Abstract
At present there is no universally accepted classification for gastritis. The first successful classification (The Sydney System) that is still commonly used by medical professionals was first introduced by Misiewicz et al in Sydney in 1990. In fact, it was the first detailed classification after the discovery of Helicobacter pylori by Warren and Marshall in 1982. In 1994, the Updated Sydney System was proposed during the International Workshop on the Histopathology of Gastritis followed by the publication in The American Journal of Surgical Pathology by Dixon et al. Using the new classification, distinction between atrophic and nonatrophic gastritis was revised, and the visual scale grading was incorporated. According to the Updated Sydney System Classification, atrophic gastritis is categorized into multifocal (H. pylori, environmental factors, specific diet) and corpus-predominant (autoimmune). Since metaplasia is a key histological characteristic in patients with atrophic gastritis, it has been recommended to use the word “metaplastic” in both variants of atrophic gastritis: autoimmune metaplastic atrophic gastritis (AMAG) and environmental metaplastic atrophic gastritis. Although there are many overlaps in the course of the disease and distinction between those two entities may be challenging, the aim of this review article was to describe the etiology, epidemiology, pathogenesis, diagnosis, clinical manifestations and treatment in patients with AMAG. However, it is important to mention that H. pylori is the most common etiologic factor for the development of gastritis in the world.
Epidemiology
The prevalence of pernicious anemia (PA; one of the distinctive manifestations of autoimmune metaplastic atrophic gastritis [AMAG]) is ~0.1% in the general population and ~2% in those older than 60 years.Citation1 For many years, it was suggested that PA is the disease of elderly females of Northern European ethnicity. Subsequently, it was shown that the prevalence of PA is similar among all populations (white, African American and non-white Hispanic).Citation2 Based on the analysis of the data from 156 patients affected by PA, in 1978, Carmel and JohnsonCitation3 concluded that black women develop PA at younger age than women of all other races (53±16 years, p<0.001). Similar to other autoimmune conditions, AMAG is more common in females than in males (3:1 ratio). Strong association between AMAG and other autoimmune disorders has been well documented.Citation4 It is believed that AMAG and PA might be underdiagnosed in all parts of the world. One of the explanations could be the fact that almost all forms of micro-and macrocytic anemia are treated with iron, folic acid and cobalamin without further identifying the etiology of the anemia. Moreover, in many cases, biopsy samples of the gastric mucosa are inadequate or taken from the wrong location.Citation5
Pathogenesis
The understanding of the pathogenesis of AMAG is somewhat challenging for several reasons: 1) the prevalence of AMAG is relatively low, 2) in many cases there is a concurrent Helicobacter pylori-induced gastritis and 3) no or minimal manifestations are present in early stages of the disease. Nevertheless, we know that both genetic and environmental factors play a role in the development of autoimmune gastritis. Using murine models, it was possible to discover autoimmune gastritis susceptibility genes (Gasa1, 2, 3 and 4) on chromosomes 4 and 6 and H2 region. Interestingly, three of these genes are located on the same locus as non-obese diabetic mouse diabetes mellitus (DM) susceptibility genes, which could explain the strong association between AMAG and DM type 1 (T1DM).Citation6,Citation7
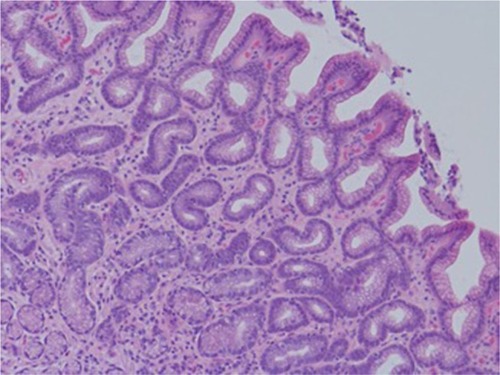
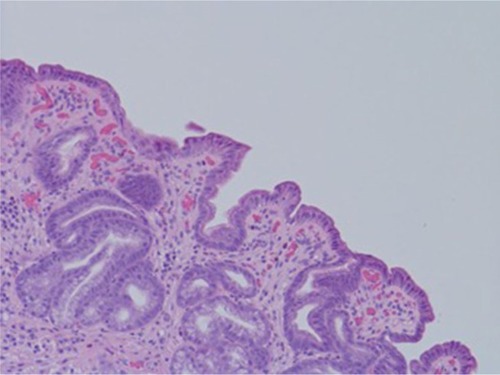
Despite a lack of understanding of the complex stages of AMAG pathogenesis, histological changes have been well studied ( and ). The initial changes include infiltration of oxyntic mucosa by lymphocytes and plasma cells. The uneven destruction of parietal cells with preserved islands of relatively normal oxyntic mucosa leads to the appearance of “islands in the sea”. This phenomenon, also known as gastric pseudopolyposis, is similar to colonic lesions in patients with ulcerative colitis.Citation8,Citation9 Hypochlorhydria, or the decrease/loss of hydrochloric acid secretion, then develops as a result of the combination of two factors: 1) loss of oxyntic mucosa and 2) disruption of maturation of parietal cells.Citation10 Absence of negative feedback from parietal cells induces G-cell hyperplasia and increased gastric secretion in the tantrum, which, in turn, leads to parietal cell pseudo hypertrophy resembling proton pump inhibitor-induced effects on parietal cells.Citation11 It is worth mentioning that this phenomenon cannot develop in atrophic glands, since anti-parietal cell antibodies also bind selectively to H+/K+ ATPase.Citation12 Another important effect of elevated gastric secretion is its direct stimulation and proliferation of enterochromaffin-like (ECL) cells, which depends on severity and can be hyperplastic, dysplastic and neoplastic.Citation13 Progression of ECL cell hyperplasia to neoplastic subtype can result in carcinoid tumor formation, which will be described subsequently. Areas of metaplasia develop within gastric body and fundus: pseudopyloric, intestinal metaplasia (IM) and pancreatic. Pseudopyloric metaplasia (“oxyntic antralization”) develops in oxyntic glands from mucus-secreting cells phenotypically resembling antral mucous cells. Although histologically pseudopyloric metaplasia may be indistinctive from antral gland cells, pepsinogen (PG) immunostaining can be helpful in differentiating: pepsinogen I (PGI) is characteristic of cells of oxyntic mucosa and is absent in the antrum.Citation14 Recently, a new term to describe pseudopyloric metaplasia has been widely used: spasmolytic polypeptide-expressing metaplasia (SPEM). The etiology of SPEM is not clear. Several theories have been proposed: 1) longstanding inflammation of oxyntic mucosa, 2) acute direct effect of toxic substances on parietal cells (DMP-777)Citation15,Citation16 and 3) transdifferentiation of chief cells.Citation17 Chief cells and SPEM express MAL2. This protein is involved in vesicle trafficking and considered the first trafficking protein, which is upregulated in SPEM.Citation18 It has been shown that SPEM is a preneoplastic gastric lesionCitation19 that can also transform into IM.Citation20 IM is the replacement of glandular, foveolar and surface epithelium of gastric mucosa by intestinal epithelium. Depending on the histological features, two subtypes have been described: small intestinal and colonic. They, in turn, can be grouped into three types, type 1, or small intestinal, with brush border, “complete”, which are replaced fully by small intestinal epithelium with all types of cells (goblet, Paneth, etc), expresses syalomucins. Type 3, or colonic type, without brush border, “incomplete”, are metaplastic cells that are formed in the neighborhood of normal gastric cells, expresses sulfomucins. Type 2, or colonic type, without brush border, “incomplete”, where metaplasia is similar to Type 3, expresses both gastric and intestinal mucins.Citation21 Apart from the abovementioned pathological changes, inflammatory and hyperplastic polyps develop in the later stages of AMAG.Citation22 Oxyntic mucosa can be totally absent in advanced disease.
Association with H. pylori
It is a well-known fact that H. pylori can cause atrophic gastritis on its own. On the other hand, it is important to remember that in many cases patients with AMAG may have concurrent H. pylori infection.Citation23 A third possible scenario is the progression of H. pylori-induced gastritis to AMAG. It is thought that etiology of this process is antigenic mimicry or cross-reactivity.Citation24 Many patients with H. pylori develop a wide spectrum of antibodies, which includes antifoveolar, anticanalicular and the classic APCA. The most frequently detected antibodies are anticanalicular antibodies that, similar to APCA, are directed against H+/K+ ATPase (proton pump).Citation25 Despite many overlaps in the course of the disease, it is important to differentiate AMAG from H. pylori-induced gastritis. AMAG affects only the body and fundus of the stomach, while H. pylori-induced lesions are known to have a multifocal pattern ().Citation26 Other important factors that help differentiate between AMAG and H. pylori-induced gastritis are 1) ECL hyperplasia (more common in AMAG), 2) parietal cell pseudohypertrophy (in AMAG; can be seen in H. pylori infection secondary to proton pump inhibitor use) and 3) oxyntic gland involvement (more common in AMAG).
Table 1 Comparison of AMAG with H. pylori-induced atrophic gastritis
Additionally, inflammatory changes are quite distinctive in both of these conditions: lymphocytes and plasma cells infiltrating lamina propria with involvement of deep layers (AMAG), superficial band-like lesions with active inflammation (H. pylori-induced atrophic gastritis).Citation27 Gastrin-17 (high in AMAG, low although may be elevated in H. pylori infection) and PGI levels (low in AMAG, normal in H. pylori infection) may also be utilized in patients at risk for gastric cancer (GC).Citation28
Association with other autoimmune conditions
It has been well recognized that AMAG has tendency to occur more often in patients with other autoimmune conditions.Citation29 Up to one-third of patients with autoimmune thyroid disease (AITD) and 6–10% of patients with T1DM have concurrent AMAG.Citation30,Citation31 Patients with polyglandular autoimmune (PGA) syndromes (especially PGA type 3B, which always includes AITD) are known to have a high prevalence of PA.Citation32 The other autoimmune conditions that have been known to co-occur with AMAG (or its advanced form PA) are vitiligo, Addison’s disease, myasthenia gravis and perioral cutaneous autoimmune conditions (especially, erosive oral lichen planus).Citation33–Citation35
Familial cases of pernicious anemia (FPA) have been described including those in twins, suggesting genetic component of the disease.Citation36 However, more studies need to be conducted to shed more light on how genetic variations predispose to the development of AMAG.Citation37 Very rare cases of coexistence of two inherited disorders (FPA and hereditary hemochromatosis) have also been described in the literature.Citation38
Diagnosis
In this section, we discuss the most common diagnostic tests used for screening and confirming a diagnosis of AMAG: serologic tests, endoscopy and histopathology.
Serological tests
The detection of target-specific antibodies has been well recognized as an effective method for screening and confirmation purposes. Among antibodies used for the diagnosis of AMAG, the following group is most widely used: APCA, anti-intrinsic factor antibodies (AIFAs) and anti-H. pylori antibodies (anti-HP-IgM and anti-HP-IgG). The significance of the measurement of anti-HP-antibodies is due to the frequent coexistence of H. pylori-induced gastritis and AMAG. APCA are known to have high sensitivity (~80%) but low specificity for PA.Citation39 In contrast, AIFAs have been shown to be less sensitive (~50%) but more specific for PA.Citation40 In patients with PA and negative AIFA, seroconversion may occur later in the course of the disease.Citation41 Measurement of gastrin level (mainly Gastrin-17) is another diagnostic test that can be abnormal in patients with AMAG due to oxyntic gland atrophy, leading to elevated gastrin production by G-cells in the antrum. The combined assay of APCA, AIFA and anti-HP-antibodies along with the measurement of serum gastrin (Gastrin-17) are also known as “serological gastric biopsy”. It has been recognized to be effective for diagnostic purposes and highly correlates with the histological findings.Citation42
The hypergastrinemia observed may be clinically difficult to differentiate from the other causes of hypergastrinemia. One method to identify the cause of hypergastrinemia is to measure the level of gastric acid output. With atrophic gastritis, the level of gastric acid output is low (<5 mEq/h), whereas with the hypergastrinemia associated with Zollinger-Ellison syndrome, the gastric acid output is >10 mEq/h. Furthermore, the secretin test is negative in >80% of patients.Citation43 Another commonly overlooked cause of hypergastrinemia is gastric outlet obstruction and gastric dysmotility, which may require an upper endoscopy and radiological studies to be evaluated. With gastric dysmotility, the parietal cell complement will be either normal or increased.Citation44 The measurement of PGI and PGII as well as PGI/PGII ratio can also be used to suspect AMAG. Specifically, PGI is secreted by the chief cells of oxyntic mucosa of gastric corpus and fundus, while PGII is produced by the chief cells and mucous neck cells of the entire gastric mucosa. Therefore, oxyntic atrophy is characteristic of AMAG, resulting in a decrease in PGI level along with low PGI/PGII ratio (<3).Citation45 PGII level is mainly unaffected by atrophy of oxyntic mucosa.
Patients with laboratory confirmation of macrocytic anemia require serum vitamin B12 measurement. When high suspicion of PA is present, normal vitamin B12 level should be followed by homocysteine (HCys) and methylmalonic acid (MMA) measurements.Citation46 However, it has also been shown that the serum levels of all three tests (vitamin B12, HCys and MMA) can fluctuate over time and even be normal in cobalamin-responsive disorders.Citation47
The measurement of the plasma chromogranin A (CgA) level has been suggested for the diagnosis of AMAG, ECL hyperplasia and gastric carcinoids. CgA levels have been found to correlate well with the degree of ECL hyperplasia in patients with AMAG. In one study, the elevated CgA is thought to be associated with the development of nonalcoholic fatty liver disease (NAFLD) and is undergoing additional investigation.Citation48 At the same time, the specificity of CgA level is too low (23%) to reveal gastric carcinoids in that group of patients.Citation49
In other conditions, CgA can lead to false-positive results, including in inflammatory bowel diseases, hepatocellular carcinomasCitation50 or other conditions such as with the chronic use of proton pump inhibitors or in renal insufficiency.
Endoscopy
In Western countries, endoscopic techniques for the diagnosis of AMAG have been used mainly for biopsy sampling purposes. The limitations related to endoscopy are the following: 1) low sensitivity, 2) low specificity and 3) interobserver variability.Citation51 However, with the advent of novel endoscopic modalities (magnifying endoscopy, narrow-band imaging [NBI] and autofluorescence imaging [AFI]), it has become possible to detect minimal atrophic changes of the gastric mucosa.Citation52 For instance, it has been shown that normal gastric corpus and fundus mucosal microvessels are characterized by the presence of 1) subepithelial capillary network (SECN) resembling honeycomb and 2) collecting venules in regular shape and appearance. In patients with atrophic gastritis, these normal findings are not seen.Citation53 It is worth noting that none of the endoscopic findings should be used alone to make a diagnosis of atrophic gastritis. In fact, the combination of them (for example, vascular pattern and swelling of areae gastrica) can significantly improve diagnostic accuracy.Citation54 As previously mentioned, in patients with high suspicion of atrophic gastritis, endoscopy has been used to get biopsy samples. According to the updated Sydney system recommendations, five biopsy samples should be obtained: two from the corpus, two from the antrum and one from the incisura angularis.Citation55
Histopathology
Biopsy with subsequent histology is considered the most reliable method for the diagnosis of metaplastic atrophic gastritis. Changes described in the “Pathogenesis” section may be seen. In some cases, when severe inflammation is present, it is hard to reliably evaluate oxyntic atrophy. Another limitation can happen when interpreting histological results from patients with early stages of AMAG. Several diagnostic hints have been suggested that may be characteristic of AMAG before profound loss of oxyntic mucosa: 1) infiltrates of lymphocytes and plasma cells in lamina propria, 2) focal atrophy of oxyntic mucosa along with SPEM or IM, 3) pseudohypertrophy of parietal cells and 4) ECL hyperplasia (at least, linear level).
Since ECL hyperplasia is the precursor of gastric carcinoid tumors, it is important to stain corpus and fundus samples with CgA and synaptophysin.Citation56 Additionally, staining for gastrin (negative in case of corpus/fundus biopsy) can help in localizing the site of a biopsy sample.Citation57
Clinical manifestations
The symptoms related to atrophic gastritis develop slowly and, in fact, may have a long asymptomatic period. In many cases, it is challenging to diagnose AMAG or its advanced form PA based only on clinical manifestations. The affected patients may present with a variety of signs and symptoms ranging from weakness to severe neurological manifestations such as paranoia (megaloblastic madness).Citation58 That is why among medical professionals, PA is also known as a “great pretender”. In this article, we would like to categorize clinical manifestations into three major groups: hematological, neurological and gastrointestinal.
Hematological manifestations
Iron-deficiency anemia (IDA) is one of the earliest presentations of AMAG that develops due to achlorhydria from oxyntic atrophy. Several studies have shown that refractory or unexplained IDA should increase clinicians’ suspicion of AMAG not only in adults but also in pediatric population.Citation59–Citation61 PA is the most common cause of cobalamin deficiency.Citation62 Although the underlying mechanisms of how cobalamin deficiency causes megaloblastosis have not been fully elucidated, it is believed that it is due to cobalamin’s essential role in DNA synthesis.Citation63 The asymptomatic increase in mean corpuscular volume and hypersegmented neutrophils are usually the initial laboratory findings in PA. With progression of the disease patients may complain of the weakness, light-headedness and palpitations. In advanced stages, symptoms of angina and congestive heart failure (peripheral edema and shortness of breath) may manifest.Citation64 Other very significant laboratory findings include thrombocytopenia, increased levels of LDH and bilirubin (signs of hemolysis). In rare cases, schistocytes in the peripheral smear may mimic other more serious conditions, such as disseminated intravascular coagulopathy (DIC) or thrombotic thrombocytopenic purpura/hemolytic uremic syndrome (TTP/HUS).Citation65 Cobalamin deficiencies have been associated with increased risk of thrombosis likely as a result of hyperhomocysteinemia. Elevated levels of HCys cause endovascular dysfunction. This, in turn, activates the coagulation system, increases platelet aggregation and constricts vessels. Acute myocardial infarction and pulmonary embolism have been described in young patients with severe hyperhomocysteinemia secondary to PA.Citation66,Citation67
Neurological manifestations
Neurological manifestations of cobalamin deficiency have long been associated with demyelination followed by axonal damage and eventually neuronal death.Citation68 The pathophysiological changes are not fully understood, however, MMA accumulation has been recognized to have direct impact on myelin formation and attributes to the myriad of neurological problems in patients with cobalamin deficiency.Citation69 Interestingly, neurological symptoms associated with cobalamin deficiency may be present in the absence of hematological changes.Citation70,Citation71 Subacute combined degeneration (SCD) is one of the most prominent neurological manifestations of PA. Posterior and lateral columns of the cervical and upper thoracic segments of the spinal cord are involved. This results in sensory abnormalities (usually initial symptoms) such as loss of vibratory and position sensations along with distal paresthesias. In advanced stages, corticospinal tract can also be affected.Citation72 Although in many situations, the neurological damage is irreversible, it is crucial to timely treat these patients with parenteral vitamin B12 in order to stop progression and improve neurological deficits.Citation73 Peripheral neuropathy is another common neurological manifestation of PA. The initial symptoms include paresthesia and numbness of the lower extremities. In this regard, it can be very difficult to distinguish clinically between peripheral neuropathy and SCD.Citation74 Both asymptomatic and overt optic neuropathy cases have been described in the medical literature.Citation75
Neuropsychiatric conditions associated with PA include mania, depression, obsessive-compulsive disorder (OCD), psychosis and dementia.Citation76 It is worth mentioning that the use of high dose of vitamins B12, B6 and folic acid has been shown to slow the shrinkage of the whole brain as well as reduce the cerebral atrophy in patients with Alzheimer’s disease (AD).Citation77
Gastrointestinal manifestations
Counterintuitively, AMAG rarely causes gastrointestinal symptoms. It has been suggested that this is due to the fact that most of the upper gastrointestinal-related complaints are secondary to increased level of hydrochloric acid. Hence, AMAG resulting in hypo- or even achlorhydria usually presents only with vague dyspeptic symptoms such as bloating, early satiety and epigastric discomfort.Citation78 Atrophic glossitis, which usually presents as burning sensation of the tongue, has also been known as an early clinical manifestation of cobalamin deficiency.Citation79
Neoplastic complications
The incidence of gastric neoplasms is higher in patients with AMAG compared to the general population.Citation80,Citation81 Overall, AMAG has been associated with the development of two types of gastric neoplasms: intestinal type GC and type I gastric carcinoid (TIGC).Citation82
Intestinal-type gastric cancer
Two main factors that have been known to explain the occurrence of GC in AMAG patients are IM and concurrent H. pylori infection, which per se is the most common trigger of IM of the gastric mucosa.Citation83 It should be pointed out that eradication of H. pylori in patients with known precancerous lesions (gastric atrophy, IM or gastric dysplasia) does not significantly lower the incidence of GC.Citation84 The pathogenesis of the development of GC has been described by Correa and PiazueloCitation85 and is better known as “Correa cascade”. A simplified model of the cascade can be divided into following steps: 1) normal gastric mucosa, 2) nonatrophic gastritis, 3) multiple atrophic gastritis without (initially) and with (later) IM, 4) dysplasia progressing from low grade to high grade and 5) GC.Citation86 It should be noted that AMAG without concurrent H. pylori infection is not considered to be part of the abovementioned cascade. Not all patients with H. pylori-induced gastritis develop GC. The chances are higher when certain virulence factors are present. For instance, CagA-positive strains of H. pylori have been shown to have significantly higher risk of the development of peptic ulcer and GC compared to CagA-negative strains.Citation87 Another well-known virulence factor known to be associated with GC is VacA gene. Variations in this gene can be explained by the presence of signal (s) and middle (m) regions.Citation88 Several studies have demonstrated the increased incidence of peptic ulcer and GC in patients infected with s1m1 compared to those infected with s2m2.Citation89
Type I gastric carcinoid
Although it has been recognized that AMAG is associated with increased risk of the development of TIGC, the exact incidence is not known. There are three known types of gastric carcinoids: type I is associated with AMAG, type II can be present in patients with multiple endocrine neoplasia (MEN) I and Zollinger-Ellison syndrome and type III, the most aggressive variant, usually occurs sporadically. Serum gastrin levels vary depending on the type of gastric carcinoid: types I and II – high, and type III – normal ().Citation90 The pathologic changes in T1GC are initiated by the loss of negative feedback by parietal cells on gastrin secretion. Hypo-/achlorhydria subsequently results in hypergastrinemia which, in turn, has trophic effects on ECL cells. ECL hyperplasia followed by ECL dysplasia is considered precancerous lesions and over time can progress to T1GC.Citation91 The detection of body polyps during endoscopy in patients with AMAG is strongly associated with the presence of TIGC. Patients with TIGC are usually asymptomatic, although symptoms of dyspepsia and IDA can be present. That is why the diagnosis is usually made during gastroscopy.Citation92
Table 2 Comparison of different types of gastric carcinoids
Treatment
The management strategies for AMAG and its advanced form PA depend on clinical manifestations, laboratory and imaging results. The therapy with the supplementation of iron, folic acid and cobalamin is commonly recommended in the early stages prior to progression to PA. Oral vitamin B12 supplement is used since it has been shown 1% of free vitamin B12 can be absorbed in the small intestine via passive diffusion.Citation93 However, in patients with neurological manifestations, parenteral administration of vitamin B12 is currently recommended.
Given the fact that AMAG is highly associated with other autoimmune conditions, appropriate diagnostic investigation should be conducted especially for disorders such as autoimmune thyroiditis and T1DM.
Detection and subsequent treatment for H. pylori infection is another very important therapeutic strategy due to associated risks related to H. pylori coinfection. Since it has been confirmed by several studies that H. pylori infection can induce autoimmune process in the gastric lining including oxyntic mucosa, eradication of H. pylori can decrease the levels of antibodies associated with AMAG and has been proven effective to cure early stages of autoimmune gastritis.Citation94,Citation95
T1GC has an excellent prognosis, therefore, different approaches have been suggested: surveillance, polypectomy and antrectomy (removal of gastrin-producing part of the stomach).Citation96 One of the potential treatments for TIGC has been recently introduced. Netazepide, a gastrin receptor antagonist, has been shown to decrease the plasma level of CgA along with tumor number and size.Citation97–Citation99 Another treatment option is to consider using somatostatin analogs. In one prospective study in a population of 107 with chronic atrophic gastritis, the authors showed that the use of somatostatin analogs resulted in a reduction in median gastrin and CgA levels and thus should be considered as effective therapy.Citation100 A new and emerging form of therapy for the treatment of neuroendocrine tumors is the use of peptide receptor radiotherapy (PRRT), although these newer therapies have not been prospectively studied to date for autoimmune atrophic gastritis.Citation101
Acknowledgments
This work received grant support from Department of Veterans Affairs RR&D Merit Review (JRP) I01 RX000194; Human Studies CORE through CURE: Digestive Diseases Research Center supported by NIH grant P30DK41301 and NIH NIDDK T32 NIH5T32DK07180 (JNB).
Disclosure
The authors report no conflicts of interest in this work.
References
- AndresESerrajKOptimal management of pernicious anemiaJ Blood Med201239710323028239
- ParkJYLam-HimlinDVemulapalliRReview of autoimmune meta-plastic atrophic gastritisGastrointest Endosc201377228429223199649
- CarmelRJohnsonCSRacial patterns in pernicious anemia. Early age at onset and increased frequency of intrinsic-factor antibody in black womenN Engl J Med197829812647650628388
- Lam-TseWKBatstraMRKoelemanBPThe association between autoimmune thyroiditis, autoimmune gastritis and type 1 diabetesPediatr Endocrinol Rev200311223716437010
- NeumannWLCossERuggeMGentaRMAutoimmune atrophic gastritis – pathogenesis, pathology and managementNat Rev Gastroenterol Hepatol201310952954123774773
- SilveiraPAWilsonWEEstebanLMIdentification of the Gasa3 and Gasa4 autoimmune gastritis susceptibility genes using congenic mice and partitioned, segregative and interaction analysesImmunogenetics200153974175011862406
- BaxterAGJordanMASilveiraPAWilsonWEVan DrielIRGenetic control of susceptibility to autoimmune gastritisInt Rev Immunol2005241–2556215763989
- IkedaTSenoueIHaraMTsutsumiYHarasawaSMiwaTGastric pseudopolyposis: a new clinical manifestation of type A gastritisAm J Gastroenterol198580282903970005
- KrasinskasAMAbrahamSCMetzDCFurthEEOxyntic mucosa pseudopolyps: a presentation of atrophic autoimmune gastritisAm J Surg Pathol200327223624112548171
- JuddLMGleesonPATohBHvan DrielIRAutoimmune gastritis results in disruption of gastric epithelial cell developmentAm J Physiol19992771 pt 1G209G21810409169
- ChlumskaABoudovaLBenesZZamecnikMAutoimmune gastritis. A clinicopathologic study of 25 casesCesk Patol200541413714216382988
- StolteMBethkeBRuhlGRitterMOmeprazole-induced pseudohypertrophy of gastric parietal cellsZ Gastroenterol19923021341381553828
- SolciaEFioccaRVillaniLLuinettiOCapellaCHyperplastic, dysplastic, and neoplastic enterochromaffin-like-cell proliferations of the gastric mucosa. Classification and histogenesisAm J Surg Pathol199519Suppl 1S1S77762735
- LiPHeCSunLDongNYuanYPepsinogen I and II expressions in situ and their correlations with serum pesignogen levels in gastric cancer and its precancerous diseaseBMC Clin Pathol201313111023360534
- GoldenringJRRayGSCoffeyRJJrReversible drug-induced oxyntic atrophy in ratsGastroenterology200011861080109310833483
- NomuraSYamaguchiHOgawaMWangTCLeeJRGoldenringJRAlterations in gastric mucosal lineages induced by acute oxyntic atrophy in wild-type and gastrin-deficient miceAm J Physiol Gastrointest Liver Physiol20052882G362G37515647607
- NozakiKOgawaMWilliamsJAA molecular signature of gastric metaplasia arising in response to acute parietal cell lossGastroenterology2008134251152218242217
- WeisVGPetersenCPMillsJCTumaPLWhiteheadRHGoldenringJREstablishment of novel in vitro mouse chief cell and SPEM cultures identifies MAL2 as a marker of metaplasia in the stomachAm J Physiol Gastrointest Liver Physiol20143078G777G79225190476
- HalldorsdottirAMSigurdardottrirMJonassonJGSpasmolytic polypeptide-expressing metaplasia (SPEM) associated with gastric cancer in IcelandDig Dis Sci200348343144112757153
- GoldenringJRNamKTWangTCMillsJCWrightNASpasmolytic polypeptide-expressing metaplasia and intestinal metaplasia: time for reevaluation of metaplasias and the origins of gastric cancerGastroenterology20101387220722102210.e120450866
- CorreaPPiazueloMBWilsonKTPathology of gastric intestinal metaplasia: clinical implicationsAm J Gastroenterol2010105349349820203636
- AbrahamSCSinghVKYardleyJHWuTTHyperplastic polyps of the stomach: associations with histologic patterns of gastritis and gastric atrophyAm J Surg Pathol200125450050711257625
- VeijolaLIOksanenAMSipponenPIRautelinHIKAssociation of autoimmune type atrophic corpus gastritis with Helicobacter pylori infectionWorld J Gastroenterol2010161838820039453
- NegriniRSavioAPoiesiCAntigenic mimicry between Helicobacter pylori and gastric mucosa in the pathogenesis of body atrophic gastritisGastroenterology199611136556658780570
- FallerGSteiningerHEckMHensenJHannEGKirchnerTAnti-gastric autoantibodies in Helicobacter pylori gastritis: prevalence, in-situ binding sites and clues for clinical relevanceVirchows Arch199642754834868624577
- GentaRMHelicobacter pylori, inflammation, mucosal damage, and apoptosis: pathogenesis and definition of gastric atrophyGastroenterology19971136 supplS51S559394760
- TorbensonMAbrahamSCBoitnottJYardleyJHWuTTAutoimmune gastritis: distinct histological and immunohistochemical findings before complete loss of oxyntic glandsMod Pathol200215210210911850538
- De ReVOrzesECanzonieriVPepsinogens to distinguish patients with gastric intestinal metaplasia and Helicobacter pylori infection among populations at risk for gastric cancerClin Transl Gastroenterol201677e18327441820
- CastoroCLe MoliRArpiMLAssociation of autoimmune thyroid diseases, chronic atrophic gastritis and gastric carcinoid: experience from a single institutionJ Endocrinol Invest201639777978426928404
- CentanniMMarignaniMGarganoLAtrophic body gastritis in patients with autoimmune thyroid disease: an under diagnosed associationArch Intern Med1999159151726173010448775
- De BlockCEDe LeeuwIHVan GaalLFAutoimmune gastritis in type 1 diabetes: a clinically oriented reviewJ Clin Endocrinol Metab200893236337118029461
- Ness-AbramofRNabriskiDABravermanLEPrevalence and evaluation of B12 deficiency in patients with autoimmune thyroid diseaseAm J Med Sci2006332311912216969140
- AmerioPTracannaMDe RemigisPVitiligo associated with other autoimmune diseases: polyglandular autoimmune syndrome types 3B+C and 4Clin Exp Dermatol200631574674916803462
- ZelissenPMBastEJCroughsRJAssociated autoimmunity in Addison’s diseaseJ Autoimmun1995811211307734032
- ChangKHLyuRKRoLSWuYRChenCMCoexistence of pernicious anemia and myasthenia gravis – a rare combination of autoimmune diseases in TaiwanJ Formos Med Assoc20061051194694917098697
- DelvaPLMacDonellJEMacIntoshOCMegaloblastic anemia occurring simultaneously in white female monozygotic twinsCan Med Assoc J196592211129113114285300
- BankaSRyanKThomsonWNewmanWGPernicious anemia – genetic insightsAutoimmun Rev201110845545921296191
- BonafouxBHenryLDelfourCAssociation of familial pernicious anaemia and hereditary haemochromatosisActa Haematol20081191121418176074
- RusakEChobotAKrzywickaAWenzlauJAnti-parietal cell antibodies – diagnostic significanceAdv Med Sci201661217517926918709
- KhanSDel-DucaCFentonELimited value of testing for intrinsic factor antibodies with negative gastric parietal cell antibodies in pernicious anaemiaJ Clin Pathol200962543944119398595
- OttesenMFeldt-RasmussenUFAndersenJHippeESchouboeAPernicious anemia. A study of initial forms of the disease and diagnostic significance of determination of the intrinsic factor antibody and parietal cell antibodyUgeskr Laeger199215452375837621471305
- AnticoATampoiaMVillaltaDTonuttiETozzoliRBizzaroNClinical usefulness of the serological gastric biopsy for the diagnosis of chronic autoimmune gastritisClin Dev Immunol2012201252097023251219
- ShahPSinghMHYangYXMetzDCHypochlorhydria and achlorhydria are associated with false-positive secretin stimulation testing for Zollinger-Ellison syndromePancreas201342693223851430
- PhanJBenhammouJNPisegnaJRGastric hypersecretory states: investigation and managementCurr Treat Options Gastroenterol201513438639726342486
- CarmelRPepsinogens and other serum markers in pernicious anemiaAm J Clin Pathol19889044424453177265
- WainwrightPNarayananSCookPFalse-normal vitamin B12 results in a patient with pernicious anaemiaClin Biochem201548181366136726277634
- SolomonLRCobalamin-responsive disorders in the ambulatory care setting: unreliability of cobalamin, methylmalonic acid, and homocysteine testingBlood2005105397898515466926
- WuPBDengYZShuYXTanSYLiMFangGIncreased plasma CgA levels associated with nonalcoholic fatty liver diseaseTurk J Gastroenterol201526540440726215060
- PeracchiMGebbiaCBasiliscoGPlasma chromogranin A in patients with autoimmune chronic atrophic gastritis, enterochromaffin-like cell lesions and gastric carcinoidsEur J Endocrinol2005152344344815757862
- MassironiSFraquelliMPaggiSChromogranin A levels in chronic liver disease and hepatocellular carcinomaDig Liver Dis2009411313518762462
- ParkYHKimNReview of atrophic gastritis and intestinal metaplasia as a premalignant lesion of gastric cancerJ Cancer Prev2015201254025853101
- DaiY-CTangZ-PZhangY-LHow to assess the severity of atrophic gastritisWorld J Gastroenterol201117131690169321483628
- AnagnostopoulosGKRagunathKShondeAHawkeyCJYaoKDiagnosis of autoimmune gastritis by high resolution magnification endoscopyWorld J Gastroenterol200612284586458716874879
- NomuraSIdaKTeraoSEndoscopic diagnosis of gastric mucosal atrophy: multicenter prospective studyDig Endosc201426670971924698334
- DixonMFGentaRMYardleyJHCorreaPClassification and grading of gastritis. The updated Sydney System. International workshop on the histopathology of gastritis, Houston 1994Am J Surg Pathol19962010116111818827022
- WongHHChuPImmunohistochemical features of the gastrointestinal tract tumorsJ Gastrointest Oncol20123326228422943017
- SepulvedaARPatilMPractical approach to the pathologic diagnosis of gastritisArch Pathol Lab Med2008132101586159318834216
- SmithADMMegaloblastic madnessBr Med J1960252161840184520789014
- HershkoCHoffbrandAKeretDRole of autoimmune gastritis, Helicobacter pylori and celiac disease in refractory or unexplained iron deficiency anemiaHaematologica200590558559515921373
- GonçalvesCOliveiraMEPalhaAMFerrãoAMoraisALopesAIAutoimmune gastritis presenting as iron deficiency anemia in childhoodWorld J Gastroenterol20142042157801578625400463
- MiguelNCostaESantalhaMJrRefractory iron-deficiency anemia and autoimmune atrophic gastritis in pediatric age group: analysis of 8 clinical casesJ Pediatr Hematol Oncol201436213413924327126
- StablerSPClinical practice. Vitamin B12 deficiencyN Engl J Med2013368214916023301732
- TefferiAPruthiRKThe biochemical basis of cobalamin deficiencyMayo Clin Proceed1994692181186
- AsimacopoulosPJGrovesMDFischerDKPernicious anemia manifesting as angina pectorisSouth Med J19948766716728202783
- TadakamallaAKTalluriSKBesurSPseudo-thrombotic thrombocytopenic purpura: a rare presentation of pernicious anemiaN Am J Med Sci201131047247422363087
- MelhemADesaiAHofmannMAAcute myocardial infarction and pulmonary embolism in a young man with pernicious anemia-induced severe hyperhomocysteinemiaThromb J2009711519232081
- ShamkaniWAJafarNSNarayananSRRajappanAKAcute myocardial infarction in a young lady due to vitamin B12 deficiency induced hyperhomocysteinemiaHeart Views2015161252925838876
- MetzJCobalamin deficiency and the pathogenesis of nervous system diseaseAnnu Rev Nutr19921259791354465
- FrancisGHoholKJawadZAyerATothCMethylmalonic acid accumulation and the development of peripheral neuropathy (IN1-1.010)Neurology2012781 supplIN1IN1
- RalapanawaDMJayawickremeKPEkanayakeEMJayalathWAB(12) deficiency with neurological manifestations in the absence of anaemiaBMC Res Notes2015845826385097
- LindenbaumJHealtonEBSavageDGNeuropsychiatric disorders caused by cobalamin deficiency in the absence of anemia or macrocytosisN Engl J Med198831826172017283374544
- HemmerBGlockerFXSchumacherMDeuschlGLückingCHSubacute combined degeneration: clinical, electrophysiological, and magnetic resonance imaging findingsJ Neurol Neurosurg Psychiatry19986568228279854956
- VasconcelosOMPoehmEHMcCarterRJCampbellWWQuezadoZMNPotential outcome factors in subacute combined degeneration: review of observational studiesJ Gen Intern Med200621101063106816970556
- SapersteinDSBarohnRJPeripheral neuropathy due to cobalamin deficiencyCurr Treat Options Neurol20024319720111931726
- ChuCScanlonPVitamin B12 deficiency optic neuropathy detected by asymptomatic screeningBMJ Case Rep20112011 bcr0220113823
- MetzlerDMillerWHStephen EdwardsCPsychiatric manifestation of vitamin B-12 deficiency: an updateJefferson J Psychiatry199192
- DouaudGRefsumHde JagerCAPreventing Alzheimer’s disease-related gray matter atrophy by B-vitamin treatmentProc Natl Acad Sci U S A2013110239523952823690582
- LahnerEAnnibaleBPernicious anemia: new insights from a gastroenterological point of viewWorld J Gastroenterol200915415121512819891010
- ZhuJCWangYFShengJChenFXTangGYAtrophic glossitis is attributed to cobalamin deficiencyShanghai J Stomatol20132215862
- VannellaLLahnerEOsbornJAnnibaleBSystematic review: gastric cancer incidence in pernicious anaemiaAliment Pharmacol Ther201337437538223216458
- VannellaLSbrozzi-VanniALahnerEDevelopment of type I gastric carcinoid in patients with chronic atrophic gastritisAliment Pharmacol Ther201133121361136921492197
- LahnerEEspositoGGalliGAnnibaleBAtrophic gastritis and pre-malignant gastric lesionsTransl Gastrointest Cancer201544272281
- SchnellerJGuptaRMustafaJVillanuevaRStrausEWRaffanielloRDHelicobacter pylori infection is associated with a high incidence of intestinal metaplasia in the gastric mucosa of patients at inner-city hospitals in New YorkDig Dis Sci200651101801180916944298
- WongBCLamSKWongWMChina Gastric Cancer Study GroupHelicobacter pylori eradication to prevent gastric cancer in a high-risk region of China: a randomized controlled trialJAMA2004291218719414722144
- CorreaPPiazueloMBThe gastric precancerous cascadeJ Dig Dis20121312922188910
- YongXTangBLiB-SHelicobacter pylori virulence factor CagA promotes tumorigenesis of gastric cancer via multiple signaling pathwaysCell Commun Signal201513111325589173
- YamaokaYMechanisms of disease: Helicobacter pylori virulence factorsNat Rev Gastroenterol Hepatol201071162964120938460
- van DoornLJFigueiredoCSannaRClinical relevance of the cagA, vacA, and iceA status of Helicobacter pyloriGastroenterology1998115158669649459
- WroblewskiLEPeekRMWilsonKTHelicobacter pylori and gastric cancer: factors that modulate disease riskClin Microbiol Rev201023471373920930071
- ZhouKHoWGastric carcinoids: classification and DiagnosisPisegnaRJManagement of Pancreatic Neuroendocrine TumorsNew York, NYSpringer New York20158393
- BurkittMDPritchardDMReview article: pathogenesis and management of gastric carcinoid tumoursAliment Pharmacol Ther20062491305132017059512
- LiT-TQiuFQianZRWanJQiX-KWuB-YClassification, clinicopathologic features and treatment of gastric neuroendocrine tumorsWorld J Gastroenterol201420111812524415864
- AndresEFothergillHMeciliMEfficacy of oral cobalamin (vitamin B12) therapyExpert Opin Pharmacother201011224925620088746
- StolteMMeierEMeiningACure of autoimmune gastritis by Helicobacter pylori eradication in a 21-year-old maleZ Gastroenterol19983686416439773482
- FallerGWinterMSteiningerHDecrease of antigastric autoantibodies in Helicobacter pylori gastritis after cure of infectionPathol Res Pract1999195424324610337662
- NikouGCAngelopoulosTPCurrent concepts on gastric carcinoid tumorsGastroenterol Res Pract2012201228782523316222
- DockrayGJClinical endocrinology and metabolism. GastrinBest Pract Res Clin Endocrinol Metab200418455556815533775
- MooreARBoyceMSteeleIACampbellFVarroAPritchardDMNetazepide, a gastrin receptor antagonist, normalises tumour biomarkers and causes regression of type 1 gastric neuroendocrine tumours in a nonrandomised trial of patients with chronic atrophic gastritisPLoS One2013810e7646224098507
- FossmarkRSordalOJianuCSTreatment of gastric carcinoids type 1 with the gastrin receptor antagonist netazepide (YF476) results in regression of tumours and normalisation of serum chromogranin AAliment Pharmacol Ther20123611–121067107523072686
- MassironiSZilliAFanettiICiafardiniCConteDPeracchiMIntermittent treatment of recurrent type-1 gastric carcinoids with somatostatin analogues in patients with chronic autoimmune atrophic gastritisDig Liver Dis2015471197898326321479
- KwekkeboomDJKrenningEPPeptide receptor radionuclide therapy in the treatment of neuroendocrine tumorsHematol Oncol Clin North Am201630117919126614376