Abstract
Background and Objectives
The success rate of Helicobacter pylori (H. pylori) eradication in China is declining. The aim of this study was to evaluate eradication outcomes in clinical practice and identifies factors contributing to treatment failure.
Methods
A retrospective review was conducted on patients treated for H. pylori infection with 14-day bismuth-containing quadruple therapy at a Beijing medical center from January 2020 to December 2023. We analyzed demographic and clinical data, eradication rates across regimens, and performed multivariate analysis to pinpoint predictors of failure.
Results
Out of 3340 participants, 2273 (68.1%) achieved eradication. Amoxicillin-based combinations (69.2%) outperformed other antibiotic regimens (58.9%, p < 0.001), with amoxicillin plus doxycycline reaching a 71.4% success rate. Esomeprazole-based regimens were more effective (73.6%) than other PPI regimens (65.2%, p = 0.001), notably, a rabeprazole, amoxicillin, doxycycline, and bismuth combination had an 80.0% success rate. Age, gender, and smoking and drinking were significant eradication failure predictors.
Conclusion
In real-world settings, 14-day amoxicillin and esomeprazole-based quadruple regimens have been demonstrated to be more effective than other regimens. Age, gender, and lifestyle habits are identified as independent risk factors for eradication failure.
Registration
This study was registered in the Chinese Clinical Trial Registry on 08/01/2024 (clinical trial registration number: ChiCTR2400079647).
Introduction
Helicobacter pylori (H. pylori), a bacterium capable of colonizing the human gastric mucosa, can establish a persistent infection that lasts a lifetime.Citation1 Epidemiological studies highlight its widespread impact, showing a prevalence rate of 24–50% in industrialized countries and up to 79% in developing regions.Citation2 The global health community recognizes H. pylori infection as a critical public health issue due to its association with several gastric pathologies, including gastritis, gastric ulcers, and atrophic gastritis leading to intestinal metaplasia.Citation3 Most notably, H. pylori is implicated as the primary risk factor in the etiology of gastric cancer, with chronic infection accounting for about 90% of all noncardia gastric cancer diagnoses.Citation4 There is compelling evidence to support the eradication of H. pylori as a cost-effective strategy for gastric cancer prevention, particularly when implemented before the onset of pre-neoplastic changes and in regions with high incidence rates.Citation5,Citation6
Triple therapy, comprising a proton pump inhibitor (PPI) alongside amoxicillin and either clarithromycin or metronidazole, has historically been the cornerstone of H. pylori eradication efforts, endorsed by a majority of consensus guidelines.Citation7 Despite its initial success rates surpassing 90% in the 1990s, efficacy has significantly waned to below 70% in recent years, a decline largely attributed to escalating antimicrobial resistance. This downturn is further exacerbated by the variable effectiveness of acid-suppressive medications.Citation8 In light of these challenges, contemporary guidelines have shifted towards advocating for a 14-day regimen that incorporates dual antibiotics, a PPI, and bismuth.Citation9 Currently, the antibiotic arsenal against H. pylori encompasses amoxicillin, metronidazole, clarithromycin, levofloxacin, furazolidone, and tetracycline. Pertinently, the fifth national consensus report from China (2016) delineated resistance rates to metronidazole, clarithromycin, and levofloxacin between 60%-70%, 20%-38%, and 30%-38%, respectively, whereas resistance to amoxicillin, furazolidone, and tetracycline remained comparatively low at 1%-5%.Citation10,Citation11 Despite these insights, a palpable void persists in large-scale, real-world eradication data within China, underscoring a pressing need for expansive studies. Such investigations are crucial for refining treatment protocols and enhancing clinical outcomes. Additionally, elucidating the influence of factors such as gastric acidity during treatment and patient demographics on eradication success warrants further exploration.
This study involved a review of medical records from a large group of patients diagnosed with H. pylori infection at the Civil Aviation General Hospital. We aimed to evaluate the success rate of H. pylori eradication treatments in the local population of Beijing, China, under real-world clinical conditions. Our research further sought to explore the factors that may contribute to the failure of these treatments. By doing so, we hope to shed light on the practical challenges faced in H. pylori management and suggest ways to enhance treatment efficacy.
Methods
Ethical Approval
This retrospective study was conducted in accordance with the Declaration of Helsinki and the guidelines of the Consolidated Standards of Reporting Trials (CONSORT). The study protocol was approved by the Institutional Ethics Board of the Civil Aviation General Hospital, Beijing, China (No. 2023-L-K-22). The trial was registered in the Chinese Clinical Trials Registration (www.chictr.org.cn) with the registration number ChiCTR2400079647. Because patient information was collected anonymously, the Institutional Ethics Board of the Civil Aviation General Hospital waived the need for individual informed consent.
Study Population and Data Collection
This study encompassed all patients identified with H. pylori infection via the electronic medical records system at the Civil Aviation General Hospital, Beijing, China, from January 2020 to December 2023. We extracted detailed patient information, including age, gender, prescribed treatment regimens, outcomes from the 13C/14C urea breath test (13C/14C-UBT), and endoscopic findings. Each patient’s data were anonymized and assigned a unique identifier to ensure privacy. Two independent clinicians verified the treatment regimens to ensure accuracy and consistency.
Inclusion Criteria: Availability of comprehensive general, clinical, and prescription data; confirmed diagnosis of H. pylori infection pre-treatment via the urea breath test, had no past history of H. pylori eradication; underwent a 14-day bismuth-containing quadruple therapy (PPI, bismuth, and two antibiotics) as the main empirical therapy for H. pylori eradication, according to the standard antibiotic combinations and dosages of the Fifth Chinese National Consensus Report on the management of Helicobacter pylori infection;Citation12 post-treatment confirmation of H. pylori eradication status with a urea breath test conducted 4–8 weeks after completing the therapy. Exclusion Criteria: Patients who were lost to follow-up or treatment regimens were altered; had received previous eradicated therapy once or more times; received additional drugs, including probiotics and/or traditional Chinese medicines.
Study Outcomes
Primary: The main outcome was the H. pylori eradication rate, determined by a negative 13C/14C-UBT result after at least four weeks post-quadruple therapy. The therapy combines two antibiotics, a PPI, and bismuth, aiming for H. pylori eradication. Secondary: identifying factors that contribute to eradication failure constituted the secondary outcome. This aspect involved examining various patient and treatment-related variables. For each patient group, eradication rates were computed as the ratio of patients with negative post-treatment 13C/14C-UBT results to the total patient count in the group. A detailed list of drugs used, including SFDA approval numbers and applications, is available in .
Table 1 The SFDA Approval Number and Usage of Different Drugs in This Study
Statistical Analysis
Data analysis was conducted using SPSS 26.0. For descriptive statistics, categorical variables were summarized as frequencies and percentages, while continuous variables were represented by mean values and standard deviations (SD). The analytical strategy involved employing Student’s t-test or one-way ANOVA for continuous data, depending on the distribution and homogeneity of variance, to identify significant differences. For categorical data, the χ2 (Chi-square) test was applied to assess the association between categorical variables. The Cochran-Armitage trend test was specifically used to evaluate the pattern of H. pylori eradication rates across various age demographics. To discern the predictive factors for H. pylori eradication failure, a stepwise logistic regression analysis was employed, with a significance threshold set at p < 0.05 to determine statistically significant.
Results
Patient Selection and Clinical Characteristics
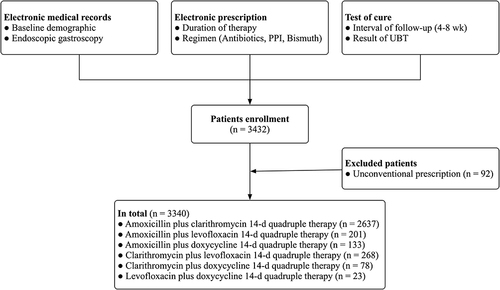
The study’s methodology and patient flow are illustrated in . Between January 2020 and December 2023, a cohort of 3432 patients tested positive for H. pylori underwent a 14-day quadruple therapy and were subsequently assessed using the 13C/14C-UBT 4–8 weeks post-therapy. Due to alterations in therapy regimens caused by drug intolerance, 92 patients were excluded from the study. Consequently, the final analysis included 3340 patients, comprising 1463 males and 1877 females. Clinical characteristics and demographic details are detailed in . The mean ages for the eradication-successful (negative) and -unsuccessful (positive) groups were 45.95±15.78 and 42.87±13.68 years, respectively. The study achieved an overall H. pylori eradication rate of 68.1%, with eradication being successful in 2273 patients and unsuccessful in 1067 patients. Significant differences in demographic characteristics such as age, gender, smoking, and drinking history were noted between groups (all p < 0.01). Gastroscopy results showed that 74.1% had chronic superficial gastritis, followed by chronic atrophic gastritis (10.2%), gastroduodenal polyps (6.7%), reflux esophagitis (3.8%), and gastroduodenal ulcer (3.6%), with no significant differences in these diagnoses between the eradication-successful and -unsuccessful groups (p > 0.05).
Table 2 Baseline Characteristics of Study Patients
Eradication Rates by Antibiotic Combination Regimens
delineates the eradication success rates across various antibiotic combination regimens. Notably, quadruple therapies incorporating amoxicillin demonstrated a significantly superior eradication rate (69.2%) compared to those without amoxicillin (58.9%, p < 0.001). Among these, the combination of amoxicillin and doxycycline outperformed others, achieving the highest eradication rate of 71.4%, followed by amoxicillin plus clarithromycin (70.3%), levofloxacin plus doxycycline (65.2%), clarithromycin plus levofloxacin (61.2%), amoxicillin plus levofloxacin (53.2%), and clarithromycin plus doxycycline (48.7%).
Table 3 Eradication Rates of Specific Eradication Regimens Classified by Antibiotic Combinations
Impact of Proton Pump Inhibitor Choice on Eradication Rates
Further analysis, as depicted in , revealed the influence of PPI selection on eradication outcomes. Esomeprazole-containing quadruple regimens were significantly more effective, with an eradication rate of 73.6%, compared to regimens based on other PPIs (65.2%, p = 0.001). Esomeprazole-based therapies led the efficacy chart at 73.6%, followed by rabeprazole (69.8%), ilaprazole (63.7%), and omeprazole (60.7%). A standout regimen combining rabeprazole, amoxicillin, doxycycline, and bismuth reported the highest eradication success at 80.0%, with esomeprazole, amoxicillin, clarithromycin, and bismuth regimens following at a 75.2% success rate ().
Table 4 Eradication Rates of Specific Eradication Regimens Classified by PPI
Table 5 Subgroups Comparison of Eradication Rates
Risk Factors Associated with H. pylori Eradication Failure
To discern the determinants of eradication failure, stepwise logistic regression analysis was employed, revealing significant variances across different demographic and behavioral factors. As delineated in , four primary factors exhibited a statistically significant association with eradication outcomes. A decrease in odds of eradication failure with increasing age was observed (AOR = 0.988, 95% CI: 0.983–0.993), indicating younger individuals had a higher risk of failure. Males had lower odds of eradication failure compared to females (AOR = 0.768, 95% CI: 0.650–0.908). Individuals with a history of smoking were significantly less likely to experience eradication failure (AOR = 0.212, 95% CI: 0.167–0.269). A history of alcohol consumption was associated with decreased odds of failure (AOR = 0.513, 95% CI: 0.411–0.640). All identified factors were statistically significant (all p < 0.01), underscoring their importance in influencing the success of H. pylori eradication efforts.
Table 6 Multivariate Analyses for Risk Factors of Eradication Failure
Discussion
In our extensive retrospective analysis, we scrutinized the efficacy of various 14-day quadruple therapies recommended for H. pylori eradication. The study’s findings illuminate the enhanced efficacy of amoxicillin-inclusive and esomeprazole-based quadruple regimens over alternative treatments. Notably, the regimen comprising rabeprazole, amoxicillin, and doxycycline was identified as particularly effective, achieving an 80% eradication rate. This highlights the potential of specific antibiotic combinations in optimizing treatment outcomes. Further insights were garnered from multivariate analysis, revealing that factors such as age, gender, smoking, and drinking histories significantly impact the risk of eradication failure. These findings underscore the necessity of considering patient-specific characteristics when planning H. pylori eradication strategies, suggesting a tailored approach may enhance treatment success rates.
A standard triple therapy, comprising of a PPI and two antibiotics (clarithromycin and amoxicillin), has been prescribed as a first-line regimen for H. pylori infection in China since 2011.Citation13 As the resistance of H. pylori to clarithromycin increases, the eradication rate of standard triple therapy has been reduced to an unacceptable level (eradication rate <80%), resulting in the widespread abandonment of this therapy.Citation14 The Maastricht V/Florence Consensus guideline recommended that in areas with high clarithromycin resistance (>15%), bismuth quadruple therapy should be used as the first-line eradication therapy, and in the fifth national consensus report on the treatment of H. pylori infection (in China, 2016), in which bismuth-containing quadruple therapy was recommended as a first-line treatment for H. pylori.Citation12 Our study unveiled a modest overall eradication rate of 68.1%, underscoring the limitations inherent in the empirical treatment regimens endorsed by current international guidelines. This adherence to empirical strategies, despite their convenience and cost-effectiveness, may not adequately address the clinical nuances of H. pylori treatment, particularly in the face of mounting antibiotic resistance. Meta-analyses have yet to firmly position susceptibility-guided treatment over empirical methods due to the former’s accessibility challenges.Citation15 While empirical regimens have been deemed cost-effective and relatively efficient,Citation16 our study did not evaluate antibiotic resistance in all participants, a notable limitation given the significant role of antimicrobial resistance in treatment failure.Citation17,Citation18 Antibiotic resistance emerges as an undeniable and critical one to achieving higher eradication rates, with patient compliance and environmental factors also influencing outcomes.Citation19 A questionnaire survey of 100 hospitals across China revealed that the application rate of bismuth-containing quadruple therapy was only 33% until 2017.Citation20 The reason for this is that the addition of bismuth to triple therapy has been found to reduce patient compliance due to the high frequency of adverse events, including vomiting, abdominal pain, black tongue, and diarrhoea.Citation21 Nevertheless, adding bismuth to triple therapy has been shown to counteract resistance, improving cure rates by 30–40% even amid rising antimicrobial resistance.Citation22 Our findings, particularly the 80.0% success rate with a rabeprazole-amoxicillin-doxycycline-bismuth regimen, indicate potential pathways to enhance eradication efforts. However, the limited sample size for this regimen calls for further research to validate its effectiveness broadly. The predominance of the esomeprazole-amoxicillin-clarithromycin regimen, despite its 75.2% eradication rate, highlights the pressing challenge of clarithromycin and levofloxacin resistance. Such resistance compromises the efficacy of adapted quadruple therapies, making the achievement of desired success rates (90% or higher) increasingly difficult. Our previous study demonstrated that the feasibility and high efficacy of using a real-time PCR assay on stool samples to detect H. pylori infection (kappa = 0.929, p < 0.001) and assess antibiotic resistance to clarithromycin (kappa = 0.788, p < 0.001) and levofloxacin (kappa = 0.739, p < 0.001) were comparable to those observed in gastric biopsy samples from the same patient.Citation23 This approach represents a compelling alternative to more invasive gastric biopsy, particularly in settings where endoscopy is less accessible or contraindicated. The use of non-invasive sample types has the potential to enhance patient compliance and therapeutic outcomes, thereby optimising the time and cost implications of disease management, particularly in the context of future increases in resistance rates.Citation24
According to the 2022 National Clinical Practice Guidelines issued by the Chinese Society of Gastroenterology, 14-day bismuth-containing quadruple therapy is recommended, boasting an average eradication rate of 81.3% to 83.6%.Citation25 Our study’s findings, highlighting a 70.3% eradication rate for the commonly used amoxicillin plus clarithromycin regimen, underscore the impact of antibiotic resistance on treatment efficacy. With macrolides and quinolones being among the most prescribed antibiotics in China from 2018 to 2020,Citation26 the resistance of H. pylori to clarithromycin, metronidazole, and levofloxacin has notably increased, reported at 30.0%, 70.0%, and 31.0%, respectively.Citation27 Conversely, resistance rates for amoxicillin, tetracycline, and furazolidone remain low, underlining the potential of these antibiotics in maintaining high eradication rates.Citation28 Given the growing concern over antibiotic resistance, alternative strategies such as high-dose PPI and amoxicillin dual therapy have gained attention for their potential to reduce unnecessary antibiotic use while maintaining efficacy.Citation29,Citation30 Our prior research supports this, demonstrating a 76.3% eradication rate with high-dose ilaprazole-amoxicillin dual therapy.Citation31 Furthermore, the advent of vonoprazan, a novel potassium-competitive acid blocker, offers a promising alternative with its superior gastric acid suppression capabilities.Citation32 Preliminary findings suggest that a vonoprazan and amoxicillin dual regimen can achieve eradication rates up to 87%,Citation33 indicating a strategic shift towards minimizing antibiotic resistance and treatment costs.
Consistent with earlier research, our study reinforces the critical function of acid-suppressive medications in H. pylori eradication protocols. Meta-analyses preceding our investigation have already established those therapies incorporating newer-generation PPIs, such as esomeprazole and rabeprazole, offer superior eradication outcomes compared to those utilizing first-generation PPIs like omeprazole.Citation34 In our cohort, esomeprazole-based regimens emerged as the predominant choice (33.8%), delivering an eradication rate of 73.6%, while rabeprazole-based therapies followed closely, achieving a 69.8% success rate. This distinction underscores the importance of selecting potent, advanced PPIs that provide robust gastric acid suppression, thereby enhancing antibiotic efficacy against H. pylori.Citation35 The efficacy of PPIs is partly determined by their ability to elevate gastric pH levels, rendering the bacteria more vulnerable to antibiotics such as amoxicillin and clarithromycin. Opting for a PPI that maintains consistent effectiveness regardless of CYP2C19 genotype variations is crucial for optimizing eradication rates.Citation36 Ilaprazole, an emerging PPI with primary metabolism via CYP3A, presents a novel alternative worth exploring further. Despite a 63.7% eradication rate observed with ilaprazole-based treatments in our study, this suggests a potential need for dosage adjustments to achieve optimal acid suppression and therapeutic outcomes.Citation37
The success of H. pylori eradication therapy is contingent upon a complex interplay of factors, including antibiotic susceptibility, the degree of acid secretion inhibition—which itself is influenced by the choice of PPI, its dosage, and the specific eradication regimen—and patient-related environmental factors. Notably, smoking has been identified as a detrimental factor; tobacco carcinogens inflict direct damage on the gastric mucosa, potentially prolonging H. pylori infections and diminishing the effectiveness of eradication treatments.Citation38 Moreover, a synergistic effect of smoking and alcohol consumption has been observed, with combined usage providing a more accurate prediction of eradication outcomes than either factor alone.Citation39 Our findings corroborate these observations, establishing a significant association between smoking, alcohol consumption, and H. pylori eradication rates. This underscores the necessity of considering these lifestyle factors in the management and treatment strategy for H. pylori, highlighting the need for a holistic approach to eradication that extends beyond pharmacological intervention.
This study’s retrospective nature introduces inherent constraints, notably in tracking patient adherence to medication and the impact of polypharmacy, which are pivotal in H. pylori eradication efforts. The complexity of multi-drug regimens, often required for effective treatment, poses a risk of diminishing patient compliance due to the burdensome nature of such therapies. Nevertheless, the completion of the urea breath test by all participants 4–8 weeks post-treatment may imply a commendable level of adherence among our study cohort. Further, the exclusion of certain patients based on predefined criteria may circumscribe the generalizability of our findings, potentially narrowing their applicability to the wider population. Additionally, the singular source of our data—a single medical center—coupled with inherent limitations in our hospital information system, restricts our ability to furnish a comprehensive portrayal of participant baseline characteristics. This limitation may impede the extrapolation of our results to different geographical contexts, where variations in resistance patterns could significantly influence eradication success. Moreover, the diminished sample sizes for specific treatment regimens, particularly those involving levofloxacin plus doxycycline and clarithromycin plus doxycycline, detract from the robustness of findings associated with these combinations. This limitation underscores the need for cautious interpretation of the efficacy associated with these less-represented regimens.
Conclusions
This study revealed an unsatisfactory H. pylori eradication rate in Beijing, China, emphasizing a pressing need for more effective and selective treatment strategies. Our analysis identified that quadruple regimens combining amoxicillin with doxycycline yielded the highest eradication rates, surpassing those regimens that included amoxicillin with clarithromycin. Notably, quadruple therapies based on esomeprazole demonstrated superior efficacy over those with omeprazole, underscoring the significance of selecting the most effective PPI in treatment protocols. The regimen incorporating rabeprazole, amoxicillin, doxycycline, and bismuth emerged as particularly potent, offering promising directions for optimizing H. pylori eradication approaches. These insights into the differential effectiveness of various antibiotic and PPI regimens provide a valuable foundation for enhancing treatment outcomes in clinical practice.
Ethics Approval and Informed Consent
The study was approved by the Institutional Ethics Board of the Civil Aviation General Hospital, Beijing, China (No. 2023-L-K-22) and was registered in the Chinese Clinical Trials Registration (www.chictr.org.cn) with the registration number ChiCTR2400079647. Due to the retrospective observational design of the study and that the study evaluated clinical practice there was no consent obtained from the patients.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
All of the authors declare that they have no conflicts of interest to disclose for this work.
Data Sharing Statement
Availability of data and materials Data are available from the corresponding author ([email protected]) on reasonable request.
Additional information
Funding
References
- Noto JM, Chopra A, Loh JT, et al. Pan-genomic analyses identify key Helicobacter pylori pathogenic loci modified by carcinogenic host microenvironments. Gut. 2018;67(10):1793–1804. doi:10.1136/gutjnl-2017-313863
- Khosravi Y, Loke MF, Goh KL, Vadivelu J. Proteomics analysis revealed that crosstalk between Helicobacter pylori and streptococcus mitis may enhance bacterial survival and reduces carcinogenesis. Front Microbiol. 2016;7:1462. doi:10.3389/fmicb.2016.01462
- Li N, Liu SF, Dong K, et al. Exosome-transmitted miR-25 induced by H. pylori promotes vascular endothelial cell injury by targeting KLF2. Front Cell Infect Microbiol. 2019;9:366. doi:10.3389/fcimb.2019.00366
- Watanabe M, Ito H, Hosono S, et al. Declining trends in prevalence of Helicobacter pylori infection by birth-year in a Japanese population. Cancer Sci. 2015;106(12):1738–1743. doi:10.1111/cas.12821
- Kakiuchi T, Okuda M, Hashiguchi K, Imamura I, Nakayama A, Matsuo M. Evaluation of a novel stool antigen rapid test kit for detection of Helicobacter pylori infection. J Clin Microbiol. 2019;57(3):e01825–18. doi:10.1128/jcm.01825-18
- Hussein KS. Hyperemesis gravidarum in first-trimester pregnant Saudi women: is Helicobacter pylori a risk factor? Front Physiol. 2020;11:575. doi:10.3389/fphys.2020.00575
- Zhu YJ, Zhang Y, Wang TY, et al. High dose PPI-amoxicillin dual therapy for the treatment of Helicobacter pylori infection: a systematic review with meta-analysis. Therap Adv Gastroenterol. 2020;13:1756284820937115. doi:10.1177/1756284820937115
- Gatta L, Vakil N, Vaira D, Scarpignato C. Global eradication rates for Helicobacter pylori infection: systematic review and meta-analysis of sequential therapy. BMJ. 2013;347:f4587. doi:10.1136/bmj.f4587
- Ailloud F, Didelot X, Woltemate S, et al. Within-host evolution of Helicobacter pylori shaped by niche-specific adaptation, intragastric migrations and selective sweeps. Nat Commun. 2019;10(1):2273. doi:10.1038/s41467-019-10050-1
- Kong S, Huang K, Wang J, et al. Efficacy of tailored second-line therapy of Helicobacter pylori eradication in patients with clarithromycin-based treatment failure: a multicenter prospective study. Gut Pathog. 2020;12:39. doi:10.1186/s13099-020-00378-1
- Liu DS, Wang YH, Zeng ZR, et al. Primary antibiotic resistance of Helicobacter pylori in Chinese patients: a multiregion prospective 7-year study. Clin Microbiol Infect. 2018;24(7):780.e5–780. doi:10.1016/j.cmi.2017.11.010
- Liu WZ, Xie Y, Lu H, et al. Fifth Chinese National Consensus Report on the management of Helicobacter pylori infection. Helicobacter. 2018;23(2):e12475. doi:10.1111/hel.12475
- Hu Q, Peng Z, Li L, et al. The Efficacy of berberine-containing quadruple therapy on Helicobacter Pylori eradication in China: a systematic review and meta-analysis of randomized clinical trials. Front Pharmacol. 2019;10:1694. doi:10.3389/fphar.2019.01694
- Liou JM, Chen CC, Chang CY, et al. Sequential therapy for 10 days versus triple therapy for 14 days in the eradication of Helicobacter pylori in the community and hospital populations: a randomised trial. Gut. 2016;65(11):1784–1792. doi:10.1136/gutjnl-2015-310142
- Muñoz N, Sánchez-Delgado J, Baylina M, et al. Systematic review, meta-analysis, and meta-regression: successful second-line treatment for Helicobacter pylori. Helicobacter. 2018;23(3):e12488. doi:10.1111/hel.12488
- Zhang XY, Shen WX, Chen CF, et al. Detection of the clarithromycin resistance of Helicobacter pylori in gastric mucosa by the amplification refractory mutation system combined with quantitative real-time PCR. Cancer Med. 2019;8(4):1633–1640. doi:10.1002/cam4.1986
- Pichon M, Pichard B, Barrioz T, et al. Diagnostic accuracy of a noninvasive test for detection of Helicobacter pylori and resistance to clarithromycin in stool by the amplidiag H. pylori+ClariR real-time PCR assay. J Clin Microbiol. 2020;58(4):e01787–19. doi:10.1128/jcm.01787-19
- Kuo CJ, Chen CW, Le PH, et al. Efficacy of dexlansoprazole-based triple therapy for Helicobacter pylori infections. Therap Adv Gastroenterol. 2019;12:1756284819870960. doi:10.1177/1756284819870960
- Emara MH, Mohamed SY, Abdel-Aziz HR. Lactobacillus reuteri in management of Helicobacter pylori infection in dyspeptic patients: a double-blind placebo-controlled randomized clinical trial. Therap Adv Gastroenterol. 2014;7(1):4–13. doi:10.1177/1756283x13503514
- Xie C, Lyu NH. Advantages and disadvantages of Helicobacter pylori eradication in Chinese patients. Zhonghua Nei Ke Za Zhi. 2017;56(5):327–330. doi:10.3760/cma.j.issn.0578-1426.2017.05.003
- Graham DY, Lee SY. How to effectively use bismuth quadruple therapy: the good, the bad, and the ugly. Gastroenterol Clin North Am. 2015;44(3):537–563. doi:10.1016/j.gtc.2015.05.003
- Chen Y, Liu Q, Hu F, Ma J. Identifying the best regimen for primary eradication of Helicobacter pylori: analysis of 240 cases. Microbiologyopen. 2020;9(11):e1120. doi:10.1002/mbo3.1120
- Fan CJ, Li Z, Zhai LL, et al. Diagnostic accuracy of a real-time PCR assay for detection of Helicobacter pylori and resistance to clarithromycin and levofloxacin directly from stool. Eur Rev Med Pharmacol Sci. 2024;28(12):3836–3840. doi:10.26355/eurrev_202406_36460
- Lehours P, Mégraud F. Culture-based antimicrobial susceptibility testing for Helicobacter pylori. Methods Mol Biol. 2021;2283:45–50. doi:10.1007/978-1-0716-1302-3_6
- Zhou L, Lu H, Song Z, et al. 2022 Chinese national clinical practice guideline on Helicobacter pylori eradication treatment. Chin Med J. 2022;135(24):2899–2910. doi:10.1097/cm9.0000000000002546
- Lee YC, Dore MP, Graham DY. Diagnosis and treatment of Helicobacter pylori infection. Annu Rev Med. 2022;73:183–195. doi:10.1146/annurev-med-042220-020814
- Chang YL, Tung YC, Tu YK, et al. Efficacy of second-line regimens for Helicobacter pylori eradication treatment: a systemic review and network meta-analysis. BMJ Open Gastroenterol. 2020;7(1). doi:10.1136/bmjgast-2020-000472
- Hu S, Zhou Y, Deng Y, et al. Characteristics of phenotypic antibiotic resistance of Helicobacter pylori and its correlation with genotypic antibiotic resistance: a retrospective study in Ningxia. Helicobacter. 2023;28(3):e12960. doi:10.1111/hel.12960
- Quera R, Córdova A, Núñez P, von Muhlenbrock C. Effectiveness and safety of high-dose dual therapy PPI-amoxicillin dual therapy for first-line Helicobacter pylori in Chile: experience from the retrospective study. Gastroenterol Hepatol. 2023;46(10):806–808. doi:10.1016/j.gastrohep.2022.12.001
- Bi H, Chen X, Chen Y, et al. Efficacy and safety of high-dose esomeprazole-amoxicillin dual therapy for Helicobacter pylori rescue treatment: a multicenter, prospective, randomized, controlled trial. Chin Med J. 2022;135(14):1707–1715. doi:10.1097/cm9.0000000000002289
- Cheng J, Fan C, Huang K, et al. Efficacy and safety of high-dose ilaprazole-amoxicillin dual therapy for Helicobacter pylori eradication: a prospective, single-center, randomized trial. Front Pharmacol. 2023;14:1272744. doi:10.3389/fphar.2023.1272744
- Chey WD, Mégraud F, Laine L, López LJ, Hunt BJ, Howden CW. Vonoprazan triple and dual therapy for Helicobacter pylori infection in the United States and Europe: randomized clinical trial. Gastroenterology. 2022;163(3):608–619. doi:10.1053/j.gastro.2022.05.055
- Suzuki S, Gotoda T, Kusano C, et al. Seven-day vonoprazan and low-dose amoxicillin dual therapy as first-line Helicobacter pylori treatment: a multicentre randomised trial in Japan. Gut. 2020;69(6):1019–1026. doi:10.1136/gutjnl-2019-319954
- Yan TL, Gao JG, Wang JH, Chen D, Lu C, Xu CF. Current status of Helicobacter pylori eradication and risk factors for eradication failure. World J Gastroenterol. 2020;26(32):4846–4856. doi:10.3748/wjg.v26.i32.4846
- Kadkhodaei S, Siavoshi F, Foroumadi A, Sarrafnejad A, Kolahdoozan S. Proton pump inhibitor-treated H. pylori adjust cell envelope fatty acid and cholesterol content to survive. Arch Iran Med. 2020;23(1):7–14.
- Zhao X, Zhang Z, Lu F, et al. Effects of CYP2C19 genetic polymorphisms on the cure rates of H. pylori in patients treated with the proton pump inhibitors: an updated meta-analysis. Front Pharmacol. 2022;13:938419. doi:10.3389/fphar.2022.938419
- Niu M, Zhou Y, Xie Y, et al. Comparison of the dual therapy of ilaprazole-amoxicillin and the bismuth quadruple therapy of ilaprazole-amoxicillin-furazolidone-bismuth glycyrrhizinate for eradication of Helicobacter pylori. Front Pharmacol. 2022;13:771876. doi:10.3389/fphar.2022.771876
- Camargo MC, Koriyama C, Matsuo K, et al. Case-case comparison of smoking and alcohol risk associations with Epstein-Barr virus-positive gastric cancer. Int J Cancer. 2014;134(4):948–953. doi:10.1002/ijc.28402
- Liao XM, Nong GH, Chen MZ, et al. Modified sequential therapy vs quadruple therapy as initial therapy in patients with Helicobacter infection. World J Gastroenterol. 2015;21(20):6310–6316. doi:10.3748/wjg.v21.i20.6310