Abstract
Strongyloides stercoralis is an intestinal nematode that is able to infect the host tissue and persist asymptomatic for many years through autoinfection. It causes life-threatening hyperinfection in immunocompromised hosts. This report describes a rare case of strongyloidiasis in a 40-year-old male following renal transplant, which was diagnosed by colonoscopic biopsy. The literature on the subject is also reviewed.
Introduction
Strongyloides stercoralis is a soil-transmitted intestinal nematode that has been estimated to infect at least 60 million people, especially in tropical and subtropical regions.Citation1–Citation4 Many infected patients are completely asymptomatic and the infection can remain undetected for years. The uncomplicated intestinal form of the disease usually produces nonspecific abdominal symptoms with or without mild sporadic diarrhea. Strongyloides infection, in contrast, has been described in a variety of conditions including those on immunosuppressant therapy, post-transplantation, hematologic malignant disease, human immunodeficiency virus, malnutrition, diabetes mellitus, rheumatoid arthritis, chronic renal failure, hypogammaglobulinemia, and chronic alcohol consumption.Citation5–Citation18 In these patients, hyperinfection can occur, which, if not recognized and treated aggressively, can result in mortality rates as high as 87%.Citation1,Citation19 In humans, S. stercoralis infestation most commonly involves the upper small intestine and the usual clinical presentation is nonspecific and vague and the infestation can mimic several other conditions such as inflammatory bowel disease. Given the increasing numbers of immunocompromised individuals, physicians caring for these patients should be aware of this potential and sometimes fatal complication. This report describes a 40-year-old male who underwent renal transplant and developed colonic hyperinfection with S. stercoralis.
Case report
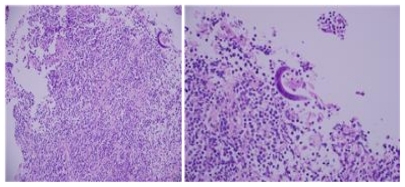
In 2008, a 40-year-old male was diagnosed with end-stage renal disease of unknown etiology and was started on regular hemodialysis. During this time he was also found to be hypertensive and was treated with antihypertensive medications. In February 2010, he underwent renal transplant after induction with antithymoglobulin. Four months after the operation, he started to complain of severe nausea, vomiting, and significant loss of weight. At the time of presentation, he was maintained on: tacrolimus 1 mg orally twice daily, mycophenolate mofetil 500 mg orally three times daily, prednisolone 5 mg orally once daily, esomeprazole 40 mg orally once daily, bisoprolol 5 mg orally once daily, methyldopa 500 mg orally three times daily, and calcitriol and cotrimoxazole 480 mg orally twice daily. His examination was normal apart from a palpable transplanted kidney in the right iliac fossa. Investigations showed a white blood cell count of 6.19 × 109/L; neutrophils 5.37 × 109/L (87.1%); eosinophils 2.5 × 109/L (0.15%); hemoglobin 10.4 g/dL; hematocrit 33.2%, with a mean cell volume of 80.1 and a mean cell hemoglobin of 26.2. His platelet count was 301 × 109/L, renal panel showed creatinine of 145 μmol/L, blood urea nitrogen 6.3 mmol/L, sodium 128 mmol/L, and potassium 3.7 mmol/L. He underwent upper gastrointestinal endoscopy, which showed mild gastritis, and the biopsy was negative for Helicobacter pylori. As there was no improvement on proton pump inhibitors and prokinetics, colonoscopy was performed. This revealed aphthoid-like ulcers at the rectum and rectosigmoid areas. The ascending colon showed mucosal segments with granularity, pin-point ulceration with fibrin deposits (see ), and bleeding on touch. The findings were suggestive of inflammatory bowel disease. However, the biopsy revealed focal nonspecific inflammation, with larva-like parasites spotted on rectal biopsy (see ). Fecal examination confirmed the presence of a large number of S. stercoralis. He was started on a 10-day course of albendazole 400 mg orally twice daily. His symptoms subsided and he gradually started gaining weight. Fecal examinations 2 and 4 weeks after the initiation of therapy were normal.
Discussion
S. stercoralis is an intestinal nematode of humans. Although most infected individuals are asymptomatic,Citation19,Citation20 S. stercoralis is capable of causing a fulminant illness that is often fatal if not recognized and treated. This is seen in certain conditions associated with a decrease in host immunity, including immunosuppressive therapy (particularly the use of glucocorticoids), hematological malignancies, bone marrow and renal transplants, human T-cell lymphotropic virus type 1 infection, human immunodeficiency virus infection, hypogammaglobulinemia, and malnutrition.Citation5–Citation18 Although various immunocompromising conditions have been associated with hyperinfection, steroids and human T-cell lymphotropic virus type 1 infection are the most consistent. In these conditions S. stercoralis causes hyperinfection.Citation1,Citation19 The patient discussed had a S. stercoralis hyperinfection following renal transplant. Of interest is that the majority of cases of hyperinfection with S. stercoralis that have occurred following organ transplant were seen in patients following renal transplant and most of these cases seem to have been precipitated by increased glucocorticoid doses in response to rejection.Citation8,Citation17 The authors’ patient did not show signs of rejection, but he was on glucocorticoid therapy and this probably contributed to the development of superinfection. Given the increasing numbers of immunocompromised patients throughout the world, this calls for a closer evaluation and observation of all conditions under which S. stercoralis infection becomes dangerous. This is of paramount importance to physicians caring for these patients, as early identification and treatment of those at risk is likely to decrease the morbidity and mortality associated with S. stercoralis superinfection.
S. stercoralis commonly causes gastrointestinal symptoms that are nonspecific and easily attributed to other diseases. This was the case in the patient discussed, who was complaining of nausea and vomiting only; the striking and alarming feature was the sudden and significant weight loss. This called for further investigation including colonoscopy, which showed features suggestive of inflammatory bowel disease. The diagnosis of S. stercoralis infection was made on colonic biopsy and subsequently on fecal examination. The definitive diagnosis of S. stercoralis infection depends on the demonstration of larvae in the feces or duodenal fluid. In uncomplicated cases, the intestinal worm load is low and larval output is minimal. A single fecal examination thus fails to detect larvae in up to 70% of cases.Citation21 Repeated fecal examinations increase the sensitivity of detection of S. stercoralis infection.Citation22 In immunocompromised patients, the autoinfective cycle of S. stercoralis can become amplified into a potentially fatal hyperinfection syndrome, characterized by increased numbers of infective filariform larvae in the feces.
Strongyloidiasis is a curable disease and early diagnosis and appropriate therapy with anthelmintics can reduce morbidity and mortality.Citation23–Citation27 Ivermectin, when compared with albendazole and thiabendazole, shows similar or better rates of larval clearance from feces with similar side effects but is much better tolerated and has become the treatment of choice. An important point which must be considered is the fact that hyperinfections are often complicated by infections caused by gut flora that gain access to extra-intestinal sites, presumably through gut ulcers induced by the filariform larvae. Gut flora can include Escherichia coli, Klebsiella pneumoniae, Proteus mirabilis, Pseudomonas spp, Enterococcus faecalis, coagulase-negative staphylococci, Streptococcus bovis, and Streptococcus pneumoniae. Patients on immunosuppressive therapy may also develop systemic candidemia in addition to enteric Gram-negative infections.
Disclosure
The authors report no conflicts of interest in this work.
References
- AltintopACakarBHokelekMBektasAYildizLKaraoglanogluMStrongyloides stercoralis hyperinfection in a patient with rheumatoid arthritis and bronchial asthma: a case reportAnn Clin Microbiol Antimicrob201092720849666
- RowlandsPCSpeechly-DickMEGrechPStrongyloidiasis of the colonBr J Radiol1990637526506522400885
- AlSammanMHaqueSLongJDStrongyloidiasis colitis: a case report and review of the literatureJ Clin Gastroenterol199928177809916676
- NamSCHanMHKimYSKumYSSuhISBaeHITwo cases of strongyloidiasis diagnosed by colonoscopic biopsyKorean Journal of Pathology200741343346
- AdamMMorganOPersaudCGibbsWNHyperinfection syndrome with Strongyloides stercoralis in malignant lymphomaBr Med J1973158482642664685318
- ArmignaccoOCapecchiADe MoriPGrilloLRStrongyloides stercoralis hyperinfection and the acquired immunodeficiency syndromeAm J Med19898622582643876
- Brandt de OliveiraRVoltarelliJCMeneghelliUGSevere strongyloidiasis associated with hypogammaglobulinaemiaParasite Immunol1981321651697243341
- BrinerJEckertJFreiDLargiaderFBinswangerUBlumbergAStrongyloidiasis following kidney transplantationSchweiz Med Wochenschr19781084216321637 German360382
- BussDHStrongyloides stercoralis infection complicating granulocytic leukemiaN C Med J19713272692745284284
- CahillKMShevchukMFulminant, systemic strongyloidiasis in AIDSAnn Trop Med Parasitol19969033133188758145
- CeledonJCMathur-WaghUFoxJGarciaRWiestPMSystemic strongyloidiasis in patients infected with the human immunodeficiency virus. A report of 3 cases and review of the literatureMedicine (Baltimore)19947352562637934810
- CohenJSpryCJStrongyloides stercoralis infection and small intestinal lymphomaParasite Immunol197912167178317839
- CoovadiaYMRajputMCBhanaRHDisseminated strongyloidiasis in a diabetic patientTrop Geogr Med19934541791808236470
- DaubentonJDBuysHAHartleyPSDisseminated strongyloidiasis in a child with lymphoblastic lymphomaJ Pediatr Hematol Oncol19982032602639628440
- DebusscheXToublancMCamillieriJPAssanROverwhelming strongyloidiasis in a diabetic patient following adrenocorticotropin treatment and keto-acidosisDiabetes Metab1988143294298
- de OliveiraLCRibeiroCTde MendesDMOliveiraTCCosta-CruzJMFrequency of Strongyloides stercoralis infection in alcoholicsMem Inst Oswaldo Cruz200297111912111992161
- DeVaultGAJrKingJWRohrMSLandreneauMDBrownSTMcDonaldJCOpportunistic infections with Strongyloides stercoralis in renal transplantationRev Infect Dis19901246536712201067
- GotuzzoETerashimaAAlvarezHStrongyloides stercoralis hyperinfection associated with human T cell lymphotropic virus type-1 infection in PeruAm J Trop Med Hyg19906011461499988339
- SiddiquiAABerkSLDiagnosis of Strongyloides stercoralis infectionClin Infect Dis20013371040104711528578
- KishimotoKHokamaAHirataTEndoscopic and histopathological study on the duodenum of Strongyloides stercoralis hyperinfectionWorld J Gastroenterol200814111768177318350608
- KooshaSFesharakiMRokniMBComparison of enzyme-linked immunosorbent assay and indirect immunofluorescence assay in the diagnosis of human strongyloidiasisIndian J Gastroenterol200423621421615627660
- HirataTNakamuraHKinjoNIncreased detection rate of Strongyloides stercoralis by repeated stool examinations using the agar plate culture methodAm J Trop Med Hyg200777468368417978071
- GroveDITreatment of strongyloidiasis with thiabendazole: an analysis of toxicity and effectivenessTrans R Soc Trop Med Hyg19827611141187080143
- DatryAHilmarsdottirIMayorga-SagastumeRTreatment of Strongyloides stercoralis infection with ivermectin compared with albendazole: results of an open study of 60 casesTrans R Soc Trop Med Hyg19948833443457974685
- MartiHHajiHJSavioliLA comparative trial of a single-dose ivermectin versus three days of albendazole for treatment of Strongyloides stercoralis and other soil-transmitted helminth infections in childrenAm J Trop Med Hyg19965554774818940976
- NandyAAddyMPatraPBandyopashyayAKFulminating strongyloidiasis complicating Indian kala-azarTrop Geogr Med19954731391417483007
- TorresJRIsturizRMurilloJGuzmanMContrerasREfficacy of ivermectin in the treatment of strongyloidiasis complicating AIDSClin Infect Dis19931759009028286637