Abstract
Background
3,4,5-Trihydroxybenzoic acid glucoside (THBG), a molecule produced by an original biocatalysis-based technology, was assessed in this study with respect to its skin photoprotective capacity and its skin color control property on Asian-type skin at a clinical level and on skin explant culture models.
Methods
The double-blinded clinical study was done in comparison to a vehicle by the determination of objective color parameters thanks to recognized quantitative and qualitative analysis tools, including Chroma-Meter, VISIA-CR™, and SIAscope™. Determination of L* (brightness), a* and b* (green–red and blue–yellow chromaticity coordinates), individual typology angle, and C* (chroma) and h* (hue angle) parameters using a Chroma-Meter demonstrated that THBG is able to modify skin color while quantification of ultraviolet (UV) spots by VISIA-CR™ confirmed its photoprotective effect. The mechanism of action of THBG molecule was determined using explant skin culture model coupled to histological analysis (epidermis melanin content staining).
Results
We have demonstrated that THBG was able to modulate significantly several critical parameters involved in skin color control such as L* (brightness), a* (redness), individual typology angle (pigmentation), and hue angle (yellowness in this study), whereas no modification occurs on b* and C* parameters. We have demonstrated using histological staining that THBG decrease epidermis melanin content under unirradiated and irradiated condition. We also confirmed that THBG molecule is not a sunscreen agent.
Conclusion
This study demonstrated that THBG controls skin tone via the inhibition of melanin synthesis as well as the modulation of skin brightness, yellowness, and redness.
Introduction
The diversity of human skin color is a result of a combination of specific skin chromophores.Citation1 The red-colored skin chromophore is represented by oxyhemoglobin, blue by deoxygenated hemoglobin, yellow–orange by carotene (an exogenous pigment), and brown by melanin. Nevertheless, melanin is the major chromophore which influences the skin color. Based on this pigmentation variability, the need of an objective quantification of skin color independent of ethnicity was raised in the cosmetic research field. Chroma-Meter tool using the Commission Internationale de l’Eclairage (CIE) L*a*b* system was widely used to assess and compare color in industrial applications such as food industryCitation2 and medicalCitation3 and cosmetic fields.Citation4 In the CIE L*a*b* system, each color is described by a combination of three coordinates L*, a*, and b*. L* describes skin brightness or lightness (and at the opposite, darkness), a* describes a color ranging from green (negative value) to red (positive value), and b* describes a color ranging from blue (negative value) to yellow (positive value). But, often this tool was misused because color parameters L*, a*, and b* obtained from CIE L*a*b* are not sufficient to fully qualify a color.Citation5 In fact, robust qualification and evaluation of color modification are obtained from the L*C*h system. In the L*C*h system, a* and b* are converted into two polar coordinates (C* and hue angle). L* indicates lightness and is the same as the lightness scale L* of the CIE L*a*b* system. C* is a measure of intensity or saturation of the color, and hue angle parameter is a measure of color shading or basic color.Citation6 Individual typology angle (ITA°) is also calculated from the CIE L*a*b* system and qualifies the skin tones from dark to fair.Citation7 provides a summary of these different parameters and their interpretations.
Table 1 Summary of the different parameters related to color assessment
In this research work, we decided to assess the effect of the molecule 3,4,5-trihydroxybenzoic acid glucoside (THBG) on skin color using only objectives tools by a determination after 3 months of daily treatments of the parameters L*, a*, b*, and then C*, hue, and ITA°. Finally, to evaluate the protective effect of THBG against ultraviolet (UV), we used the VISIA-CR™ tool to quantify the number of UV spots. Macrophotographies obtained from VISIA-CR™ also allowed visualizing the improvement of skin redness and brightness.
Materials and methods
Description of the ingredient and creams used
Ingredient (International nomenclature for cosmetic ingredient [INCI])
The ingredient used for active cream preparation was THBG with the following INCI composition: water, glycerin, and diglucosyl gallic acid (reference: Brightenyl, batch number 34144, Induchem AG, Volkestwil, Switzerland). The production process is described in EP2027279 B1.
Vehicle cream composition (INCI)
The vehicle cream was composed of aqua, Alcohol Denat., glycerin, Glyceryl Stearate SE, Simmondsia chinensis seed oil, cetearyl alcohol, palmitic acid, stearic acid, tocopherol, Helianthus annuus seed oil, and perfume.
Active cream containing THBG composition (INCI)
The active cream contained the following composition: aqua, Alcohol Denat., glycerin, Glyceryl Stearate SE, S. chinensis seed oil, cetearyl alcohol, palmitic acid, stearic acid, tocopherol, H. annuus seed oil, perfume, and +2% THBG.
Both applied products (vehicle cream and active cream) get the same, white color, so there is no visible difference between them allowing a double-blind study.
Description of the panel and study condition
A double-blind and vehicle-controlled clinical evaluation was carried out under a dermatologist control with 20 Korean women (age between 30 and 60 years, mean age 46±7 years) showing clinical signs of hyperpigmentation (face spots) and redness. The recommendations of the Declaration of Helsinki and the guidelines of the International Conference on Harmonization Good Clinical Practice were observed as applicable to a non-drug study. All volunteers provided written and informed consent and also approved the use of the pictures in this study.
The volunteers applied either a vehicle cream on one side of their face or a cream containing 2% THBG, twice a day.
The evolution of skin pigmentation was evaluated at days 14, 28, 56, and 84.
This study was carried out around Paris (France) from October 15th to December 10th. The following minimum and maximum temperatures were recorded on D0 (+9.6°C, +28.3°C), D14 and D28 (+8°C, +25°C), D56 (+3.9°C, +21.4°C), and D84 (+0.7°C, +8.2°C). Volunteers were submitted during the study to approximately 416 hours of sun exposure (METEO FRANCE). The INTERSUN Programme publishes the UV index of Paris, France. The UV index is a 1–10 scale, with 10 being the highest UV radiation level. In October, November and December, 2014, the Paris UV index was 2, 1, and 0.
Volunteers were asked not to use sunscreen cream protection during the period of study. All the biometrological measurements were taken in a controlled-atmosphere room (22°C±2°C) after stabilization of the volunteers for at least 10 minutes.
Chroma-Meter analysis: L*, a*, C*, hue, and ITA° parameters
The measure of the skin color intensity was conducted by the colorimetric method performed with a Chroma-Meter (CM 2600d™ KONICA MINOLTA, Toulouse, France). This instrument is a reflectance spectrophotometer that measures reflected light in the visible spectrum (range: 400–700 nm) and is also a tri-stimulus recording colors in a three-dimensional space known as CIE 1976 L*a*b* color space. Chroma-Meter is a portable spectrophotometer with a measurement sensor surface of 1 cm2. The sensor is applied on the face skin surface for 3 seconds. The following skin color parameters were measured and/or calculated: L*, a*, b*, ITA°, hue angle, and C*. Three repeated measures were carried out on the dark spot on each volunteer at all time points. Only the average is taken into account.
SIAscope™ analysis
The SIAscope V, a digital epiluminescence microscopy system designed for taking shadow-free magnified images of skin, was used. It is generally used to measure and image the amount of melanin present in the epidermal layer of skin. The instrument consists of a handheld probe containing light sources and a digital imaging sensor. Two measures were carried out on the dark spot on each volunteer at all time points. Only the average was taken into account for each volunteer. The results were expressed in arbitrary units.
VISIA-CR™ analysis
VISIA-CR™ Facial Complexion Analysis System (Canfield Scientific Inc., Fairfield, NJ, USA) was used to quantify UV spots on the hemi-face at each study time (D0, D14, D28, D56, and D84) on UV photographs obtained by placing glass UV filters in front of the light source. VISIA-CR™ detects stains through the selective absorption of UV light by the epidermal melanin. For each UV photograph, spots were defined as areas of skin meeting a threshold level of color contrast to adjacent skin. The VISIA-CR™ software then calculates UV scores quantifying the percent area of the face comprising the spots in each of the photographs. The results were retrieved as absolute scores. The photographs of UV spots make the sun damage immediately apparent before it is otherwise discernible. UV spots happen when melanin coagulates below the surface of the skin because of the sun exposure. UV spots are invisible under normal lighting and to the naked eye.Citation8 One measure was done on each volunteer for each formula tested at all study times. Only the average from all volunteers was taken into account. A specific color chart purchased from Newtone Technologies (Lyon, France) based on 48 individual colors was also used with the VISIA-CR™ tool to identify potential colorimetric deviation between images.
SPF determination and absorption spectrum product determination studies
Determination of the sun protection factor (SPF) was done by the spectrophotometric method initially described by Diffey and Robson,Citation9 then modified and improved, in view of the evaluation of the protection of the product against effects of ultraviolet B and ultraviolet A on the skin. This method is largely used and recognized internationally. KONTRON 930 spectrophotometer equipped with a UV source and a monochromator and capable of delivering a flow of energy between 290 and 400 nm was used. Products are displayed on PMMA PLATES “Sunplate HD6”.
Lightening mechanism of action assessment study
Explants preparation, treatment, culture, and sampling
Full-thickness skin explants of an average diameter of 11 mm were prepared from an abdominal plasty coming from a 43-year-old healthy female donor of Caucasian origin and with a phototype III to IV. The study was performed in accordance with the Declaration of Helsinki after the patients had given informed consent.
The explants were kept in survival in BIO-EC’s explants medium at 37°C in a humid, 5%-CO2 atmosphere. A cream containing THBG at 2% or kojic acid at 1% (Sigma-Aldrich, St Louis, MO, USA, reference K3125, batch 036K2502) was topically applied on the basis of 2 mg/cm2 using a small spatula on day 0 (D0), D1, D2, D3, D5, D7, D8, and D9. Kojic acid was used as a positive control since this molecule is well known to induce a whitening effect. The skin-whitening effect of the product was studied under two conditions: on UV-irradiated and on unirradiated skin sample. The tested products were applied 30 minutes before the irradiation. Explants exposed to UV were irradiated with a dose of 1.125 J/cm2 ultraviolet A, containing 6%–8% of ultraviolet B using a Vilbert Lourmat UV simulator RMX 3W on D0, D1, D2, D3, D5, D7, D8, and D9. Untreated skin explants were kept in the dark. On D0 and D10, explants were immediately collected and fixed in buffered formol solution for 24 hours. Each condition was done in triplicate.
Histological processing and optical microscopy study
After fixation for 24 hours in buffered formol solution, skin samples were dehydrated and impregnated in paraffin using a Leica TP 1010 dehydration automat (Leica, Rueil-Malmaison, France). The samples were then embedded using a Leica EG 1160 embedding station. Using a Leica RM 2125 Minot-type microtome, 5 µm thick sections were realized, and the sections were then mounted on Superfrost® Plus silanized glass slides. The microscopical observations were realized using an Olympus BX43 microscope equipped with a CCD DXC 390 Sony camera. Pictures were digitized with an Olympus DP72 camera and Cell^D data storing software.
Melanin visualization has been realized by silver impregnation according to Fontana Masson’s staining protocol.
Data analysis and statistical analysis
The mean and standard deviation were calculated for each parameter measured at all time points. Then, the calculation of percentage variation compared to the initial measurement allowed the assessment of the overall effect of the product studied in comparison to the vehicle cream. Statistical analysis of the data was performed using Student’s t-test for paired data. The statistic significances are reported as follows: “ns” for non-significant (P>0.05) and “s” for significant (P≤0.05).
Results
Chroma-Meter analysis
illustrates the results obtained for placebo and THBG. We noticed that placebo did not modify skin color parameters (L*, a*, b*, C*, hue angle, and ITA°). In contrast to the vehicle cream, THBG-containing cream demonstrated a statistically significant effect on all skin color parameters (L*, a*, hue angle, and ITA°), with the exception of b* and C* parameters. The presence of THBG increased L* parameter from D28 (+0.9%) to D84 (+2.2%) demonstrating a lightening effect on the skin. The effect seen was time dependent.
Table 2 Color parameters recorded (L*, a*, b*) or calculated (chroma C*, hue angle, and ITA°) from a Chroma-Meter applied on the face skin of 20 volunteers before and after 14, 28, 56, and 84 days of vehicle cream or THBG cream application
THBG decreased a* parameter after 28 days of use (–12.9%). The effect seen was maintained after 56 days (–7.3%) and 84 days (–7%) of use demonstrating an anti-redness effect on the skin.
THBG cream increased the hue angle parameter after 28 days (+5.1%), 56 days (+4%), and 84 days (+4.6%) demonstrating a distance from the initial yellow color of the volunteer face.
THBG cream significantly increased the ITA° parameter after 56 days (+10.4%) and 84 days of use (+11.5%), corresponding to a skin-lightening effect. The effect was time dependent (ITA° parameter increased from D14 to D84).
SIAscope analysis
Melanin content quantification
THBG cream induced a significant decrease of skin melanin content from 4% to 7.5% from 14 to 84 days of daily use. The placebo treatment also induced a significant decrease in melanin content by approximately 3% from D28 to D84. The effect seen was better and stronger with the THBG cream treatment than with vehicle cream. In comparison to placebo, a significant decrease of melanin content by +150% was quantified after 84 days of THBG treatment ().
Table 3 Melanin content quantification by SIAscope™ applied on the face skin of 20 volunteers at the beginning of the study (D0) and after 14, 28, 56, and 84 days of vehicle and THBG treatment
Melanin content visualization
illustrates melanin content pictures obtained from SIAscope™ equipment.
Figure 1 Melanin content visualization at D0 and after 14, 28, 56, and 84 days of placebo and THBG treatments (SIAscope™ tool, selection of two volunteers).
Abbreviations: THBG, 3,4,5-trihydroxybenzoic acid glucoside; n°, number; D, day.
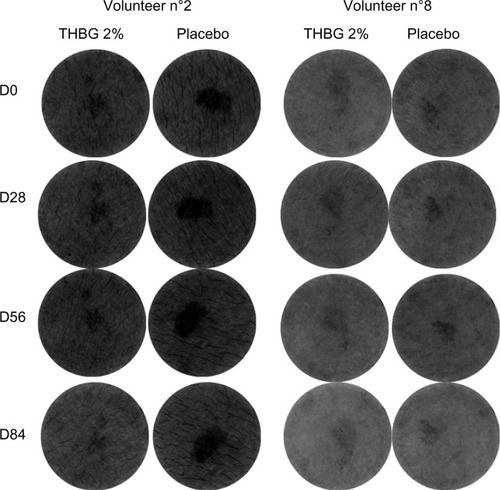
THBG induced a decrease of the melanin content on the spot and non-spot areas. These results demonstrate that THBG has an anti-melanogenesis effect. The vehicle cream treatment did not modify or only slightly modified melanin content in epidermis as illustrated in and .
VISIA-CR™ analysis
UV spots quantification and visualization
The vehicle cream treatment showed a significant increase in UV spots quantity after 84 days of use (+9.3%). In contrast, the use of the cream containing THBG reduced significantly (or nearly significantly) (–7%) the quantity of UV spots after 28, 56, and 84 days of daily use. In comparison to placebo and after 84 days, the quantity of UV spots recorded after THBG treatment was reduced significantly by 18-fold ( and ).
Figure 2 Macrophotographies taken under visible or UV light from one volunteer before and after vehicle cream or THBG cream application for 84 days.
Abbreviations: UV, ultraviolet; THBG, 3,4,5-trihydroxybenzoic acid glucoside; D, day.

Table 4 UV spots parameters quantification
Skin redness and skin brightness improvement
is an illustration of the results obtained on three representative volunteers after the application of THBG and vehicle creams. The application of the cream containing THBG induced an improvement of skin redness. Indeed, volunteer 1 at the beginning of the study (D0) got a red halo on both the hemi-faces. After 84 days of THBG treatment, we recorded a strong decrease of this halo. Moreover, volunteers 2 and 3 showed a strong redness at the beginning of the study on their noses (alar area). After 84 days of twice-daily use of THBG, the redness was strongly decreased. The hemi-faces treated with vehicle cream did not show any improvement of skin redness in this specific area. On these same pictures, we confirmed the brightening effect of THBG.
Figure 3 Macrophotographies taken using visible light from three volunteers before and after vehicle cream or THBG cream application for 84 days.
Abbreviations: THBG, 3,4,5-trihydroxybenzoic acid glucoside; D, day.

Absorption spectra and SPF determination of THBG molecule
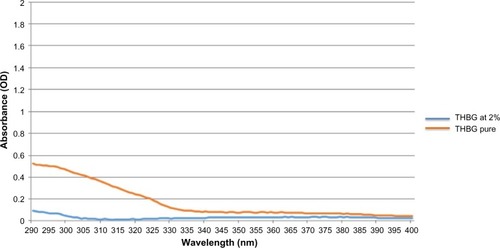
THBG diluted at 2% has no filter effect as no absorption was observed. The pure product THBG absorbs a little in the ultraviolet B (). The SPF value calculated for THBG pure and THBG diluted at 2% was 2.1 and 1.1, respectively. The product THBG is not a sunscreen agent.
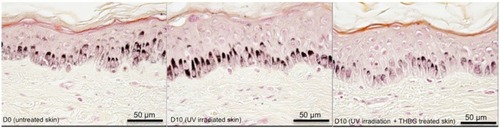
Melanin content visualization
Kojic acid topically applied on skin explants showed a decrease in epidermis melanin content (); this effect was not surprising as kojic acid is a known whitening agent. As expected, UV irradiation applied on skin stimulates melanin synthesis. This result validates the study model (). THBG cream induced a strong and visible decrease of epidermis melanin content under unirradiated () and irradiated conditions ().
Discussion
Most of cosmetics studies related to characterization of skin color after application of active cosmetics focus only on skin pigmentation modifications based either on self-assessmentCitation10 and/or assessment by a trained technician using grading scales.Citation11 In our study, we used a well-recognized objective tool, the Chroma-Meter, to assess skin color (not only skin pigmentation) by a determination of its brightness (L*), saturation (chroma C*), and hue angle (basic color) values. We noticed in this study that THBG modifies skin color by increasing its brightness (L*) and its basic color (hue angle) but has no effect on its saturation (C*). The results are consistent with those of Brenner et alCitation12 showing a direct correlation between L* and hue angle. But, we do not confirm their results showing a correlation between L* and the chroma component C*. Li-Tsang et alCitation13 have shown that skin color modification in scars implies modification of all parameters at the exception of C*. These data are consistent with our results. Then, we combined to this tool a complementary equipment SIAscope™ to determine if the skin color modification detected was also related to melanin content, the major pigment involved in skin color. In this study, we have shown that THBG decreases melanin content in epidermis, so we could assume that the skin color modification determined by Chroma-Meter is in part due to melanin content fluctuation. With vehicle cream we have recorded a decrease in melanin content; this effect could be considered as negligible because it is not correlated to a modification of skin color. This slight decrease of melanin content seen with placebo is indeed due to the massage effect that occurs during application of the cream. It is known that massaging stimulates the epidermis renewal leading to a decrease in melanin content.Citation14
An interesting finding was highlighted in our study by the quantification of UV spots as we observed maintenance of skin protection against UV damage. UV spots are a recognized measure of sun damage by dermatologists.Citation8,Citation15 Indeed, UV spots obtained from UV photographs reveal existing skin damage (melanin alteration) not yet perceptible by eye. The study was done without the use of sunscreen creams, and as recorded by INTERSUN Programme, the volunteer’s skins were exposed to low UV ray radiation on October 2014 (index 2) and November (index 1). Even this exposition to UV radiation was low; it could induce the increased number of UV spots (+9.3% in comparison to D0) recorded in the placebo group. UV spots appear when melanin coagulates below the skin surface as a result of sun damage and appears under the aspect of a mottle skin pigmentation non-visible under normal lightening. This non-visible mottled pigmentation will lead later to visible dark spots, contributing to uneven skin tone and in some cases to melanomas.Citation15 In contrast, half the face treated with THBG got fewer UV spots at the end of the study. This result is not due to a potential filter effect of THBG molecule, as THBG at 2% does not absorb UV light, and its SPF calculated was negligible.
Actives molecules used in cosmetics to modify skin color are often whitening agents orallyCitation16 or topically applied.Citation17 Agents topically applied include hydroquinone and hydroquinone derivatives such as arbutin,Citation18 tretinoin,Citation19 kojic acid, azelaic acid, vitamin C, fruit or plant extracts,Citation20 and licorice extract,Citation21 used alone or in combination.Citation22
Even if these whitening agents have shown efficiency as lightening agents, their mode of action described in scientific literature concerns the inhibition of melanogenesis process through an inhibition of enzymes (tyrosinase, tyrosinase related protein 1 …), signaling pathways and transcription factors involved in melanogenesis, or through an anti-inflammatory action.Citation18,Citation23 But, most of them do not really improve the global skin color and skin tone.Citation24,Citation25 To our knowledge and based on literature data analysis on PubMed databases, known cosmetics lightening agents do not offer at the same time skin protection and control of skin color (brightness, redness, yellowness, and brownness) by modulation of L*, a*, hue angle, ITA° parameters, and melanin content of the skin. The modulation of epidermis melanin content was confirmed on skin explants by histological analysis.
Conclusion
This clinical study highlights two intrinsic properties of THBG: UV ray protectant effect and skin color modulation. THBG protects skin against UV rays by a significant decrease of UV spots detection over time. This UV ray protection is not due to a filter effect of the molecule. Skin color modulation property of THBG is shown by the modifications of skin brightness, redness, yellowness, and brownness. The modulation of the skin color is in part due to its anti-melanogenesis properties demonstrated by the decrease of skin melanin content and most probably by an anti-inflammatory property of THBG leading to a decrease of skin redness (data under submission).
Acknowledgments
The authors would like to thank Magalie Daniel and Dr Elian Lati (Laboratoire Bio-EC, Longjumeau, France) for clinical and ex vivo study management. The authors also thank Dr Jean Claude Hubaud (Helioscience, Marseille, France) for UV spectrum determination and SPF analysis.
Disclosure
The authors report no conflicts of interest in this work.
References
- KolliasNThe physical basis of skin color and its evaluationClin Dermatol19951343613678665444
- RuizDEgeaJTomas-BarberanFAGilMICarotenoids from new apricot (Prunus armeniaca L.) varieties and their relationship with flesh and skin colorJ Agric Food Chem200553166368637416076120
- RahDKKimSCLeeKHParkBYKimDWObjective evaluation of treatment effects on port-wine stains using L*a*b* color coordinatesPlast Reconstr Surg2001108484284711547137
- ChardonACretoisIHourseauCSkin colour typology and suntanning pathwaysInt J Cosmet Sci199113419120819291061
- TakiwakiHMeasurement of skin color: practical application and theoretical considerationsJ Med Invest1998443–41211269597799
- Saint-LegerDThe colour of the human skin: fruitful science, unsuitable wordingsInt J Cosmet Sci201537325926525533569
- HuixiaQXiaohuiLChengdaYInstrumental and clinical studies of the facial skin tone and pigmentation of Shanghaiese women. Changes induced by age and a cosmetic whitening productInt J Cosmet Sci2012341495421848763
- FultonJEJrUtilizing the ultraviolet (UV detect) camera to enhance the appearance of photodamage and other skin conditionsDermatol Surg19972331631699145957
- DiffeyBLRobsonJA new substrate to measure sunscreen protection factors throughout the ultra violet spectrumJSCC198940127133
- SiglerMLStephensTJAssessment of the safety and efficacy of topical copper chlorophyllin in women with photodamaged facial skinJ Drugs Dermatol201514440140425844615
- FabiSMassakiNGoldmanMPEfficacy and tolerability of two commercial hyperpigmentation kits in the treatment of facial hyperpigmentation and photo-agingJ Drugs Dermatol201211896496822859242
- BrennerAVInstrumental measurements of skin color and skin ultraviolet light sensitivity and risk of cutaneous malignant melanoma: a case-control study in an Italian populationAm J Epidemiol2002156435336212181106
- Li-TsangCWLauJCLiuSKValidation of an objective scar pigmentation measurement by using a spectrocolorimeterBurns200329877978414636751
- Li-TsangCWLauJCChoiJChanCCJiananLA prospective randomized clinical trial to investigate the effect of silicone gel sheeting (Cica-Care) on post-traumatic hypertrophic scar among the Chinese populationBurns200632667868316837136
- GambleRGAsdigianNLAalborgJSun damage in ultraviolet photographs correlates with phenotypic melanoma risk factors in 12-year-old childrenJ Am Acad Dermatol201267458759722406230
- WuSShiHWuHTreatment of melasma with oral administration of tranexamic acidAesthetic Plast Surg201236496497022552446
- AlexisAFNew and emerging treatments for hyperpigmentationJ Drugs Dermatol201413438238524719055
- ThornfeldtCRizerRLTrookmanNSBlockade of melanin synthesis, activation and distribution pathway by a nonprescription natural regimen is equally effective to a multiple prescription-based therapeutic regimenJ Drugs Dermatol201312121449145424301247
- KuritaMKatoHYoshimuraKA therapeutic strategy based on histological assessment of hyperpigmented skin lesions in AsiansJ Plast Reconstr Aesthet Surg200962795596318456589
- KhanBAAkhtarNHussainIAbbasKARasulAWhitening efficacy of plant extracts including Hippophae rhamnoides and Cassia fistula extracts on the skin of Asian patients with melasmaPostepy Dermatol Alergol201330422623224278079
- LeydenJJShergillBMicaliGDownieJWalloWNatural options for the management of hyperpigmentationJ Eur Acad Dermatol Venereol201125101140114521623927
- MomosawaAKuritaMOzakiMCombined therapy using Q-switched ruby laser and bleaching treatment with tretinoin and hydroquinone for periorbital skin hyperpigmentation in AsiansPlast Reconstr Surg2008121128228818176232
- KimKEffect of ginseng and ginsenosides on melanogenesis and their mechanism of actionJ Ginseng Res20153911625535470
- LeeAYNohMThe regulation of epidermal melanogenesis via cAMP and/or PKC signaling pathways: insights for the development of hypopigmenting agentsArch Pharm Res201336779280123604723
- Woolery-LloydHKammerJNTreatment of hyperpigmentationSemin Cutan Med Surg201130317117521925372