Abstract
Microscopic colitis (MC) is a chronic inflammatory bowel disease characterized by nonbloody diarrhea in the setting of normal appearing colonic mucosa. MC has two main subtypes based on histopathologic features, collagenous colitis and lymphocytic colitis. Management of both subtypes is the same, with treatment goal of reducing the number of bowel movements and improving consistency. First-line treatment involves counseling the patient about decreasing their risk factors, like discontinuing smoking and avoiding medications with suspected association such as NSAIDs, proton pump inhibitor, ranitidine, and sertraline. Starting loperamide for immediate symptomatic relief is used as an adjunct to therapy with glucocorticoids. Budesonide is considered first-line treatment for MC given its favorable side effect profile and good efficacy, though relapse rates are high. Systemic glucocorticoids should be reserved to patients unable to take budesonide. In glucocorticoid refractory disease, medications that have been tried include cholestyramine, bismuth salicylate, antibiotics, probiotics, aminosalicylates, immunomodulators, and anti-tumor necrosis factor-alpha inhibitors. More research is needed for the creation of a systematic stepwise approach for relapsing and refractory disease.
Introduction
Microscopic colitis (MC) is a chronic inflammatory bowel disease characterized by nonbloody diarrhea in the setting of normal appearing colonic mucosa and distinct histopathologic features. It has a preponderance for middle-aged women and is associated with various autoimmune disorders, as well as widely used medications including NSAIDs.Citation1 MC has two main subtypes, collagenous colitis (CC) and lymphocytic colitis (LC), as well as an incomplete variant. Although MC has been well-described in the medical literature since the 1970s, many aspects of this disease remain poorly understood and few high-quality studies are available to guide therapy. There have been promising advancements in the understanding of MC, as several international medical societies have published recent statements and guidelines on the diagnosis and treatment of MC, and various studies are on the horizon exploring new therapies such as novel biologics and even fecal transplant.Citation2,Citation3
General overview
Epidemiology
Based on a recent meta-analysis, the annual overall incidence of CC is 4.14 per 100,000 person-years and 4.85 per 100,000 person-years for LC. The overall prevalence of CC is 49.21 cases per 100,000 person-years and 63.05 cases per 100,000 person-years for LC.Citation4 It is important to note that most of the data about the incidence and prevalence of MC are from the developed Western world, namely the USA, Canada, Spain, the Netherlands, and Denmark. Data from the developing world are lacking. Age increases the risk of MC with an OR of 8.3 for age >65 years compared with <65 years.Citation5,Citation6 The incidence is higher in women than in men, with a female-to-male incidence ratio of 3.05 for CC and 1.92 for LC.Citation4
Risk factors
While the etiology of MC is still unknown, various independent risk factors, broadly including medications, tobacco, and autoimmune conditions, have been identified, which are implicated in both developing and flaring of MC. The widely used medications include proton pump inhibitors, NSAIDs, beta-blockers, statins, and selective serotonin reuptake inhibitors.Citation7 In fact, a recent Danish case–control study of 10,652 patients found a strong association of proton pump inhibitors with both CC (OR 6.98) and LC (OR 3.95), with the strongest association being with the current use of lansoprazole.Citation8 In addition to the classically described medications thought to have association with MC, new medications, namely novel chemotherapeutic agents immune checkpoint inhibitors (ICPIs), have been implicated in causing histologically proven MC. It is important to distinguish this entity as patients on ICPIs had a more aggressive course often requiring hospitalization and were treated with more aggressive immunosuppression such as oral and intravenous corticosteroids and infliximab as well as vedolizumab.Citation9 While medications are classically thought of as being causative for MC, evidence to this fact remains present only in certain individual cases with larger scale studies unable to replicate the cause and effect relationship.Citation10 Smoking has also been found to have an association with MC, leading to the onset of disease >10 years earlier than seen in nonsmokers.Citation11 Various autoimmune disorders, including celiac disease, type 1 diabetes, autoimmune thyroiditis, and inflammatory arthritis, are also associated with greater risk of MC.Citation7 In fact, patients with celiac disease have a 70-fold risk of developing MC over the general population, thought to be due to association with the human leukocyte antigen-DR3-DQ2, which is prevalent in both MC and celiac disease.Citation12,Citation13 Lastly, other lymphocytic disorders of the gastrointestinal tract, such as lymphocytic gastritis, lymphocytic esophagitis, and duodenal intraepithelial lymphocytosis, have also been associated with MC.Citation14
Pathophysiology
The exact mechanism of diarrhea in MC remains largely unknown but is thought to be multifactorial. Mucosal inflammation has been proposed as the most pathophysiologic mechanism of the diarrhea. This may be due to mucosal changes due to inflammation that lead to reduced sodium and chloride absorption, inhibition of the chloride/bicarbonate exchange channels, and a decrease in passive permeability.Citation15 These changes consequently lead to a secretory diarrhea. An osmotic element has also been studied and is supported by the finding that periods of fasting decrease fecal weight.Citation16 Bile salt malabsorption may also play a factor, as bile acid sequestrants have successfully been used to treat diarrhea in MC. In one study, a selenium-labeled homocholic acid taurine test was used to study bile acid malabsorption in patients with CC, and 44% (12/27) were found to have an abnormal test.Citation17 Mucosal injury from luminal contents has also been proposed as another factor leading to diarrhea. This was evidenced by studying patients who underwent diverting ileostomy, who were found to have histologic improvement of the MC. This improvement later reverted when the ileostomy was reversed.Citation18 The microbiome has also been implicated in the pathogenesis of MC, with an identified increase in the proinflammatory sulfur-reducing bacterial family Desulfovibrionales and a decrease in Coriobacteriaceae, which is seen in abundance in the healthy gastrointestinal tract.Citation19 Additionally, given that the disease is most prevalent in postmenopausal women, hormones are thought to play a role in the pathophysiology of MC. In a pooled analysis by the Nurses’ Health Study, exogenous oral contraceptive and menopausal hormone therapy use were associated with the increased risk of MC, thereby implicating estrogen in playing a role in inflammation of the gastrointestinal tract.Citation20
Symptoms
The hallmark symptom of MC is chronic, nonbloody, watery diarrhea. The diarrhea can develop suddenly, or develop progressively, to a frequency reported up to 15 times a day. The watery diarrhea is often associated with abdominal pain, urgency, incontinence, nocturnal symptoms, and/or weight loss.Citation6,Citation21 Fatigue has also been noted to be a prevalent symptom in MC, as reported by both Nyhlin et al and Kane et al.Citation22,Citation23 Fatigue severity was associated with concurrent anxiety, depression, and somatization in MC.Citation23 While a recent systematic review and meta-analysis showed that one in three patients with MC can have symptoms of irritable bowel syndrome, namely alterations in bowel habits and abdominal pain, the rate of symptoms was similar to the general population, despite recent case–control studies showing the opposite.Citation24 Given overlap with various other gastrointestinal illnesses, the diagnosis can often be difficult to pinpoint and as such, the differential diagnosis for MC is broad, including irritable bowel syndrome with diarrhea, medication-induced diarrhea, inflammatory bowel disease, and an array of malabsorptive disorders.
Diagnosis
Once MC is suspected, the patient is sent for endoscopic evaluation with biopsies, and the diagnosis is ultimately made via characteristic histologic findings. While there can be laboratory abnormalities that can occur in up to 50% of patients with MC, including elevated erythrocyte sedimentation rate and autoantibodies such as antinuclear antibody, rheumatoid factor, antimitochondrial antibody, antineutrophilic cytoplasmic antibodies, anti-Saccharomyces cerevisiae antibodies, and antithyroid peroxidase antibodies, these are neither sensitive nor specific to the disease and are not necessary for diagnosis.Citation6,Citation25 Similar to laboratory evaluation, fecal biomarkers such as calprotectin and lactoferrin are of little utility for diagnosing MC. While calprotectin levels were found to be increased in active vs quiescent disease, 38% of patients in the study with active MC had negative calprotectin levels.Citation26 Fecal lactoferrin fared worse, with only 3 of 39 patients evaluated having a positive test result in one study, and 1 of 21 patients in another.Citation26,Citation27 Colonoscopy usually reveals normal colonic mucosa on endoscopic examination. The American Society of Gastrointestinal Endoscopy recommends two or more biopsies of the transverse, sigmoid, and descending colon if flexible sigmoidoscopy is performed and two of more biopsies of the right, transverse, descending, and sigmoid colon if colonoscopy is performed.Citation28 We recommend that colonoscopy, rather than flexible sigmoidoscopy, be routinely performed if MC is suspected as histologic changes can be patchy in distribution, and inflammatory severity is greatest in the more proximal colon. Flexible sigmoidoscopy, however, can diagnose >90% of MC.Citation29,Citation30 Classic histologic features of LC include >20 intraepithelial lymphocytes per 100 epithelial cells. Histologic features of CC include a 10–20 µm diameter of thickened subepithelial collagen band, detachment of surface epithelial cells from subepithelial collagen, and an increase in intraepithelial lymphocytes however not to the same extent as of LC and not essential to histologic diagnosis.Citation31 The histology of incomplete MC, which seeks to widen the catchment of symptomatic patients who may not classically fit into the diagnostic criteria above, includes >10 and <20 intraepithelial lymphocytes for iLC and >5 and <10 µm thickness of the collagen band for iCC.Citation32
Prognosis
While the diagnosis of MC does not alter mortality or longevity, it certainly impacts the quality of life. A Spanish study evaluating the natural history of MC with a median follow-up time of 8 years showed that 75% of patients achieved remission free from drugs for more than a year. However, while 93% of patients who achieved remission spontaneously went on to have sustained remission, only 60.5% of patients who achieved drug-induced remission remained disease free after a year.Citation33 Additionally, despite being in clinical remission, patients can often have lasting symptoms including abdominal pain, fatigue, arthralgia, or myalgia, several years after diagnosis compared with controls.Citation22 While MC can have a lasting impact on the health-related quality of life (HRQOL) of patients, it is important to note that it is not associated with an increased risk of colorectal cancer. In fact, patients with MC had a negative association with neoplastic polyps compared with patients who had chronic diarrhea without MC, with an OR =0.22.Citation34
Management
The overall goal in the management of MC is symptomatic improvement, the exact definition of which varies greatly between studies. A large population-based study has defined clinical remission as improvement in bowel movements to less than three per day or less than one watery stool daily over the course of 1 week.Citation1,Citation2,Citation35 This has been shown to correlate significantly with an increase in HRQOL and consequently has been widely utilized. It is yet unclear whether histologic remission should be a goal that drives therapy.Citation36,Citation37 Given that, to date, no biomarker has been identified to assess the severity of disease, defining disease activity by clinical variables is crucial. The Microscopic Colitis Disease Activity Index was developed recently to help further define management goals. It is the first prospective study to identify disease activity and to name six variables (unformed stools, nocturnal stools, abdominal pain, weight loss, fecal urgency, and fecal incontinence), which they showed to correlate significantly with quality of life. The study, which included 162 patients, hopes to standardize guidelines for remission and offer a more direct comparison of available therapies.Citation21,Citation38 Lastly, there is currently discussion regarding including histologic remission as a potential end point of therapy.Citation39
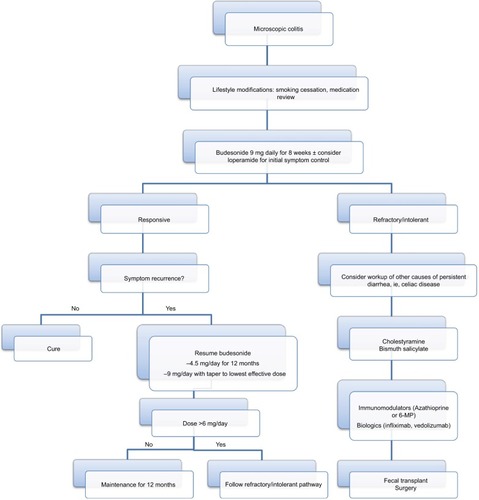
We have provided an algorithmic approach to the therapeutic management of MC below ().
Lifestyle modifications and symptom management
MC has very clearly defined risk factors, including smoking and various medications. Lifestyle modifications including decreasing caffeine, dairy (in patients with lactose intolerance), and alcohol consumption may improve the diarrhea seen in MC.Citation39 It is also critical that concomitant celiac disease and bile acid malabsorption be appropriately diagnosed and managed, as they can be associated with MC.Citation40
Withdrawal of medications that have been implicated in causing MC may be considered as an addition to the standard first-line therapy. The medications with the strongest known association are acarbose, aspirin, NSAIDs, proton pump inhibitors (lansoprazole and omeprazole), ranitidine, sertraline, and ticlopidine.Citation39,Citation41 In a true case of a drug-induced MC, clinical and histologic improvement as well as recurrence with rechallenge should be documented.Citation42
Loperamide was until recently the only identified therapy for MC. It continues to have a role in symptomatic management with doses of 2–16 mg/day according to retrospective studies.Citation40 It is important to note that clinical remission is seldom achieved in loperamide monotherapy, and there is no evidence of histologic improvement.Citation37 No randomized placebo-controlled trials have been done to study the use of loperamide in MC.
Budesonide
Budesonide is an oral corticosteroid with very low systemic bioavailability. This is achieved via the capsule, which is formulated to dissolve in a pH-dependent manner to deliver the drug into the ileum and ascending colon.Citation43 The 2016 AGA clinical guideline for the management of MC recommends that budesonide be used as first-line therapy.Citation3 This is based on six randomized clinical trials showing clinical response and five showing histological response.Citation44–Citation49 This was further augmented by a favorable side effect profile as well as the ease of once daily dosing, though cost was noted as a barrier to therapy.
A recent 2017 Cochrane review echoed these sentiments and demonstrated that budesonide 9 mg/day for 6–8 weeks was effective in inducing both clinical and histologic remission. In two examined studies with a total of 57 patients, 88% showed clinical response to budesonide as opposed to 38% to placebo and 78% showed histologic response compared with 33% with placebo.Citation50 The “number needed to treat” was two for CC and three for LC. Notably, the median time to remission was ~10.5 days.Citation51 A recent randomized, placebo-controlled, multicenter study showed that budesonide 9 mg daily induced clinical remission at 8 weeks in 79% of patients vs 42% with placebo. Histologic remission was attained in 68% of budesonide group vs 21% of placebo group.Citation52 Further randomized controlled trials have shown that remission can be maintained for 6 months, with doses as low as 6 mg/day.Citation42,Citation51 Skin hematoma, cataracts, and increased blood glucose levels have been reported as side effects of budesonide therapy.Citation42
Despite the effectiveness of budesonide, relapse rates have been reported at 40%–81% and can occur as soon as 2 weeks after cessation of therapy.Citation53 Certain factors, such as longer duration of symptoms prior to initiation of therapy, age over 60 years, and more severe baseline diarrhea, can be foreboding.Citation1,Citation41,Citation51,Citation53 A prospective, randomized, placebo-controlled study by Münch et al aimed to tackle the high relapse rate by examining low-dose (4.5 mg/day) budesonide maintenance therapy for 12 months. Remission was maintained at 1 year in 61.4% of patients in the budesonide arm vs 16.7% in the placebo arm. There were no serious adverse events reported with more long-term therapy in this study, and overall side effects were reported in 7 out of 44 patients.Citation51 In another study by Fernandez-Bañares, 53% of patients had at least one clinical relapse after initial withdrawal of budesonide and were either resumed on 9 mg/day and tapered to the lowest effective dose or resumed at the previous lowest effective dose. Twenty-one percent of patients needed a budesonide dose >6 mg daily to maintain clinical remission, and the others tolerated 3 mg/day or 3 mg every other day for maintenance of remission. The authors did note that in long-term use of >6 mg budesonide daily, consideration for alternative therapies such as thiopurines could be considered.Citation54
On the horizon are new studies on the use of beclomethasone dipropionate, a synthetic corticosteroid with topical colonic release. In an open-label multicenter study of 23 patients, patients were given beclomethasone 10 mg/day for 4 weeks, followed by 5 mg/day for 4 weeks. Their symptoms were assessed via the Bristol stool scale and a telephone interview. Remission was defined as less than eleven loose stools over 7 days. At week 8, 70% of patients were in remission.Citation55 While beclomethasone does appear to induce remission, a 2010 trial demonstrated that only 26% of patients (from the 84% with initial response) maintained clinical remission at 1 year, bringing its longevity into question.Citation50 While beclomethasone dipropionate is promising, it is not available in the USA and to date is only in use in Europe.
Systemic corticosteroids
Unlike budesonide, the role of systemic corticosteroids in the treatment of MC is limited. The 2016 AGA guideline recommends treatment with prednisone or prednisolone only when no other treatment is available or when cost is a significant hindrance.Citation3 Most of the evidence for the use of systemic corticosteroids is inferred from the successes of budesonide as well as their long-standing use in medical practice, however, is considerably limited by their side effect profile. One small randomized trial of 12 patients showed a 22% response rate in the prednisone arm vs no response in the three patients in the control arm.Citation56 A population-based study in 2013 by Gentile et al found that the response to prednisolone was 52.9% (as compared to 82.5 with budesonide) and the rate of recurrent disease was higher than with budesonide therapy (HR 0.38, CI 0.18–0.85, P=0.02).Citation57 A double-blind, placebo-controlled randomized trial of 50 mg/day of prednisolone for CC showed incomplete remission in two of nine patients treated.Citation58 Overall, there is a paucity of evidence for systemic corticosteroids in the treatment of MC, and its effects are marginal compared with budesonide.Citation39
Refractory MC
Bismuth salicylate
Bismuth salicylate is recommended by the 2016 AGA guideline as a second-line therapy for MC when budesonide is unable to be used, either due to cost or adverse effects.Citation3 This is based on a small randomized study of 14 patients which showed that all seven of seven patients in the intervention arm (eight to nine 262 mg bismuth tablets divided into three doses per day for 8 weeks) had clinical response vs none of the patients in the placebo arm.Citation59 The study included nine patients with CC and five patients with LC. Additionally, patients treated with bismuth salicylate had a 3-fold, albeit not statistically significant, likelihood of achieving a concomitant histologic response. A retrospective study showed complete response in 53% of patients and partial response in 28% of patients taking three tablets (262 mg each) of bismuth salicylate three times a day.Citation60 Therapy was noted to be more effective in patients with milder symptoms and older patients. There has also been a case report of lower dose bismuth sub-salicylate, two tablets of 262 mg each, three times daily for 1 month, resulting in clinical and histologic remission.Citation61 While there have not been any adverse events related to bismuth salicylate treatment and the cost of therapy is relatively low, there is potential for neurotoxicity and nephrotoxicity with long-term use, and the significant pill burden is a conceivable barrier to compliance with therapy.Citation62
Cholestyramine
Cholestyramine is thought to play a role in the treatment of MC due to its bile acid-binding capacity, as bile acid mal-absorption has been thought to play a role in pathogenesis of MC; however, it also adheres to bacterial toxins, which have been implicated in the pathophysiology of CC.Citation2 In a retrospective study of 27 patients with biopsy-proven CC, the rate of bile acid malabsorption was noted to be 44%, and cholestyramine therapy with 4 g two to three times daily (or colestipol 5 g two to three times daily) resulted in clinical remission in 11/12 (92%) patients with bile acid malabsorption compared with 10/15 (67%) without. Ultimately, 21/27 (78%) patients had improvement with bile acid-binding therapy.Citation17 Cholestyramine was also studied as an adjunct to mesalamine in a randomized control trial of 41 patients and did not show any added benefit.Citation63 Given the significant potential for drug–drug interactions and the lack of proven benefit, the AGA recommended against combination therapy with cholestyramine. No randomized clinical trials have been done to elucidate the appropriateness of cholestyramine monotherapy in MC. Retrospective studies, however, have shown response rates of 59%–65%.6,64
Antibiotics and probiotics
AGA recommends against treatment with Boswellia serrata as well as other probiotics. While there has been evidence showing some efficacy, including a single randomized controlled trial of 31 patients in which 44% of patients treated with Boswellia showed clinical improvement (however, no histologic or quality of life improvement) compared with 27% of patients treated with placebo, the results were not statistically significant.Citation65 There is also concern about the lack of standardization between preparations of B. serrata.Citation3 Similar concerns apply to the wide variety of probiotics available on the market at present. A randomized placebo-controlled trial of Lactobacillus acidophilus LA-5 and Bifidobacterium animalis AB-Cap-10 failed to demonstrate a benefit over placebo.Citation66 An open-label uncontrolled trial of Escherichia coli strain Nissle 1917 did show improvement in stool frequency (64% of patients) and stool consistency (50% of patients).Citation67 A randomized open-label trial comparing the probiotic VSL#3 to mesalamine in 30 patients found that 5/11 (46%) patients on VSL#3 compared with 1/13 (8%) patients on mesalamine achieved remission.Citation68 While VSL#3 may offer a benefit, randomized placebo-controlled trials would be necessary. No controlled clinical trials evaluating antibiotic use exist; however, metronidazole and erythromycin have been used anecdotally with varying success.Citation1 In a large retrospective clinical review of 163 patients with CC, the rate of response to antibiotics (metronidazole, erythromycin, and penicillin G) was noted to be 60%, but there was no mention of concomitant treatment, dosing, or relapse rate.Citation6 Another large retrospective review of 199 patients with LC found that 23 patients were given metronidazole with 14 showing clinical response (61%), however, six relapsed within 1 month.Citation69
Aminosalicylates
Mesalamine can be considered as an alternative to budenoside therapy when the latter is not feasible due to contraindications or poor clinical response, despite varying evidence on its success.Citation3 Two randomized placebo-controlled trials did not show any effect of mesalamine 3 g/day compared with placebo in short-term 8-week induction.Citation48,Citation52 As previously mentioned, a comparison between mesalamine and mesalamine plus cholestyramine was undertaken and showed a high remission rate (85% in LC and 91% in CC) in both treatment arms, with the addition of cholestyramine being slightly superior.Citation63 Efficacy has otherwise been supported solely by observational studies and case series. While the 2016 AGA guideline recommends mesalamine as an alternative, the European guidelines (Spanish microscopic Colitis Group, European Microscopic Colitis Group) do not, as there is a clear need for more research on the matter.Citation2,Citation3,Citation37
Immunomodulators
Immunomodulators such as azathioprine or 6-MP may have a role in the treatment of severe, steroid dependent, or refractory disease. In one small open study, azathioprine induced partial or complete remission in eight of nine patients with MC.Citation70 A retrospective study found that the overall response rate to thiopurines (azathioprine 2 mg/kg/day) was 41% (19/46 patients); however, there were significant side effects that often led to withdrawal of therapy including hepatitis, pancreatitis, bone marrow suppression, and infection.Citation39,Citation71 A recent Mayo Clinic case series treated 49 patients with thiopurines for 4 months, and a complete response was seen in 43%, while a partial response was seen in 22%. Thirty-five percent of patients experienced adverse events leading to cessation of therapy.Citation72
The use of methotrexate in MC has had conflicting results. In a study of 19 patients with CC naïve to budesonide treated with methotrexate 5–25 mg orally weekly, the median dose 7.5–10 mg, a complete response was seen in 14 patients and a partial response was seen in two patients.Citation73 In another study of nine patients with CC treated with methotrexate 15–25 mg subcutaneously weekly, not a single patient improved and four patients experienced adverse events leading to cessation of therapy.Citation74 A Mayo Clinic case series examined 12 patients treated with methotrexate (mix of subcutaneous and oral dosing) 25 mg/week, of which 7 (58%) achieved complete response, 2 (17%) achieved partial response, and 3 (25%) had no response.Citation72 Seventy-five percent of the patients in the Mayo Clinic cohort, however, were on concomitant budesonide therapy, limiting generalizability in the use of methotrexate as monotherapy. Given the conflicting reports on the efficacy of methotrexate in MC and the potential for significant adverse effects, further studies on methotrexate should be performed prior to recommending its use.
Calcineurin inhibitors have also been used in the treatment of MC. In one study, two patients were treated with calcineurin inhibitors (one with tacrolimus and one with cyclosporine), with one patient (tacrolimus) achieving complete response without the use of budesonide.Citation72 As this was the only article that included the use of calcineurin inhibitors, we do not recommend their use until more research is published.
Pentoxifylline
Pentoxifylline, a xanthine oxidase derivative with anti-tumor necrosis factor (TNF)-alpha properties, has been used in alcoholic hepatitis and intermittent claudication and may play a role in the treatment of MC according to a recent case report. Nine patients with MC either refractory to, intolerant of, or dependent on budesonide received pentoxifylline 400 mg three times a day for a median of 3 months. Complete response occurred in one patient (11%) and partial response occurred in three patients (33%); however, it should be noted that the one complete responder was intolerant to budesonide, leading the authors to surmise that this therapy could perhaps be used in patients intolerant to budesonide or those with a contraindication to its use.Citation72
Biologics
Overall, the use of anti-TNF-alpha drugs in MC can be considered for refractory cases as rescue therapy prior to surgical intervention.Citation2 As refractory MC is extremely uncommon, there is a lack of evidence on the use of anti-TNF-alpha therapy. What little data exist originates from case series involving adalimumab and infliximab. One such case series of ten patients (six with CC and four with LC) refractory to budesonide and immunomodulators prospectively evaluated adalimumab and infliximab at standard doses for inducing remission in inflammatory bowel disease.Citation2,Citation75 The study found that eight of ten patients achieved clinical and histologic remission as well as improvement in HRQOL.
The role of vedolizumab in the treatment of MC was highlighted in a case report of a 75-year-old woman with CC for 4 years who was refractory to budesonide and dependent on steroids. A standard induction dosing regimen was undertaken, and the patient experienced significant clinical improvement after two infusions, and histologic resolution was achieved at 3 months.Citation76 A recent case series of eleven cases of refractory MC (nine of eleven failed one immunosuppressant, ten of eleven failed at least one anti-TNF agent) treated with standard induction and maintenance dosing of vedolizumab (300 mg IV at weeks 0, 2, and 6, then every 8 weeks) observed clinical remission in five of eleven (45%) patients of whom 75% also had histologic remission.Citation77
Fecal transplant
Due to advances in the understanding of the gut microbiome, fecal transplant has become a new therapeutic avenue in disease such as Clostridium difficile. Its use in MC (specifically CC) has been examined in one case report of a patient refractory to budesonide who received three fecal transplants and achieved remission after the third for 11 months.Citation78 Interestingly, while the patient did ultimately relapse, she was then treated with budesonide with good clinical response, an effect that was unattainable prior to fecal transplant.
Surgery
The role of surgical management in MC is diminishing with considerable improvement and efficacy of available medical therapy. Nevertheless, it does have a role in severe and unresponsive MC.Citation39 Surgical therapy for MC includes ileostomy, subtotal colectomy, and ileal pouch anal anastomosis; however, data on this matter remain limited to individual reports.Citation41,Citation79,Citation80
Conclusion
MC is a disorder characterized by chronic diarrhea that is frequently encountered by gastroenterologists. The incidence and consequently awareness of this disease have been increasing. It is crucial to maintain a high index of suspicion in specific affected populations presenting with chronic diarrhea, particularly middle-aged women and the elderly, and to appropriately refer for colonoscopy with biopsy when needed. While there are two distinct histologic subtypes of MC, namely LC and CC, their clinical features and response to therapy do not differ significantly, and therefore, for the purposes of diagnosis and management, they can be treated as one entity of MC. While lifestyle modifications such as smoking cessation as well as a thorough medication review to remove potential triggers are beneficial, budesonide has been recommended by multiple international societies as the first-line therapy for the treatment of MC, replacing previous symptomatic-based therapies. Despite the high success rates with budesonide, there is a risk of relapse. Low-dose maintenance budesonide appears to be effective in treating relapsing MC, but further data are still needed. Alternative therapies have been described in MC, including methotrexate, mesalamine, antibiotics, and probiotics, but the limited available data thus far suggest these are not adequately effective. Cholestyramine may have a role in patients with concomitant bile acid malabsorption or in addition to mesalamine. The challenge arises with severe, budesonide-refractory disease. These patients may benefit from immunomodulators or anti-TNF-alpha therapy though more data, particularly randomized placebo-controlled trials, are necessary. Surgery may be considered a last resort in severe disease unresponsive to other aforementioned therapies. Lastly, the burgeoning field exploring the gut microbiome is on the horizon for potential use in budesonide-refractory patients, via fecal transplant, to enhance response to standard therapy or as a means of therapy in itself.
Disclosure
The authors report no conflicts of interest in this work.
References
- O’TooleAOptimal management of collagenous colitis: a reviewClin Exp Gastroenterol20169313926929656
- Fernández-BañaresFCasanovaMJArguedasYCurrent concepts on microscopic colitis: evidence-based statements and recommendations of the Spanish microscopic colitis groupAliment Pharmacol Ther201643340042626597122
- NguyenGCSmalleyWEVegeSSCarrasco-LabraAClinical Guidelines CommitteeAmerican gastroenterological association Institute guideline on the medical management of microscopic colitisGastroenterology2016150124224626584605
- TongJZhengQZhengQLoRShenJRanZIncidence, prevalence, and temporal trends of microscopic colitis: a systematic review and meta-analysisAm J Gastroenterol2015110226527625623658
- ZabanaYFerrerCAceitunoMSalasAFernández-BañaresFAdvances for improved diagnosis of microscopic colitis in patients with chronic diarrhoeaGastroenterol Hepatol201740210711626996466
- BohrJTyskCErikssonSAbrahamssonHJärnerotGCollagenous colitis: a retrospective study of clinical presentation and treatment in 163 patientsGut19963968468519038667
- MacaigneGLahmekPLocherCMicroscopic colitis or functional bowel disease with diarrhea: a French prospective multicenter studyAm J Gastroenterol201410991461147025001258
- BonderupOKNielsenGLDallMPottegårdAHallasJSignificant association between the use of different proton pump inhibitors and microscopic colitis: a nationwide Danish case-control studyAliment Pharmacol Ther201848661862530039564
- ChoiKAbu-SbeihHSamdaniRCan immune checkpoint inhibitors induce microscopic colitis or a brand new entity?Inflamm Bowel Dis201925238539330169584
- LucendoAJDrug exposure and the risk of microscopic colitis: a critical updateDrugs R D2017171798928101837
- VigrenLSjöbergKBenoniCIs smoking a risk factor for collagenous colitis?Scand J Gastroenterol201146111334133921854096
- KoskelaRMKarttunenTJNiemeläSEHuman leucocyte antigen and TNFalpha polymorphism association in microscopic colitisEur J Gastroenterol Hepatol200820427628218334870
- GreenPHYangJChengJAn association between microscopic colitis and celiac diseaseClin Gastroenterol Hepatol20097111210121619631283
- SonnenbergATurnerKOGentaRMAssociations of microscopic colitis with other lymphocytic disorders of the gastrointestinal tractClin Gastroenterol Hepatol201816111762176729535059
- BürgelNBojarskiCMankertzJZeitzMFrommMSchulzkeJDMechanisms of diarrhea in collagenous colitisGastroenterology2002123243344312145796
- BohrJJärnerotGTyskCJonesIErikssonSEffect of fasting on diarrhoea in collagenous colitisDigestion2002651303411961340
- UngKAGillbergRKilanderAAbrahamssonHRole of bile acids and bile acid binding agents in patients with collagenous colitisGut200046217017510644309
- JärnerotGBohrJTyskCErikssonSFaecal stream diversion in patients with collagenous colitisGut1996381154155
- MillienVRosenDHouJShahRProinflammatory sulfur-reducing bacteria are more abundant in colonic biopsies of patients with microscopic colitis compared to healthy controlsDig Dis Sci201964243243830324555
- BurkeKEAnanthakrishnanANLochheadPIdentification of menopausal and reproductive risk factors for microscopic colitis–results from the Nurses’ Health studyGastroenterology201815561764177530144433
- GentileNYenEFPrevalence, pathogenesis, diagnosis, and management of microscopic colitisGut Liver201812322723528669150
- NyhlinNWickbomAMontgomerySMTyskCBohrJLong-term prognosis of clinical symptoms and health-related quality of life in microscopic colitis: a case-control studyAliment Pharmacol Ther201439996397224612051
- KaneJSIrvineAJDerwaYFordACFatigue and its associated factors in microscopic colitisTherap Adv Gastroenterol20181111175628481879959
- KampEJKaneJSFordACIrritable bowel syndrome and microscopic colitis: a systematic review and meta-analysisClin Gastroenterol Hepatol201614565966826453949
- RothBGustafssonRJOhlssonBAuto-antibodies and their association with clinical findings in women diagnosed with microscopic colitisPLoS One201386e6608823776613
- WildtSNordgaard-LassenIBendtsenFRumessenJJMetabolic and inflammatory faecal markers in collagenous colitisEur J Gastroenterol Hepatol200719756757417556903
- FineKDOgunjiFGeorgeJNiehausMDGuerrantRLUtility of a rapid fecal latex agglutination test detecting the neutrophil protein, lactoferrin, for diagnosing inflammatory causes of chronic diarrheaAm J Gastroenterol1998938130013059707055
- ASGE Standards of Practice CommitteeSharafRNShergillAKEndoscopic mucosal tissue samplingGastrointest Endosc201378221622423867371
- MooreMColemanHGAllenPBLoughreyMBMicroscopic colitis: a population-based case series over a 9-year period in Northern IrelandColorectal Dis201820111020102729742325
- MacaigneGLahmekPLocherCOver 90% of cases of microscopic colitis can be diagnosed by performing a short colonoscopyClin Res Hepatol Gastroenterol201741333334028215538
- LangnerCAustDEnsariAHistology of microscopic colitis-review with a practical approach for pathologistsHistopathology201566561362625381724
- GuagnozziDLandolfiSVicarioMTowards a new paradigm of microscopic colitis: incomplete and variant formsWorld J Gastroenterol201622388459847127784958
- Fernández-BañaresFZabanaYAceitunoMRuizLSalasAEsteveMPrevalence and natural history of microscopic colitis: a population-based study with long-term clinical follow-up in Terrassa, SpainJ Crohns Colitis201610780581126818762
- TontiniGEPastorelliLSpinaLMicroscopic colitis and colorectal neoplastic lesion rate in chronic nonbloody diarrhea: a prospective, multicenter studyInflamm Bowel Dis201420588289124681653
- HjortswangHTyskCBohrJDefining clinical criteria for clinical remission and disease activity in collagenous colitisInflamm Bowel Dis200915121875188119504614
- ClaraAPMagnagoFDFerreiraJNGrilloTGMicroscopic colitis: a literature reviewRev Assoc Med Bras201662989590028001266
- MünchAAustDBohrJMicroscopic colitis: current status, present and future challengesJ Crohns Colitis20126993294522704658
- CotterTGBinderMLoftusEVDevelopment of a Microscopic Colitis Disease Activity Index: a prospective cohort studyGut201867344144627965284
- BohrJWickbomAHegedusANyhlinNHultgren HornquistETyskCDiagnosis and management of microscopic colitis: current perspectivesClin Exp Gastroenterol20148273284
- IngleSBAdgaonkarBDIngleCRHingeCMicroscopic colitis: common cause of unexplained nonbloody diarrheaWorld J Gastrointest Pathophysiol201451485324891975
- CotterTGPardiDSCurrent approach to the evaluation and management of microscopic colitisCurr Gastroenterol Rep2017192828265892
- MünchALangnerCMicroscopic colitis: clinical and pathologic perspectivesClin Gastroenterol Hepatol201513222823624407107
- McKeageKGoaKLBudesonide (Entocort EC capsules): a review of its therapeutic use in the management of active Crohn’s disease in adultsDrugs200262152263228212381231
- MiehlkeSMadischAKupcinskasLBudesonide is more effective than mesalamine or placebo in short-term treatment of collagenous colitisGastroenterology201414651222123024440672
- BaertFSchmitAD’HaensGBudesonide in collagenous colitis: a double-blind placebo-controlled trial with histologic follow-upGastroenterology20021221202511781276
- BonderupOKHansenJBBirket-SmithLVestergaardVTeglbjaergPSFallingborgJBudesonide treatment of collagenous colitis: a randomised, double blind, placebo controlled trial with morphometric analysisGut200352224825112524408
- MiehlkeSHeymerPBethkeBBudesonide treatment for collagenous colitis: a randomized, double-blind, placebo-controlled, multicenter trialGastroenterology2002123497898412360457
- MiehlkeSMadischAKarimiDBudesonide is effective in treating lymphocytic colitis: a randomized double-blind placebo-controlled studyGastroenterology200913672092210019303012
- PardiDSLoftusEVTremaineWJSandbornWJT1193 a randomized, double-blind, placebo-controlled trial of budesonide for the treatment of active lymphocytic colitisGastroenterology20091365A-519A-520
- ChandeNAl YatamaNBhanjiTInterventions for treating lymphocytic colitisCochrane Database Syst Rev20177CD00609628702956
- MünchABohrJMiehlkeSBUC-63 investigatorsLow-dose budesonide for maintenance of clinical remission in collagenous colitis: a randomised, placebo-controlled, 12-month trialGut2016651475625425655
- MiehlkeSAustDMihalyEEfficacy and safety of budesonide, vs mesalazine or placebo, as induction therapy for lymphocytic colitisGastroenterology201815561795180430195447
- BolandKNguyenGCMicroscopic colitis: a review of collagenous and lymphocytic colitisGastroenterol Hepatol (N Y)2017131167167729230146
- Fernandez-BañaresFPiquerasMGuagnozziDCollagenous colitis: requirement for high-dose budesonide as maintenance treatmentDig Liver Dis201749997397728457904
- DeCorteTJanssensEThorrezKBeclomethasone dipropionaat is effective for microscopic colitis: results of an open-label multicentre study (COLCO)European Crohn’s and Colitis Organisation Digital Oral Presentation Session 4: Practicalities of IBD Patient Care2018Vienna, Austria
- MunckLKKjeldsenJPhilipsenEFischer HansenBIncomplete remission with short-term prednisolone treatment in collagenous colitis: a randomized studyScand J Gastroenterol200338660661012825868
- GentileNMAbdallaAAKhannaSOutcomes of patients with microscopic colitis treated with corticosteroids: a population-based studyAm J Gastroenterol2013108225625923295275
- MunckLKieldsenJFischer HansenBIncomplete remission with short-term prednisolone treatment in collagenous colitis: a randomized studyScand Gastroenterol2003386606610
- FineKLeeELafonGRandomized double-blind, placebo-controlled trial of bismuth subsalicylate for microscopic colitisGastroenterology1999116A880
- GentileNMKhannaSLoftusEVTremaineWJKammerPPPardiDSSu1353 outcomes of patients with microscopic colitis treated with bismuth subsalicylateGastroenterology20151484S-483
- AmaroRPonieckaARogersAICollagenous colitis treated successfully with bismuth subsalicylateDig Dis Sci20004571447145010961728
- TillmanLADrakeFMDixonJSWoodJRReview article: safety of bismuth in the treatment of gastrointestinal diseasesAliment Pharmacol Ther19961044594678853750
- CalabreseCFabbriAAreniAMesalazine with or without cholestyramine in the treatment of microscopic colitis: randomized controlled trialJ Gastroenterol Hepatol200722680981417565633
- PardiDSRamnathVRLoftusEVTremaineWJSandbornWJLymphocytic colitis: clinical features, treatment, and outcomesAm J Gastroenterol200297112829283312425555
- MadischAMiehlkeSEicheleOBoswellia serrata extract for the treatment of collagenous colitis. A double-blind, random-ized, placebo-controlled, multicenter trialInt J Colorectal Dis200722121445145117764013
- WildtSMunckLKVinter-JensenLProbiotic treatment of collagenous colitis: a randomized, double-blind, placebo-controlled trial with Lactobacillus acidophilus and Bifidobacterium animalis subsp. lactisInflamm Bowel Dis200612539540116670529
- TrommANiewerthUKhouryMThe probiotic E. coli strain Nissle 1917 for the treatment of collagenous colitis: first results of an open-label trialZ Gastroenterol200442536536915136935
- RohatgiSAhujaVMakhariaGKVSL#3 induces and maintains short-term clinical response in patients with active microscopic colitis: a two-phase randomised clinical trialBMJ Open Gastroenterol201521e000018
- OlesenMErikssonSBohrJJärnerotGTyskCLymphocytic colitis: a retrospective clinical study of 199 Swedish patientsGut200453453654115016748
- PardiDSLoftusEVTremaineWJSandbornWJTreatment of refractory microscopic colitis with azathioprine and 6-mercaptopurineGastroenterology200112061483148411313319
- MünchAFernandez-BanaresFMunckLKAzathioprine and mercaptopurine in the management of patients with chronic, active microscopic colitisAliment Pharmacol Ther201337879579823432370
- CotterTGKambojAKHicksSBTremaineWJLoftusEVPardiDSImmune modulator therapy for microscopic colitis in a case series of 73 patientsAliment Pharmacol Ther201746216917428488312
- RiddellJHillmanLChiragakisLClarkeACollagenous colitis: oral low-dose methotrexate for patients with difficult symptoms: long-term outcomesJ Gastroenterol Hepatol200722101589159317845686
- MünchABohrJVigrenLTyskCStrömMLack of effect of methotrexate in budesonide-refractory collagenous colitisClin Exp Gastroenterol2013614915224039441
- EsteveMMahadevanUSainzERodriguezESalasAFernández-BañaresFEfficacy of anti-TNF therapies in refractory severe microscopic colitisJ Crohns Colitis20115661261822115383
- CushingKCMino-KenudsonMGarberJLochheadPKhaliliHVedolizumab as a novel treatment for refractory collagenous colitis: a case reportAm J Gastroenterol2018113463263329610507
- RivièrePMünchAMichettiPVedolizumab in refractory microscopic colitis: an international case seriesJ Crohns Colitis Epub20181017
- GünaltaySRademacherLHultgren HörnquistEBohrJClinical and immunologic effects of faecal microbiota transplantation in a patient with collagenous colitisWorld J Gastroenterol20172371319132428275312
- VargheseLGalandiukSTremaineWJBurgartLJLymphocytic colitis treated with proctocolectomy and ileal J-pouch-anal anastomosis: report of a caseDis Colon Rectum200245112312611786777
- YusufTESoemijarsihMArpaiaAGoldbergSLSottileVMChronic microscopic enterocolitis with severe hypokalemia responding to subtotal colectomyJ Clin Gastroenterol199929328428810509959