Abstract
Ectodermal dysplasia (EDD) is a developmental disorder that affects the skin, hair, and teeth among other organs generated in the ectoderm. Dental implants have been used to successfully treat partial edentulism in EDD patients, but the success rate is much lower for these patients. The report herein is a successful case of a single mini, small diameter, implant used to support a single crown of a mandibular right second premolar. A review of implant treatment in EDD patients is included.
Introduction
Dental implants can be used to successfully restore partial and complete edentulism. There are patients who present with systemic disorders that may affect outcomes. Ectodermal dysplasia (EDD) is one of these.Citation1,Citation2 There have been reports on successful dental implant treatment in patients with EDD, but the success rate is much lower for EDD patients.Citation3,Citation4 This is a case report of a successful single crown supported by a small diameter, mini, implant in a patient with EDD.
EDD
EDD is a large group of disorders with developmental abnormalities in ectodermal structures that include skin, hair, nails, teeth, and glands.Citation1,Citation2 Among a variety of signs and symptoms of EDD are dry hypoplastic skin, sparse scalp and body hair, dystrophic fingernails, deficient sweat glands, and oligodontia.Citation1,Citation2 These patients exhibit two or more affected structures that develop from ectoderm.Citation1,Citation2 Teeth affected by EDD is one of the criteria for distinguishing between affected and unaffected individuals in a clinical examination. There are over 120 syndromes in which oligodontia is one of the associated findings.Citation4,Citation5 The majority of these are hereditary. The most commonly associated with missing teeth are Down syndrome and EDD.Citation6 Oligodontia is defined as the absence of more than six teeth, excluding third molars.Citation2,Citation6–Citation9 There are more than 200 types of EDD, but the causative gene is known in only 60 types.Citation7–Citation9 This disorder has an incidence of 1:100,000 births and is more common among boys.Citation1,Citation2,Citation7–Citation9 The phenotypical outcome is the result of an autosomal dominant, autosomal recessive, or X-linked genetic expression.Citation9–Citation13 The most common form is the X-linked, hypohidrotic form and constitutes about 80% of those affected.Citation14–Citation16 Edentulous sites are often hypoplastic with sharp narrow atrophic ridges.Citation17,Citation18 Early diagnosis of EDD is essential for appropriate treatment. To address all aspects of EDD, multidisciplinary treatment planning may be important from childhood to adulthood.Citation19–Citation26
Dental implant treatment of patients with EDD
The dentition and smile are crucial for the oral function and overall facial esthetics.Citation27,Citation28 Generally, patients desire dental treatment for functional and esthetic reasons. Oral rehabilitation of EDD patients in the past has involved partial or complete removable prostheses supported by tissue or teeth. Dental implant-supported prostheses has provided an additional treatment option for these patients.Citation29
Wong et al studied the oral health and related quality of life (QL) in patients with EDD.Citation25 They targeted young individuals aged 11–15 years. These patients lacked a mean of 8.9 teeth and reported this to have a considerable QL impact. The majority (88%) reported functional limitations and emotional well-being issues.Citation25 Locker et al studied QL in 36 Canadian children who were missing a mean of 6.8 teeth; 75% reported functional and psychosocial impacts “often” or “every day/almost every day”.Citation26
Small diameter implants (SDIs) can be considered for the retention of removable dentures and the support of fixed prostheses especially in narrow ridges. Patients treated with SDIs for removable prosthetic retention had more satisfaction with their rehabilitation than those treated with conventional nonimplant-supported prostheses.Citation30 The treating clinicians reported better retention, masticatory efficiency, and comfort with a positive impact on their QL.Citation30
Some reports in literature described the use of mini implants for prosthetic rehabilitation of children and in children affected by EDD.Citation31–Citation33 The early insertion of dental implants is recommended in children with severe hypodontia.Citation34,Citation35 Buser et al at an International Team of Oral Implantology Consensus Conference 2000 described EDD as a condition which may affect oral tissues by increasing their susceptibility to other diseases by interfering with healing and increasing the risk of implant failure.Citation36 Guckes et al, in a prospective study done on 51 patients with EDD, aged 8–68 years, placed implants in anterior mandibles and anterior maxilla.Citation37 The implant survival rates were 91% in the mandible and 76% in the maxilla.Citation37 A literature review by Yap and Klineberg concluded that implant survival rates vary between 88.5% and 97.6% in patients with EDD and between 90% and 100% in patients with tooth agenesis.Citation38 Implants placed in adolescents with EDD do not have a significant effect on craniofacial growth, but there is a higher risk of implant failure.Citation38,Citation39
Case report
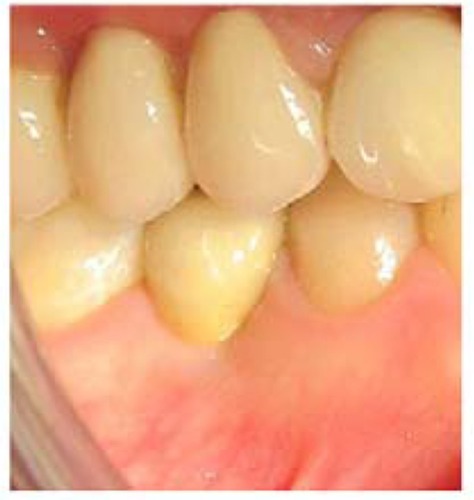
A 20-year-old female affected by EDD presented with a chief complaint of a painful, mobile, and carious mandibular right second deciduous molar. Extraoral examination revealed hypotonicity of the perioral musculature. Her hair was thin and sparse. Her skin was dry, prone to rashes and easily sunburned. A medical consultation was made but no genetic testing was obtained on this patient, so a specific diagnosis type could not be made. The oral examination disclosed carious deciduous teeth and oligodontia (–). On the right side, missing permanent teeth were the maxillary second and third molars, second premolar, central and lateral incisors, left premolars, and second and third molars. In the mandible missing teeth were the right third molar, second premolar, left third molar and second premolar, and central incisors. Eleven teeth were absent from agenesis. The mandibular incisors were incompletely developed (). Multiple carious deciduous teeth were deemed hopeless ( and ). After a discussion and informed consent was obtained from the patient to have the case details and any accompanying images published, implant treatment was decided upon.
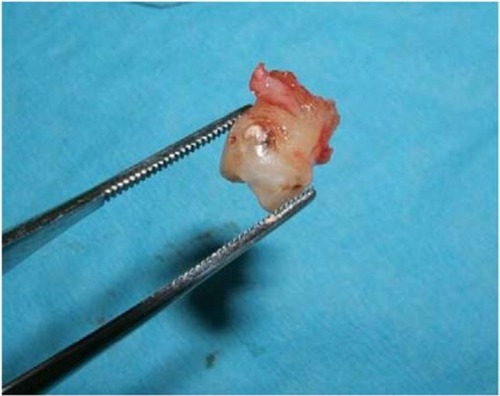
First, carious deciduous teeth were extracted, the maxillary lateral incisors, and right second molar and left first molar and the mandibular right second molar (). The maxillary right first premolar was extracted due to coronal caries and radicular malformation. The mandibular left first premolar had a malformed root but was left in place. The mandibular second premolar was absent due to agenesis. The overlying deciduous second molar was slightly submerged. Orthodontic treatment was then instituted over a 7-year period at the Department of Orthodontics, University of Genoa, Italy, without complications ( and ).
A maxillary 12 unit all-ceramic fixed partial denture, from first molar to first molar, was fabricated. This was supported by the first molars and cuspids. Preemptive cuspid endodontics were needed due to large pulp chambers. Endodontic therapy was performed on the maxillary left first molar due to occlusal caries. Implants were not considered because of the high failure rate in EDD patients. Additionally, SDIs may not perform well in the maxilla due to probable low bone density and off-axial loading from the mandibular incisors.
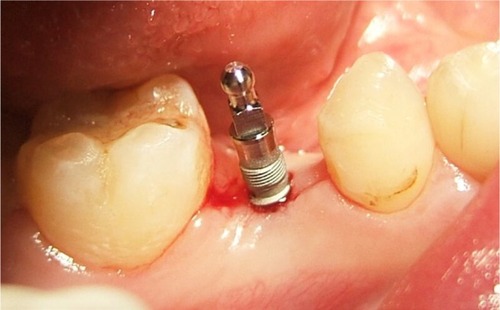
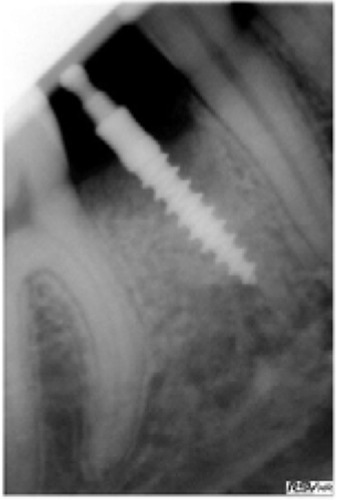
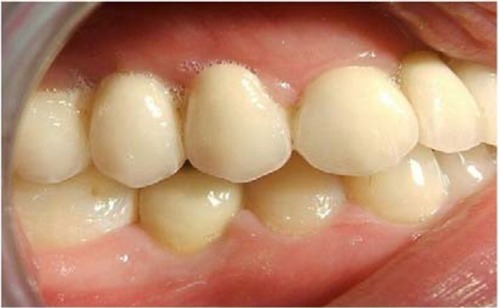
The mandibular right second premolar site had healed well (). This implant was planned to be placed flaplessly. A 2.5×13 mm SDI (MDL Intra-Lock International®, Boca Raton, FL, USA) was selected and placed according to SDI guidelines.Citation48 An osteotomy was performed with a 1.2 mm drill sited equidistantly between the premolar and first molar and the center of the ridge crest. During osteotomy, a qualitative assessment of type 3 bone was made. The implant was then seated at 12 rpm and water cooled to prevent any significant insertion heat (–). An impression was done at insertion appointment and fabricated during the osseointegration time. After 3 months, a low cusp ceramic crown was inserted, assessed, and definitively cemented with Cement-Over™ Abutment (Intra-Lock International) ( and ). The crown has been in uneventful successful function for 4 years ().
Discussion
EDD is a rare genetic disorder that is usually transmitted as an X-linked recessive trait.Citation40 Ninety-five percent of patients with EDD have the X-linked form.Citation40 Because of subtle manifestations, EDD is difficult to diagnose. The number of teeth that develop are a basis of diagnosis. Hypodontia, anodontia, and dental malformations are part of the disorder. Because the teeth give the alveolar ridges osseous stimulation, absence of teeth results in narrow atrophic edentulous ridges that make poor support for removable dentures.Citation40 Thus, endosseous implants can provide support and retention for effective function of fixed or removable prostheses.Citation40 However, endosseous dental implants should not be placed until skeletal growth is complete.Citation40 The implants may stabilize and maintain the osseous ridges.Citation40 The goal of treatment is to improve function and provide an esthetic outcome.Citation40 Poor alveolar development, a larger number of missing teeth, and the morphology and position of the teeth that did develop complicate the management of treatment.Citation40
Patients with hypodontia are frequently treated with complete or partial conventional removable prostheses.Citation41,Citation42 In the case described herein, a small diameter implant was selected because of its small displacement. A small physical displacement may be beneficial, in that the implant has a substantial supporting bone volume for remodeling. In case of a failure, there would be less osseous resorption and more remaining bone for a revision. Nonetheless, SDIs exert more osseous load than standard implants.Citation43–Citation45 Load attenuation needs to be addressed by an occlusal scheme that minimizes off-axial forces.Citation43,Citation44 Additionally, assessing the patients’ load generating capability may be an important parameter to assess the risk of overload.Citation43–Citation45 An excessive jaw force capability may indicate a larger diameter implant to exert less per-square-mm load on the supporting bone.Citation43–Citation45 Although no bite force assessment was made, the qualitative load assessment was deemed to be of low magnitude. After functional loading, the implant showed no marginal bone loss with apparent appropriate bone remodeling at a 4-year follow-up (–).
When there is alveolar ridge resorption, the facial cortex approaches the lingual cortex and narrows the residual ridge.Citation43 There is less medullary bone as compared to dense cortical bone. This may enable better support for SDIs because the implant then engages the dense cortical bone throughout its complete length. The dense cortical bone is highly resistant to occlusal loads that are delivered to the bone.Citation43
Bergendal demonstrated a 64.3% implant failure in patients with EDD.Citation23 Nonetheless, other reports showed that dental implants can be used successfully in partially and completely edentulous patients affected by congenital disorders, such as EDD.Citation31–Citation33 Thus, children and adults with EDD may be treated with SDIs in atrophic ridges due to the residual cortices.
Oral prostheses supported by implants provide comfortable function and psychological benefits for children with EDD.Citation40 Sfeir et al affirmed that mini implants can be a part of dental treatment for EDD patients and that their use reduces the number of surgeries.Citation33
Literature reports indicate that different cusp inclinations can have a significant effect on bone remodeling responses in terms of bone density and osseous stability.Citation46 A higher cusp inclination can lead to a higher bone remodeling rate and greater bone–implant interfacial stress.Citation46 Degidi et al found functional loading to stimulate bone remodeling at the bone–implant interface.Citation48 A high percentage of lamellar bone was found in loaded implants.Citation47
The low SDI volume of displacement may allow appropriate healing by not physically blocking angiogenesis and osteogenesis, as well as subsequent bone remodeling.Citation48,Citation49 Nonetheless, the SDI puts a high load on the embedding bone, and the use of a longer SDI may be required to minimize the risk of osseous overload.Citation43,Citation48,Citation49 A low cusp height in the occlusal scheme may also lessen the risk of overload of an SDI.Citation43,Citation46
Heat may be generated during seating of SDIs, so water coolant may be used to prevent an inordinate temperature increase that may be detrimental to the bone.Citation50 EDD complete edentulism can be successfully treated with CAD-CAM implant-supported overdentures.Citation51 CAD-CAM prosthetic fabrication is a definitive technical advance for accuracy, and occlusal loads may be better controlled.Citation51
The small percutaneous exposure of SDIs may dramatically reduce the incidence of peri-implant mucositis and peri-implantitis.Citation44 No marginal bone loss was seen with this patient in the postoperative 4 years. Implants may not be appropriate in children who have no complete osseous growth due to drifting and displacement of the bones during maturation.Citation45
Conclusions
SDIs may be a minimally invasive approach for support in fixed prosthetics in selected patients with EDD. Preoperative site evaluation and evaluation of the patient’s disorder and an appropriate occlusal scheme that minimizes off-axial loads is required. This is a case report and is of a low credibility level. In the future, a meta-analysis of case reports and case series may elucidate this topic for appropriate treatment of these individuals.
Disclosure
The authors report no conflicts of interest in this work.
References
- SalinasCFJorgensonRJWrightJTDigiovannaJJFeteMD2008 International Conference on Ectodermal Dysplasias Classification: conference reportAm J Med Genet A2009149A91958196919681152
- IrvineADTowards a unified classification of the ectodermal dysplasias: opportunities outweigh challengesAm J Med Genet A2009149A91970197219681131
- WorsaaeNJensenBNHolmBHolskoJTreatment of severe hypodontia-oligodontia--an interdisciplinary conceptInt J Oral Maxillofac Surg200736647348017433622
- TaloTAcun KayaFThe effects of ectodermal dysplasia on periodontal tissuesJ Int Dent Med Res2009225357
- BaniMTezkireciogluAMAkalNTuzunerTEctodermal dysplasia with anodontia: a report of two casesEur J Dent20104221522220396456
- UlmMRKratochwilAUlmBSolarPAroGBernaschekGThree-dimensional ultrasound evaluation of fetal tooth germsUltrasound Obstet Gynecol19981242402439819853
- ItinPHRationale and background as basis for a new classification of the ectodermal dysplasiasAm J Med Genet A2009149A91973197619353583
- VisinoniAFLisboa-CostaTPagnanNAChautard-Freire-MaiaEAEctodermal dysplasias: clinical and molecular reviewAm J Med Genet A2009149A91980200219681154
- BergendalBOligodontia ectodermal dysplasia–on signs, symptoms, genetics, and outcomes of dental treatmentSwed Dent J Suppl201020578
- AydinbelgeMGumusHOSekerciAEDemetoğluUEtozOAImplants in children with hypohidrotic ectodermal dysplasia: an alternative approach to esthetic management: case report and review of the literaturePediatr Dent201335544144624290558
- KereJSrivastavaAKMontonenOX-linked anhidrotic (hypohidrotic) ectodermal dysplasia is caused by mutation in a novel trans-membrane proteinNat Genet19961344094168696334
- ZiadaHHollandTEctodermal dysplasia: a case reportJ Ir Dent Assoc19974341271299584748
- SakaiVTOliveiraTMPessanJPSantosCFMachadoMAAlternative oral rehabilitation of children with hypodontia and conical tooth shape: a clinical reportQuintessence Int200637972573017017635
- HuangCYangQKeTA novel de novo frame-shift mutation of the EDA gene in a Chinese Han family with hypohidrotic ectodermal dysplasiaJ Hum Genet200651121133113717066260
- LexnerMOBardowAHertzJMNielsenLISAKreiborgSAnomalies of tooth formation in hypohidrotic ectodermal dysplasiaInt J Paediatr Dent2007171101817181574
- GruberJKreitzbergGEctodermal dysplasia. A seven-year case reportN Y State Dent J2006726283117203852
- GlavinaDMajstorovicMLulic-DukicOJuricHHypohidrotic ectodermal dysplasia: dental features and carrier detectionColl Anthropol2001251303310
- FreimanABorsukDBarankinBSperberGHKrafchikBDental manifestations of dermatologic conditionsJ Am Acad Dermatol200960228929819027989
- ClaussFManièreMCObryFDento-craniofacial phenotypes and underlying molecular mechanisms in hypohidrotic ectodermal dysplasia (HED): a reviewJ Dent Res200887121089109919029074
- BergendalBBergendalTHallonstenALKochGKurolJKvintSA multidisciplinary approach to oral rehabilitation with osseointegrated implants in children and adolescents with multiple aplasiaEur J Orthod19961821191298670924
- HobsonRSCarterNEGillgrassTJThe interdisciplinary management of hypodontia: the relationship between an interdisciplinary team and the general dental practitionerBr Dent J2003194947948212835777
- KotsiomitiEKassaDKapariDOligodontia and associated characteristics: assessment in view of prosthodontic rehabilitationEur J Prosthodont Restor Dent2007152556017645065
- BergendalBWhen should we extract deciduous teeth and place implants in young individuals with tooth agenesis?J Oral Rehabil200835Suppl 1556318181934
- GotfredsenKCarlssonGEJokstadAImplants and/or teeth: consensus statements and recommendationsJ Oral Rehabil200835Suppl 12818181929
- WongATMcmillanASMcgrathCOral health-related quality of life and severe hypodontiaJ Oral Rehabil2006331286987317168928
- LockerDJokovicAPrakashPTompsonBOral health-related quality of life of children with oligodontiaInt J Paediatr Dent201020181420059588
- SomaniANewtonJTDunneSGilbertDBThe impact of visible dental decay on social judgements: comparison of the effects of location and extent of lesionInt Dent J201060358
- HavensDCMcnamaraJASiglerLMBaccettiTThe role of the posed smile in overall facial estheticsAngle Orthod201080232232819905858
- JohnsonELRobertsMWGuckesADBaileyLJPhillipsCLWrightJTAnalysis of craniofacial development in children with hypohidrotic ectodermal dysplasiaAm J Med Genet2002112432733412376932
- PreoteasaEMarinMImreMLernerHPreoteasaCTPatients’ satisfaction with conventional dentures and mini implant anchored overdenturesRev Med Chir Soc Med Nat Iasi2012116131031623077914
- GülerNCildirSIseriUSandalliNDilekOHypohidrotic ectodermal dysplasia with bilateral impacted teeth at the coronoid process: a case rehabilitated with mini dental implantsOral Surg Oral Med Oral Pathol Oral Radiol Endod2005995E34E3815829868
- GiannettiLMurri dello DiagoAVecciFConsoloUMini-implants in growing patients: a case reportPediatr Dent201032323924420557708
- SfeirENassifNMoukarzelCUse of mini dental implants in ectodermal dysplasia children: follow-up of three casesEur J Paediatr Dent2014152 Suppl20721225101504
- KramerFJBaethgeCTschernitschekHImplants in children with ectodermal dysplasia: a case report and literature reviewClin Oral Implants Res200718114014617224035
- SweeneyIPFergusonJWHeggieAALucasJOTreatment outcomes for adolescent ectodermal dysplasia patients treated with dental implantsInt J Paediatr Dent200515424124816011782
- BuserDvon ArxTTen BruggenkateCWeingartDBasic surgical principles with ITI implantsClin Oral Implants Res200011Suppl5968
- GuckesADScurriaMSKingTSMccarthyGRBrahimJSProspective clinical trial of dental implants in persons with ectodermal dysplasiaJ Prosthet Dent2002881212512239475
- YapAKKlinebergIDental implants in patients with ectodermal dysplasia and tooth agenesis: a critical review of the literatureInt J Prosthodont200922326827619548409
- SingerSLHenryPJLiddelowGRosenbergILong-term follow-up of implant treatment for oligodontia in an actively growing individual: a clinical reportJ Prosthet Dent2012108527928523107235
- KnoblochLALarsenPESaponaroPCL’Homme-LangloisEEarly implant placement for a patient with ectodermal dysplasia: Thirteen years of clinical careJ Prosthet Dent2018119570270929195821
- PaulSTTandonSKiranMProsthetic rehabilitation of a child with induced anodontiaJ Clin Pediatr Dent1995201588634197
- PettitSCampbellPREctrodactyly-ectodermal dysplasia-clefting syndrome: the oral hygiene management of a patient with EECSpec Care Dentist201030625025421044105
- BulutEGulerAUSen TuncETelciogluNTOral rehabilitation with endosseous implants in a child with ectodermal dysplasia: a case reportEur J Paediatr Dent201011314915221080757
- FlanaganDMascoloAThe mini dental implant in fixed and removable prosthetics: a reviewJ Oral Implantol20113712313220553165
- FlanaganDIliesHO’BrienBMcmanusALarrowBJaw bite force measurement deviceJ Oral Implantol201238436136420822470
- FlanaganDBite force and dental implant treatment: a short reviewMed Devices201710141148
- RungsiyakullCRungsiyakullPLiQLiWSwainMEffects of occlusal inclination and loading on mandibular bone remodeling: a finite element studyInt J Oral Maxillofac Implants201126352753721691599
- DegidiMScaranoAPiattelliMPerrottiVPiattelliABone remodeling in immediately loaded and unloaded titanium dental implants: a histologic and histomorphometric study in humansJ Oral Implantol2005311182415751384
- SerraGMoraisLSEliasCNSequential bone healing of immediately loaded mini-implantsAm J Orthod Dentofacial Orthop20081341445218617102
- FlanaganDHeat generated during seating of dental implant fixturesJ Oral Implantol201440217418124400840
- ChrcanovicBRDental implants in patients with ectodermal dysplasia: A systematic reviewJ Cranio Maxilloofac Surg Epub2018521
- AlsayedHDAlqahtaniNMAlzayerYMMortonDLevonJABabaNZProsthodontic rehabilitation with monolithic, multichromatic CAD-CAM complete overdentures in an adolescent patient with ectodermal dysplasia: A clinical reportJ Prosthet Dent2018119687387829150132