Abstract
The failure rate of endoscopic retrograde cholangiopancreatography for biliary cannulation is approximately 6%–7% in cases of obstructive jaundice. Percutaneous transhepatic biliary drainage (PTBD) is the procedure of choice in such cases. Endoscopic ultrasound-guided biliary drainage (EGBD) is a novel technique that allows biliary drainage by echoendoscopy and fluoroscopy using a stent from the biliary tree to the gastrointestinal tract. Information in PubMed, Scopus, clinicaltrials.gov and Cochrane review were analyzed to obtain studies comparing EGBD and PTBD. Six studies fulfilled the inclusion criteria. Technical (odds ratio (OR): 0.34; confidence interval (CI) 0.10–1.14; p=0.05) and clinical (OR: 1.48; CI 0.46–4.79; p=0.51) success rates were not statistically significant between the EGBD and PTBD groups. Mild adverse events were nonsignificantly different (OR: 0.36; CI 0.10–1.24; p=0.11) but not the moderate-to-severe adverse events (OR: 0.16; CI 0.08–0.32; p≤0.00001) and total adverse events (OR: 0.34; CI 0.20–0.59; p≤0.0001). EGBD is equally effective but safer than PTBD.
Introduction
An estimated 500,000 endoscopic retrograde cholangiopancreatographies (ERCPs) are performed in the United States for diagnostic and therapeutic reasons.Citation1,Citation2 The failure rate of ERCP is approximately 6%–7% in cases of obstructive jaundice due to obstruction or altered anatomy.Citation3,Citation4 Surgical biliary decompression had been the mainstay of treatment for biliary decompression in such patients. However, it had significantly high morbidity and mortality in the postoperative period.Citation5–Citation7 Percutaneous transhepatic biliary drainage (PTBD) has a more favorable adverse events profile than surgical decompression but is associated with complications like fistula formation, repeat intervention, recurrent infection, and needs a long-term external catheter drainage, thereby leading to poor quality of life.Citation8–Citation10 Endoscopic ultrasound-guided biliary drainage (EGBD) is a novel technique that allows visualization and access of biliary tree by echoendoscopy and fluoroscopy, which was first described by Giovannini et al.Citation11 It has the perceived benefits of being physiologic with anatomic internal drainage, improved comfort and recovery with less adverse events, and low cost.Citation12 However, there are few studies published, to date, comparing the EGBD with PTBD in terms of success rate and adverse events profile in cases of failed ERCP.Citation4,Citation12–Citation16 Therefore, we conducted a meta-analysis to determine the aggregated efficacy and adverse events of EGBD and PTBD in such cases of failed ERCP.
Methodology
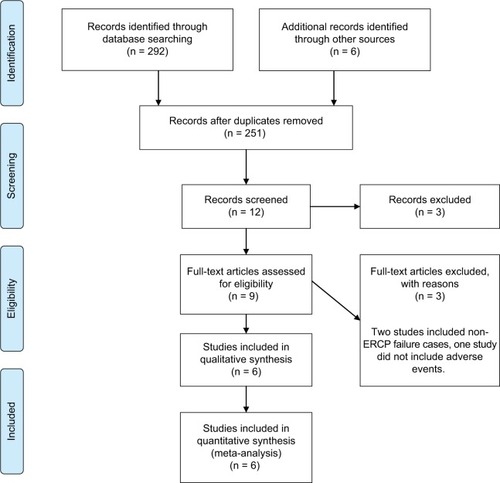
The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement for reporting meta- analysis and systematic reviews as recommended by the Cochrane Collaborative was used for this meta-analysis ().Citation17 A comprehensive electronic literature search was conducted for all the clinical trials on treatment of failed ERCP-guided biliary decompression between the years 2000 and 2016 on PubMed, Scopus, Cochrane library and clinicaltrials.gov using all field “failed ERCP,” all field “Percutaneous biliary drainage” and all field “EUS-guided biliary drainage”; all three search headings were connected with Boolean operator “AND.” Studies published in English comparing EGBD with PTBD in cases of failed ERCP were included. Two hundred and ninety-two articles were found in the database. We included randomized controlled trials (RCTs), retrospective comparative studies and published abstracts reporting at least some adverse events. We excluded prospective non-RCTs, case reports, letters and comments. Studies were also excluded if the sample size was <20. Only human studies were included. A total of six studies met the above-mentioned criteria.Citation4,Citation12–Citation16 Two studies were excluded as they included primary EGBD cases where ERCP was not tried as the primary procedure.Citation18,Citation19 A third study was excluded as they did not include the adverse event profile.Citation20
Figure 1 PRISMA statement of the study.
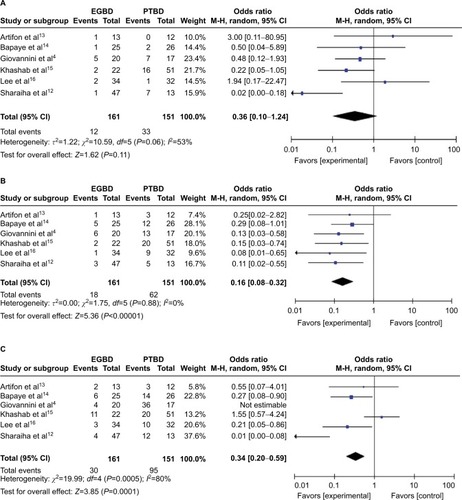
From the selected studies, we extracted the following baseline study details (): total number of patients enrolled, number of patients in each arm, mean age, gender ratio, comorbidity index, mean pre-procedural bilirubin, mean diameter of bile duct, etiology of biliary obstruction and reasons for ERCP failure. Technical and clinical success rates () and adverse event profile () were also extracted from each study. The outcomes were calculated with RevMan, version 5.2 Windows (Cochrane Collaboration, Oxford, UK). Analysis was performed by Mantel–Haenszel test. Odds ratio (OR) was calculated using 95% confidence interval (CI). A randomized model was used because of the low heterogeneity from the low number of studies. A p-value of <0.05 was considered to be significant. Technical success rate was defined as successful catheter or stent placement. Clinical success was defined as resolution of biliary obstruction without the need for repeat intervention. Biloma and perihepatic bile collection, recurrent abdominal pain, subcapsular hematoma, pancreatitis, pneumoperitoneum, hemobilia and infection of drain site or sepsis were considered mild adverse events in all the studies. Similarly, sheared guide wire, bleeding, hepatic abscess, bile leak and peritonitis, cholangitis, cutaneous leak, tube malposition or dysfunction and venous fistula were considered moderate adverse events, while cholecystitis and death were considered severe adverse events ().
Table 1 Baseline characteristics, etiology of obstruction and reason for ERCP failure
Table 2 Technical and clinical success rates of the included studies
Table 3 Adverse events of EGBD vs PTBD
Result
A total of 312 and 300 patients were analyzed for the technical and clinical success rates. Technical (odds ratio (OR): 0.34; CI 0.10–1.14; p=0.05; ) and clinical (OR: 1.48; CI 0.46–4.79; p=0.51; ) success rates were not statistically significant between the EGBD and PTBD groups (). Similarly, there was no significant difference in the mild adverse events profile between the two groups (OR: 0.36; CI 0.10–1.24; p=0.11; ). On the contrary, the moderate and severe, and total adverse events were significantly less in the EGBD group (OR: 0.16; CI 0.08–0.32; p≤0.00001 and OR: 0.34; CI 0.20–0.59; p≤0.0001, respectively; ). Cost analysis of the procedure was done in two studies.Citation13,Citation15 From both the studies, it was found that EGBD was less costly compared to PTBD (). The re-intervention rate was also less in the EGBD group for all the three studies reporting it ().Citation12,Citation15,Citation16
Figure 2 (A) Forest plot of technical success and (B) forest plot of clinical success.
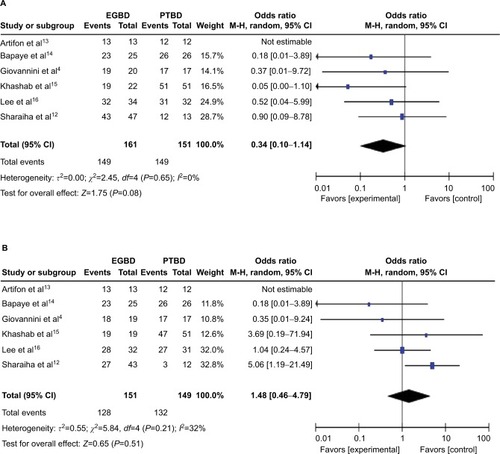
Figure 3 Forest plots of mild, moderate to severe, and total adverse events.
Abbreviations: EGBD, endoscopic ultrasound-guided biliary drainage; PTBD, percutaneous transhepatic biliary drainage; M–H, Mantel–Haenszel test.
Discussion
The standard technique to access the biliary tree is ERCP. The success rate of bile duct cannulation by ERCP is over 90% in cases of unaltered upper gastrointestinal anatomy.Citation15 The common reasons for the failed cannulation are altered or variant anatomy, ampullary pathology (stones, stenosis and tumor infiltration), periampullary diverticulum, gastric outlet obstruction, indwelling duodenal stent or previous gastric bypass surgery.Citation9,Citation21,Citation22 Traditionally, such cases were managed with PTBD or surgery.Citation23–Citation27 The adverse events profile of these procedures is significantly high. Data show that drain occlusion, dislocation and cholangitis are the common complications with long-term PTBD therapy that lead to frequent interventions and long-term hospital stay.Citation28 Also, patients are left with a long-term external drain which remains with the patients till the end of life, thereby, leading to poor quality of life.Citation19 EGBD has emerged as a noble option that is feasible, extremely safe, efficacious and minimally invasive.Citation29–Citation34 This procedure involves accessing the biliary tree from within the lumen of the gastrointestinal system using echoendoscopy and fluoroscopy, creating a fistulous tract and deploying a stent in a single-step procedure, thus, obviating the need for external drain.Citation22,Citation35 However, the success rate and adverse events rate of this procedure were unknown. Our study shows that this procedure is safe and effective with the same technical and clinical success rate at skilled centers with better adverse events profile.
The result of our study shows a similar success rate of both the procedures at this time. A high technical and functional success rate has been obtained in most clinical studies, as observed in a systemic review by Wang et al, of 94.71% and 91.66%, respectively.Citation36 This is partly because EGBD is being performed in high-volume centers by an experienced endoscopist. As the technique evolves, the success rate and the rate of complications of EGBD are bound to improve. At most centers, PTBD is an alternative procedure for failed ERCP. The development of EGBD, a technique that started just a decade ago as the fourth technique for biliary decompression (surgical drainage, percutaneous transhepatic drainage, endoscopic transpapillary drainage, EGBD), is currently replacing PTBD in high-volume centers.Citation37 Although, at present, local expertise determines the type of technique used for biliary drainage in failed ERCP, EGBD is a less invasive and more physiologic technique. It provides better nutrition absorption, avoids electrolyte loss, requires fewer re-interventions and prevents the stress of external drain.Citation38 If appropriate consent is obtained from the patient before ERCP, it can be done at a single setting.
EGBD is not without glitches. There are unique problems associated with EGBD at this time. This procedure is technically complex and diverse, with inherent risk of advanced endoscopy requiring specialized training and a steep learning curve.Citation39 Therefore, EGBD is only feasible at high-volume therapeutic centers where appropriate interventional radiology and surgical backup are present.Citation40 Otherwise, complications, such as bile leak, pneumoperitoneum, bleeding and stent migration, are likely to occur.Citation41,Citation42 There is a small theoretical risk of introducing infection in EGBD because of the invasion of sterile biliary tree by transmural puncture from the luminal side of the gastrointestinal tract.Citation43 But, the overall adverse events are bound to improve as in-roads are being made for this noble technique. Although labeled as rescue therapy for failed ERCP, primary EGBD is being currently compared to ERCP, and a recent study found comparable short-term outcomes of EGBD and ERCP.Citation44 Also, unlike ERCP, there is no risk of postprocedural pancreatitis. In the hands of expert endoscopists, clinical success rate and complications have not been found to be different in the two groups.Citation44,Citation45
Conclusion
EGBD is an effective alternative procedure when ERCP fails in terms of success rate and adverse events profile. As the technique is evolving, EGBD is replacing PTBD as the standard procedure of choice in cases of failed ERCP.
Disclosure
The authors report that no conflicts of interest in this work.
References
- VaradarajuluSKilgoreMLWilcoxCMEloubeidiMARelationship among hospital ERCP volume, length of stay, and technical outcomesGastrointest Endosc200664333834716923479
- CotéGASinghSBucksotLGAssociation between volume of endoscopic retrograde cholangiopancreatography at an academic medical center and use of pancreatobiliary therapyClin Gastroenterol Hepatol201210892092422387254
- EnochssonLSwahnFArneloUNilssonMLöhrMPerssonGNationwide, population-based data from 11,074 ERCP procedures from the Swedish Registry for Gallstone Surgery and ERCPGastrointest Endosc2010726117511841184.e1e320970787
- GiovanniniMBoriesENapoleonBBarthetMCaillolFPesentiC855 multicenter randomized phase II study: percutaneous biliary drainage vs EUS guided biliary drainage : results of the intermediate analysisGastrointest Endosc2015815AB174
- LuuCLeeBStabileBECholedochoduodenostomy as the biliaryenteric bypass of choice for benign and malignant distal common bile duct stricturesAm Surg201379101054105724160798
- KhajancheeYSCasseraMAHammillCWSwanströmLLHansenPDOutcomes following laparoscopic choledochoduodenostomy in the management of benign biliary obstructionJ Gastrointest Surg201216480180522331393
- SpanheimerPMCyrARLiaoJComplications and survival associated with operative procedures in patients with unresectable pancreatic head adenocarcinomaJ Surg Oncol2014109769770124395080
- ArtifonELSakaiPCunhaJESurgery or endoscopy for palliation of biliary obstruction due to metastatic pancreatic cancerAm J Gastroenterol200610192031203716968509
- LamérisJSStokerJNijsHGMalignant biliary obstruction: percutaneous use of self-expandable stentsRadiology199117937037072027978
- PiñolVCastellsABordasJMPercutaneous self-expanding metal stents versus endoscopic polyethylene endoprostheses for treating malignant biliary obstruction: randomized clinical trialRadiology20022251273412354980
- GiovanniniMMoutardierVPesentiCBoriesELelongBDelperoJREndoscopic ultrasound-guided bilioduodenal anastomosis: a new technique for biliary drainageEndoscopy2001331089890011571690
- SharaihaRZKumtaNADesaiAPEndoscopic ultrasound-guided biliary drainage versus percutaneous transhepatic biliary drainage: predictors of successful outcome in patients who fail endoscopic retrograde cholangiopancreatographySurg Endosc201630125500550527129552
- ArtifonELAparicioDPaioneJBBiliary drainage in patients with unresectable, malignant obstruction where ERCP fails: endoscopic ultrasonography-guided choledochoduodenostomy versus percutaneous drainageJ Clin Gastroenterol201246976877422810111
- BapayeADubaleNAherAComparison of endosonography-guided vs. percutaneous biliary stenting when papilla is inaccessible for ERCPUnited European Gastroenterol J201314285293
- KhashabMAValeshabadAKA comparative evaluation of EUS-guided biliary drainage and percutaneous drainage in patients with distal malignant biliary obstruction and failed ERCP. Dig Dis Sci2015602557565
- LeeTHChoiJHPark doHSimilar efficacies of endoscopic ultrasound-guided transmural and percutaneous drainage for malignant distal biliary obstructionClin Gastroenterol Hepatol201614710111019.e326748220
- BellerEMGlasziouPPAltmanDGPRISMA for Abstracts GroupPRISMA for Abstracts: reporting systematic reviews in journal and conference abstractsPLoS Med2013104e100141923585737
- TybergASaumoyMSequeirosEVEUS-guided versus percutaneous gallbladder drainage: Isn’t it time to convert?J Clin Gastroenterol Epub20161222
- ChoiJHKimHWLeeJCPercutaneous transhepatic versus EUS-guided gallbladder drainage for malignant cystic duct obstructionGastrointest Endosc201785235736427566055
- Torres-RuizMFDe La Mora-LevyJGAlonso-LarragaJODel MonteJSHernandez-GuerreroASu1337 biliary drainage in malignant obstruction: a comparative study between EUS-guided vs percutaneous drainage in patients with failed ERCPGastrointest Endosc2016835AB356
- PüspökALomoschitzFDejacoCHejnaMSautnerTGanglAEndoscopic ultrasound guided therapy of benign and malignant biliary obstruction: a case seriesAm J Gastroenterol200510081743174716086710
- ItoiTItokawaFSofuniAEndoscopic ultrasound-guided choledochoduodenostomy in patients with failed endoscopic retrograde cholangiopancreatographyWorld J Gastroenterol200814396078608218932289
- SmithACDowsettJFRussellRCHatfieldARCottonPBRandomised trial of endoscopic stenting versus surgical bypass in malignant low bileduct obstructionLancet19943448938165516607996958
- FerrucciJTJrMuellerPRHarbinWPPercutaneous transhepatic biliary drainage: technique, results, and applicationsRadiology198013511137360943
- HarbinWPMuellerPRFerrucciJTJrTranshepatic cholangiography: complicatons and use patterns of the fine-needle technique: a multi-institutional surveyRadiology1980135115226987704
- BahraMJacobDSurgical palliation of advanced pancreatic cancerRecent Results Cancer Res200817711112018084953
- GuptaKMallerySHunterDFreemanMLEndoscopic ultrasound and percutaneous access for endoscopic biliary and pancreatic drainage after initially failed ERCPRev Gastroenterol Disord200771223717392627
- NennstielSWeberAFrickGDrainage-related complications in percutaneous transhepatic biliary drainageJ Clin Gastroenterol201549976477025518004
- SongTJParkDHEumJBEUS-guided cholecystoenterostomy with single-step placement of a 7F double-pigtail plastic stent in patients who are unsuitable for cholecystectomy: a pilot study (with video)Gastrointest Endosc201071363464020189528
- SúbtilJCBetesMMuñoz-NavasMGallbladder drainage guided by endoscopic ultrasoundWorld J Gastrointest Endosc20102620320921160934
- ChoiJHLeeSSChoiJHLong-term outcomes after endoscopic ultrasonography-guided gallbladder drainage for acute cholecystitisEndoscopy201446865666124977397
- WidmerJAlvarezPGaidhaneMEndoscopic ultrasonography-guided cholecystogastrostomy in patients with unresectable pancreatic cancer using anti-migratory metal stents: a new approachDig Endosc201426459960224102709
- JangJWLeeSSParkDHSeoDWLeeSKKimMHFeasibility and safety of EUS-guided transgastric/transduodenal gallbladder drainage with single-step placement of a modified covered self-expandable metal stent in patients unsuitable for cholecystectomyGastrointest Endosc201174117618121704816
- IraniSBaronTHGrimmISKhashabMAEUS-guided gallbladder drainage with a lumen-apposing metal stent (with video)Gastrointest Endosc20158261110111526142558
- TeohAYBinmoellerKFLauJYSingle-step EUS-guided puncture and delivery of a lumen-apposing stent for gallbladder drainage using a novel cautery-tipped stent delivery systemGastrointest Endosc2014806117124830582
- WangKZhuJXingLWangYJinZLiZAssessment of efficacy and safety of EUS-guided biliary drainage: a systematic reviewGastrointest Endosc20168361218122726542374
- ItoiTMoving closer to developing an optimal algorithm for EUS-guided biliary drainageGastrointest Endosc201684694794927855799
- HoltBAHawesRHasanMBiliary drainage: role of EUS guidanceGastrointest Endosc201683116016526215648
- JamesPDAntonovaLMartelMBarkunAMeasures of trainee performance in advanced endoscopy: a systematic reviewBest Pract Res Clin Gastroenterol201630342145227345650
- KahalehMArtifonELPerez-MirandaMEndoscopic ultrasonography guided biliary drainage: summary of consortium meeting, May 7th, 2011, ChicagoWorld J Gastroenterol20131991372137923538784
- NakaiYIsayamaHYamamotoNSafety and effectiveness of a long, partially covered metal stent for endoscopic ultrasound-guided hepaticogastrostomy in patients with malignant biliary obstructionEndoscopy201648121125112827716860
- KawakuboKIsayamaHKatoHMulticenter retrospective study of endoscopic ultrasound-guided biliary drainage for malignant biliary obstruction in JapanJ Hepatobiliary Pancreat Sci201421532833424026963
- LakhtakiaSComplications of diagnostic and therapeutic Endoscopic UltrasoundBest Pract Res Clin Gastroenterol201630580782327931638
- DhirVItoiTKhashabMAMulticenter comparative evaluation of endoscopic placement of expandable metal stents for malignant distal common bile duct obstruction by ERCP or EUS-guided approachGastrointest Endosc201581491392325484326
- KawakuboKKawakamiHKuwataniMEndoscopic ultrasound-guided choledochoduodenostomy vs. transpapillary stenting for distal biliary obstructionEndoscopy201548216416926517848
