Abstract
Introduction
Lichen sclerosus is a chronic inflammatory dermatological condition of unknown etiology, primarily impacting the genital epidermis in individuals of all genders, with a higher prevalence observed among postmenopausal women and prepubescent girls. Additionally, extragenital manifestations occur in approximately 20% of the patients diagnosed with genital lichen sclerosus. Notably, folliculocentric extragenital lichen sclerosus is rare and unusual, with only limited instances documented in existing literature.
Case Description
We report a 33 years old lady presented with multiple asymptomatic lesions on the dorsal feet for 1 year and similar lesions on the left hand for 4 months. On examination: folliculocentric, shiny, atrophic papules coalescing into reticulated plaques over the dorsum of both feet and few shiny, flat-topped, pink papules over the dorsum of the left hand. A skin biopsy was performed and confirmed the diagnosis of extragenital lichen sclerosus.
Conclusion
Acral folliculocentric extragenital lichen sclerosus is an unusual and rare clinical variant. Clinicopathologic correlation is necessary to establish the correct diagnosis.
Contribution to the Literature
Herein, we present an unusual presentation of extragenital lichen sclerosus, and we highlight the importance of considering it in the differential diagnosis of guttate acral skin lesions. We also review and summarize relevant cases from the literature in hope to aid physicians, especially dermatologists, to consider and swiftly reach the diagnosis and offer appropriate management. We also hope to bring about new insights and broaden future research efforts regarding lichen sclerosus especially and atrophic skin disease in general.
Introduction
Lichen sclerosus is a chronic inflammatory dermatological condition of unknown etiology, primarily impacting the genital epidermis in individuals of all genders, with a higher prevalence observed among postmenopausal women and prepubescent girls. Extragenital manifestations are documented in approximately 6% to 20% of LS cases, with isolated occurrences accounting for only 6%.Citation1 Furthermore, the folliculocentric subtype of extragenital LS is rare and uncommon, with only four reported instances documented in literature. We present the case of a 33-year-old female with isolated acral folliculocentric extragenital lichen sclerosus.
Case Presentation
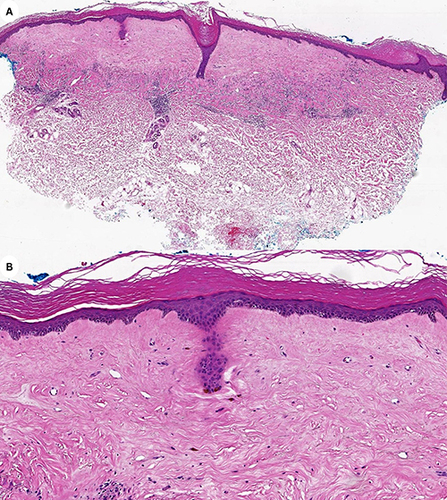
A 33 years old lady presented to the outpatient clinic with a complaint of lesions over the dorsal aspect of the foot for 1 year and dorsum of the left hand for 4 months. The lesions were asymptomatic and started to increase in number over the past year. There was no history of genital pruritus or lesions in other body sites. Past medical history is positive for hypothyroidism, Diabetes mellitus, dyslipidemia, generalized anxiety disorder and bariatric surgery. Upon examination, there were numerous folliculocentric, shiny, atrophic papules coalescing into reticulated plaques over the dorsum of both feet (). And few shiny, flat-topped, pink papules over the dorsum of the left hand (). She had never been treated with topical or oral medications regarding her condition. Biopsy from the foot was taken and showed hyperkeratosis, epidermal atrophy and papillary dermal sclerosis consistent with a diagnosis of Lichen sclerosus ( and ). The patient was then prescribed Clobetasol propionate ointment daily and reported signs of significant improvement and disappearance of lesions.
Figure 1 (A) Multiple shiny atrophic folliculocentric reticulated papules and plaques over the dorsum of the foot. (B) Few shiny pink flat topped papules over the dorsum of the hand.
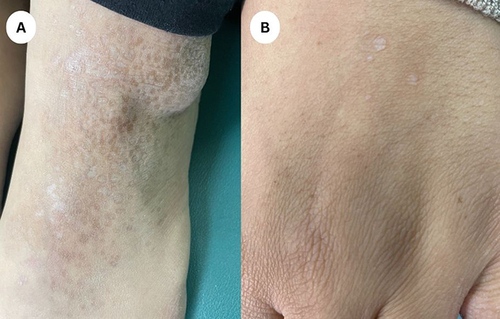
Figure 2 (A) Photomicrograph of lower power of skin punch biopsy shows hyperkeratosis, papillary dermal sclerosis. (B) High power exhibits hyperkeratosis, epidermal atrophy, and sclerosis in papillary dermis.
Discussion
Lichen sclerosus is a chronic inflammatory condition affecting both genders, though it exhibits a higher prevalence in females and demonstrates a bimodal age distribution.Citation1 The precise cause of the disorder remains unidentified; however, it has been associated with various factors such as trauma, infections, autoimmune responses, estrogen deficiency, and certain medications like carbamazepine and imatinib mesylate.Citation1–5 Extragenital manifestations of the disease are primarily observed on the trunk, neck, and shoulders, with acral sites being seldom affected. Previous similar cases of folliculocentric extragenital lichen sclerosus have been documented in the medical literature. These cases are referenced briefly with detailed information presented in ().Citation1,Citation2,Citation6,Citation7 For a thorough review of these cases, please refer to the cited studies.
El Habr et al and Uzuncakmak et al describe the condition in two pediatric patients,Citation1,Citation2 while Mann et al and Lo et al report it in two postmenopausal women.Citation6,Citation7 Mann et al detailed the case of a 71-year-old black woman with pruritic white lesions distributed perifollicularly over the chest, back, elbows, and legs. Lo et al later described a woman in her 60s with a decade-long history of numerous white papules extending from her back to the waist and inframammary area. Additionally, El Habr et al reports a 10-year-old girl with asymptomatic, hypopigmented, atrophic papules on both upper and lower extremities, while Uzuncakmak et al document a 7-year-old girl with a two-year history of asymptomatic white lesions on the trunk, arms, and legs. Clinical features are summarized in (), with previously reported cases depicting a widespread distribution and topology, notably lacking isolated acral involvement. Our patient, a middle-aged woman, presented with lesions confined solely to the dorsum of her hands and feet, clinically appearing as atrophic, shiny, and reticulated papules and plaques. The clinical differential diagnosis encompasses atrophic lichen planus, mycosis fungoides, morphea, anetoderma, and follicular atrophoderma. Given the unusual presentation, a clinicopathologic correlation was imperative for diagnosis. Treatment options for localized disease include topical corticosteroids, topical calcineurin inhibitors, and topical retinoids, whereas generalized disease may necessitate phototherapy, methotrexate, systemic corticosteroids, systemic retinoids, or pulse dye laser therapy.Citation2
Table 1 Summary of Previous Cases of Folliculocentric Extragenital Lichen Sclerosus
Conclusion
We present an unusual presentation of extragenital LS. The age and acral nature of our patient’s disease made the presentation unique and the diagnosis challenging. Folliculocentric variant of extragenital LS should be part of the differential diagnosis of atrophic follicular presentations, and a clinicopathologic correlation is necessary to reach the correct diagnosis.
Declaration of Patient Consent
Written informed consent was obtained from the patient for publication of the details of their medical case and any accompanying images.
Statement of Ethics
Ethical approval is not required for this study in accordance with local or national guidelines.
Disclosure
The authors declare that there are no conflicts of interest.
Data Sharing Statement
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Additional information
Funding
References
- El Habr C, Mannava K, Koch S, et al. Folliculocentric lichen sclerosus et atrophicus in a 10-year-old girl. Am J Dermatopathol. 2017;39(1):59–61. doi:10.1097/DAD.0000000000000661
- Uzuncakmak TK, Akdeniz N, Suslu H, Zemheri E, Karadag AS. Folliculocentric hyperkeratotic lichen sclerosus in a 7-year-old child successfully treated with narrowband ultraviolet B phototherapy. Clin Exp Dermatol. 2018;43(1):91–93. doi:10.1111/ced.13216
- Kirtschig G. Lichen sclerosus—presentation, diagnosis and management. Dtsch Arztebl Int. 2016;113:337–343. doi:10.3238/arztebl.2016.0337
- Pranteda G, Muscianese M, Grimaldi M, et al. Lichen sclerosus et atrophicus induced by carbamazepine: a case report. Int J Immunopathol Pharmacol. 2013;26:791–794. doi:10.1177/039463201302600326
- Skupsky H, Abuav R, High W, Pass C, Goldenberg G. Development of lichen sclerosus et atrophicus while receiving a therapeutic dose of imatinib mesylate for chronic myelogenous leukemia. J Cutan Pathol. 2010;37:877–880. doi:10.1111/j.1600-0560.2009.01398.x
- Mann DJ, Vergilis-Kalner IJ, Wasserman JR, Petronic-Rosic V. Folliculocentric lichen sclerosus et atrophicus. Skinmed. 2010;8(4):242–244.
- Lo Y, Chu C, Chen Y. Scattered hypopigmented, atrophic, and folliculocentric papules on the trunk. JAMA Dermatol. 2018;154(4):469–470. doi:10.1001/jamadermatol.2017.5174
