Abstract
Aggressive digital papillary adenocarcinomas are rare malignant tumors often located on the digits of the hand. Due to lack of pain, slow growth, and an inconspicuous appearance, diagnosis is often missed or delayed. We report two cases and review the present literature to give recommendations for diagnosis and treatment.
Introduction
Sweat gland carcinomas are rare malignant tumors of the skin.Citation1–Citation5 One entity is the aggressive digital papillary adenocarcinoma. These tumors are capable of aggressive local invasion resulting in a high recurrence rate, and are characterized by predominantly digital location. As the tumor is slow-growing, painless, and clinically inconspicuous, the diagnosis is often missed or delayed. We report two cases of aggressive digital papillary adenocarcinoma, including clinical course, pathological findings, and therapeutic approach, and review the present literature.
Case report 1
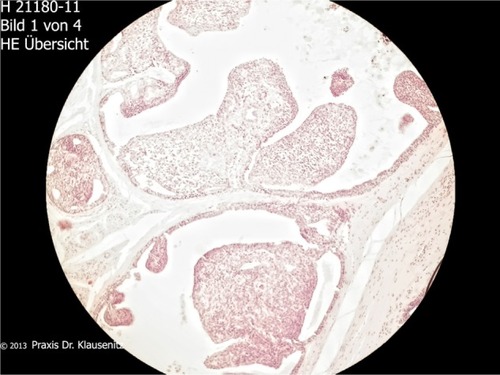
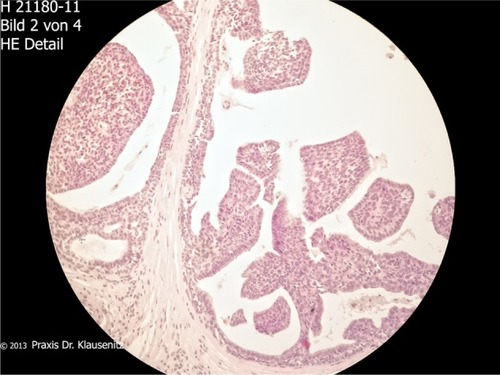
A 52-year-old man presented with a 12-month history of a swelling of the distal phalanx of the right middle finger without prior trauma or infection (). The tumor was not palpable because the fingertip was plump and sometimes painful. There was no redness, discoloration, or inflammation of the skin. Sensation, motion, and perfusion were not impaired. X-ray findings showed no bony involvement. Intraoperatively, we observed a cystic brown tumor with a soft consistency (). Histologic examination revealed a cystic tubulopapillary epithelial tumor. A computed tomographic scan of the chest, ultrasound of the abdomen, and bone scintigraphy showed no evidence of metastasis. We chose an aggressive surgical approach consisting of amputation of the middle phalanx and regional lymph node dissection. The surgical margins of the finger and the lymph nodes were free of tumor. Ten-year follow-up did not show any recurrence.
Case report 2
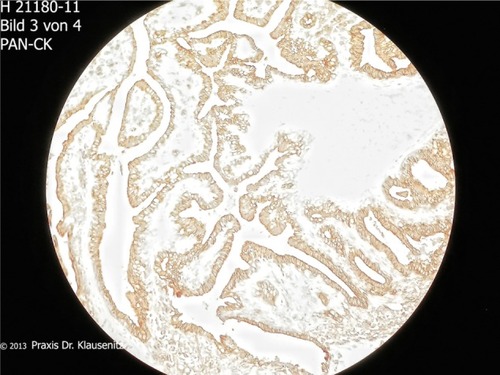
A 54-year-old man presented with a 1×1 cm solid painless tumor on the dorsal side of the middle phalanx of the right middle finger. The tumor showed slow growth over 14 months. The tumor had been previously resected at another institution under local anesthesia. The histologic report disclosed an aggressive digital papillary adenocarcinoma with margins not free of tumor (–). Physical examination at our institution showed a bland scar on the middle dorsal phalanx with full function of the hand. X-ray imaging of the hand, magnetic resonance imaging, and a computed tomographic scan of the chest and abdomen were not suspicious for tumor spread. The patient refused finger amputation. An excision of the scar with adequate safety margins was done once again. There were no tumor cells detected in the histological specimen. The defect was covered with a full-thickness skin graft (). The sentinel lymph node was free of tumor. Postoperative wound healing was very good, and function of the right hand was not impaired. Staging procedures, including colonoscopy, bronchoscopy, gastroscopy, and ultrasound of the thyroid gland revealed no further tumor localization. No recurrence was detected at follow-up after 18 months.
Discussion
Aggressive digital papillary adenocarcinoma is a rare cutaneous malignancy.Citation1–Citation9 It was first described in 1984 by Helwig et al, who used the term “eccrine acrospiroma”. The term “aggressive digital papillary adenocarcinoma” was introduced decades later by Duke et al,Citation2 although it is a low-grade rather than a high-grade malignancy. Histologically, tumor features include a grenz zone, fibrocollagenous stroma, a mixed tubuloalveolar and papillary pattern, and focal squamous metaplasia.Citation10 The differential diagnosis comprises apocrine adenocarcinoma, adenoid cystic carcinoma of the sweat glands, and mucinous eccrine carcinoma. Large series published about this entity are rare. There is one initial retrospective clinicopathological study published by Kao et al, which included 57 patients.Citation7 The authors reported a local recurrence rate of 47% and a 41.2% rate of distant spreading. Patients with metastases died 5–20 years after diagnosis, indicating the low-grade malignancy of the tumor. Authors classified subgroups as aggressive digital papillary adenomas and aggressive digital papillary adenocarcinomas based on histological criteria. Currently, it is recommended to avoid the term aggressive digital papillary adenoma, as all such tumors possess metastatic potential.Citation2 Other authors report lymph node and lung metastases developing in up to 14% of cases.Citation6,Citation8 There is no effective treatment for widespread disease. Another follow-up study of aggressive digital papillary adenocarcinomas from the same institution was published in 2000 by Duke et al.Citation2 Sixty-seven cases were included in this study. These authors found subsequent radical excision to be imperative to prevent local recurrence. In this series, only 5% recurrence occurred when the tumor was treated with subsequent excision or digital amputation, compared with 50% recurrence when not so treated. Interestingly, none of the clinical or histological features described above was predictive for local recurrence or metastasis. The findings of a recent study from 2012 that included 31 patients are in accordance with the results described above.Citation11 These authors recommended wide excision or amputation as treatment, and reported a local recurrence rate of 16% thereafter. The metastasis rate was reported to be 19%, and 16% of metastases were located in the lung. Concerning the clinical appearance, the lesion often presents as a nonspecific mass in the fingers or toes, which gradually enlarges over years.Citation7,Citation9 Dorsal localization, as in our second case, is very uncommon, but should be taken into consideration. The typical age of patients with aggressive digital papillary adenocarcinoma is the fifties to seventies, with a predominance of male over female patients.Citation7,Citation11 The history in both our cases was very similar, ie, a painless tumor with slow growth. The histology of our cases showed partly solid and partly cystic tumor tissue with papillary epithelial proliferation. No recurrence or metastasis has been detected in our patients during follow-up. Due to the slow growth and absence of symptoms, the patient and the physician in charge often trivialize the findings. The tumor can be easily confused with infection, a ganglion, or a cyst, which can lead to wrong or delayed therapy.
In accordance with recommendations given in a previous study,Citation12 we propose an exact diagnosis followed by a radical excision of the tumor (excisional biopsy plus subsequent radical excision) and staging of the regional lymph nodes, lung, and abdomen. The benefit of sentinel lymph node biopsy is still controversial.Citation13 We recommend a clinical follow-up period of 10 years.
Conclusion
Digital papillary adenocarcinoma is a rare but life-threatening malignancy, and the diagnosis is easily missed or delayed. Physicians in charge should be aware of their potential existence and confirm the diagnosis by biopsy in suspicious cases. In the event of a confirmed diagnosis, excision biopsy should be followed by radical excision and patient follow-up for a period of 10 years.
Disclosure
No funding was received for the present work. The authors have no financial or other conflicts of interest to disclose.
References
- DaigelerAFansaHTammerMSchneiderWAggressive digital papillary adenocarcinoma – case reportHandchir Mikrochir Plast Chir2002342137139 German12073193
- DukeWHSherrodTTLuptonGPAggressive digital papillary adenocarcinoma (aggressive digital papillary adenoma and adenocarcinoma revisited)Am J Surg Pathol200024677578410843279
- FreyJShimekCWoodmanseeCAggressive digital papillary adenocarcinoma: a report of two diseases and review of the literatureJ Am Acad Dermatol200960233133918819728
- GoleGNTatiSYDeshpandeAKGoleSGAggressive digital papillary adenocarcinoma in a young female – a rare presentationJ Hand Microsurg201131313322654416
- HornerCWSpellerAMcBrideTDiasRRare digital tumours: two case reports and mini reviewHand Surg201217226727022745098
- HsuHCHoCYChenCHYangCHHongHSChuangYHAggressive digital papillary adenocarcinoma: a reviewClin Exp Dermatol201035211311919874325
- KaoGFHelwigEBGrahamJHAggressive digital papillary adenoma and adenocarcinoma. A clinicopathological study of 57 patients, with histochemical, immunopathological, and ultrastructural observationsJ Cutan Pathol19871431291463301927
- KeramidasEGMillerGRevelosKKitsantaPPageREAggressive digital papillary adenoma-adenocarcinomaScand J Plast Reconstr Surg Hand Surg200640318919216687341
- RuttenARequenaLSweat gland carcinomas of the skinHautarzt2008592151160 German18214401
- JihDMElenitsasRVittorioCCBerkowitzARSeykoraJTAggressive digital papillary adenocarcinoma: a case report and review of the literatureAm J Dermatopathol200123215415711285414
- SuchakRWangWLPrietoVGCutaneous digital papillary adenocarcinoma: a clinicopathologic study of 31 cases of a rare neoplasm with new observationsAm J Surg Pathol201236121883189123026931
- SinglaAKShearinJCAggressive surgical treatment of digital papillary adenocarcinomaPlast Reconstr Surg1997997205820609180731
- MoritaRHattaNShirasakiFHayakawaIOhishiNTakeharaKLymphatic mapping and sentinel lymph node biopsy for staging of aggressive digital papillary adenocarcinomaPlast Reconstr Surg2006117271071216462393