Abstract
Refining diagnostic criteria has identified key characteristics differentiating rosacea, a chronic skin disorder, from other common cutaneous inflammatory conditions. The current classification system developed by the National Rosacea Society Expert Committee consists of erythematotelangiectatic, papulopustular, phymatous, and ocular subtypes. Each subtype stands as a unique entity among a spectrum, with characteristic symptoms and physical findings, along with an intricate pathophysiology. The main treatment modalities for rosacea include topical, systemic, laser, and light therapies. Topical brimonidine tartrate gel and calcineurin inhibitors are at the forefront of topical therapies, alone or in combination with traditional therapies such as topical metronidazole or azelaic acid and oral tetracyclines or isotretinoin. Vascular laser and intense pulsed light therapies are beneficial for the erythema and telangiectasia, as well as the symptoms (itching, burning, pain, stinging, swelling) of rosacea. Injectable botulinum toxin, topical ivermectin, and microsecond long-pulsed neodymium-yttrium aluminum garnet laser are emerging therapies that may prove to be extremely beneficial in the future. Once a debilitating disorder, rosacea has become a well known and manageable entity in the setting of numerous emerging therapeutic options. Herein, we describe the treatments currently available and give our opinions regarding emerging and combination therapies.
Introduction and epidemiology
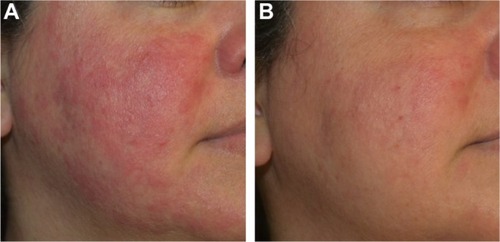
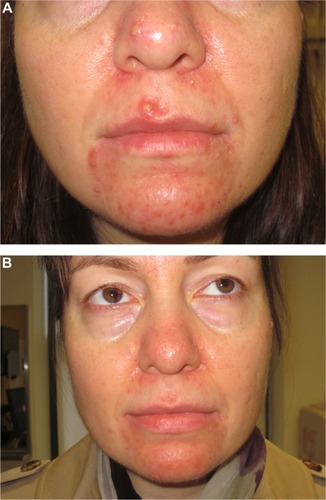
Fascination with rosacea has been historically illustrated in medical art and literature, with imagery found in the Louvre dating back to the 15th century.Citation1 Through the refinement of diagnostic criteria, several key characteristics differentiating rosacea from common skin findings have been identified, particularly central facial erythema and acneiform papules and pustules. Specific sparing of the perioral and periocular regions has emerged as an essential criterion for the diagnosis.Citation2 In 2002, the National Rosacea Society Expert Committee developed a classification system for rosacea in order to standardize subtypes and variants that has since been widely accepted and continues to aid in research and epidemiological studies.Citation3 The committee defined four subtypes based on clinical characteristics: subtype I, or erythematotelangiectatic rosacea (ETR), defined by flushing and persistent central facial erythema (); subtype II, or papulopustular rosacea (PPR), consistent with constant erythema and transient pustules and papules in the central facial distribution (); subtype III, or phymatous rosacea, characterized by thickened skin with irregular contours overlying the ears, cheeks, chin (gnathophyma), forehead (metophyma), and nose (rhinophyma) (); and subtype IV, or ocular rosacea, represented by a watery, burning, dry, itchy, and light sensitive ocular sensation with a bloodshot appearance. An associated cutaneous rosacea may or may not be present (). However, a wide range of overlapping symptoms makes coinciding subtypes a clinical reality.
Figure 1 Erythematotelangiectatic rosacea.

Figure 2 Papulopustular rosacea.

Figure 3 Phymatous rosacea.
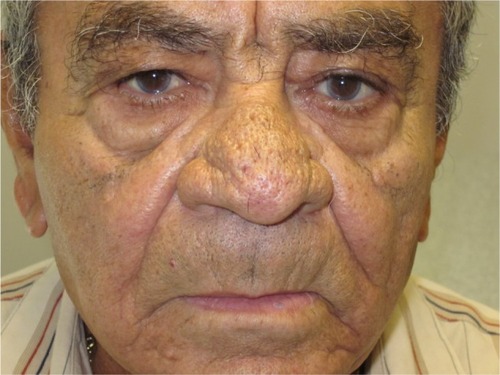
Figure 4 Ocular rosacea.

The prevalence of rosacea in recent years ranges from 1% to 22% depending on the methodology and population sample analyzed.Citation4–Citation6 Reports from general population surveys assess higher sample numbers and may be more reflective of overall prevalence, whereas reports from dermatology clinics represent a more select population and yield smaller prevalence ranges. More recently, large retrospective database studies have yielded prevalence rates ranging from 1.3% to 2.1%.Citation7–Citation12 Such low rates may be misrepresentative since the administrative databases only recorded patients with severe rosacea symptoms, potentially missing a significant percentage of patients with mild disease.
Generally, women are more often affected than men. Subtype I (ETR) is found to be most prevalent, followed by subtype II (PPR), and rhinophyma is seen mostly in men over 40 years of age.Citation13 Ocular rosacea is difficult to diagnose due to wide diagnostic criteria; consequently, incidence rates range from 6% to 72%, with the greatest prevalence reported from ophthalmology clinics. Unlike facial rosacea, ocular rosacea affects both sexes equally.Citation14 The prevalence rates are highly dependent on the classification system, cohort selection, and methodology of collection. Considering these limitations, rosacea as a dermatological entity might be more common than previously suspected.
Natural history and pathophysiological mechanisms underlying rosacea
Despite the depth of current research, the pathophysiology of rosacea remains primarily theoretical and requires further investigation. There is continued debate between rosacea variants representing distinct phenotypes or different stages within one pathological progression. Histologically, dilated lymphatics and blood vessels, as well as perivascular infiltration of CD4+ helper T-cells, macrophages, and mast cells can be readily seen.Citation15 In healthy skin, activation of keratinocyte toll-like receptors (TLRs) by pathogenic cell wall fragments stimulates the cells to coordinate an appropriate defense response, releasing antimicrobial peptides (AMPs) such as cathelicidins and defensins. Originally synthesized as propeptides, these AMPs remain inactive until cleaved by proteases into active fragments. In rosacea, genetic predisposition may precipitate an inappropriate response to different environmental stimuli via TLRs including extremes of temperature, abnormal microbial skin colonization, and ultraviolet light exposure.
The first identified human cathelicidin AMP, LL-37, is released by keratinocytes and cleaved by skin serine proteases (kallikrein 5) into its immunogenic antimicrobial form. Specifically, vitamin D activation by ultraviolet light exposure and endoplasmic reticulum stressors sensed by TLRs on keratinocytes have been shown to induce increased expression of cathelicidin LL-37, triggering molecular cascades ultimately resulting in erythema.Citation16 This partially explains why the face, a highly sun-exposed area, is the main site affected in rosacea.Citation17 LL-37 has been extensively involved in describing the pathogenic inflammatory response, impaired antimicrobial activity, and vascular dysfunction of rosacea.
Another trigger for cutaneous protease activation of cathelicidins is upregulation of TLR-2 in keratinocytes by Demodex folliculorum, a species of commensal saprophytic mite that colonizes pilosebaceous follicles of the skin. D. folliculorum releases an antigen that sensitizes TLR-2 on keratinocytes to induce the pathway of inflammation associated with protease activation of AMPs, including LL-37.Citation18,Citation19 Other microbial agents reportedly associated with rosacea are Bacillus oleronius, Staphylococcus epidermidis, Helicobacter pylori, and Chlamydophila pneumoniae. The exact mechanisms implicating the aforementioned microorganisms in ERT and PPR are yet to be identified or substantiated.Citation20
In addition to erythema, neurocutaneous symptoms, including pain, burning, and stinging, have also been reported in rosacea. Activation of peripheral sensory nerve endings like transient receptor potential channels by heat, cold, alcohol, spicy foods, and exercise releases vasoactive neuropeptides that contribute to neurogenic inflammation.Citation21 As a result, not only do the blood vessels adapt and become hyperpermeable, allowing for increased blood flow and influx of inflammatory cells, but lymphatic vessels also expand to contribute to characteristic flushing, erythema, and edema. Dilation of precapillary arterioles and post-capillary venules allow protein leakage and leukocyte recruitment via upregulation of selectins and cell adhesion molecules.Citation16 Future research will help to clarify the exact pathophysiological mechanisms involved in rosacea. Currently, it is clear that the innate immune and the sensory and autonomic nervous systems are overstimulated with dysregulated interactions, leading to a chronic pathological inflammatory state. Defining the precise molecular interactions and the importance of genetic predisposing factors are puzzle pieces that remain to be solved.
Current and emerging treatments: topical, systemic, laser, and light therapies
No single treatment is completely curative for rosacea. Fortunately, many treatments have been studied and can give relief when used in the right clinical scenario (). Pharmacological agents, when used in combination with medical devices, show better results than either treatment alone and can provide improvements never thought possible in the past (). Since rosacea is a chronic inflammatory condition that waxes and wanes, with many triggers, the goal of treatment should be to subside acute flares with rapid-acting treatments and maintain the results with lifestyle modification and prolonged combination therapy. The avoidance of triggers, particularly ultraviolet light exposure, is critical for long-term improvement and disease control, and should be an essential component of patient education when prescribing at-home skin care and lifestyle adjustments.
Figure 5 Before (A) and after (B) injectable botulinum toxin (Botox®, 10 U, 0.05 mL aliquots every 1–2 cm) intradermally into each cheek in combination with pulsed dye laser (10 mm, 10 msec, 7 J/cm).
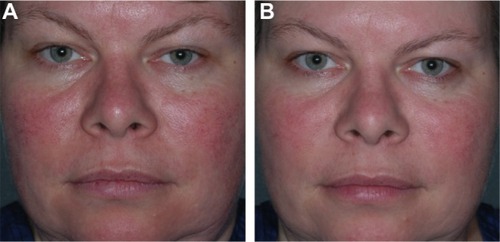
Table 1 Rosacea subtypes and corresponding topical, oral, and alternative treatments
Topical therapies
Brimonidine tartrate gel (Mirvaso®, Galderma Laboratories, Fort Worth, TX, USA), an α-2 adrenergic receptor agonist, is the only approved topical treatment for the persistent facial redness of rosacea and works by reversing skin vasodilation. In a recent year-long study, brimonidine tartrate gel 0.5% applied once daily proved to be both efficacious and safe, regardless of the presence of concomitant therapies.Citation22 The clinician’s erythema assessment, patient’s self-assessment, telangiectasia grading assessment, and inflammatory lesion count were utilized to quantify disease severity.Citation23 Three hours following application, the clinician’s erythema assessment and patient’s self-assessment were reassessed and found to be significantly improved, an effect that was maintained throughout the study. Supporting this result, Jackson et al showed improvement in facial erythema within 30 minutes of initial daily application of brimonidine tartrate in Phase III clinical studies.Citation24 Oxymetazoline, a potent α-1 and partial α-2 receptor agonist, is another efficacious agent for reducing facial erythema, with data primarily limited to case reports, and is now in clinical development for the treatment of ETR. In two adults with refractory erythema and flushing associated with rosacea, oxymetazoline nasal solution 0.05% applied to facial skin demonstrated significant decreased erythema one hour after application that progressed to dramatic improvement within 3 hours and remained throughout the dayCitation25 ().
Figure 6 Before (A) and after (B) oxymetazoline (Afrin®) combined with a topical moisturizing cream (CeraVe®) applied twice daily. Significant improvement in facial erythema was seen after only one day of application.
Some of the more commonly used US Food and Drug Administration (FDA)-approved topical agents for PPR are metronidazole and azelaic acid, both of which are available in a variety of strengths and formulations. The efficacy, safety, and cost-effectiveness of both agents are well demonstrated in a number of well controlled randomized studies.Citation26 A few studies show comparable efficacy of metronidazole and azelaic acid, with one study of azelaic acid gel 15% twice daily yielding a superior reduction in facial erythema versus metronidazole gel 0.75% twice daily after 8 weeks of use.Citation27,Citation28 Long available sodium sulfacetamide 10% + sulfur 5% cleansers and leave-on formulations have also proven to be efficacious for the treatment of inflammatory lesions and facial erythema based on small studies; however, they are not used as frequently, perhaps due to their malodorous sulfur content, irritant potential, and limited published data.Citation29 The mechanisms of action for these topical agents are unknown and the decision to utilize monotherapy or combination regimens depends on the severity of PPR.
There are a number of alternative topical non-FDA-approved therapies for patients with rosacea that is refractory to primary topical treatments. These agents include topical calcineurin inhibitors such as tacrolimus and pimecrolimus, macrolides such as erythromycin, clindamycin, and azithromycin, and others such as retinoids, permethrin, benzoyl peroxide (BP), and BP-clindamycin. Their therapeutic benefits are widely recognized despite the limited evidence in the small number of clinical studies.Citation30 Pimecrolimus cream 1% has been used to treat both PPR and ETR with mixed results, but worthy of a trial in unmanageable cases.Citation31,Citation32 In an open-label randomized study of 49 patients, pimecrolimus 1% cream was as effective as metronidazole 1% cream.Citation33 The senior author (JE) has found considerable benefit in using topical pimecrolimus in combination with oral treatments and/or vascular laser therapy for both ETR and PPR types, and this is his “go-to” therapy for patients with refractory or flared moderate to severe presentations.
Macrolides, such as erythromycin and its analogs, clindamycin and azithromycin, have limited data with regard to reduction of inflammatory lesions and are not recommended as treatments of choice due to potential induction of antibiotic-resistant bacterial strains.Citation30 However, many practicing physicians continue to use these treatments as first-line because they believe them to have intrinsic anti-inflammatory properties that not only improve facial erythema and papules but also the associated symptoms of rosacea.
The antiparasitic properties of permethrin showed efficacy in one study of 63 subjects comparing permethrin cream, topical metronidazole, and placebo.Citation34 Patients were randomly divided into three treatment groups and received either permethrin 5% cream (n=23), metronidazole (n=20), or placebo cream (n=20) for up to 2 months of treatment twice daily. Outcomes of erythema, numbers of papules/pustules/nodules, and D. folliculorum colonization were assessed at baseline and every 15 days. D. folliculorum colonization was reduced by both agents; however, permethrin 5% had a greater effect than metronidazole. Both active treatments reduced erythema and papules, but had no effect on pustules or telangiectasia. Overall, permethrin 5% was found to be a new and powerful tool against dense colonization of D. folliculorum, a proposed key player in the pathogenesis of rosacea.
These results clarify previous equivocal findings of permethrin 5% cream and metronidazole 0.75% gel in a pilot study of six patients who used each therapy on half of the face for up to 10 weeks twice daily.Citation35 More recently, a case study of an immunocompetent patient with refractory rosacea secondary to Demodex dermatitis demonstrated symptom resolution with oral ivermectin and permethrin 5% cream.Citation36
A novel topical agent, ivermectin 1% cream, recently approved by the FDA, was studied in the treatment of PPR in two randomized, double-blind, vehicle-controlled Phase III studies of identical design conducted in the USA (n=683) and Canada (n=688).Citation37 Stein et al compared once-daily ivermectin 1% cream with vehicle for a duration of 12 weeks utilizing the investigator global assessment of disease and inflammatory lesion counts as efficacy parameters. A statistically significant percentage of patients at both trial sites treated with ivermectin 1% compared with vehicle achieved success according to the investigator global assessment, defined as “clear” or “almost clear” skin at week 12. There was also a significantly greater percent reduction in inflammatory lesion counts in the treatment group when compared with control. Adverse events were assessed throughout and were found to be more frequent in the patients treated with vehicle only. The most common complaints were skin burning, pruritus, and dry skin, with no serious adverse events reported. The results of these two 12-week studies identified ivermectin 1% cream as unequivocally potent and safe in treating inflammatory lesions in PPR patients.
Developed from the naturally occurring antiparasitic compound avermectin, ivermectin has both anti-inflammatory and antiparasitic properties that have been utilized orally in the treatment of rosacea-like demodicidosis with topical promethazine and as monotherapy topically for head lice and orally for chronic blepharitis secondary to Demodex.Citation38–Citation40 Selective binding of ivermectin to glutamate-gated chloride channels in invertebrates has been shown to reduce Demodex colonization in both demodicidosis and blepharitis. Ivermectin induces anti-inflammatory effects via nuclear factor-κB pathway inhibition and subsequently decreases the release of inflammatory cytokines. Given that none of the classic rosacea therapies address both the inflammatory and infectious pathogenesis of the disorder, innovative use of ivermectin may prove to be beneficial in the future and warrants further investigation.
Benzoyl peroxide and antibiotic combinations, eg, BP-erythromycin and BP-clindamycin, have long been used for reduction of papulopustular lesions. In a randomized, double-blind, vehicle-controlled trial of BP-clindamycin gel, daily application demonstrated efficacy in 26 patients with moderate to severe rosacea.Citation41 The percentage change in number of papules and pustules from beginning to end of the 12 weeks was reduced by a mean 71.3% in the treatment group compared with 19.3% in the vehicle only group, with a statistically significant difference between the two results. Side effects of itching, burning, and bleaching of hair and clothing were reported in eleven patients. Consequentially, a recent randomized, dose-ranging Phase II study of 1% and 5% BP-encapsulated in silica microcapsules proved to be both highly effective and well tolerated in PPR patients, as the encapsulation added protection for the epidermis from the irritant effects of BP.Citation42
Natural cosmeceutical options serve as an additional branch of the market available to rosacea patients. Natural ingredients reported in the literature that provide hydrating, anti-inflammatory, and antioxidant properties capable of calming the inflammatory manifestations of rosacea include colloidal oatmeal, niacinamide, feverfew, licorice, teas, coffeeberry, aloe vera, chamomile, turmeric, and mushroom extracts.Citation43 Further, a novel topical lotion (Redness Neutralizer®, SkinCeuticals, New York, NY, USA) containing caffeine, zinc gluconate, bisabolol, Eperua falcata bark extract, and palmitoyl tripeptide-8, was used twice daily in a group of 25 patients with PPR who had been previously treated successfully with topical or oral therapy, but were unsatisfied with the remaining background erythema.Citation44 All efficacy categories demonstrated statistically significant improvement between baseline and follow-up at weeks 4 and 8. Although one patient developed burning and increased erythema and withdrew from the study, the remaining 24 patients found the treatment very tolerable without clinical signs of irritation. Overall, 95% of patients were satisfied with the products and the results after 8 weeks of twice-daily use.
In another single-center, open-label study, a group of 30 patients with rosacea of variable severity were treated with 4% Quassia amara extract topical gel for 6 weeks. Reportedly, Q. amara possesses antiparasitic and anti-inflammatory properties that have the capability to decrease the inflammatory response with few complications.Citation45 Efficacy comparable with that of first-line topical treatments like azelaic acid and metronidazole was observed after Q. amara treatment, with superb tolerability. Finally, a formulation of low molecular weight hyaluronic acid sodium salt 0.2% cream (Bionect® Cream, Innocutis Holdings, Charleston, SC, USA) applied twice daily for 8 weeks showed a statistically significant reduction in papules, erythema, burning, stinging, and dryness in a small study.Citation46 Along with excellent tolerability, a reduction in papules, erythema, burning/stinging, and dryness was clearly apparent by week 4 and remained by the final visit at week 8. Notably, erythema was reduced by the greatest amount, with an approximate 50% improvement by week 2. This study demonstrates the importance of skin barrier maintenance and repair in the pathogenesis of rosacea. With a hydrophilic structure, low molecular weight hyaluronic acid penetrates the stratum corneum where it interacts with fibrin and collagen to support remodeling of the extracellular matrix. This mechanism, along with induction of the antimicrobial peptide β-defensin 2 release from keratinocytes, ultimately accelerates re-epithelialization and reduces pain and edema.Citation47
Systemic therapies
Modified-release doxycycline 40 mg once daily (Oracea®, Galderma Laboratories) is the only systemic agent that is approved by the FDA for the treatment of PPR and provides anti-inflammatory effects with subantimicrobial dosing. The formulation allows for immediate release of 30 mg with delayed release of 10 mg once ingested.Citation48 Through inhibition of numerous matrix metalloproteinases, a reduction in the quantity and activity of serine protease kallikrein 5 results in decreased production of cathelicidin LL-37, the same AMP that has been highlighted in the pathogenesis of rosacea.Citation49 Key anti-inflammatory actions of doxycycline in rosacea include: downregulation of cytokines, reducing neutrophil infiltration, inhibition of nitric oxide and its vasodilatory effects, reduction of reactive oxygen species, slowing connective tissue destruction, and inhibition of matrix metalloproteinases.Citation50
Several studies have shown the effectiveness of doxycycline at subantimicrobial doses in the treatment of PPR, both as monotherapy and in conjunction with topical agents.Citation51 In a pivotal randomized, dose-ranging, double-blind trial, similar therapeutic effects were seen in patients with PPR using metronidazole 1% gel and either 40 mg or 100 mg delayed-release doxycycline over 16 weeks.Citation52 Notably, no statistically significant difference was seen between the two treatment groups in any outcome measures; however, adverse events, including nausea, vomiting, diarrhea, and abdominal pain, occurred solely in those treated with doxycycline at an antibiotic dose. Subsequently, a large-scale study demonstrated excellent results in 826 patients with mild to moderately severe rosacea taking daily doxycycline 40 mg monotherapy (30 mg immediate-release and 10 mg delayed-release beads).Citation53,Citation54 Nearly 75% of participants achieved clear or near clear results on the five-point investigator global assessment scale.
Combination therapy has demonstrated more substantial improvements than monotherapy. Oral doxycycline as well as minocycline with azelaic acid or metronidazole has shown substantial improvements in inflammatory lesion counts in multiple studies.Citation55–Citation65
Alternative systemic therapies for PPR and ocular rosacea, which are not FDA-approved, include tetracycline derivatives (doxycycline and minocycline at antimicrobial doses), macrolides (erythromycin, azithromycin, and clarithromycin), metronidazole, and oral isotretinoin. There are several considerations when using systemic treatments, including allergic reactions, drug rash with eosinophilia and systemic symptoms (DRESS syndrome), cutaneous hyperpigmentation, benign intracranial hypertension, autoimmune hepatitis, and drug-induced lupus-like syndrome. More common concerns, and ones to discuss with patients at treatment onset, include gastrointestinal intolerance (antibiotics), metallic taste (macrolides > metronidazole), drug interactions, and photosensitivity (doxycycline > minocycline). Tetracyclines should be avoided in pregnant or lactating women and in children with developing teeth because they can result in permanent staining (dark yellow-gray teeth with a darker horizontal band across the top and bottom rows of teeth), and may also affect bone and tooth growth.
When patients cannot tolerate tetracyclines due to photosensitivity or gastrointestinal adverse effects, such as pill esophagitis, azithromycin has been suggested as an alternative oral treatment option.Citation62 In one case report, a 52-year-old patient with rosacea was successfully treated with azithromycin 500 mg daily after failing numerous regimens, including topical BP, topical metronidazole twice daily, oral metronidazole 500 mg for 2 weeks, oral isotretinoin 10 mg for one month, and oral doxycycline 200 mg for one month.Citation63 With dramatic improvement noticed after 2 weeks of treatment, the patient’s lesions had almost completely disappeared by week 10, with no medication-induced side effects. Another case study in a post-menopausal woman of the same age (52 years) with progressive rosacea symptoms and ocular involvement showed gradual erythema and papulopustule improvement while using combination therapy with tacrolimus 0.1% ointment for 30 days in addition to azithromycin 1,000 mg daily for 45 days, then 500 mg daily for an additional 45 days.Citation64 Historical data show than oral metronidazole 200 mg taken twice daily for 6 weeks resulted in marked improvement in papular and pustular lesions; however, its link to potential side effects such as neuropathy, seizures, and a disulfiram-like reaction have limited further research.Citation65
Oral isotretinoin is typically reserved for severe cases of all rosacea subtypes. This retinoid derivative of vitamin A not only reduces the size of sebaceous glands and subsequently sebum production, but also possesses anti-inflammatory, immunomodulatory, and antineoplastic properties.Citation66 For acne, it is commonly given for a duration of 6 months in daily doses ranging from 0.2 mg/kg to 1.0 mg/kg.Citation13 Participation in the iPledge program, which is mandated by the FDA in order to minimize the risk of teratogenicity from pregnancy while on therapy, as well as numerous drug-induced side effects, such as mucosal dryness, retinoid dermatitis, photosensitivity, and increased blood triglycerides and liver function tests, make prescribing more tedious.
In a large dose-finding, randomized, double-blind trial comparing the use of different systemic isotretinoin dosages with both doxycycline and placebo, the ultimate effective dose of isotretinoin was found to be 0.3 mg/kg for a minimum duration of 3 months.Citation67 Patients with subtypes II (papulopustular) and/or III (phymatous) rosacea were randomly assigned into one of five treatment groups: doxycycline 100 mg daily for 14 days then 50 mg daily (n=143), isotretinoin 0.1 mg/kg (n=109), 0.3 mg/kg (n=142), or 0.5 mg/kg (n=109), or placebo (n=46). These groups were followed until the interim analysis, at which point isotretinoin 0.3 mg/kg stood out as the most efficacious and tolerable dosage. The two other isotretinoin dosage arms were closed, leaving doxycycline and isotretinoin 0.3 mg/kg for the final analysis after 12 weeks of treatment. Overall, isotretinoin 0.3 mg/kg showed statistically significant noninferiority when compared with doxycycline therapy, with investigators documenting complete remission in 24% of patients treated with isotretinoin 0.3 mg/kg compared with 13.6% of patients treated with doxycycline. Notably, more patients in the isotretinoin group reported adverse drug reactions (33%) compared with the doxycycline group (25%); however, these differences did not reach statistical significance. For recalcitrant rosacea with problematic relapses, continuous “microdose” isotretinoin (0.04–0.11 mg/kg daily) in patients without a risk of teratogenesis has shown promise.Citation68,Citation69
For the senior author (JE), oral isotretinoin has been particularly useful in the PPR and phymatous subtypes (). When multiple subtypes coexist in patients with rosacea, it is often beneficial to combine vascular laser treatments and oral isotretinoin. Contrary to historical belief, there is no increased risk of scarring or abnormal wound healing with this combination, and both symptoms of rosacea and central facial erythema and telangiectasia can be reduced dramatically. Many reports of skin sensitivity or fragility while on isotretinoin have been reported, which is a real concern.Citation70,Citation71 Therefore, patient education is important before initiating therapy with regards to facial or body waxing, scratching or picking, and exposure to extremes of temperature (hot tubs, steam rooms, skiing) as these can predispose to easier skin trauma. Atypical keloid formation has also been documented following dermabrasion while on isotretinoin.Citation72,Citation73 However, recent controlled investigations have analyzed skin healing in patients on oral isotretinoin therapy and have debunked previous concerns.
Figure 7 (A) Severe perioral dermatitis (a version of acne-rosacea). (B) Dramatic improvement after initiation of oral isotretinoin.
One comparative retrospective study assessed the effect of invasive acne scar treatment and laser hair removal in a group of 55 patients on a combination of topical therapy and isotretinoin 0.5 mg/kg daily compared with a group of 55 patients on topical monotherapy.Citation74 Notably, there were no differences between the two groups with regard to adverse outcomes, with no development of keloids, atypical scarring, or delayed wound healing following laser therapy. No complications were seen in 35 patients taking isotretinoin 10 mg/kg daily for at least one month prior to a mean of 3.1 sessions with 1,550 nm erbium-doped fiber laser therapy.Citation75
Finally, oral zinc sulfate has been proposed as an additional oral treatment for rosacea. In a randomized, controlled, double-blind, crossover study of 19 patients receiving 100 mg zinc sulfate capsules or placebo three times daily, significantly reduced scores were seen in both treatment arms during the zinc treatment arm, with a relative plateau during the placebo phase.Citation76 In contrast, a similar trial of 220 mg zinc sulfate dosed twice daily showed no difference in patients receiving zinc therapy versus placebo.Citation77 Neither of the studies on oral zinc products produced any side effects of concern. Since both studies did not account for rosacea subtypes, future studies should focus on precise data collection to determine which subtypes, if any, are benefited most by the antioxidant and anti-inflammatory properties of zinc.
Lasers and lights
Many lasers have created a paradigm shift in the treatment of erythema and telangiectasias associated with rosacea. Those most commonly used include the pulsed dye laser (PDL, 585−595 nm), intense pulsed light (IPL, 500−1,200 nm), potassium titanyl phosphate (KTP, 532 nm) laser, and long-pulsed neodymium:yttrium-aluminum-garnet laser (Nd:YAG, 1,064 nm).Citation78–Citation82 Carbon dioxide (CO2) and erbium:yttrium-aluminum-garnet (Er:YAG) induce drastically higher target temperatures resulting in vaporization, and are therefore implemented in ablative correction of rhinophyma and other manifestations of phymatous rosacea. The older generation of argon, copper bromide, and krypton lasers paved the way for new lasers and lights developed specifically for cutaneous vascular lesions with more precision to minimize such side effects as hypopigmentation, atrophic scars, and recovery time.Citation83,Citation84 Laser settings used in major studies of the treatment of rosacea with prominent telangiectasia and erythema () and phymatous rosacea () are outlined in detail, with laser manufacturers listed when specified by the authors. An in-depth review of all the published studies using lasers and/or lights for the treatment of rosacea is beyond the scope of this current review.
Table 2 Data from nonablative laser and light studies in rosacea treatment
Table 3 Data from studies on ablative lasers in the treatment of phymatous rosacea
Pulsed dye laser
PDL historically emitted light at 577 nm and more recently at 585 nm or 595 nm, all wavelengths that closely correspond with the absorption peak of oxyhemoglobin and thus target superficial vasculature.Citation78,Citation85 Post-treatment purpura was a disadvantage of classic PDL treatments, but has been minimized in modern studies.Citation86 The latest generation of PDL utilizes longer pulse durations and has the ability to emit variable energies that specifically target telangiectasias with less purpura and dyspigmentation than previously (“subpurpuric dosing”).Citation87–Citation89
PDL has been shown to improve both the clinical findings of rosacea (erythema, telangiectasia) as well as the associated symptoms.Citation87–Citation97,Citation107,Citation117 In one study, after verifying sensitivity with a provocative lactic acid test, 32 patients with rosacea were treated with one session of 585 nm PDL.Citation93 Thirty-one patients who were stinger positive before treatment showed decreased scores after treatment, and one patient had the same stinger test score before and after treatment. In addition, biopsies taken before and 3 months after treatment were analyzed immunohistochemically for changes in substance P, calcitonin gene-related peptide, and vasoactive intestinal polypeptide, all of which are neuropeptides implicated in microvascular pathophysiology. Dermal papillae demonstrated a statistically significant reduction in the number of substance P-positive nerve fibers; however, no effect was seen on either vasoactive intestinal polypeptide or calcitonin gene-related peptide immunoreactivity. This finding highlights substance P as a potential key player in the pathophysiology of the vascular changes prominent in rosacea and responsive to PDL therapy.
Intense pulsed light
IPL has been shown to be applicable in various clinical settings, including rosacea, port wine stains, disseminated porokeratosis, seborrheic keratosis, sarcoidosis, and hypertrophic keloid scars.Citation98 Parameter flexibility enables the targeting of deep vessels, as well as large areas of telangiectasia, erythema, and flushing, but does require clinical expertise and experience to perfect treatments and decrease complications. Most IPL systems provide a large spot size, reducing patient discomfort, increasing efficiency of treatment, and enabling deeper light penetration. When used appropriately, IPL appears to provide impressive results in various settings with a relatively negligible side effect profile.Citation97–Citation111
Early on, Angermeier demonstrated 75%−100% clearance after one or two treatments in 174 of 188 patients with vascular lesions at a 2-month follow-up.Citation99 Soon after, these same results were confirmed in a study specific to rosacea only.Citation100 Thirty-two patients treated with double-pulsed IPL for an average of 3.6 times with at least 3-week intervals achieved improved redness (83%), flushing and texture (75%) and acneiform breakouts (64%) subjectively at 3−4-month follow-up self-assessments. Notably, very few patients experienced purpura (n=1), peeling (n=1), or post-inflammatory hyperpigmentation (n=1).
IPL demonstrated a decrease in blood flow (30%), a decrease in surface area of telangiectasias (29%), and a decrease in the intensity of erythema (21%) in one study using a 510 nm filter.Citation101 This implies that IPL treatments have a clinically relevant effect on the local cutaneous vasculature, which is central to the symptomatology seen in patients with rosacea.
Taub et al tackled the persistent background erythema often remaining after effective targeted therapy of telangiectasia in patients with ETR.Citation106 Twenty-one patients with ETR received five monthly facial treatments of a electro-optical synergy device combining pulsed light (470−980 nm) with bipolar radiofrequency (Elos, Syneron). The electro-optical synergy parameters were complex, with a combination of short pulses (13 msec light and 80 msec radiofrequency) performed horizontally and long pulses (12 msec light and 85 msec radiofrequency) performed vertically. Outcome measures of erythema and telangiectasia were assessed by clinicians comparing before and after photographs in addition to self-assessment scores. Significant improvement was achieved in both erythema and telangiectasia assessed by both physicians and patients at all follow-up intervals. Notably, patients reported significant improvement in flushing, one of the most psychosocially challenging disease manifestations.
Of note, IPL (560 nm filter) has been compared with nonpurpuric (6 msec) PDL in a head-to-head, randomized, controlled, split-face trial, and it was found that both treatment modalities demonstrated similar efficacy in improving erythema and telangiectasia in 29 patients with ETR.Citation107
Potassium-titanyl phosphate laser
Ideal for linear, arborizing, and discrete telangiectasia, KTP laser, a product of the 1,064 nm yttrium-aluminum-garnet laser family, results from passing Nd:YAG light through a KTP crystal that halves the wavelength, producing a 532 nm green light. Emitting light twice the frequency of Nd:YAG, KTP interacts with superficial chromophores, making it quite useful for superficial vessels and with less healing time.Citation112–Citation117 Although beneficial for such lesions, such low wavelengths have the disadvantage of interacting with melanin and are limited to lighter skin tones due to the risk of post-inflammatory hyperpigmentation. With minimal discomfort, KTP can target vessels 1−3 mm below the skin surface, and increasing pulse widths enable treatment of vessels of larger diameter. Some recommend cooling the skin with chilled water-based gel and utilizing post-treatment ice, basing each treatment session off an endpoint when vascular lesions appear grayish and are no longer readily visible.Citation113
PDL (595 nm, 1.5 msec) and KTP was studied head-to-head in 20 female patients with facial or leg telangiectasias.Citation117 Photographs taken before treatment and on four different follow-up visits were scored on a five-point scale (zero to four) by the patient and a blinded physician and nurse in addition to patient-rated 10-point pain scores. Twelve weeks after one to two treatments, PDL resulted in an average telangiectasia improvement score of 3.1 in the lower extremities and 3.8 on the face compared with 1.8 and 2.3 for lesions treated with KTP on the five-point efficacy scale. Despite the clearly superior efficacy of PDL in this study, patients noted significantly more pain, hyperpigmentation, and purpura lasting up to 2 weeks, and therefore may prefer multiple KTP treatments. KTP has also be studied against IPL, with clinical improvements demonstrated for both, but with a significant skin temperature rise immediately after KTP as compared with no change in skin temperature after IPL.Citation118
Neodymium:yttrium-aluminum-garnet laser
Long-pulsed Nd:YAG is efficacious in the treatment of large deep vessels with blue tones.Citation112 When evaluated in a split-face comparative study of 15 patients with ETR, both long pulsed Nd:YAG (1,064 nm) and short wavelength PDL yielded comparative responses with regard to erythema and telangiectasia.Citation119 This laser is not as commonly used in rosacea because larger blue veins or deep vascular networks are rarely present, but are useful for dilated leg or facial veins or recalcitrant vascular malformations/port wine stains.
CO2 laser and erbium:yttrium-aluminum-garnet laser
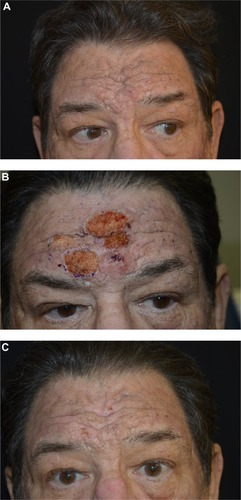
Many consider ablative lasers such as CO2 (10,600 nm) and Er:YAG (2,940 nm) as first-line treatment options for rhinophyma; however, various other surgical techniques have been shown to improve disfigurement, including cold steel, hot loop/radiowave and scalpel excision, electrosurgery, dermabrasion, and cryosurgery.Citation120–Citation139 All may be cosmetically limited due to excessive intraoperative bleeding obstructing visualization and causing imprecise tissue removal, along with the risk of scarring. Technological enhancements such as scanned and “superpulsed” systems emit shorter pulses with high power, reducing common adverse effects such as scarring and dyspigmentation. Ablative laser therapy can be used to contour the deformed nasal shape by partial excision of the sebaceous follicle to the bases. Despite transient swelling, erythema, and crusting which require longer healing times than nonablative lasers and risk permanent dyspigmentation, textural changes, and scarring, the ultimate results can be cosmetically and psychosocially life-changing in just one or two treatments ().
Figure 8 Before (A) and immediately after (B) continuous wave fully ablative carbon dioxide laser treatment, and 2 weeks following (C) treatment for metaphyma (enlargement of sebaceous glands on the forehead).
Clinical challenges: combination therapy and managing erythema in rosacea
Since rosacea is a chronic inflammatory condition, it is uncommon for a single treatment to effect a permanent cure, and many frequently fall short of dramatic improvement. In mild disease, topical treatments and lifestyle modification may be adequate. Most patients, however, have only slight responses to monotherapy and combination approaches are generally required. Erythema and telangiectasias are best treated by laser and light therapies, and often require combination with oral tetracyclines and topical immunotherapy and/or brimonidine topical gel (Mirvaso®). PPR often responds to a combination of oral tetracyclines with topical metronidazole, but if recurrent, recalcitrant, or severe, may require oral prednisone or isotretinoin. As previously stated, rhinophyma requires surgical or laser interventions for best results. Although oral isotretinoin has been reported to help sebaceous hyperplasia permanently, in the opinion of the senior author (JE) this is not seen in rhinophyma. A recent case report utilizing low-dose isotretinoin (20 mg daily for one year, followed by 10 mg daily for an additional year) prevented troublesome recurrence following CO2 ablation for a 20-year history of sebaceous hyperplasia in a 55-year-old Korean man.Citation140
Sebaceous hyperplasia has also troubled transplant patients on immunosuppression. Two cases of cyclosporine-induced sebaceous hyperplasia resolved 3 months after treatment with 10 or 20 mg isotretinoin daily.Citation141 No side effects, drug interactions, or transplant-associated complications were experienced. Higher doses of isotretinoin (40 mg each morning and 20 mg each evening) were used to treat refractory sebaceous hyperplasia in a 57-year-old Caucasian female, with reduction in lesion size after one month which was nearly complete by 2 months.Citation142 Despite these case reports, in our experience, rhinophyma requires surgical or laser intervention for a cure.
Most importantly, physicians must assess patient concerns and expectations at the first visit and educate about the condition, the long-term treatments required, and the at-home compliance and skin care (gentle cleansing, moisturizing, and photoprotection) needed for best results.Citation143
Pathophysiological changes in the erythematous and sebaceous skin of rosacea might differ between patients, yielding nonuniform treatment responses. For example, the vasculature involved in erythematous manifestations could be enlarged, thickened, dilated, or even newly formed, and conventional therapies may only target one dimension of these pathological changes. Thus, multiple modalities are often required and may not yield a permanent cure, but require lifelong maintenance after initial improvement.
Patient-focused perspectives: quality of life and patient satisfaction
As stated earlier, there is a significant burden on the quality of life (QoL) in patients with rosacea, not only cosmetically due to their unwanted appearance but also due to the painful and irritating symptoms associated with the condition. Rosacea patients present with higher rates of anxiety and depression, develop greater general symptom intensity, experience difficulty functioning in everyday life, perceive general health more negatively, and subjectively feel they receive poor social support.Citation144 They experience not only high loads of stress, but also embarrassment and social phobia as a result of their skin condition. Contrary to historical belief, rosacea patients have the highest comorbidity of depression, while alcohol abuse has a very mild association.Citation145
Clinical trials have tried to measure outcomes by improvement in patient QoL, which may be assessed by various standardized questionnaires, such as the Dermatology Life Quality Index (DLQI), Skindex-29, and rosacea-specific QoL indices. The DLQI questionnaire is a reliable and valid instrument that is quite sensitive to QoL changes brought about by various treatment options.Citation146,Citation147 The rosacea-specific QoL and Skindex-29 measure which characteristics of rosacea affect the patient’s life the most. Interestingly, flushing was found to be the most troubling symptom reported by patients affected by rosacea, stressing the importance of treating both the cosmetic and medical aspects of this condition.Citation148
The DLQI questionnaire evaluates QoL with ten questions covering the feelings, daily activities, clothing, physical or social activities, exercise, education or job, relationships, and treatments impacted by dermatological conditions. Developed in 1994, this measure has been utilized in the study of a variety of diseases, including rosacea. Variables are scored by patients on a Likert scale and final results range from 0 to 30, with higher numbers signifying more extreme effects on a patient’s QoL. Tan and Tope first applied this outcome measure to 16 ETR patients treated with PDL, and demonstrated a significant reduction from 7.8 to 1.9 at 2 months following two laser treatment sessions.Citation91 When measured in 20 patients before and after 595 nm PDL treatment, averaged DLQI scores decreased from 17.3 to 4.3, indicating a significant improvement in QoL from the patient perspective.Citation149 Finally, Menezes et al used this index to assess the impact of PDL in a prospective study of 22 patients with ETR and found a significant reduction from 5.6 before treatment to 1.5 after three treatment sessions.Citation150
Recommendations
Systemic isotretinoin therapy
As previously discussed, isotretinoin is a viable alternative for recalcitrant cases of rosacea. In a large-scale, placebo-controlled, randomized, 12-week, multicenter study, Gollnick et al demonstrated complete remission in 24% and marked improvement in 57% of patients with isotretinoin 0.3 mg/kg therapy daily, in contrast with remission in 14% and marked improvement in 55% of patients treated with doxycycline 100 mg daily for 14 days, then 50 mg daily. Patients treated with isotretinoin rated treatment results at the end of the study as “excellent improvement” more frequently, at 32.6% in comparison with 24.2% for patients treated with doxycycline.Citation67
OnabotulinumtoxinA injections
Anecdotal results of reduced erythema and acne with the use of OnabotulinumtoxinA (Botox®, Allergan, Irvine, CA, USA) for cosmetic purposes led Dayan et al to experiment further in 13 patients with rosacea.Citation151 Over the course of 2 years, patients received intralesional microdroplet injections (0.05 mL) of onabotulinumtoxinA in a dilution of 7 mL of saline solution per 100 units. The results indicated significant reduction in erythema and flushing of the affected area 2–4 weeks after treatment. Their predecessors reported similar results after a 26-year-old male was injected with 10 units of onabotulinumtoxinA at 1 cm intervals into one cheek.Citation152
Excel V laser: combining KTP and Nd:YAG
The new Excel V laser combines KTP and Nd:YAG, two previously discussed lasers with different wavelengths. KTP emits light at a wavelength of 532 nm, which targets redness, hyperpigmentation, and damaged capillaries at the surface of the skin, while Nd:YAG has a laser wavelength of 1,064 nm designed for treating more deep blood vessels with larger diameters. Following absorption of energy, abnormal blood vessels are thermosealed while hyperpigmented lesions are fragmented, resulting in an overall improved appearance.
Conclusion
Rosacea is a chronic inflammatory condition without a permanent cure. Recent advances in combination treatments offer treatments with better initial results and longer-term maintenance than in the past. The fundamental key for successful management of rosacea is based on identification of the specific subtype, understanding the severity of presentation, and tailoring treatments to best suit the expectations of the patient. Continued research into both the cosmetic and medical aspects of this condition will further define treatment protocols that ultimately will refine the current options available to patients.
Acknowledgments
The patient consent was received for the use of their images.
Disclosure
The authors report no conflicts of interest in this work.
References
- CribierBMedical history of the representation of rosacea in the 19th centuryJ Am Acad Dermatol2013696 Suppl 1S2S1424229633
- CrawfordGHPelleMTJamesWDRosacea: I. Etiology pathogenesis, and subtype classificationJ Am Acad Dermatol200451332734115337973
- WilkinJDahlMDetmarMStandard classification of rosacea: Report of the National Rosacea Society Expert Committee on the classification and staging of rosaceaJ Am Acad Dermatol200246458458711907512
- AbramKSilmHOonaMPrevalence of rosacea in an Estonian working population using a standard classificationActa Derm Venereol201090326927320526544
- TanJBergMRosacea: current state of epidemiologyJ Am Acad Dermatol2013696 Suppl 1S27S3524229634
- LomholtGPrevalence of skin diseases in a population; a census study from the Faroe IslandsDan Med Bull1964111714120983
- RomanowiczMStephensonJJDel RossoJQLenhartGHealthcare utilization and costs of patients with rosacea in an insured populationJ Drugs Dermatol200871414918246697
- McAleerMAFitzpatrickPPowellFCPapulopustular rosacea: prevalence and relationship to photodamageJ Am Acad Dermatol2010631333920462665
- SchaeferIRustenbachSJZimmerLAugustinMPrevalence of skin diseases in a cohort of 48,665 employees in GermanyDermatology2008217216917218525204
- AugustinMHerbergerKHintzenSHeigelHFranzkeNSchaferIPrevalence of skin lesions and need for treatment in a cohort of 90,880 workersBr J Dermatol2011165486587321623753
- BergMLidenSAn epidemiological study of rosaceaActa Derm Venereol19896954194232572109
- GuttmanCRosacea prevalence underestimatedDermatology Times2006274857
- TüzünYWolfRKutlubayZKarakuşOEnginBRosacea and rhinophymaClin Dermatol2014321354624314376
- VieiraACMannisMJOcular rosacea: common and commonly missedJ Am Acad Dermatol2013696 Suppl 1S36S4124229635
- SteinhoffMBuddenkotteJAubertJClinical, cellular and molecular aspects in the pathophysiology of rosaceaJ Investig Dermatol Symp Proc2011151211
- SteinhoffMSchauberJLeydenJNew insights into rosacea pathophysiology: a review of recent findingsJ Am Acad Dermatol2013696 Suppl 1S15S2624229632
- SchauberJGalloRLThe vitamin D pathway: a new target for control of the skin’s immune response?Exp Dermatol200817863363918573153
- Meyer-HoffertUSchroderJMEpidermal proteases in the pathogenesis of rosaceaJ Investig Dermatol Symp Proc20111511623
- GeorgalaSKatoulisACKylafisGDKoumantaki-MathioudakiEGeorgalaCAroniJIncreased density of Demodex folliculorum and evidence of delayed hypersensistivity reaction in subjects with papulopustular rosaceaJ Eur Acad Dermatol Venereol200115544144411763386
- HolmesADPotential role of microorganisms in the pathogenesis of rosaceaJ Am Acad Dermatol20136961025103224011460
- AubdoolAABrainSDNeurovascular aspects of skin neurogenic inflammationJ Investig Dermatol Symp Proc20111513339
- MooreAKempersSMirakawaGLong-term safety and efficacy of once-daily topical brimonidine tartrate gel 0.5% for the treatment of moderate to severe facial erythema of rosacea: results of a 1-year open-label studyJ Drugs Dermatol2014131566124385120
- FowlerJJarrattMMooreAOnce-daily topical brimonidine tartrate gel 0.5% is a novel treatment for moderate to severe facial erythema of rosacea: results of two multicenter, randomized and vehicle-controlled studiesBr J Dermatol2012166363364122050040
- JacksonJMFowlerJMooreAImprovement in facial erythema within 30 minutes of initial application of brimonidine tartrate in patients with rosaceaJ Drugs Dermatol201413669970424918560
- ShanlerSDOndoALSuccessful treatment of the erythema and flushing of rosacea using a topically applied selective alpha 1-adrenergic receptor agonist, oxymetazolineArch Dermatol2007143111369137118025359
- ThomasKYelvertonCBYentzerBABalkrishnanRFleischerABJrFeldmanSRThe cost-effectiveness of rosacea treatmentsJ Dermatol Treat20092027275
- ElewskiBEFleischerABJrPariserDMA comparison of 15% azelaic acid gel and 0.75% metronidazole gel in the topical treatment for papulopustular rosacea: results of a randomized trialArch Dermatol2003139111444145014623704
- WolfJEJrKerroucheNArsonnaudSEfficacy and safety of once-daily metronidazole 1% gel compared with twice-daily azelaic acid 15% gel in the treatment of rosaceaCutis2006774 Suppl31116706244
- TrumboreMWGoldsteinJAGurgeRMTreatment of papulopustular rosacea with sodium sulfacetamide 10% – sulfur 5% emollient foamJ Drugs Dermatol20098329930419271381
- Del RossoJQThiboutotDGalloRConsensus recommendations from the American Acne and Rosacea Society on the management of rosacea. Part 2: a status report on topical agentsCutis201392627728424416742
- KarabulutAAIzol SerelBEksiogluHMA randomized, single-blind, placebo-controlled, split-face study with pimecrolimus cream 1% for papulopustular rosaceaJ Eur Acad Dermatol Venereol200822672973418328059
- CrawfordKMRussBBostromPPimecrolimus for treatment of acne rosaceaSkinmed20054314715015891250
- KocaRAltinyazarHCAnkaraliHMuhtarSTekinNSCinarSA comparison of metronidazole 1% cream and pimecrolimus 1% cream in the treatment of patients with papulopustular rosacea: a randomized open-label clinical trialClin Exp Dermatol201035325125619594764
- KocakMYağliSVahapoğluGEksioğluMPermethrin 5% cream versus metronidazole 0.75% gel for the treatment of papulopustular rosacea: A randomized double-blind placebo-controlled studyDermatology2002205326527012399675
- SignoreRJA pilot study of 5 percent permethrin cream versus 0.75 percent metronidazole gel in acne rosaceaCutis19955631771798565604
- AllenKJDavisCLBillingsSDMousdicasNRecalcitrant papulopustular rosacea in an immunocompetent patient responding to combination therapy with oral ivermectin and topical permethrinCutis200780214915117944176
- SteinLKircikLFowlerJEfficacy and safety of ivermectin 1% cream in treatment of papulopustular rosacea: results of two randomized, double-blind, vehicle-controlled pivotal studiesJ Drugs Dermatol201413331632324595578
- ForstingerCKittlerHBinderMTreatment of rosacea-like demodicidosis with oral ivermectin and topical permethrin creamJ Am Acad Dermatol1999415 Pt 177577710534645
- PariserDMMeinkingTLBellMRyanWGTopical 0.5% ivermectin lotion for treatment of head liceN Engl J Med2012367181687169323113480
- FilhoPAHazarbassanovRMGrisoliaABPazosHBKaisermanIGomesJAThe efficacy of oral ivermectin for the treatment of chronic blepharitis in patients tested positive for Demodex sppBr J Ophthalmol201195689389521349944
- BrenemanDSavinRVandePolCVamvakiasGLevySLeydenJDouble-blind, randomized, vehicle-controlled clinical trial of once-daily benzoyl peroxide/clindamycin topical gel in the treatment of patients with moderate to severe rosaceaInt J Dermatol200443538138715117375
- LeydenJJRandomized, phase 2, dose-ranging study in the treatment of rosacea with encapsulated benzoyl peroxide gelJ Drugs Dermatol201413668568824918558
- EmerJWaldorfHBersonDBotanicals and anti-inflammatories: natural ingredients for rosaceaSemin Cutan Med Surg201130314815521925368
- BaldwinHBersonDVitaleMYatskayerMChenNOresajoCClinical effects of a novel topical composition on persistent redness observed in patients who had been successfully treated with topical or oral therapy for papulopustular rosaceaJ Drugs Dermatol201413332633124595579
- FerrariADiehlCEvaluation of the efficacy and tolerance of a topical gel with 4% quassia extract in the treatment of rosaceaJ Clin Pharmacol2012521848821343346
- SchlesingerTEPowellCREfficacy and tolerability of low molecular weight hyaluronic acid sodium salt 0.2% cream in rosaceaJ Drugs Dermatol201312666466723839183
- GariboldiSPalazzoMZanobbioLLow molecular weight hyaluronic acid increases the self-defense of skin epithelium by induction of beta-defensin 2 via TLR2 and TLR4J Immunol200818132103211018641349
- Del RossoJQWebsterGFJacksonMTwo randomized phase III clinical trials evaluating anti-inflammatory dose doxycycline (40-mg doxycycline, USP capsules) administered once daily for treatment of rosaceaJ Am Acad Dermatol200756579180217367893
- KanadaKNNakatsujiTGalloRLDoxycycline indirectly inhibits proteolytic activation of tryptic kallikrein-related peptidases and activation of cathelicidinJ Invest Dermatol201213251435144222336948
- LaytonAThiboutotDEmerging therapies in rosaceaJ Am Acad Dermatol2013696 Suppl 1S57S6524229638
- Del RossoJQThiboutotDGalloRConsensus recommendations from the American Acne and Rosacea Society on the management of rosacea. Part 3: a status report on systemic therapiesCutis2014931182824505581
- Del RossoJQSchlessingerJWerschlerPComparison of anti-inflammatory dose doxycycline versus doxycycline 100 mg in the treatment of rosaceaJ Drugs Dermatol20087657357618561589
- Del RossoJQThe ORCA (Oracea for Rosacea: a Community-based Assessment) trial: a large-scale, phasae 4 trial in papulopustular rosaceaCutis2010865 Suppl4621229825
- WebsterGFAn open-label, community-based, 12-week assessment of the effectiveness and safety of monotherapy with doxycycline 40 mg (30-mg immediate-release and 10-mg delayed-release beads)Cutis2010865 Suppl71521229826
- AlexisAFWebsterGPrestonNJCaveneySWGottschalkRWEffectiveness and safety of once-daily doxycycline capsules as monotherapy in patients with rosacea: an analysis by Fitzpatrick skin typeJ Drugs Dermatol201211101219122223134987
- JacksonJMKircikLHLorenzDJEfficacy of extended-release 45 mg oral minocycline and extended-release 45 mg oral minocycline plus 15% azelaic acid in the treatment of acne rosaceaJ Drugs Dermatol201312329229823545911
- SobolewskaBDoychevaDDeuterCPfefferISchallerMZierhutMTreatment of ocular rosacea with once-daily low-dose doxycyclineCornea201433325726024452213
- PfefferIBorelliCZierhutMSchallerMTreatment of ocular rosacea with 40 mg doxycycline in a slow release formJ Dtsch Dermatol Ges201191190490721672164
- MantelliFDi ZazzoASacchettiMDianzaniCLambiaseABoniniSTopical azithromycin as a novel treatment for ocular rosaceaOcul Immunol Inflamm201321537137723875944
- ThiboutotDMFleischerABDel RossoJQRichPA multicenter study of topical azelaic acid 15% gel in combination with oral doxycycline as initial therapy and azelaic acid 15% gel as maintenance monotherapyJ Drugs Dermatol20098763964819588640
- FowlerJFJrCombination effect of anti-inflammatory dose doxycycline (40-mg doxycycline, USP monohydrate controlled-release capsules) and metronidazole topical gel 1% in the treatment of rosaceaJ Drugs Dermatol20076664164517668530
- ModiSHartingMRosenTAzithromycin as an alternative rosacea therapy when tetracyclines prove problematicJ Drugs Dermatol20087989889919112809
- KimJHOhYSChoiEHOral azithromycin for treatment of intractable rosaceaJ Korean Med Sci201126569469621532865
- SehgalVNSharmaSSardanaKRosacea/acne rosacea: efficacy of combination therapy of azithromycin and topical 0.1% tacrolimus ointmentJ Eur Acad Dermatol Venereol200822111366136818435734
- PyeRJBurtonJLTreatment of rosacea by metronidazoleLancet1976179711211121258258
- ParkHDel RossoJQUse of oral isotretinoin in the management of rosaceaJ Clin Aesthet Dermatol201149546121938271
- GollnickHBlume-PeytaviUSzaboELSystemic isotretinoin in the treatment of rosacea – doxycycline- and placebo-controlled, randomized clinical studyJ Dtsch Dermatol Ges20108750551520337772
- HoferTContinuous ‘microdose’ isotretinoin in adult recalcitrant rosaceaClin Exp Dermatol200429220420514987287
- PalmerRASidhuSGoodwinPG‘Microdose’ isotretinoinBr J Dermatol2000143120520610886171
- PavlisMBLieblichLIsotretinoin-induced skin fragility in a teenaged athlete: a case reportCutis2013921333423961523
- HolmesSCThomsonJIsotretinoin and skin fragilityBr J Dermatol199513211657756141
- RubensteinRRoenigkHHJrStegmanSJHankeCWAtypical keloids after dermabrasion of patients taking isotretinoinJ Am Acad Dermatol1986152 Pt 12802853018052
- ZachariaeHDelayed wound healing and keloid formation following argon laser treatment or dermabrasion during isotretinoin treatmentBr J Dermatol198811857037062969261
- ChandrashekarBSVarshaDVVasanthVMaduraCRajashekarMLSafety of performing invasive acne scar treatment and laser hair removal in patients on oral isotretinoin: a retrospective study of 110 patientsInt J Dermatol201453101281128525039864
- YoonJHParkEJKwonIHConcomitant use of an infrared fractional laser with low-dose isotretinoin for the treatment of acne and acne scarsJ Dermatolog Treat201425214214623336106
- SharquieKENajimRAAl-SalmanHNOral zinc sulfate in the treatment of rosacea: a double-blind, placebo controlled studyInt J Dermatol200645785786116863527
- BamfordJTGessertCEHallerIVKrugerKJohnsonBPRandomized, double-blind trial of 220 mg zinc sulfate twice daily in the treatment of rosaceaInt J Dermatol201251445946222435439
- AndersonRRParishJASelective photothermolysis: precise microsurgery by selective absorption of pulsed radiationScience198322045965245276836297
- BenciniPLTourlakiADe GiorgiVGalimbertiMLaser use for cutaneous vascular alterations of cosmetic interestDermatol Ther201225434035122950561
- CameronHIbbotsonSHFergusonJDaweRSMoseleyHA randomized, blinded, controlled study of the clinical relevance of matching pulse duration to thermal relaxation time when treating facial telangiectasiaLasers Med Sci2005203−411712116151607
- TanghettiEDel RossoJQThiboutotDConsensus recommendations from the American acne and rosacea society on the management of rosacea. Part 4: a status report on physical modalities and devicesCutis2014932717624605343
- MansouriYGoldenbergGDevices and topical agents for rosacea managementCutis2014941212525101340
- ArndtKAArgon laser therapy of small cutaneous vascular lesionsArch Dermatol198211842202246461295
- LaubeSLaniganSWLaser treatment of rosaceaJ Cosmet Dermatol20021418819517147538
- ErcegAde JongEMvan de KerkhofPCSeygerMMThe efficacy of pulsed dye laser treatment for inflammatory skin diseases: a systematic reviewJ Am Acad Dermatol201369460961523711766
- ButterwickKJButterwickLSHanALaser and light therapies for acne rosaceaJ Drugs Dermatol200651353916468290
- BernsteinEFKligmanARosacea treatment using the new-generation, high-energy, 595 nm, long pulse-duration pulsed-dye laserLasers Surg Med200840423323918412227
- LoweNJBehrKLFitzpatrickRGoldmanMRuiz-EsparzaJFlash lamp pumped dye laser for rosacea-associated telangiectasia and erythemaJ Dermatol Surg Oncol19911765225251828257
- AlamMDoverJSArndtKATreatment of facial telangiectasia with variable-pulse high-fluence pulsed-dye laser: comparison of efficacy with fluences immediately above and below the purpura thresholdDermatol Surg200329768168512828690
- JasimZFWooWKHandleyJMLong-pulsed (6-ms) pulsed dye laser treatment of rosacea-associated telangiectasia using subpurpuric clinical thresholdDermatol Surg2004301374014692924
- TanSRTopeWDPulsed dye laser treatment of rosacea improves erythema, symptomatology, and quality of lifeJ Am Acad Dermatol200451459259915389196
- TanSTBialostockiAArmstrongJRPulsed dye laser therapy for rosaceaBr J Plast Surg200457430331015145732
- Lonne-RahmSNordlindKEdstromDWRosAMBergMLaser treatment of rosacea: a pathoetiological studyArch Dermatol2004140111345134915545543
- Togsverd-BoKWiegellSRWulfHCHaedersdalMShort and limited effect of long-pulse dye laser alone and in combination with photodynamic therapy for inflammatory rosaceaJ Eur Acad Dermatol Venereol200923220020118452529
- KimTGRohHJChoSBLeeJHLeeSJOhSHEnhancing effect of pretreatment with topical niacin in the treatment of rosacea-associated erythema by 585-nm pulsed dye laser in Koreans: a randomized, prospective, split-face trialBr J Dermatol2011164357357921143465
- KashlanLGraberEMArndtKAHair dryer use to optimize pulsed dye laser treatment in rosacea patientsJ Clin Aesthet Dermatol201256414422768356
- LaniganSReduction of pain in the treatment of vascular lesions with a pulsed dye laser and pneumatic skin flatteningLasers Med Sci200924461762019050824
- PiccoloDDi MarcantonioDCrismanGUnconventional use of intense pulsed lightBiomed Res Int2014201461820625276803
- AngermeierMCTreatment of facial vascular lesions with intense pulsed lightJ Cutan Laser Ther1999129510011357295
- TaubAFTreatment of rosacea with intense pulsed lightJ Drugs Dermatol20032325425912848109
- MarkKASparacioRMVoigtAMarenusKSarnoffDSObjective and quantitative improvement of rosacea-associated erythema after intense pulsed light treatmentDermatol Surg200329660060412786702
- SchroeterCAHaff-von BelowSNeumannHAEffective treatment of rosacea using intense pulsed light systemsDermatol Surg200531101285128916188180
- PapageorgiouPClaytonWNorwoodSChopraSRustinMTreatment of rosacea with intense pulsed light: significant improvement and long-lasting resultsBr J Dermatol2008159362863218565174
- KassirRKolluruAKassirMIntense pulsed light for the treatment of rosacea and telangiectasiasJ Cosmet Laser Ther201113521622221848421
- SperberBRWallingHWArpeyCFWhitakerDCVesiculobullous eruption from intense pulsed light treatmentDermatol Surg200531334534815841640
- TaubAFDevitaEFSuccessful treatment of erythematotelangiectatic rosacea with pulsed light and radiofrequencyJ Clin Aesthet Dermatol200811374021103309
- NeuhausIMZaneLTTopeWDComparative efficacy of nonpurpuragenic pulsed dye laser and intense pulsed light for erythematotelangiectatic rosaceaDermatol Surg200935692092819397667
- LaneJEKhachemouneAUse of intense pulsed light to treat refractory granulomatous rosaceaDermatol Surg201036457157320402938
- LiuJLiuJRenYLiBLuSComparative efficacy of intense pulsed light for different erythema associated with rosaceaJ Cosmet Laser Ther201416632432725151911
- LimHSLeeSCWonYHLeeJBThe efficacy of intense pulsed light for treating erythematotelangiectatic rosacea is related to severity and ageAnn Dermatol201426449149525143679
- TsunodaKTakahashiKOginoNYoshidaAAkasakaTTreatment of facial telangiectasia with a small spot of intense pulsed light: a case series of three patientsJ Dermatol201441763864124931642
- PelleMTCrawfordGHJamesWDRosacea: II. TherapyJ Am Acad Dermatol200451449951215389184
- BassichisBASwamyRDayanSHUse of the KTP laser in the treatment of rosacea and solar lentiginesFacial Plast Surg2004201778315034818
- BecherGLCameronHMoseleyHTreatment of superficial vascular lesions with the KTP 532-nm laser: experience with 647 patientsLasers Med Sci201429126727124401943
- ClarkCCameronHMoseleyHFergusonJIbbotsonSHTreatment of superficial cutaneous vascular lesions: experience with the KTP 532 nm laserLasers Med Sci20041911515316851
- MillerATreatment of erythematotelangiectatic rosacea with a KTP YAG laserJ Drugs Dermatol20054676076216302564
- WestTBAlsterTSComparison of the long-pulse dye (590−595 nm) and KTP (532 nm) lasers in the treatment of facial and leg telangiectasiasDermatol Surg19982422212269491116
- GeorgeJBensafiASchmittAMValidation of a non-contact technique for local skin temperature measurementsSkin Res Technol200814438138418937770
- SalemSAAbdel FattahNSTantawySMEl-BadawyNMAbd El-AzizYANeodymium-yttrium aluminum garnet laser versus pulsed dye laser in erythemato-telangiectatic rosacea: comparison of clinical efficacy and effect on cutaneous substance (P) expressionJ Cosmet Dermatol201312318719423992160
- AlamMVoravutinonNWarychaMComparative effectiveness of nonpurpuragenic 595-nm pulsed dye laser and microsecond 1064-nm neodymium:yttrium-aluminum-garnet laser for treatment of diffuse facial erythema: a double-blind randomized controlled trialJ Am Acad Dermatol201369343844323688651
- MattonGPickrellKHugerWPoundEThe surgical treatment of rhinophyma: an analysis of 57 casesPlast Reconstr Surg196230403414
- LimRYContact Nd:YAG laser excision of rhinophymaW V Med J199490262638165809
- WenigBLWeingartenRTExcision of rhinophyma with Nd:YAG laser: a new techniqueLaryngoscope19931031 Pt 11011038421411
- ApfelbergDBSide effects, sequelae, and complications of carbon dioxide laser resurfacingAesthet Surg J199717636537219328086
- CampolmiPBonanPCannarozzoGHighlights of thirty-year experience of CO2 laser use at the Florence (Italy) department of dermatologyScientificWorldJournal2012201254652822593693
- ShapshaySMStrongMSAnastasiGWVaughanCWRemoval of rhinophyma with the carbon dioxide laser: a preliminary reportArch Otolaryngol198010652572596445187
- MadenVFergusonJEAugustPJCarbon dioxide laser treatment of rhinophyma: a review of 124 patientsBr J Dermatol2009161481481819624541
- LimSWLimSWBekhorPRhinophyma: carbon dioxide laser with computerized scanner is still an outstanding treatmentAustralas J Dermatol200950428929319916975
- CravoMCanelasMMCardosoJCVieiraRFigueiredoACombined carbon dioxide laser and bipolar electrocoagulation: another option to treat rhinophymaJ Dermatol Treat2009203146148
- RaiSMadanVTreatment of metophyma with the carbon dioxide laserDermatol Surg201238351351522385227
- MoreiraALeiteIGuedesRBaptistaAMotaGSurgical treatment of rhinophyma using carbon dioxide (CO2) laser and pulsed dye laser (PDL)J Cosmet Laser Ther2010122737620331343
- SerowkaKLSaediNDoverJSZacharyCBFractionated ablative carbon dioxide laser for the treatment of rhinophymaLasers Surg Med201446181224123064
- SinghSPetersonJDFriedmanPMManagement of mild to moderate rhinophyma using ablative fractional photothermolysisDermatol Surg20133971110111323773176
- CarradinoBDi LorenzoSMoschellaF“Downward steps techinique” with CO2 ultrapulsed laser for the treatment of rhinophyma: our protocolActa Chir Plast2013551161824188317
- BassiACampolmiPDindelliMLaser surgery in rhinophymaG Ital Dermatol Venereol9182014 Epub ahead of print
- LazzeriDLarcherLHuemerGMSurgical correction of rhinophyma: comparison of two methods in a 15-year-long experienceJ Craniomaxillofac Surg201341542943623232283
- OrensteinAHaikJTamirJTreatment of rhinophyma with Er:YAG laserLasers Surg Med200129323023511573224
- GoonPKDalalMPeartFCThe gold standard for decortication of rhinophyma: combined erbium-YAG/CO2 laserAesthetic Plast Surg200428645646015625593
- FincherEFGladstoneHBUse of a dual-mode erbium:YAG laser for the surgical correction of rhinophymaArch Facial Plast Surg20046426727115262723
- NohSSinJUJungJYLeeJHA case of sebaceous hyperplasia maintained on low-dose isotretinoin after carbon dioxide laser treatmentIn J Dermatol2014532e151e153
- McDonaldSKGohMSChongAHSuccessful treatment of cyclosporine-induced sebaceous hyperplasia with oral isotretinoin in two renal transplant recipientsAustralas J Dermatol201152322723021834824
- YuCShahsavariMStevensGLiskanichRHorowitzDIsotretinoin as monotherapy for sebaceous hyperplasiaJ Drugs Dermatol20109669970120645535
- Del RossoJQAdvances in understanding and managing rosacea. Part 2: the central role, evaluation, and medical management of diffuse and persistent facial erythema of rosaceaJ Clin Aesthet Dermatol201253263622468177
- MoustafaFLewallenRSFeldmanSRThe psychosocial impact of rosacea and the influence of current management optionsJ Am Acad Dermatol201471597398024993600
- GuptaMAGuptaAKChenSJJohnsonAMComorbidity of rosacea and depression; an analysis of the National Ambulatory Medical Care Survey and National Hospital Ambulatory Care Survey – Outpatient department data collected by the US National Center for Health Statistics from 1995 to 2002Br J Dermatol200515361176118116307654
- AksoyBAltaykan-HapaAEgemenDKaragözFAtakanNThe impact of rosacea on quality of life: effects of demographic and clinical characteristics and various treatment modalitiesBr J Dermatol2010163471972520545683
- FinlayAYKhanGKDermatology life quality index (DLQI) – a simple practical measure for routine clinical useClin Exp Dermatol19941932102168033378
- NicholsonKAbramovaLChrenMMYeungJChonSYChenSCA pilot quality-of-life instrument for acne rosaceaJ Am Acad Dermatol200757221322117445948
- ShimTNAbdullahHThe effect of pulsed dye laser on the dermatology life quality index in erythematotelangiectatic rosacea patients: an assessmentJ Clin Aesthet Dermatol201364303223630639
- MenezesNMoreiraAMotaGBaptistaAQuality of life and rosacea: pulsed dye laser impactJ Cosmet Laser Ther200911313914119462330
- DayanSHPritzkerRNArkinsJPA new treatment regimen for rosacea: onabotulinumtoxinAJ Drugs Dermatol20121112e76e7923377526
- YuraitisMJacobCIBotulinum toxin for the treatment of facial flushingDermatol Surg200430110210414692937
