Abstract
Medication-related osteonecrosis of the jaw (MRONJ) can be a debilitating complication that can arise in patients who took or are taking antiresorptive (including bisphosphonates) or antiangiogenic agents, leading to visible bone or a fistula that continues for more than eight weeks, without any history of radiotherapy. This clinical case aimed to describe the treatment of MRONJ with topical active oxygen therapy using blue®m oral gel. A 63-year-old female patient that had been taking weekly sodium alendronate (70 mg) for four years by oral via, presented discomfort and implant movement in the #46 region, by that underwent surgical extraction of the implant. After three months the patient returned and was diagnosed with MRONJ. Initially, conventional therapies were performed, including surgical debridement and antibiotic therapy, but without success. The patient still had clinical signs of osteonecrosis six months after the implant extraction. The entire socket was then filled with blue®m oral gel by topical application. The patient was instructed to continue applying the gel to the region every 8 hours for 15 days. After this period, the patient returned, and it was observed that the wound was in the healing process, with the presence of epithelialized tissue and without bone exposure. The 2-year clinical follow-up showed the lesion had healed entirely, and a new implant was installed. After the osseointegration period, the final prosthesis was placed. The patient remains under clinical follow-up. Therefore, it can be concluded that the application of blue®m oral gel in this clinical case assisted in the recovery of the osteonecrosis lesion.
QR Code
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
© 2024 Deliberador et al. This work is published by Dove Medical Press Limited, and licensed under Creative Commons Attribution – Non Commercial (unported, v3.0) License. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed.
Introduction
Osteoporosis is a disease characterized by an increased fracture risk.Citation1 To treat osteoporosis, the Bisphosphonates can be administered intravenously or orally and are most widely used for their low cost and extensive range of use in different types of osteoporosis. Bisphosphonates, which have affinity for bone, are a safe treatment and compose an excellent class of antiresorptive drugs.Citation2
Medication-related osteonecrosis of the jaw (MRONJ) can be a debilitating complication of bisphosphonate therapy, and it is characterized by the presence of exposed bone longer than eight weeks. Other signs and symptoms may be present in presumed cases, including pain, swelling, paresthesia, suppuration, and ulceration of unhealed soft tissue. Lesions can occur spontaneously, but multiple hypotheses can explain the pathophysiology of this disease. That includes the inhibition of bone remodeling due to suppression of osteoclasts, angiogenesis inhibition, inflammation or infection after tooth extraction or a traumatic injury, innate or acquired immune dysfunction or genetic factors.Citation1,Citation3
Several therapies have been proposed for the treatment of osteonecrosis. The use of antibiotic therapy, surgical debridement and resections, local irrigation with antimicrobial agents, laser therapy, use of platelet-rich plasma, hyperbaric oxygen therapy, and ozone therapy are some of the main examples of proposed treatments.Citation4 Topical oxygen therapy has recently been reported in the literature as an effective and safe way to treat intraoral lesions.Citation5 A product based on the principle of improving the topical supply of oxygen for wounds has been available on the market (www.bluemcare.com). According to the available literature, blue®m oral gel showed promising results that helped in the healing process. This product seems promising due to its ease of use and positive influence on tissue healing through enhanced oxygenation without compromising the stability of the microbiome.Citation6
The aim of this paper was to report, through a clinical case, a treatment option for osteonecrosis of the jaw using topical active oxygen therapy with blue®m oral gel.
Clinical Case Report
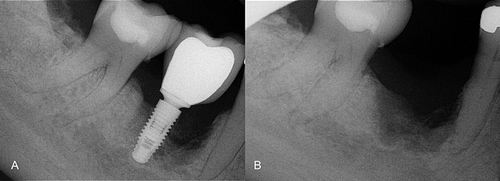
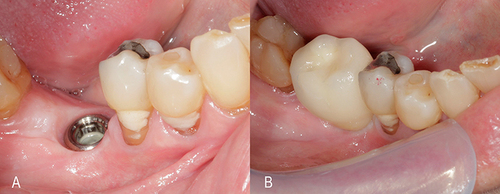
A 63-year-old female patient visited the dental clinic at Ilapeo College (Curitiba, Brazil) with the main complaint of pain and mobility of the implant of region #46. Through medical history, the patient reported that she had had breast cancer 15 years ago. She also reported controlled diabetes, osteopenia and rheumatoid arthritis, and that she was under constant medical monitoring and taking recommended medications. Clinical and radiographic examination detected significant bone loss around the referred implant (). After approval from the institution to disclose data from this clinical case, the patient signed the institutional informed consent form, authorizing the treatment plan and use of images, the dental implant was removed with surgical instruments (). After 15 days, the patient returned to have the sutures removed and, at this point, the healing process was good.
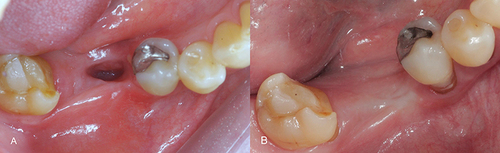
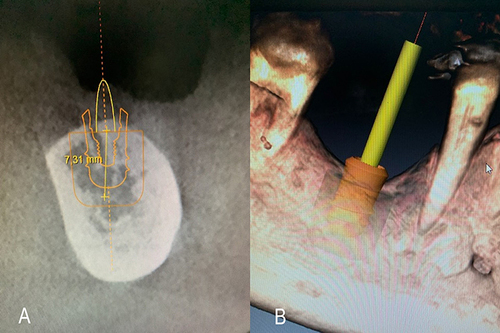
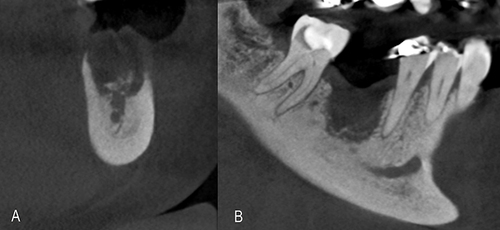
Three months after implant removal, the patient returned with purulent secretion in the affected socket. At that time, the patient reported that she had taken orally sodium alendronate (70 mg) weekly for four years but was no longer using it at the moment. The patient knew that this type of medication could be a risk to dental treatment and stopped taking the alendronate before undergoing dental implant surgery. A computed tomography (CBCT) examination revealed no bone repair at the socket (). The initial treatment selected was antibiotic therapy (Amoxicillin 875 mg, associated with potassium clavulanate 125 mg, and Metronidazole 250 mg for seven days).
Figure 2 CBCT Transversal section (A) and Longitudinal section (B) of the tomography image showing the characteristics of the bone tissue after 3 months of implant removal.
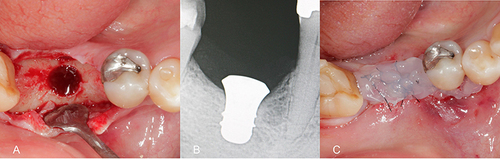
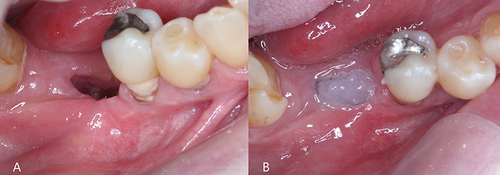
Clinical evidence of bone exposure and suppuration was seen after 3 months (), periapical radiography showed that there was still significant bone loss (), and at this moment, the MRONJ diagnosis was made. The procedure conducted for treatment was surgical debridement of the socket plus antibiotic therapy. The wound remained open after 30 days of clinical follow-up (), and the patient reported pain. At this time, a curettage was done, followed by application of blue®m oral gel to fill the socket (). The patient was instructed to continue applying the gel to the region every 8 hours for 15 days. When the patient returned after 15 days, it was observed that the wound was in a healing process, with the presence of epithelialized tissue and no bone exposure (). No pain was reported by the patient. The patient continued to be monitored at varying times and showed an excellent healing process. On the 2-year clinical follow-up, the lesion had healed entirely ().
Figure 3 Clinical diagnosis of osteonecrosis with evidence of bone exposure (A) and periapical radiograph showing extensive bone loss (B).
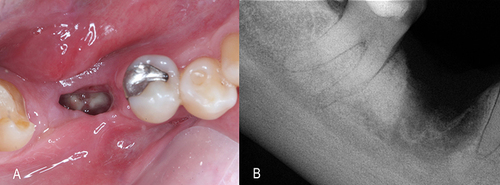
Figure 4 Thirty days of follow-up after surgical debridement (A) and topical application of blue®m oral gel (B).
After two years of monitoring MRONJ treatment with the bluem oral gel, a new CBCT showed the presence of healthy bone tissue on the socket. The installation of a new implant was performed. (). During the implant surgical procedure, it was possible to observe the quality and vitality of the existing bone (). Following the implant placement (Straumann Tissue Level WN 4.8 × 6mm) ( and ), the blue®m oral gel was applied to the wound (). After the osseointegration period, the prosthetic phase started. It was possible to see a healthy soft tissue () and a ceramic crown was installed (). The patient remains under clinical follow-up every three months.
Discussion
Patients diagnosed with MRONJ are recommended special recommendations and treatments that aim to eliminate pain, control soft and hard tissue infections and minimize the progression of bone necrosis.Citation4 It is important to find out the stage of osteonecrosis, the size of the lesion and the patient’s medical comorbidities to decide the best option of treatment.Citation7 Treatment strategies can be classified into surgical and non-surgical.Citation4
The American Association of Oral and Maxillofacial Surgeons (AAOMS) has categorized osteonecrosis into stages. In stage 0, there is no clinical evidence of necrosis, but radiographic changes and symptoms are present. Stage 1 considers the presence of exposed necrotic bone or fistulas but with no evidence of infection. Stage 2 is characterized by exposed necrotic bone and infection, as evidenced by pain and erythema in the region, with or without purulent drainage. As for stage 3, the exposed bone extends beyond the region of the alveolar bone.Citation8 The patient in this clinical case was classified as stage 2. According to the AAOMS, antibiotics are required to control symptoms in these cases, in addition to debridement of exposed necrotic bone. Because the previous treatment failed, it was decided to use topical oxygen gel as an alternative and it was observed a satisfactory result in controlling the evolution of MRONJ at the socket area.
There are no reports in the literature proving the efficacy of topical oxygen therapy with oral gel in cases of MRONJ. However, a recent literature review and meta-analysis on topical oxygen therapy have suggested that it is safe and effective in chronic wound treatment.Citation5 The blue®m oral gel was tested in a clinical study that compared the effects of topical oxygen therapy and chlorhexidine gel in the treatment of periodontitis. The group treated with oxygen-releasing gel showed better potential for reducing the probing depth.Citation9 When used to treat periodontitis, active oxygen in gel form selectively eradicates the anaerobic bacteria associated with the condition, promoting the recovery of healthy oral flora.Citation10 This clinical result corroborates the findings of the in vitro study, which showed that blue®m oral gel reduced a smaller number of bacterial species when compared to chlorhexidine during subgingival biofilm formation, but it was better than chlorhexidine in reducing red-complex bacterial proportions.Citation11
The bactericidal effect of blue®m oral gel was also seen in an in vitro study, in which it inhibited the growth of P. gingivalis similarly to the chlorhexidine digluconate action.Citation12 Angiogenesis is a noteworthy process, and it plays an important role in wound healing. Oxygen supplementation during the recovery process is known to aid in the oxidative death of bacteria, stimulate angiogenesis, accelerate the formation of the extracellular matrix, and increase fibroblast proliferation and collagen deposition, thereby facilitating faster healing. The use of blue®m oral gel as a topical oxygen therapy in histological wounds accelerated the healing of standardized, surgically done cutaneous wounds in rats, with enhanced angiogenesis and collagen fiber formation. Immunohistochemical analysis of this study’s samples revealed that the group that received the gel had significantly higher levels of vascular endothelial growth factor due to the gradual and continuous release of oxygen.Citation13 Thus, these studies showed that blue®m oral gel has bactericidal action, stimulates angiogenesis and the formation of new collagen fibers, which are fundamental factors for the tissue repair process. The potential of the bluem gel formula has also demonstrated excellent clinical results in a recently published article that showed novel oral care interventions within the scope of contemporary implantology, oral surgery and periodontology.Citation14
Conclusion
Based on this evidence, it is possible to conclude that the observed improvement in the current clinical case can be attributed to the positive effect of blue®m oral gel on the healing process of the osteonecrosis wound.
Statement of Authors
Regarding the titled manuscript, “Treatment of Medication-Related Osteonecrosis of the Jaws (MRONJ) with Topical Therapy Using Active Oxygen Gel” declare that all authors have given their consent for the publication of this clinical case.
Patient Consent
We declare that the patient authorized the use of the images for the present clinical case and agreed with their submission for publication.
Disclosure
Dra. Tatiana Deliberador is part of the bluem international board. The other authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Ruggiero SL. Reply: AAOMS position paper on medication-related osteonecrosis of the jaws-2022 update. diagnostic milestones, doubts, and perspectives on MRONJ. J Oral Maxillofac Surg. 2022;80(11):1724. doi:10.1016/j.joms.2022.07.150
- Rachner TD, Khosla S, Hofbauer LC. Osteoporosis: now and the future. Lancet. 2019;377(9773):1276–1287. doi:10.1016/S0140-6736(10)62349-5
- Uyanne J, Calhoun CC, Le AD. Antiresorptive drug-related osteonecrosis of the jaw. Dent Clin North Am. 2014;58(2):369–384. doi:10.1016/j.cden.2013.12.006
- Ruggiero SL, Dodson TB, Assael LA, Landesberg R, Marx RE, Mehrotra B. American association of oral and maxillofacial surgeons. American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws--2009 update. J Oral Maxillofac Surg. 2009;67(5 Suppl):2–12.
- Sun XK, Li R, Yang XL, Yuan L. Efficacy and safety of topical oxygen therapy for diabetic foot ulcers: an updated systematic review and meta-analysis. Int Wound J. 2022;19(8):2200–2209. doi:10.1111/iwj.13830
- Ngeow WC, Tan CC, Goh YC, Deliberador TM, Cheah CW. A narrative review on means to promote oxygenation and angiogenesis in oral wound healing. Bioengineering. 2022;9(11):636. doi:10.3390/bioengineering9110636
- Khan AA, Morrison A, Kendler DL, et al. International task force on osteonecrosis of the jaw. case-based review of Osteonecrosis of the Jaw (ONJ) and application of the international recommendations for management from the international task force on ONJ. J Clin Densitom. 2017;20(1):8–24. doi:10.1016/j.jocd.2016.09.005
- Campisi G, Mauceri R, Bedogni A, Fusco V. Re: AAOMS position paper on medication-related osteonecrosis of the jaw-2022 update. J Oral Maxillofac Surg. 2022;80(11):1723–1724. doi:10.1016/j.joms.2022.07.149
- Niveda R, Kaarthikeyan G. Effect of oxygen releasing oral gel compared to chlorhexidine gel in the treatment of periodontitis. J Pharm Res Int. 2020;32:75–82. doi:10.9734/jpri/2020/v32i1930711
- Sy K, Flamme J, Maquet H, et al. Antimicrobial effect and physical properties of an injectable ”active oxygen” gel for the treatment of periodontitis. Am J Dent. 2020;33(6):305–309.
- Shibli JA, Rocha TF, Coelho F, et al. Metabolic activity of hydro-carbon-oxo-borate on a multispecies subgingival periodontal biofilm: a short communication. Clin Oral Investig. 2021;25(10):5945–5953. doi:10.1007/s00784-021-03900-0
- Deliberador TM, Weiss S, Rychuv F, et al. Comparative analysis in vitro of the application of blue®m oral gel versus chlorhexidine on Porphyromonas gingivalis: a pilot study. Adv Appl Microbiol. 2020;10(04):194–201. doi:10.4236/aim.2020.104015
- Deliberador TM, Macalossi JMS, Tenorio C, Dall Agnol GS, Boia MF, Zielak JC. An oxygen-releasing agent promotes healing of skin wounds in rats. J Wound Care. 2023;32(11):738–747. doi:10.12968/jowc.2023.32.11.738
- Leventis M, Deliberador T, Alshehri F, Algham H. Topical oxygen therapy as a novel strategy to promote wound healing and control the bacteria in implantology, oral surgery and periodontology: a review. Saudi Dent J. 2024;36(6):841–854. doi:10.1016/j.sdentj.2024.04.004