Abstract
Objective:
To perform and confirm a simplified diagnostic indicators scoring system for predicting peptic ulcer perforation (PUP).
Methods:
A case–control study was conducted including 812 consecutive patients with PUP from retrospective medical records. Each diagnostic indicator measurable at the time of admittance was analyzed by a multiple regression. Stepwise logistic regression was applied with backward elimination of statistically significant predictors from the full model, with P ≥ 0.05 for exclusion. The item scores were transformed from regression coefficients and computed to a total score. The risk of PUP was interpreted using total scores as a simple predictor. This system was internally validated in 218 consecutive patients and compared to existing systems.
Results:
A PUP risk score was determined from the diagnostic indicators associated with PUP: gender, age, nonsteroidal antiinflammatory drugs used, history of peptic ulcer, intense abdominal pain, guarding, X-ray free air positive, and referral from other hospitals. Item scores ranged from 0–6.0 and the total score ranged from 0–34.0. The area under the receiver operating characteristic curve shows that there was 91.73% accuracy in the total scores predicting the likelihood of PUP. The likelihood of PUP among low risk (scores <10.5), moderate risk (scores 11–21), and high risk (scores ≥ 21.5) patients was 0.13, 11.44, and 1.95, respectively.
Conclusion:
This scoring system is an effective diagnostic indicator for identifying the complex cases of PUP. It is a simple system and can help guide clinicians, providing them with a more efficient way to accurately subgroup patients while also reducing potential biases.
Introduction
Patient safety is attracting worldwide attention in all disciplines of medicine. Peptic ulcer perforation (PUP) is a major crucial complication of peptic ulcer.Citation1,Citation2,Citation4 PUP accounts for about 10%–15% of peptic ulcer patients and accounts for more than 70% of deaths.Citation1 The mortality rate after PUP is approximately 10%–15% upon delayed diagnosis.Citation2,Citation3,Citation5
Severe upper abdominal pain is the most prominent symptom of PUP. About half of patients with PUP usually present with nausea, vomiting reflex, and vomiting – mostly food debris and gastric juice mixed with blood or coffee-like liquid, and can lead to intestinal paralysis. Approximately 1–5 hours after perforation, a patient’s stomach content can spill into the abdominal cavity due to an increase in peritoneal exudates. This may provide varying degrees of relief from abdominal pain and abdominal tension, but the tenderness is still significant. At this point, it would be easy to misdiagnose. In the first 10–12 hours after perforation, with peritoneal exudates absorption and secondary bacterial infection, late diagnosis and treatment of patients infected with severe peritonitis can lead to chills, fever, or even toxic intestinal sepsis, and physicians must be highly vigilant to avoid death due to toxic shock.Citation6
The literature suggests that the diagnosis of PUP should rarely be made on the basis of physical examination,Citation5,Citation7 whereas in clinical practice, the diagnosis of PUP is mainly established by patient history, signs and symptoms, physical examination, radiology investigation, and laboratory findings.Citation1
A major limitation of scoring systems is their dependence on sophisticated methods, which may not be available in developing countries. A simplified diagnostic indicators scoring system for predicting PUP – which can be easily used in developing countries – is needed.
Materials and methods
Definition
The definition of PUP according to the International Statistical Classification of Diseases and Related Health Problems, 10th Revision includes gastric ulcer (coded K25, subcategories 25.1, 25.2, 25.5, 25.6) and duodenal ulcer (coded K26, subcategories 26.1, 26.2, 26.5, 26.6).Citation8 The subcategories are defined as acute with perforation, acute with both hemorrhage and perforation, chronic or unspecified with perforation, and chronic or unspecified with both hemorrhage and perforation, respectively.
Development of the scoring system
A case–control study was conducted using medical records of PUP patients (cases and controls) – enrolled between January 1, 2005 and December 31, 2008 – that were reviewed retrospectively. PUP patients aged ≥15 years who were hospitalized in Nakornping Hospital (Chiang Mai, Thailand) were included in the cases group of the study, while nonperforation patients were included in the control group. Invariably, the diagnosis for PUP was obtained during the postoperation diagnosis by surgeons. The PUP patients with malignant ulcers or trauma were excluded.
It was important to estimate a sufficient sample size to achieve adequate statistical power. To yield a significant finding at α = 0.05, β = 0.20, and minimum detectable odds ratio = 4.9, the best sample size required 812 cases. There were 406 cases in the medical records; therefore 406 controls were analytically selected from nonperforated peptic ulcer patients immediately before and after the cases. Patient characteristics of cases and controls were compared using Student t-tests and exact probability tests to determine their suitability for possible risk indicators. The diagnostic indicators computable at the time of admittance were designated and analyzed by a stepwise logistic regression to determine a set of statistically significant predictors. Mathematical predictors were divided into three levels; the cutoff points of which were clarified from the values that produced all statistically significant regression coefficients and the utmost area under the receiver operating characteristic (ROC) curve of the logistic regression model. Regression coefficients of all diagnostic indicator predictors were changed into item assigned scores, which were then built into a total score (diagnostic indicators score) for each item. The total scores signified the summary measure of risk for PUP. Total scores were then evaluated as the sole predictor in the logistic regression model.
Validation of the scoring system
The medical records of 218 patients aged ≥15 years who underwent PUP surgery at the same setting (Nakornping Hospital) between January 1, 2009 and December 31, 2009 were reviewed retrospectively. All patient profiles for the PUP operation were assessed. The patients in whom histological diagnosis confirmed a malignant lesion in the peptic ulcer area were excluded.
The research protocol was accepted by the Chiang Mai University’s Faculty of Medicine Research in Human Subjects Ethical Review Committee and the Director of Nakornping Hospital. Information was analyzed by using Stata® statistical software package version 11.0 for Windows (StataCorp LP, College Station, TX).
Results
Patient characteristics
There were statistically significant differences between cases and controls in female gender, median age, underlying illness (diabetes mellitus P < 0.001, hypertension P < 0.001, liver disease P < 0.001, renal disease P < 0.01, arthritis P = 0.013, and history of peptic ulcer P < 0.001), patient lifestyles (tobacco smoking P < 0.001, alcohol used P < 0.001, and nonsteroidal antiinflammatory drugs used P = 0.006), signs and symptoms (hematemesis P = 0.002, intense abdominal pain P < 0.001, tenderness P < 0.001, guarding P < 0.001, melena P < 0.001, and systolic blood pressure P < 0.001), laboratory investigations (blood urea nitrogen/creatinine ratio P < 0.001), radiological finding (X-ray with free air P < 0.001), and treatment role (referral from other hospitals P < 0.001) (). The backward stepwise logistic regression analysis was used to develop a logistic regression model. The eight risk predictors were gender, age, nonsteroidal antiinflammatory drugs used, history of peptic ulcer, intense abdominal pain, guarding, X-ray free air positive, and referral from other hospitals ().
Table 1 Characteristics of patients with peptic ulcer perforation (cases) and nonperforation (controls)
Table 2 Regression coefficient, risk ratio, and 95% confidence interval of diagnostic indicators for peptic ulcer perforation from logistic regression
Development of the risk score
A risk score was determined from these eight predictors to predict the risk for PUP. Numerical predictors were categorized into three levels. Substantially better outcomes were confirmed when a greater area under the ROC curve was obtained (94.46%). The regression coefficients were transformed by dividing with the smallest coefficient in the model (0.33) and rounded up to the nearest 0.5 to obtain item scores. Every item score ranged from zero up to 2.0 or 6.0. After item scores were added to get the total scores, they ranged from zero to 34 (). The area under the ROC curve shows that there was 91.73% accuracy in the total scores predicting the likelihood of PUP ().
Figure 1 Receiver operating characteristic curve of risk for peptic ulcer perforation predicted by risk scoring (curved line) and a 50% chance prediction (diagonal line).
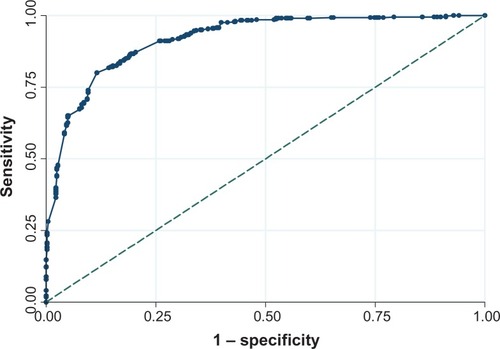
Table 3 Item scoring scheme for predictors of peptic ulcer perforation derived from coefficients of select diagnostic indicators
Validation of the scoring system
A graph mapping the proportion of PUP against total scores shows that the actual risk for higher total scores correlates well with the predicted risk from logistic estimation (). Classification of the validation cohort risk score resulted in three levels: low risk (scores < 10.5), moderate risk (scores 11–21), and high risk (scores ≥ 21.5). Of the cases that were classified as low risk, 10.16% had PUP, compared with 51.56% in the moderate-risk group and 38.28% in the high-risk group. Of the controls, 76.79% were categorized as low risk, 3.57% as moderate risk, and 19.64% as high risk. The intended likelihood ratio shows that low-risk cases were only 0.13 times more likely to result in PUP, while moderate-risk cases were 14.44 times, and high-risk cases were 1.95 times more likely to result in PUP. Even supposing that PUP occurs, the relationship between scores and treatment show that the higher scores have a higher likelihood of surgery ().
Figure 2 Score predicted risk (dots) and logistic estimated risk (solid line) of peptic ulcer perforation (%) for each total score.
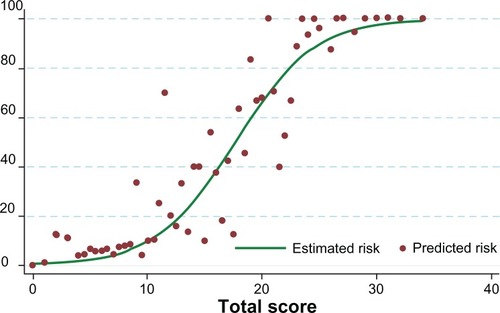
Table 4 Distribution of risk for perforation among patients with peptic ulcer perforation and nonperforation
Discussion
The development of a simplified diagnostic indicators score was based on the philosophy of clinical prediction rules applied to some areas in PUP,Citation9 such as a score to predict postoperative morbidity and mortality,Citation10–Citation13,Citation15 poor outcome,Citation14 and to compare with a validated risk score for PUP.Citation15
Clinicians and their team prefer to be able to precisely predict the presence or nonappearance of PUP. Statistical methods using logistic regression have estimated the risk of a variety of clinical outcomes.Citation10–Citation16 However, not one of these methods was relevant for estimating the risk of PUP in routine clinical practice. The process currently used to appraise the risk of PUP is very complicated. In the field, clinicians have been undergoing a paradigm shift recently as the importance of evidence is realized in practice.Citation1 Effective use of current evidence requires the clinician to draw on clinical experience and assess patient values as well as to collect, analyze, and implement the research into practice. The easy-to-use and proficient risk score for PUP might enable prompt identification of patients at high risk for PUP.
This report demonstrated a method for multivariable logistic regression analysis dividing the continuous variables into a dichotomous score yielding arithmetically identical estimates of risk. The benefit of the methodology over the typical appearance of logistic regression is that essentially anyone is able to estimate the risk of an event associated with given predictors. The risk score for predicting PUP was explained by an area under the ROC curve of 91.73%. The proportion of PUP increased sharply when the score increased from low risk to high risk.
An easy and realistic risk score was determined to predict the risk of PUP, which gained high prediction precision. To encourage the risk score to be successful in its forecasting, only the variables identifiable at the time of hospitalization were chosen.
This study demonstrated a simple and realistic method of computing the risk score to enable categorization of peptic ulcer patients into levels of PUP risk. The area under the ROC curve for PUP risk score was 91.73%. High prediction accuracy observed in this study was a result of the rigorous diagnostic indicators definition for PUP from a previous study to avoid misclassification.Citation1 It was previously known that when diagnostic indicators are transformed to a risk score, the prediction accuracy is reasonably reduced. The current study, using total scores to calculate risk, predicted PUP with an accuracy of 91.73% – a slight reduction from the unscored regression analysis which yielded an accuracy of 94.46%.
The combined results of studies suggest that the diagnostic indicators of patients are related to the multifactorial pathogenesis of peptic ulcer complications.Citation6 Older age groups and males were more likely to experience PUP last century, but that is now changing. In England, PUP most commonly affects young women.Citation18 In addition, the incidence of PUP across many countries has shown that a marked prognostic factor was patient history of peptic ulcer,Citation10,Citation11,Citation13,Citation16,Citation19 and the literature suggests a continuing increase in the use of non-steroidal antiinflammatory drugs.Citation1,Citation20
Delayed treatment of peptic ulcer patients who are referred from other hospitals with severe signs and symptoms may progress to gastrointestinal perforation. PUP at the anterior surface of the stomach is indicated by sudden intense abdominal pain. Posterior wall penetration leads to tenderness and guarding, which regularly radiates abdominal pain to the back. These variables reduce survival, increase poor clinical outcomes, and lengthen hospitalization.Citation6
It is appreciated that complications arising from perforation (eg, peritonitis) and mortality rates increase with delayed diagnosis. Higher rates of lethal outcomes in PUP emergency operations have been observed.Citation17
The diagnostic indicators score in the current study may also be used to classify patients with an increased likelihood of experiencing PUP in the future. The diagnostic indicators score might be useful for clinicians and nurses in developing countries in preparing for surgery. However, external validation of the scoring scheme will need to be applied to a different setting of PUP patients. This validation will be essential before any real use in applications such as clinical decision making and evaluation reviews of clinicians.
Additionally, the prediction rule is implemented as part of a critical pathway so that a hospital or clinic has procedures and policies established for how to manage patients identified as high or low risk for disease, which impact clinical outcomes. Therefore, the more intensively the prediction rule is implemented, the more benefits will occur. As a result, the risk of PUP may be predicted by a simplified score using eight predictors. Because of this, the risk score can accurately identify patients with low, moderate, and high risk.
Based on routine and intensive care in high-risk groups, the simplified prediction may bring some benefit, even though several studies have suggested that Helicobacter pylori colonizes the stomach and induces chronic gastritis and a long-lasting inflammation of the stomach.Citation19–Citation29 Additionally, H. pylori bacterium was first reported in the stomach and, along with acid secretion, can damage the tissue of the stomach and duodenum.Citation22 H. pylori causes inflammation and can develop into gastric and duodenal ulcer.Citation22,Citation23 H. pylori infection mutates host glycosylation and influences the pattern of putative colonization that is associated with lifetime risk of gastric perforation.Citation22 Studies have shown that H. pylori is etiologically linked to stomach cancer,Citation24–Citation27 and a study from India has shown that H. pylori infection is less common in more developed Asian nations.Citation24 Gastric cancer is common among ethnic Chinese with East Asian genotype.Citation25 H. pylori plays an important role in the pathogenesis of peptic ulcer disease, distal gastric adenocarcinoma, and gastric lymphoma in the United Kingdom and Hong Kong.Citation26,Citation27 Importantly, the exact role that H. pylori plays could not be established in the present study for two reasons. Firstly, during the 4-year study period (2005–2008), the H. pylori test was not well known in Thailand and was rarely ordered by doctors in cases of perforation. Secondly, about 70% of the patients required urgent or emergent surgery. Therefore, H. pylori was not detected in these patients.
A study from the 1950s found that the ABO blood group was associated with gastric diseases, and gastric cancer was found to be associated with blood group A in 1969.Citation29 Villalobos et al demonstrated that blood type O was associated with peptic ulcer in 1990.Citation30 The correlation between blood type A and gastric cancer has been confirmed and researchers have also confirmed that blood group O has a higher risk of peptic ulcers than those with other blood groups.Citation31 However, the ABO blood group variable was not used in the current analysis, as testing for blood type is not part of routine laboratory investigation and is therefore rarely noted in the medical records. Only subgroups who receive a blood transfusion are tested for blood type.
Study strengths and weaknesses
A strength of this study was that the simplified clinical prediction included predictor variables obtained from patient history, examination, and simple diagnostic tests, which can assist in making diagnosis appropriate management strategies.
A weakness of this study was that the retrospectively reviewed medical records were sometimes incomplete in regard to the patient’s lifestyle (eg, stress) and laboratory investigation (eg, glucocorticoids and ABO blood groups). These variables are major contributing factors to peptic ulcers and are interrelated to perforation.
Conclusion
This risk score might be relevant for clinicians and nurses to support them in early detection and treatment of patients who are at high risk for PUP. Consequently, the scoring scheme needs to be externally validated in independent patients who are undergoing PUP.
Acknowledgements
The authors would like to acknowledge the Nakornping Hospital health care team who granted access to patients’ information and for their contribution to the data collection.
Disclosures
The authors report no conflicts of interest in this work. This study was a part of Chutikarn Suriya’s PhD dissertation project in clinical epidemiology.
References
- KooJNganYKLamSKTrends in hospital admissions, perforation and mortality of peptic ulcer in Hong Kong from 1970 to 1980Gastroenterology1983846155815626840485
- MorrisAMidwinterMJPerforated peptic ulcerBrooksACottonBATaiNMahoneyPFEmergency SurgeryOxfordWiley-Blackwell20104345
- NoguieraCSilvaASSantosJNPerforated peptic ulcer: main factors of morbidity and mortalityWorld J Surg200327778278714509505
- KocerBSurmeliSSolakCFactors affecting mortality and morbidity in patients with peptic ulcer perforationJ Gastroenterol Hepatol200722456557017376052
- WayLWStomach and duodenumWayLWCurrent Surgical Diagnosis and Treatment10th edNorwalk, CTAppleton and Lange1994437459
- SilenWCope’s Early Diagnosis of the Acute Abdomen20th edNew York, NYOxford University Press2000
- FlasarMHGoldbergEAcute abdominal painMed Clin North Am200690348150316473101
- World Health OrganizationInternational Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10)GenevaWorld Health Organization1994
- GlynnPEWeisbachPCClinical Prediction Rules: A Physical Therapy Reference ManualSudbury, MAJones and Bartlett Publishers2011
- BoeyJWongJOngGBA prospective study of operative risk factors in perforated duodenal ulcersAnn Surg198219532652697059238
- LohsiriwatVPrapasrivorakulSLohsiriwatDPerforated peptic ulcer: clinical presentation, surgical outcomes, and the accuracy of the Boey scoring system in predicting postoperative morbidity and mortalityWorld J Surg2009331808518958520
- LeeFYLeungKLLaiBSNgSSDexterSLauWYPredicting mortality and morbidity of patients operated on for perforated peptic ulcersArch Surg20011361909311146785
- AriciCMesciADincerDDinckanAColakTAnalysis of risk factors predicting (affecting) mortality and morbidity of peptic ulcer perforationsInt Surg200792314715417972470
- EvansJPSmithRPredicting poor outcome in perforated peptic ulcer diseaseAust N Z J Surg199767117927959396997
- KocMYoldasOKilicYAComparison and validation of scoring systems in a cohort of patients treated for perforated peptic ulcerLangenbecks Arch Surg2007392558158517687581
- RajeshVChandraSSSmileSRRisk factors predicting operative mortality in perforated peptic ulcer diseaseTrop Gastroenterol200324314815014978992
- TestiniMPortincasaPPiccinniGLissidiniGPellegriniFGrecoLSignificant factors associated with fatal outcome in emergency open surgery for perforated peptic ulcerWorld J Gastroenterol20039102338234014562406
- CrispECases of perforation of the stomach with deductions there from relative to the character and treatment of that lesionLancet1843401040639649
- LanasAGarcia-RodriguezLAPolo-TomasMTime trends and impact of upper and lower gastrointestinal bleeding and perforation in clinical practiceAm J Gastroenterol200910471633164119574968
- RosenstockSJorgensenTBonnevieOAndersenLRisk factors for peptic ulcer disease: a population based prospective cohort study comprising 2416 Danish adultsGut200352218619312524398
- ChristensenSRiisANorgaardMSorensenHTThomsenRWShort-term mortality after perforated or bleeding peptic ulcer among elderly patients: a population-based cohort studyBMC Geriatr20077817439661
- KustersJGvan VlietAHKuipersEJPathogenesis of Helicobacter pylori infectionClin Microbiol Rev200619344949016847081
- NgCYSquiresTJBusuttilAAcute abdomen as a cause of death in sudden, unexpected deaths in the elderlyScott Med J2007521202317373420
- SinghKGhoshalUCCausal role of Helicobacter pylori infection in gastric cancer: an Asian enigmaWorld J Gastroenterol20061291346135116552799
- VilaichoneRKMahachaiVTumwasornSWuJYGrahamDYYamaokaYMolecular epidemiology and outcome of Helicobacter pylori infection in Thailand: a cultural cross roadsHelicobacter20049545345915361085
- McNamaraDEl-OmarEHelicobacter pylori infection and the pathogenesis of gastric cancer: a paradigm for host-bacterial interactionsDig Liver Dis200840750450918486572
- XiaBXiaHHMaCWTrends in the prevalence of peptic ulcer disease and Helicobacter pylori infection in family physician-referred uninvestigated dyspeptic patients in Hong KongAliment Pharmacol Ther200522324324916091062
- MatsudaRMorizaneTTsunematsuSKawanaITomiyamaMHelicobacter pylori prevalence in dentists in Japan: a seroepidemiological studyJ Gastroenterol200237425525911993508
- HavlikRJFeinleibMGarrisonRJKannelWBBlood-groups and coronary heart-diseaseLancet1969276142692704184130
- VillalobosJJVargasFVillarealHAA 10-year prolective study on cancer of the digestive systemRev Gastroenterol Mex19905511724 Spanish.2291062
- EdgrenGHjalgrimHRostgaardKRisk of gastric cancer and peptic ulcers in relation to ABO blood type: a cohort studyAm J Epidemiol2010172111280128520937632