Abstract
Aim and Background
TJ-100 is a traditional Japanese medicine that affects inflammation and gastrointestinal motility, and is used as a preventive and treatment for paralytic ileus. This study aims at determining the effect of TJ-100 on the peritoneal levels of IFN-γ/IL-9, cytokines related to ileus, after pancreaticoduodenectomy (PD) in a clinical setting.
Methods
This was a subsidiary study of the clinical trial investigating the effect of TJ-100 on postoperative bowel function. Ascites was collected from 180 patients using an abdominal drainage tube on postoperative day 1 and 3 after PD (POD 1 or POD 3) and used to measure 27 cytokines. We performed univariate and multivariate analyses using several perioperative variables and administration of TJ-100/placebo to determine the effect of TJ-100 on the levels of IFN-γ and IL-9.
Results
Peritoneal levels of IL-9 and IFN-γ decreased between POD 1 and 3 (Wilcoxon signed-rank test p<0.001). Multivariate analysis was performed after univariate analysis to select the variables and patients with a body mass index of ≥22 kg/m2, older age, use of epidural anesthesia, and longer surgery correlated with the levels of IL-9 and IFN-γ. However, we could not detect a correlation between the use of TJ-100 and cytokine levels in ascites either on POD 1 or 3.
Conclusion
TJ-100 did not affect peritoneal IL-9 and IFN-γ levels after PD. This was in accordance with published clinical findings showing no improvement in bowel function after PD and TJ-100 treatment.
Introduction
Cytokines regulate immune response and organ regeneration.Citation1–Citation3 Owing to this, cytokines and their receptors have gained importance as novel targets for disease control and/or treatment.Citation4–Citation6 Cytokine levels are investigated as potential biomarkers for postoperative complications, such as surgical site infection, anastomotic leakage,Citation7–Citation9 and postoperative ileus.Citation10
TJ-100 is a traditional Japanese herbal medicine that is used to treat conditions like paralytic ileus. The protective effect of TJ-100 on paralytic ileus after pancreaticoduodenectomy (PD) has been investigated by a multicenter randomized clinical trial. However, routine use of TJ-100 did not show any clinical benefits during the perioperative period.Citation11 Nevertheless, TJ-100 regulated the serum levels of interleukin (IL)‑4, IL‑9, IL‑10, PDGF-BB, and TNF-α in patients without severe inflammation.Citation12 This suggests that TJ-100 exerts its effects under specific conditions that should be further studied in the future.
In this study, we have measured peritoneal cytokine levels after PD to determine the effects of TJ-100. Since there is a correlation between IFN-γ and IL-9 levels and paralytic ileus, peristalsis, and bowel inflammation,Citation13–Citation18 we focused our study on IFN-γ and IL-9.
Methods
Trial Design and Patient Recruitment
The protocol employed in the main clinical trial has been previously described [10]. Patients undergoing PD for periampullary tumor or pancreas head tumors were assessed for eligibilities and enrolled. Patients were randomized according to four clinical variables that influence postoperative bowel movement. Five grams of TJ-100 (TJ-100 Group) or Placebo (Placebo Group) were administered three times per day 3 days before surgery until postoperative day (POD) 14. TJ-100 (alternative name, Daikenchuto) is composed of Japanese pepper (Zanthoxylum fruit), processed ginger (Zingiberis Siccatum Rhizoma), and ginseng (Ginseng radix).Citation19
Ascites was collected for a subsidiary study on POD 1 and 3 using an abdominal drainage tube. The samples were stored at lower than −70°C. Cytokine levels were measured by LSI Medience Corporation (Tokyo, Japan) using the Human Cytokine 27-plex assay (Bio-Rad Laboratories, California) and Bio-Plex 200 System (Bio-Rad Laboratories).
The institutional review board (IRB) of each participating institute approved the trial protocol after initial approval from the IRB of Wakayama Medical University (ID:1089). This study was conducted in accordance with the ethical principles of the Declaration of Helsinki. Patients provided written informed consent before randomization and intervention. Additional written informed consent was obtained for cytokine analysis. The study was registered at the UMIN Clinical Trial Registry (No. 000007975) and at ClinicalTrials.gov (No. NCT01607307).
Statistical Analysis
Values under the lower measurement limit were assigned the lower limit instead of discarding the data. The changes in the peritoneal levels of IL-9 and IFN-γ between samples from POD 1-3 and TJ-100/Placebo groups were assessed by the Wilcoxon signed-rank test.
The effect of TJ-100 on the peritoneal cytokine levels was studied using regression analysis. After log-transformation of the peritoneal IL-9 and IFN-γ levels, univariate regression analysis was performed to assess the correlation between the cytokines and variables. Variables used included the amount of TJ-100, age, gender, preoperative pathology, preoperative levels of gamma-glutamyl transpeptidase, estimated blood loss, length of surgery, presence of neoadjuvant chemotherapy, tumor stage, body mass index (BMI), use of epidural anesthesia, degree of lymph node dissection, presence of pancreatic fistula, and presence of abdominal abscess. Subsequently, we performed a multivariable regression analysis to determine the correlation between cytokine levels and use of TJ-100 and other factors chosen via univariate analysis with p-value <0.1. p-Value <0.05 was considered statistically significant.
Results
Patients
Drainage fluid was collected from 180 patients. The TJ-100 and Placebo group comprised 91 and 89 patients, respectively. We have previously summarized the clinical variables of these patients.Citation12 The tumor characteristics, operation variables, and patient characteristics were similar between the two groups. However, the mean age of the patients was slightly higher in the TJ-100 group than that of the Placebo group (64.9±8.0 vs 65.1±11.4, p=0.004, t-test).
Changes in Peritoneal IFN-γ and IL-9 Between Day 1 and 3
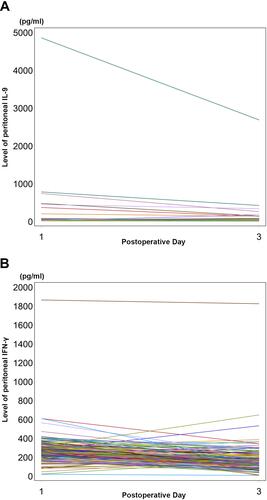
The median level of peritoneal IL-9 on POD 1 was 26.8 pg/mL (range: 10.2–4855.6 pg/mL) following which it decreased to 17.7 pg/mL (range: 10.2–2686.1 pg/mL) on POD 3 (Wilcoxon signed-rank test, p<0.001; ). The median level of peritoneal IFN-γ on POD 1 was 270.5 pg/mL (range: 19.0–1862.7 pg/mL) that decreased to 140.0 pg/mL (range: 6.5–1823.6 pg/mL) on POD 3 (Wilcoxon signed-rank test, p<0.001).
Figure 1 Peritoneal IL-9 and IFN-γ levels in patients between postoperative days 1 and 3. IL-9 (A) and IFN-γ (B) levels decreased between POD 1 and 3 in individual measurements. The peritoneal IL-9 levels accumulated in a narrow range (A), while variety of the levels were observed in IFN-γ. The patient having a high IL-9 level was different from the patient having high IFN-γ level. These two patients did not have sever postoperative complications or significant preoperative clinical features related to inflammation.
Comparison of Cytokine Levels Between TJ-100 and Placebo Groups
There were no significant differences between peritoneal IL-9 and IFN-γ levels between the TJ-100 and Placebo groups through POD 1-3 (). Cytokine levels differed widely among individuals. The levels of peritoneal IL-9 in the TJ-100 group on POD 1 ranged between 10.2 and 4855.6 pg/mL, while that in the Placebo Group on POD 1 ranged between 10.2 and 738.2 pg/mL.
Table 1 Peritoneal Levels of IL-9 and IFN-γ Within the TJ-100 and Placebo Groups
Univariate and Multivariable Analyses for Regulatory Factors for IFN-γ and IL-9 Levels
Univariate regression analysis helped identify the factors influencing the peritoneal IL-9 through POD 1-3 (). On POD 1, patients younger than 65 years showed lower IL-9 levels than that in the other categories. Longer surgical time positively correlated with IL-9 levels. On POD 3, patients with higher BMI had lower IL-9 levels as compared to that in the patients from other categories. Other variables, including gender, preoperative pathology, preoperative level of gamma-glutamyl transpeptidase, presence of neoadjuvant chemotherapy, tumor stage, degree of lymph node dissection, presence of pancreatic fistula, and presence of abdominal abscess, did not correlate with the IL-9 levels through POD 1-3. Multivariable regression analysis suggested that patients with a BMI between 22 and <25 kg/m2 exhibited lower levels of IL-9 on POD 3.
Table 2 Univariate and Multivariate Regression Analyses for IL-9 Levels After Log Transformation
Based on the univariate regression analysis of IFN-γ levels (), patients between 65 and <70 years correlated with higher levels of IFN-γ on POD 1. Patients with surgical time >480 min also showed higher levels of IFN-γ ranging POD 1-3. The use of epidural anesthesia was associated with decreased levels of IFN-γ on POD 3. Using the multivariable analysis, longer surgical times also correlated positively with higher levels of IFN-γ between POD 1 and 3; the use of epidural anesthesia correlated with decreased levels of IFN-γ on POD 3.
Table 3 Univariate and Multivariate Regression Analyses for IFN-γ Levels After Log Transformation
However, we found no correlation between the use of TJ-100 and peritoneal levels of IL-9 or IFN-γ on POD 1 or 3 ( and ).
Discussion
In animal models, TJ-100 suppresses the expression of IFN-γ in target organs, thereby reducing bacterial translocationCitation17 or inflammation of the large bowel.Citation18 Suppressed IFN-γ is associated with postoperative ileus.Citation15 It has also been shown that IL-9 levels enhance intestinal muscle contractility.Citation10,Citation13 Therefore, we focused on these two cytokines despite the availability of the remaining 25 cytokines. We could not demonstrate that TJ-100 altered peritoneal cytokine levels after PD. The strong intervention with PD may be attributed to the discrepancy between the data from the animal models and this study. PD involves the manipulation of multiple organs, such as pancreas, stomach, small intestine, and gall bladder. We speculate that the intense stress associated with surgery may have masked the effects of TJ-100.
In this study, we found that the use of epidural anesthesia suppressed IFN-γ levels on POD 3. Previous reports have shown that the decreased expression of IFN-γ in target organs is related to reduced postoperative paralytic ileus.Citation15 Thus, the use of epidural anesthesia may have reduced paralytic ileus. However, our previous clinical study demonstrated that the use of epidural anesthesia is an independent risk factor for paralytic ileus after PD.Citation11 The discrepancy between the present findings and expected results from polished studies (increased IFN-γ in patients with epidural anesthesia) may suggest that paralytic ileus is influenced by multiple factors: IFN-γ levels may not be able to predict the occurrence of paralytic ileus after PD or control paralytic ileus.
This study has limitations, one of which is the lack of the cytokine measurement before surgery. Although collecting ascites before surgery is impractical in our setting, the data would allow us to understand the transition of the cytokine levels more clearly.
In conclusion, the present study did not demonstrate the effect of TJ-100 on peritoneal IL-9 and IFN-γ after PD. Thus, these cytokines may not be promising biomarkers or therapeutic targets of paralytic ileus.
Data Sharing Statement
All available data are described within this manuscript.
Ethics Approval and Consent to Participate
All patients provided written informed consent prior to study inclusion. The institutional review board of each participating institute approved the trial protocol.
Patient Consent for Publication
All patients provided written informed consent.
Disclosure
Yasuhiro Kodera reports personal fees from Taiho Pharma, personal fees from Chugai Pharma, personal fees from Lilly Japan, personal fees from Johnson & Johnson, personal fees from Takeda, personal fees from Yakult, personal fees from Otsuka, personal fees from Ono Pharma, personal fees from Covidien, personal fees from MSD, outside the submitted work. The authors declare that they have no other competing interests for this work.
Additional information
Funding
References
- Mardpour S, Hamidieh AA, Taleahmad S, Sharifzad F, Taghikhani A, Baharvand H. Interaction between mesenchymal stromal cell-derived extracellular vesicles and immune cells by distinct protein content. J Cell Physiol. 2019;234(6):8249–8258. doi:10.1002/jcp.27669
- Spangler JB, Moraga I, Mendoza JL, Garcia KC. Insights into cytokine-receptor interactions from cytokine engineering. Annu Rev Immunol. 2015;33(1):139–167. doi:10.1146/annurev-immunol-032713-120211
- Galun E, Axelrod JH. The role of cytokines in liver failure and regeneration: potential new molecular therapies. Biochim Biophys Acta. 2002;1592(3):345–358. doi:10.1016/S0167-4889(02)00326-9
- Patel S, Srivastava S, Singh MR, Singh D. Mechanistic insight into diabetic wounds: pathogenesis, molecular targets and treatment strategies to pace wound healing. Biomed Pharmacother. 2019;112:108615. doi:10.1016/j.biopha.2019.108615
- Greenbaum AM, Link DC. Mechanisms of G-CSF-mediated hematopoietic stem and progenitor mobilization. Leukemia. 2011;25(2):211–217. doi:10.1038/leu.2010.248
- McInnes IB, Buckley CD, Isaacs JD. Cytokines in rheumatoid arthritis - shaping the immunological landscape. Nat Rev Rheumatol. 2016;12(1):63–68. doi:10.1038/nrrheum.2015.171
- Matthiessen P, Strand I, Jansson K, et al. Is early detection of anastomotic leakage possible by intraperitoneal microdialysis and intraperitoneal cytokines after anterior resection of the rectum for cancer? Dis Colon Rectum. 2007;50(11):1918–1927. doi:10.1007/s10350-007-9023-4
- Bilgin IA, Hatipoglu E, Aghayeva A, et al. Predicting value of serum procalcitonin, C-reactive protein, drain fluid culture, drain fluid interleukin-6, and tumor necrosis factor-α levels in anastomotic leakage after rectal resection. Surg Infect (Larchmt). 2017;18(3):350–356. doi:10.1089/sur.2016.222
- Kimura F, Shimizu H, Yoshidome H, et al. Increased plasma levels of IL-6 and IL-8 are associated with surgical site infection after pancreaticoduodenectomy. Pancreas. 2006;32(2):178–185. doi:10.1097/01.mpa.0000202959.63977.5c
- Okada K, Kawai M, Hirono S, et al. Perioperative administration of Daikenchuto (TJ-100) reduces the postoperative paralytic ileus in patients with pancreaticoduodenectomy. Hepatogastroenterology. 2015;62(138):466–471.
- Okada K, Kawai M, Hirono S, et al., JAPAN-PD Investigators. Evaluation of the efficacy of Daikenchuto (TJ −100) for the prevention of paralytic ileus after pancreaticoduodenectomy: a multicenter, double-blind, randomized, placebo-controlled trial. Surgery. 2016;159(5):1333–1341. doi:10.1016/j.surg.2015.11.019
- Maeda H, Okada KI, Fujii T, et al. Transition of serum cytokines following pancreaticoduodenectomy: a subsidiary study of JAPAN-PD. Oncol Lett. 2018;16(5):6847–6853.
- Khan WI, Richard M, Akiho H, et al. Modulation of intestinal muscle contraction by interleukin-9 (IL-9) or IL-9 neutralization: correlation with worm expulsion in murine nematode infections. Infect Immun. 2003;71(5):2430–2438. doi:10.1128/IAI.71.5.2430-2438.2003
- Grohmann U, Van Snick J, Campanile F, et al. IL-9 protects mice from Gram-negative bacterial shock: suppression of TNF-alpha, IL-12, and IFN-gamma, and induction of IL-10. J Immunol. 2000;164(8):4197–4203. doi:10.4049/jimmunol.164.8.4197
- Engel DR, Koscielny A, Wehner S, et al. T helper type 1 memory cells disseminate postoperative ileus over the entire intestinal tract. Nat Med. 2010;16(12):1407–1413. doi:10.1038/nm.2255
- Kono T, Kaneko A, Hira Y, et al. Anti-colitis and -adhesion effects of Daikenchuto via endogenous adrenomedullin enhancement in Crohn’s disease mouse model. J Crohns Colitis. 2010;4(2):161–170. doi:10.1016/j.crohns.2009.09.006
- Yoshikawa K, Kurita N, Higashijima J, et al. Kampo medicine “Dai-kenchu-to” prevents bacterial translocation in rats. Dig Dis Sci. 2008;53(7):1824–1831. doi:10.1007/s10620-008-0281-3
- Iwasa T, Ogino H, Nakamura K, Ihara E, Akiho H, Takayanagi R. Feeding administration of Daikenchuto suppresses colitis induced by naive CD4+ T cell transfer into SCID mice. Dig Dis Sci. 2012;57(10):2571–2579. doi:10.1007/s10620-012-2218-0
- Kono T, Shimada M, Yamamoto M, et al. Complementary and synergistic therapeutic effects of compounds found in Kampo medicine: analysis of Daikenchuto. Front Pharmacol. 2015;6:159. doi:10.3389/fphar.2015.00159
