents, corticosteroids, or tacrolimus be tried first. All other reported modalities could be used as second-line treatments in recalcitrant cases.
Medical drug therapy
Corticosteroids
High-potency topical corticosteroids have been used in most reported cases, with considerable efficacy and relative safety.Citation1,Citation22 The main disadvantage of this treatment is the possibility for skin atrophy, which should be considered in long-term application. Additionally, relapse after initial improvement has been reported after discontinuation of topical steroids.Citation1
Guarneri and Vaccaro used oral steroids in tapering doses for 12 weeks to achieve complete resolution with residual scarring alopecia in a patient with photodynamic therapy-induced EPD.Citation18 The side effects of systemic steroids and the available alternatives, however, do not justify this treatment approach.
Topical tacrolimus
Topical tacrolimus 0.1% ointment has emerged as an alternative to topical steroids with reported similar efficacy.Citation14,Citation15,Citation24,Citation25 Applied once or twice daily, it is effective not only for scalp but also for leg lesions.Citation26 Improvement is seen after 1–2 weeks of treatment, but complete resolution may take up to 16 weeks, according to literature reports.
Topical tacrolimus could be used either as monotherapy, in combination with topical steroids, or as a follow-up treatment after an initial course of topical steroids. Long-term supportive treatment with tacrolimus twice weekly for 1 year prevented a relapse in a patient with EPD on the leg.Citation26
Tacrolimus has an advantage over topical corticosteroids, since it does not cause skin atrophy. Furthermore, it has been reported to reverse EPD atrophy to a certain extent.Citation24
Dapsone
Dapsone, an anti-inflammatory agent, has been tried in two patients, with disappointing results.Citation1,Citation2 Despite its antineutrophilic action, topical concentration after systemic administration might not reach therapeutic levels.Citation2
Topical dapsone 5% gel, on the other hand, has been used in four patients, with total clearance of the lesions and a relatively long period without posttreatment recurrence.Citation2 One patient was treatment-naive, but the other three failed to respond to previous treatment with corticosteroids, tacrolimus, antibiotics, ultraviolet therapy, and topical salicylic acid. Improvement was seen within 2 weeks to 2 months from therapy initiation, and complete resolution was observed for 1–4 months. No side effects were reported.
Topical calcipotriol
Boffa used calcipotriol cream 0.005% for a patient with scalp EPD with alopecia and resulted in a remarkable improvement after 8 weeks of treatment and partial hair regrowth after 12 weeks.Citation27
Acitretin
Acitretin may be of some benefit in individual patients, but this drug needs regular laboratory monitoring.Citation28 In conclusion, medical drug therapy for EPD shows a mixed response, with a need for long-term treatment – especially with topical drugs – and higher risk of relapses. Therefore, a maintenance treatment with topical calcineurin inhibitors has been recommended.Citation29 On the other hand, stable complete resolutions have rarely been observed by conservative treatment.
Photodynamic therapy
Marked improvement was observed in a patient treated with photodynamic therapy,Citation30 though there have been reports that it could itself trigger the development of EPD.Citation18,Citation31 Meyer et al used methyl 5-amino levulinic acid cream with 630 nm irradiation for a total of two treatments, 1 week apart, leading to very good results at week 12.Citation30 Although this might be considered as a third-line therapeutic option, photodynamic therapy should be used with caution in view of the conflicting reports.
Surgery
Since EPD of the scalp shows some mimicry of squamous cell carcinoma and field cancerization, surgery has been used occasionally. Deep excision and split-skin grafting leads to rapid healing. This should not be a first-line therapy of course. In cases of widespread and recalcitrant cases of bald elderly males, however, we observed complete remissions with an acceptable aesthetic outcome in three males aged 76–86 years. During follow-up of 12–36 months, no relapse occurred. Like in other chronic wounds, the removal of chronic granulation tissue and biofilm seems to be helpful in final wound closure.Citation32
In contrast to our experience with scalp EPD, Eusen et al observed a recurrence of leg EPD after skin grafting.Citation33 In their case, no complete excision of underlying skin had been performed. More data are needed to assess the possible role of surgery in EPD.
Outlook
A potential crucial step seems to interrupt the recruitment of neutrophils in the affected skin. Recently, new compounds have been identified that interact with neutrophil recruitment, like p38 mitogen-activated protein kinase inhibitor SB203580,Citation34 Ac2–26 – an annexin A1/lipocortin 1 mimetic peptideCitation35 – or antiadhesive proteinsCitation36 may expand current opportunities to control neutrophilic recruitment in EPD. However, a better understanding of the disease is desperately needed.
Disclosure
The authors report no conflicts of interest in this work.
References
- PyeRJPeacheyRDBurtonJLErosive pustular dermatosis of the scalpBr J Dermatol19791005559566444428
- BroussardKCBergerTGRosenblumMMuraseJEErosive pustular dermatosis of the scalp: a review with a focus on dapsone therapyJ Am Acad Dermatol201266468068622074698
- PattonDLynchPJFungMAFazelNChronic atrophic erosive dermatosis of the scalp and extremities: a recharacterization of erosive pustular dermatosisJ Am Acad Dermatol200757342142717532096
- ShimadaRMasuTHanamizuHAibaSOkuyamaRInfantile erosive pustular dermatosis of the scalp associated with Klippel-Feil syndromeActa Derm Venereol201090220020120169313
- ChiaCDahlMVKerion mimicking erosive pustular dermatosis in elderly patientsCutis2013912737723513554
- Lugović-MihićLBarisićFBulatVDifferential diagnosis of the scalp hair folliculitisActa Clin Croat201150339540222384776
- DurduMBabaMSeçkinDThe value of Tzanck smear test in diagnosis of erosive, vesicular, bullous, and pustular skin lesionsJ Am Acad Dermatol200859695896418929431
- TsatsouFTrakatelliMPatsatsiAKalokasidisKSotiriadisDExtrinsic aging: UV-mediated skin carcinogenesisDermatoendocrinol20124328529723467430
- WantzMPerceauGGoeldelALGrangeFBernardPErosive pustular dermatosis of the legs: retrospective study of 16 casesAnn Dermatol Venereol201113829399 French21333818
- TodaNFujimotoNKatoTErosive pustular dermatosis of the scalp-like eruption due to gefitinib: case report and review of the literature of alopecia associated with EGFR inhibitorsDermatology20122251182122922680
- CotterillJALaniganSWErosive pustular dermatosis of the leg – a definitionBr J Dermatol199012345482095189
- BullRHMortimerPSErosive pustular dermatosis of the legBr J Dermatol199513222792827888368
- GrattanCEPeacheyRDBoonAEvidence for a role of local trauma in the pathogenesis of erosive pustular dermatosis of the scalpClin Exp Dermatol19881317103061689
- KimKRLeeJYKimMKYoonTYErosive pustular dermatosis of the scalp following herpes zoster: successful treatment with topical tacrolimusAnn Dermatol201022223223420548924
- MarzanoAVGhislanzoniMZaghisASpinelliDCrostiCLocalized erosive pustular dermatosis of the scalp at the site of a cochlear implant: successful treatment with topical tacrolimusClin Exp Dermatol2009345157159
- CorradinMTForcioneMGiulioniEFiorentinoRFerrazziAAlaibacMErosive pustular dermatosis of the scalp induced by imiquimodCase Rep Dermatol Med2012201282874923259090
- MehmiMAbdullahAErosive pustular dermatosis of the scalp occurring after partial thickness skin graft for squamous cell carcinomaBr J Plast Surg200457880680715544786
- GuarneriCVaccaroMErosive pustular dermatosis of the scalp following topical methylaminolaevulinate photodynamic therapyJ Am Acad Dermatol200960352152219231656
- Tavares-BelloRErosive pustular dermatosis of the scalp. A chronic recalcitrant dermatosis developed upon CO2 laser treatmentDermatology20092191717219339769
- ErdmannMKiesewetterFSchulerGSchultzEErosive pustular dermatosis of the leg in a patient with ankylosing spondylitis: neutrophilic dysfunction as a common etiological factor?Int J Dermatol200948551351519416383
- YamamotoTFuruseYErosive pustular dermatosis of the scalp in association with rheumatoid arthritisInt J Dermatol19953421487737780
- Van ExelCEEnglishJC3rdErosive pustular dermatosis of the scalp and nonscalpJ Am Acad Dermatol20075721114
- ArcherDFPostmenopausal skin and estrogenGynecol Endocrinol201228Suppl 22622849791
- CenkowskiMJSilverSTopical tacrolimus in the treatment of erosive pustular dermatosis of the scalpJ Cutan Med Surg200711622222518042336
- TardioNBDalyTJErosive pustular dermatosis and associated alopecia successfully treated with topical tacrolimusJ Am Acad Dermatol20116539394
- Dall’OlioERosinaPGirolomoniGErosive pustular dermatosis of the leg: long-term control with topical tacrolimusAustralas J Dermatol2011521e15e1721332681
- BoffaMJErosive pustular dermatosis of the scalp successfully treated with calcipotriol creamBr J Dermatol2003148359359512653759
- DarwichEMuñoz-SantosCMascaróJMJrErosive pustular dermatosis of the scalp responding to acitretinArch Dermatol2011147225225321339464
- Vano-GalvanSAntonioMCPedroJErosive pustular dermatosis of the scalpJ Pak Med Assoc201262550150222755320
- MeyerTLopez-NavarroNHerrera-AcostaEJoseAHerreraEErosive pustular dermatosis of the scalp: a successful treatment with photodynamic therapyPhotodermatol Photoimmunol Photomed2010261444520070839
- LópezVLópezIRamosVRicartJMErosive pustular dermatosis of the scalp after photodynamic therapyDermatol Online J20121891323031380
- NusbaumAGGilJRippyMKEffective method to remove wound bacteria:comparison of various debridement modalities in an in vivo porcine modelJ Surg Res2012176270170722440935
- EusenMFleuretCKupferIRecurrence of pustular erosive dermatosis of the leg after a skin graftAnn Dermatol Venereol20121393224225 French22401691
- XuNHossainMLiuLPharmacological inhibition of p38 mitogen-activated protein kinases affects KC/CXCL1-induced intraluminal crawling, transendothelial migration, and chemotaxis of neutrophils in vivoMediators Inflamm2013201329056523533303
- KamalyNFredmanGSubramanianMDevelopment and in vivo efficacy of targeted polymeric inflammation-resolving nanoparticlesProc Natl Acad Sci USA2013110166506651123533277
- PliyevBKAnti-adhesive proteins and resolution of neutrophil-mediated inflammationImmunobiology201321881085109223566767