Abstract
Background:
Performing experimental studies has played an important role in acquiring knowledge about esophageal carcinogenesis. In this context, the choice of a more reliable experimental model requires proof of its effectiveness in order to lend greater credibility to the results. The objective of this study was to evaluate the patency of duodenal-esophageal anastomosis during long-term postoperative follow-up in rats.
Methods:
This was an experimental study in which 45 female Wistar rats were used. A side-to-side anastomosis was performed, going from the anterior side of the esophagus to the second duodenal portion. A standardized radiological technique was used to carry out a contrasted radiological study of the esophagus, stomach, and duodenum during weeks 4, 12, 20, and 30 after surgery. Different contrast media were used, and the animals were divided into groups, ie, group 1 (100% barium sulfate), group 2 (50% barium sulfate), and group 3 (60% aqueous iodinated contrast media). Contrast radiographs were taken in each group at weeks 4, 12, 20, and 30 after the surgical procedure. The radiographic images were evaluated by two radiologists who were blinded regarding the contrast groups. Macroscopic evaluation of each animal was compared with the radiological findings.
Results:
Postoperative mortality was 13.33%. The remaining animals were divided into study groups. All the contrast radiological examinations showed evidence of the location of the esophagus, stomach, and proximal portion of the intestine, and demonstrated the laterolateral relationship of the distal esophagus and the duodenum in the epigastric region. Patency of the anastomosis was observed at each examination period. The different contrast media used were able to demonstrate this outcome shortly after the first phase of injection. Necropsies corroborated the radiological findings.
Conclusion:
Regardless of the contrast agent used, contrasted radiography revealed that side-to-side duodenal-esophageal anastomosis in rats allowed patent communication during long-term postoperative follow-up.
Introduction
Gastroesophageal reflux disease is a pathology that has attracted considerable interest, due to its prevalence and to the related clinical and surgical complications. Barrett’s esophagus is an acquired disease, often associated with the presence of chronic reflux.Citation1–Citation4 Despite other complications, this pathological condition may lead to metaplasia of the esophageal mucosa and is considered a precursor of adenocarcinoma.Citation5,Citation6
Recently, evidence of duodenal contents in the esophagus has been a determining factor in the development of a more complex subject associated with duodenal-gastroesophageal reflux (DGER), and it has thus been suggested that the term duodenal-gastroesophageal reflux disease is the most appropriate. The reverse pathway taken by these secretions implies failure of the lower esophageal sphincter and esophageal clearance. Increased pH values (over 7.0) are considered the causal factor behind several complications affecting the distal portion of the esophagus. Moreover, studies suggest that the presence of biliary salts and pancreatic juices may worsen the lesion.Citation7–Citation11
Experimental studies have been designed to evaluate the true role of duodenal reflux using surgical models to induce alkaline reflux in rats.Citation12–Citation15 The results of these studies have a potential role in directly influencing the future of DGER treatment. However, the effectiveness of the surgical model has never been satisfactorily established. When surgical effectiveness was evaluated, it was determined by necropsy after a period of exposure. This may be considered to be a confusing factor in interpreting the results obtained and thus lessen their importance.
Contrast radiographs of the upper gastrointestinal tract in Wistar rats were first described by Grossi et al.Citation15 These authors showed evidence of normal anatomical parameters in this line of rodents and thus made it possible for there to be a comparison regarding the findings of possible anatomical variables. Using an upper gastrointestinal radiological series, this study aimed to evaluate an alkaline reflux model in rats by demonstrating the patency of a pathway that was surgically induced in rats by duodenal-esophageal anastomosis over a long postoperative period.
Materials and methods
This study was conducted using an initial sample of 45 female Wistar rats (Rattus norvegicus) aged 56 days. The weight of the rats was 174–235 g. All animals were kept in cages containing five animals each, in a controlled temperature environment (22°C–24°C) under 12-hour dark:light cycles and with fresh air continuously pumped in. Water and feed were offered ad libitum. Feed and water were replaced twice a week, and cages were cleaned at the same interval. The animals were kept under these conditions until the end of the experiment. This study was performed by the Experimental Surgery Research Group at the Lutheran University of Brazil and was approved by the university ethics in research committee.
Surgical procedures
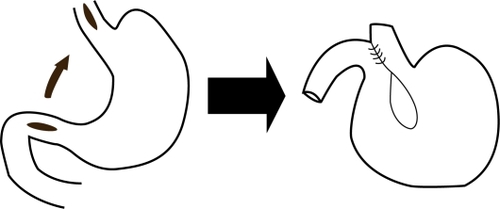
All the animals used in the present study underwent surgical duodenal-esophageal anastomosis. Feeding was suspended 8 hours before surgery, but free access to water was maintained. Anesthesia was achieved using a mixture of 20 mg of 2% xylazine and 50 mg of ketamine as intramuscular injections (0.1 mL/100 g body weight). The rats, which were deeply anesthetized by that time, were then positioned on the surgical table. The surgical section site was cleansed using iodine solution, and an abdominal trichotomy made. Sterilized sites were prepared and a median laparotomy with an incision 2–3 cm long was started. After gaining access to the abdominal cavity, the stomach was retracted and the first duodenal portion was identified. The abdominal segment of the esophagus was located by downward retraction of the larger curvature of the stomach. A size 4 French orogastric catheter was placed in the stomach until visualized, and remained in the gastric cardia throughout the experiment to avoid stenosis of the anastomosis.
In the next step, a transversal incision was performed in the duodenum 1.5 cm from the pyloric constriction. Another incision, this time a longitudinal one of the same size, was made at the anterior site of the terminal esophagus, 1 cm above the esophagogastric junction. The incisions were 1 cm in length, and this parameter was observed for all procedures. The upper and lower edges of each incision were repaired with Polypropylene 7-0 stitches, making it easier to bring the structures together. The same surgical thread was used to finalize the laterolateral duodenal-esophageal anastomosis. A running suture was performed joining the anterior and posterior edges of each incision (). Suture of the median line was performed using Polypropylene 6-0, and suture of the skin was done with Mononylon 5-0. After the surgical procedure was completed, the rats were rewarmed and placed in individual cages for the first 24 hours postoperatively. No water was offered for 6 hours, and their normal diet was resumed 24 hours after the surgery.
Radiological investigation
At weeks 4, 12, 20, and 30 after surgery, contrast radiographs of the upper gastrointestinal series were conducted to confirm surgical efficacy. Only one rat, which was selected at random from each group, was evaluated during the first three radiological examinations at weeks 4, 12, and 20. At the end of the study, considered to be postoperative week 30, all remaining rats were evaluated. The animals were placed in dorsal recumbency at a 45 degree angle to the horizontal plane of the radiological table. A size 4 French orogastric catheter was then inserted () and the position of the catheter was confirmed by radiograph to be in the anteroposterior direction.
Figure 2 Position of rats on the radiological table. A size 4 French orogastric tube is inserted and filled with barium contrast.

In the next step, the contrast medium was injected in three phases, observing the contrast regimen for each group. The volume of each injection was 0.3 mL, 0.6 mL, and 0.3 mL for the first, second, and third phases, respectively. A 5-minute interval was observed between each contrast injection, and immediately after each injection a radiograph was made in the anterior–posterior direction. This procedure included the possibility that when it was not possible to visualize the distal duodenum in the evaluation of the third radiograph, a fourth injection of 0.4 mL of contrast medium would have to be applied. When visualization of the distal duodenum was satisfactory, the rat was placed in the right lateral decubitus position to conduct the profile X-ray. The radiological parameters, which refer to the spectrum of radiation waves and the films used, were based on the initial description of the technique developed by Grossi et al.Citation15 The study sample was randomly divided into three groups that differed regarding the medium contrast used in the radiological study, ie, group 1 (100% barium sulfate, Bariogel, São Paulo, Brazil), group 2 (50% barium sulfate, with contrast medium diluted in 0.9% saline solution), and group 3 (meglumine diatrozate, ie, 60% aqueous iodinated contrast medium).
The examinations were evaluated by two experienced radiologists who were blinded regarding the contrast groups and presented reports of each examination with the aim of showing evidence of passage of the contrast medium through the duodenal-esophageal anastomosis. They also assessed which group showed the best quality regarding the images obtained.
Macroscopic evaluation
At the end of the radiological investigation, the animals were sacrificed by intracardiac injection of 10% potassium chloride whilst still deeply anesthetized. In the next step, necropsy was performed via a mentopubic incision. The structures were handled carefully, keeping the anatomical configuration.
The entire segment of the digestive tract stretching from the cervical esophagus to the proximal portion of the jejunum was removed for investigation. A size 4 French catheter was introduced to establish patent communication between the esophagus and stomach (physiological) and duodenum (surgically induced). The necropsy findings were compared with those of contrast radiography.
Results
The mortality rate observed was 13.33% (n = 6), and only immediately after surgery. The remaining 39 animals were randomly divided into the study groups. Group 1 comprised 15 animals and groups 2 and 3 comprised 12 animals each.
Radiological investigation
Contrast radiographs were conducted in all rats, and no complications were recorded. All animals remained alive under deep anesthesia and without complications throughout the radiological investigation. The anatomical pattern found in most cases defined the location of the stomach, taking in the epigastric, mesogastric, and left hypochondrial regions. The duodenum was located in the epigastric region, the right hypochondrium, the right flank, and the mesogastric region. The esophagus was located in the epigastric region. Evaluation of the radiographs showed evidence of a patent anastomosis shortly after the first phase of injecting the contrast medium, whereas in all the groups the medium used filled the distal esophagus up to the proximal portion of the duodenum (). The flow of the contrast medium through the anastomosis was located mainly in the epigastric region, right above the esophagogastric junction. The gastric cavity could only be visualized in subsequent examinations.
Figure 3 Patency of duodenal-esophageal anastomosis after injection of the first contrast volume (barium 100%). Evaluation at week 30.

The best image quality regarding intensity of the organ contrasted by totally filling with light, was observed in the group 1 animals. Group 3 was defined as the second option, according to the examiners’ judgment. Nevertheless, in terms of filling the gastric cavity, in group 1 it was satisfactorily contrasted only after the third contrast volume was injected, while in group 3 this level of contrast was achieved in all the animals only with the second contrast volume. In group 2, the contrast did not satisfactorily fill the gastric cavity, and reached the most distal portions of the small intestine in comparison with the other groups. The difference between the groups after the second contrast injection is shown in .
Figure 4 Comparison of animals of the three groups studied after the injection of the second contrast volume. Evaluation at week 30.
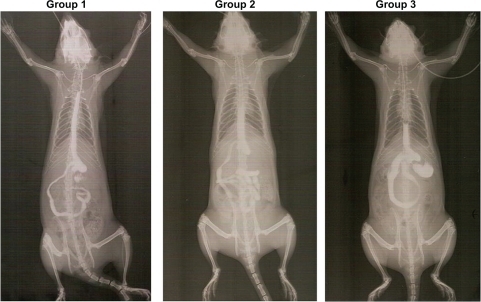
Profile radiography allowed confirmation of the patency of the anastomosis except for five cases, of which three were in group 3 and two were in group 2. In these, the course of flow between the esophagus and the duodenum could not be located due to overlapping of the intestinal loops along with the lesser intensity of the image. Patency was demonstrated in all group 1 animals ().
Necropsy
During investigation of the abdominal cavity, it was possible to observe formation of considerable adhesions at the anastomostic site. In all animals evaluated, the hepatic lobe adhered to the anterior portion of the abdominal esophagus. After complete removal of the adhesions, it was observed that the proximal portion of the duodenum remained aligned with the distal third of the esophagus.
The larger omentum was involved in all cases. The patency of the anastomosis was confirmed by passing a size 4 French catheter from the esophagus to the duodenum. With the exception of two animals, the catheter passed by the anastomosis with only slight handling of the tissues. In the other two cases, more difficulty in passing the catheter was encountered and more vigorous handling was necessary to allow passage of the catheter. Macroscopic examination demonstrated that there was patency of the anastomosis through the anterior opening of the organs. No anomalies suggesting a macroscopic lesion were observed at necropsy.
Discussion
Experimental models have been used to provide a better understanding of the mechanisms involved in carcinogenesis of the esophagus. Recent research has confirmed that reflux of the duodenal contents plays an important role in induction of esophageal cancer with or without exposure to a carcinogenic agent.Citation16–Citation19 Thus, this study was designed to assess the efficacy of surgical induction of reflux by duodenal-esophageal anastomosis in rats.
The surgical technique utilized by Melo et al in an experimental model to induce DGER was used successfully, producing significant results in the development of esophageal neoplasia without the use of a carcinogenic agent.Citation12 In that study, only animals exposed to reflux of duodenal contents actually developed carcinoma. On the other hand, in the experimental model used by Wetscher et al, gastrojejunal anastomosis associated with esophageal cardiomyotomy led only to gastric carcinoma, without evidence of neoplastic lesions in the esophagus.Citation14 The reason for these results might be related to stenosis of the esophageal cardiomyotomy, which may have prevented reflux in the esophageal mucosa. Nevertheless, this hypothesis has not been proven, and the evaluation was performed after the exposure period and only with the aim of evaluating histological changes in the esophageal mucosa, and not the patency of the anastomosis in the area in which myotomy was performed.
Gaia Filho et al proposed use of retrograde contrast injection to confirm DGER after cardiomyotomy.Citation20 Their results indicated that contrast medium was present in the esophagus in a considerable number of animals, but only in the group treated by total myotomy. These results showed evidence of an important index of error in surgical induction of DGER, and the radiological test was shown to be positive in 10% of the control cases. Furthermore, the radiological evaluation was intended to demonstrate the surgical effectiveness on postoperative day 30. Most studies assessing carcinogenesis in the esophagus have used longer periods of exposure to reflux, which may worsen the index of corroboration of reflux induction using this surgical method.Citation12–Citation14 In the studies evaluated, DGER seems to require a period of variable exposure to generate histological changes in the esophageal mucosa. Pera et al demonstrated that the presence of esophageal carcinoma is detectable as early as 20 weeks.Citation13 The series of radiological studies used in this research confirmed esophageal exposure to duodenal contents over a long postoperative period, suggesting that it is a suitable technique for studying the chronic effects of reflux on the esophageal mucosa.
Normal parameters of the radiological anatomy in rats, which has previously been described in the literature, make it possible to compare and find evidence of any structural alteration. Upon studying the initial description of the technique, which was developed by Grossi et al,Citation15 the authors of the present paper chose to use 100% barium sulfate as the contrast medium. This contrast medium is the one that is most commonly used for evaluating the gastrointestinal tract in humans.Citation21–Citation23 This study also evaluated two groups with less viscous contrast media. Due to its low viscosity, aqueous iodinated contrast medium (group 3) is an alternative to barium sulfate, albeit with precise indications. This contrast medium is used intravascularly for performing angiographic investigations. Studies performed in humans have demonstrated that iodinated contrast media are useful, especially in cases of larynx perforation.Citation24 Nevertheless, other studies have shown better results with barium sulfate than with iodinated contrast media for esophageal fistulae.Citation25,Citation26
In this study, the three contrast media used enabled identification of patency of the duodenal-esophageal anastomosis during defined exposure periods. Barium sulfate 100% showed greater efficiency in the generation of images, as judged by the radiologists. The gastric cavity was filled more easily in group 3 animals (iodinated contrast), although the present study did not aim primarily to assess the gastric cavity. It is possible that the difficulty observed in filling the stomach with contrast medium was due to the patency of the duodenal-esophageal pathway, which offers less resistant passage of contrast when compared with the resistance imposed by the lower esophageal sphincter. Therefore, when a study aims to detect duodenal-esophageal anastomosis patency, less contrast volume may be required to generate images of good diagnostic value. Furthermore, the use of less viscous contrast media may be useful to perform the evaluation and keep the animal alive without a high degree of impairment in gastrointestinal functioning. Such management can avoid the need for subsequent radiological evaluation during the follow-up period.
The results of the present study enable the conclusion that a side-to-side duodenal-esophageal anastomosis is patent in all the examinations conducted using contrast radiographs in the upper gastrointestinal series over a postoperative period of 4–30 weeks in rats. All contrasts used confirmed these outcomes. The choice of contrast agents tested should be made according to the properties of each one and the aim of the study.
Disclosure
The authors report no conflicts of interest in this work.
References
- BarrettNRChronic peptic ulcer of the esophagus and esophagitisBr J Surg19503817518214791960
- SpechlerSJBarrett’s esophagusSemin Oncol1994214314378042041
- BremmerCGLynchVPEllisFHJrBarrett’s esophagus: Congenital or acquired? An experimental study of esophageal mucosa regeneration in the dogSurgery19706820921610483471
- PetersFTMKleibeukerJHBarrett’s esophagus carcinomaScand J Gastroenterol1993285964
- DeMeesterTRAttwoodSEASmyrkTCTherkildsenDHHinderRASurgical therapy in Barrett’s esophagusAnn Surg19902125285422222018
- ThomasRMSobinLHGastrointestinal cancerJ Gastrointest Cancer199575Suppl154170
- AttwoodSEADeMeesterTRBremnerCGAlkaline gastroesophageal reflux: Implications in the development of complications in Barrett’s columnar-lined lower esophagusSurgery19891067647702799652
- AtwoodSEASmyrkTCDeMeesterTRDuodenoesophageal reflux and the development of esophageal carcinoma in ratsSurgery19921115035101598670
- IftikharSYLedinghamSSteeleRJBile reflux in columnar-lined Barrett’s oesophagusAnn R Coll Surg Engl1993754114168285543
- MiwaKHattoriTMiyazakiIDuodenogastric reflux and foregut carcinogenesisCancer199575142614327889469
- GillenPKeelingPByrnePJImplication of duodenogastric reflux in the pathogenesis of Barrett’s esophagusBr J Surg1988755405433395818
- MeloLLKruelCDPKliemannLMInfluence of surgically induced gastric gastroduodenal content reflux on esophageal carcinogenesis – experimental model in Wistar female ratsDis Esophagus19991210611510466042
- PeraMBritoMJPeraMDuodenal-content reflux esophagitis induces the development of glandular metaplasia and adenosquamous carcinoma in ratsCarcinogenesis2000211587159110910963
- WetscherGJHinderRASmyrkTGastric acid blockade with omeprazole promotes gastric carcinogenesis induced by duodenogastric refluxDig Dis Sci1999441132113510389684
- GrossiJVMNicolaRFBigolinAVDescription of the technique of upper gastrointestinal series radiological examination for the evaluation of the esophagus, stomach and duodenum of Wistar female ratsActa Cir Bras20092449049520011836
- GoldsteinSRYangCSKReuhlKLDevelopment esophageal metaplasia and adenocarcinoma in a rat surgical model without the use of the carcinogenCarcinogenesis199718226522709395230
- PeraMCardesaABombiJAInfluence of esophagojejunostomy on the induction of adenocarcinoma of the distal esophagus in Sprague-Dawley rats by subcutaneus injection of 2,6-dymethylnitrosomorpholineCancer Res198949680368082819720
- MiwaKSaharaGSegawaMReflux of duodenal or gastroduodenal contents induces esophageal carcinoma in ratsInt J Cancer1996672692748760598
- PeraMTrastekVFCarpenterHAInfluence of pancreatic and biliary reflux on the develop of esophageal carcinomaAnn Thorac Surg199355138613938512386
- Gaia FilhoEVGoldenbergACostaHOExperimental model of gastroesophageal reflux in ratsActa Cir Bras20052043744416302079
- CochranDQAlmondCHShucartWAAn experimental study of the effects of the barium and intestinal contents on the peritoneal cavityAm J Roentgenol Radium Ther Nucl Med196389883887
- NahrwoldDLIschJHBennerDAEffect of fluid administration and operation on the mortality rate in barium peritonitisSurgery1971707787815120900
- ShackletonKLStewartETHendersonJDEffect of barium sulfate on wound healing in the gastrointestinal tract on the ratRadiology200021456356710671612
- KeberleMWittenbergGTrusenAComparison of iodinated and barium-containing contrast media of different viscosity in the detection of pharyngeal perforationRofo2001173691695 German11570237
- FoleyMJGhahremaniGGRogersLFReappraisal of contrast media used to detect upper gastrointestinal perforations. Comparison of ionic water-soluble media with barium sulfateRadiology19821442312377089273
- BueckerAWeinBBNeuerburgJMEsophageal perforation: Comparison of use of aqueous and barium-containing contrast mediaRadiology19972026836869051016