Abstract
Chronic illness stigma is a global public health issue. Most widely studied in HIV/AIDS and mental illness, stigmatization of patients living with inflammatory bowel disease (IBD), chronic autoimmune conditions affecting the digestive tract, has garnered increasing attention in recent years. In this paper, we systematically review the scientific literature on stigma as it relates to IBD across its three domains: perception, internalization, and discrimination experiences. We aim to document the current state of research, identify gaps in our knowledge, recognize unique challenges that IBD patients may face as they relate to stigmatization, and offer suggestions for future research directions. Based on the current review, patients living with IBD may encounter stigmatization and this may, in turn, impact several patient outcomes including quality of life, psychological functioning, and treatment adherence. Significant gaps exist related to the understanding of IBD stigma, providing opportunity for future studies to address this important public health issue.
Introduction
Inflammatory bowel diseases (IBDs), which include Crohn’s disease (CD) and ulcerative colitis (UC), are chronic immune-mediated, inflammatory diseases of the digestive tract characterized by abdominal pain, rectal bleeding, diarrhea, and fatigue.Citation1 In some cases, extraintestinal symptoms such as eye or skin inflammation and joint pain are present.Citation2 Perianal fistulas occur in ~30% of IBD patients and may be a considerable source of distress.Citation3 Incidence and prevalence rates of IBD are increasing globally.Citation4 Treatment options for IBD include oral and injectable medications and intravenous infusions, often used in combination to induce remission as defined by symptoms, endoscopic appearance, and biomarkers.Citation1 Surgical interventions are common, with the cumulative risk for surgery 7 years after diagnosis being 29% for CD and 13% for UC.Citation5,Citation6
The physical, psychological, social, and financial ramifications of IBD are substantial, and the understanding of the role of illness stigma in these effects is minimal. Psychosocial functioning including reduced health-related quality of life,Citation7–Citation10 increased depression and anxiety,Citation11–Citation16 and relationalCitation17,Citation18 and social issuesCitation19 are common. These impacts can be due to the illness itself or side effects from some IBD medications (eg, corticosteroids) or surgery.Citation20,Citation21 Social withdrawals,Citation22 feelings of being different from others,Citation23–Citation25 and degradations in body imageCitation23,Citation26 have all been reported. Psychosocial impacts of IBD result in poorer patient reported outcomes including increased health care utilization,Citation27,Citation28 reduced treatment adherence,Citation29,Citation30 and increased disease activity.Citation31–Citation33
Financially, people living with IBD pay ~3,000 to 6,000 USD more annually for health care costs than those without IBD.Citation34 Aggregate annual estimates of total direct health care costs for IBD range from 500 million USD (UC) to 2.3 billion USD (CD).Citation35 Indirect costs from lost productivity and similar issues related to IBD are also in billions of dollars.Citation35–Citation37 Poor IBD self-management contributes to increased financial burdens, and improving illness self-management via improvements in IBD-related self-efficacy, streamlining communication between physician and patient, and increasing patient buy-in to treatments all demonstrate improvement in patient outcomes.Citation38–Citation41 While stigma has not been directly studied in relation to IBD self-management, it is associated with decreases in self-esteem and self-efficacyCitation42 suggesting that stigma may be associated with poorer disease management.
Chronic illness stigmatization, most notably characterized in mental healthCitation43–Citation45 and HIV/AIDSCitation46–Citation48 research, is a common and global social issue.Citation49 While the majority of research in this area is in the aforementioned conditions, other chronic illnesses such as cancers,Citation50–Citation52 hepatitis C,Citation53–Citation55 epilepsy,Citation56–Citation58 leprosy,Citation59–Citation61 and obesityCitation62–Citation65 have well-documented stigmatization. Illness stigma has a myriad of public health implications including limiting access to medical care, increasing treatment nonadherence, increased psychological distress, decreased self-esteem and self-efficacy, and increased illness symptoms.Citation66–Citation73 The construct of stigma has evolved since Erving Goffman’s seminal work defining stigma as a state of “spoiled identity” brought on being “deeply discredited” and socially rejected for having a particular trait.Citation74 In 2001, Link and PhelanCitation75 expanded the stigma model to include a convergence of labeling, prevailing cultural beliefs, disconnection of the stigmatized from others, and loss of social status combined with discrimination experiences. Research into stigma remains steady, with several hundred studies being published per year over the past decade.
Prevailing stigma theory delineates stigma into three domains: perceived or felt stigma, where the individuals sense that others hold negative attitudes or beliefs toward them or their condition; enacted stigma, or actual discriminatory experiences; internalized or self-stigma, or belief by the stigmatized individuals that negative attitudes or stereotypes about their condition are true and apply to them.Citation76 A fourth and adaptive domain, stigma resistance, has been captured via research utilizing the Internalized Stigma Scale for Mental Illness by Boyd et al.Citation77 In any particular individual, one to all four of these stigma domains may be at play, and the relationships between each and patient outcomes are well documented.Citation49,Citation70,Citation78–Citation81
Jones et alCitation82 identified six traits of a condition or trait that lend it to stigmatization: concealability, variability in course, aesthetic qualities, disruptiveness, origin, and perceived threat. Of these, the severity of the illness and a perception that the condition was caused by behavior of its bearer are most likely to predict stigmatization.Citation83 Based on these parameters, combined with the social taboo related to bowel symptoms in most cultures, IBD is susceptible to illness-related stigma. The severity of IBD varies by patient, but as a whole IBD is considered a serious illness with complex medical regimens to keep inflammation and symptoms in a state of remission, including the use of intravenous infusions (eg, infliximab and vedolizumab). While the etiology of IBD is better understood today as an immune-mediated disease, historically IBD was viewed as a psychosomatic illness with personality traits that made an individual susceptible to its occurrence. The notion that a person could develop CD due to “obsessional behavior” lends it to stigmatization.Citation84 Today, multiple triggers of disease onset and/or activity are identified including infection, antibiotic use, smoking, low mood, nonsteroidal anti-inflammatory drug use, and stress.Citation85 Perceived stress, negative mood, and stressful life events are often associated with IBD flares.Citation85 Identifying psychological reasons for disease activity is important, yet brings with it the potential for others to view IBD symptoms as under the person’s control due to a lack of ability to manage his or her psychological state or stress levels.
Initial inquiries into stigmatization of gastrointestinal illness occurred with the irritable bowel syndrome (IBS). Stigma studies in IBS find that a significant percentage of patients report some illness stigmatization.Citation86 However, differences in the etiology between IBS and IBD (ie, functional vs organic) lend themselves to potential differences in stigmatization.Citation87 Some patients with IBD are also diagnosed with IBS when their CD or UC is considered to be in remission via physiological markers yet the patient continues to exhibit symptoms.Citation88 Unfortunately, to date, no studies exist evaluating stigma experiences in IBD patients diagnosed with IBS. To date, no current reviews of illness stigmatization exist for IBD. In this review, we evaluate the three primary stigma domains and the relationship of each to patient outcomes, disease management, and course.
Systematic review
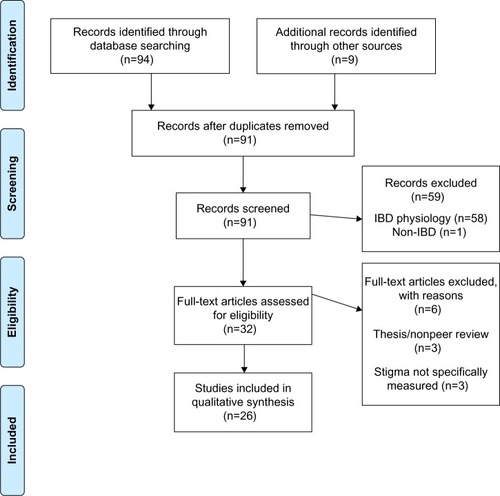
A literature search of studies published in English between 1985 and July 2015 was performed via the online databases PubMed, PsycINFO, and Google Scholar. The 1985 cutoff was selected based on the seminal Jones et al study which better defines stigma as it relates to chronic medical illness.Citation82 The following keyword combinations were used: 1) inflammatory bowel disease, Crohn’s Disease, ulcerative colitis combined using the “AND” operator with 2) stigma, stigmatized, stigmatization, discrimination, prejudice, stereotype, shame, bullying, blame, and teasing (eg, “Crohn’s disease” AND “stigmatization”). Article titles and abstracts were screened for relevance and full-text articles retrieved for a more detailed review. Reference lists of identified articles and book chapters were also reviewed for additional studies. Unpublished manuscripts and dissertations are not included. Articles identified via the database searches were reviewed by the authors for relevance to the stigma construct and those not specifically addressing stigma were removed from the final review. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram for the literature search is outlined in .
Identified studies
Twenty-six studies are reviewed. The majority was published in the USA and evaluate perceived stigma (15 studies). Four studies evaluate internalized stigma, five evaluate enacted stigma, and two evaluate more than one stigma domain. Adult and child/adolescent studies of stigma were included. Specific measures of health-related stigma are abundant and summarized elsewhere.Citation89 The findings are organized by the three stigma domains ().
Table 1 Relevant studies of inflammatory bowel disease (IBD) stigmatization
Perceived or felt stigma
The most widely studied of the stigma domains in IBD is perceived or felt stigma, with 84% of participants in a recent study reporting some perceived stigma.Citation42 Several studies report persons living with IBD having concerns about how others see them,Citation25,Citation26,Citation90 feeling different than others,Citation26 feeling shame,Citation91 and feeling discredited, including by medical providers.Citation26,Citation87 For example, hospitalized patients requiring pain management report being labeled as a difficult patient, needy, that they cannot tolerate pain properly, or are inappropriately seeking narcotic painkillers (ie, drug-seeking patients).Citation92 Fatigue is a commonly reported IBD symptom and patients report significant social impact with little understanding from their medical providers.Citation93 A follow-up inquiry by the same author with health care providers found that considerable frustration and difficulty in understanding IBD-related fatigue was common,Citation94 indicating a significant disconnect between providers and patients. Older patients, especially women and patients with UC, tend to report greater disease felt stigma as do patients with lower educational backgrounds.Citation95,Citation96 Stigma perceptions appear to be stable whether the disease is active or in remission and do not appear to vary between UC and CD.Citation23
As IBD is a concealable illness, the issue of disclosure is a salient concern for many patients. Individuals living with concealable conditions may opt to “pass” as someone without a chronic illness or “cover” by downplaying the severity of its symptoms.Citation97,Citation98 Most often, persons living with IBD report nondisclosure due to embarrassment related to its symptoms.Citation98 Fears of the threat of incontinence, bowel sounds, or urgency while in public can have significant negative impacts on patients’ social interactions, often leading to withdrawal and isolation as to protect themselves from potential shame.Citation26,Citation90 Passing can be challenging, especially when the patient must use the toilet multiple times per day,Citation98 so covering is more often employed especially to “safe others”. Guilt about being a burden to others and stoicism may also contribute to nondisclosure.Citation26,Citation99 Concealment is often associated with reduced communication, interactions, and transactions with others thereby increasing feelings of isolation and depression. Disclosure can yield positive results, providing a sense of relief from the stress of keeping IBD hidden and mitigating the effects of stigma.Citation99
As can be expected, experiences with IBD disclosure vary considerably. Some patients report being very open about their condition while others may tend to keep it hidden except with family and close friends.Citation99 Disclosure in employment settings comes with its own unique challenges.Citation100 Racial differences exist, with Caucasians more likely than African-Americans to disclose their IBD status to their employer or fellow employees.Citation101 The reactions in occupational settings are mixed. A 1992 study of patients with CD found that 37% of patients currently employed felt their employer did not need to know about their IBD and 30% were in favor of active concealment. Additionally, 24% felt IBD had limited their employment prospects including avoiding seeking a promotion or being denied promotion because of their illness.Citation102 Conversely, a 1988 study found the majority of participants reported high workplace disclosure (81%), and that 80% of coworkers and 77% of employers had been generally helpful.Citation103 These significantly different findings on employer attitudes may be related to a wide variability in employment culture as a whole, geographic differences in health-related stigma, or the level of familiarity that surveyed employers had with IBD. It highlights that IBD patient experiences with perceptions of negative attitudes from employers will likely vary widely, highlighting the importance of inquiring about each individual’s experience in a clinical setting. Academic and school settings also present challenges for people living with IBD. In one study, 50% of children reported that their teachers were unsympathetic toward their illness.Citation104 Another study found that 21% of college-aged students found lecturers to be indifferent and 8% found them to be hostile toward their disease.Citation102
Perceived stigma in IBD patients is associated with several outcomes including increases in psychological distress,Citation42,Citation105 decreases in health-related quality of life, reduced medication adherence, and decreased self-esteem and self-efficacy.Citation42 Patients who perceive poor social support prior to surgery report poorer quality of life after the procedure.Citation106 If the surgical intervention results in an ostomy, quality of life may improve in some patients in that they feel more in control of their illnessCitation107 while others may experience an increase in both perceived and internalized stigma.Citation108 Simply perceiving that others hold these negative attitudes is sufficient to degrade patient well-being. Whether or not the individual internalizes the stigma can lead to even greater distress, and thus, is an important line of inquiry in stigma research.
Internalized or self-stigma and stigma resistance
Internalized or self-stigma may be related to the poorest outcomes of the three stigma domains in that patients apply negative attitudes and stereotypes to themselves rather than rejecting them as false. Internalized stigma includes alienation, stereotype endorsement, discrimination experiences, and social withdrawal.Citation77 Patients with IBD report feeling damaged,Citation26 especially as it relates to physical changes from the disease or its treatments (eg, weight loss or gain, stunted growth, and skin rashes). Self-blame regarding the onset of IBD or the presence of its symptoms postdiagnosis is associated with poorer adjustment to the illness.Citation109 The presence of an ostomy can contribute to self-stigma in some cases,Citation110,Citation111 while in others it produces positive results including feelings of satisfaction with their illness management.Citation112
One study specifically evaluates internalized stigma and stigma resistance in IBD.Citation113 Overall, 33% of people living with IBD report internalized stigma with alienation and social withdrawal being the most common. In general, IBD patients report mild levels of internalized stigma while a larger majority report stigma resistance attitudes and behaviors suggesting that while IBD patients perceive others hold stigmatizing views, they tend to not incorporate them into their sense of self. Levels of internalized stigma are associated with lower educational levels, residing in an urban setting, and having extraintestinal symptoms. Unlike stigma perception, patients who identified themselves as in remission reported less internalized stigma and greater use of stigma resistance behaviors. Internalized stigma in IBD patients predicts reduced health-related quality of life, poorer self-esteem and self-efficacy, and increased psychological distress. These findings are similar to internalized stigma studies in other patient populations.Citation53,Citation70,Citation114
Enacted stigma
Studies on enacted stigma in IBD are limited. Patients report many people simply do not understand IBD, which may cause some to accuse persons with IBD of exaggerating their condition for secondary gain.Citation26 In 1992, Mayberry found that 50% of CD patients compared to 24% of matched healthy controls had significant trouble finding work and long-term unemployment exceeding 6 weeks.Citation102 MayberryCitation115 evaluated employer attitudes and practices toward people living with CD. Only two out of 35 companies would reject candidates because of IBD. However, 33 of 35 would rely on preemployment medical examinations to make hiring decisions and 8% said IBD would negatively impact promotion consideration. Sixty percent would support employee experiencing a relapse by providing a lighter work period and 16% would pay for private care; 30% would not extend paid leave time for outpatient appointments. Due to the dearth of studies on enacted stigma in IBD patients, additional research is important to close the gaps in the understanding of how common enacted stigma is, what the more common sources of discrimination are, and how enacted stigma influences outcomes.
Discussion
Based on the results of this review, IBD is susceptible to stigma because of its concealability, embarrassing symptoms, and historical view of IBD being a psychosomatic condition. The most commonly studied type of stigma is perceived stigma, evident in 17 studies and demonstrating that the majority of IBD patients perceive stigma from their peers, significant others, colleagues, and physicians.Citation42 Perceived stigma is the easiest construct to identify, but may have less to do with outcomes than “deeper” levels of stigma such as internalized or enacted. For example, patients who perceive stigma but do not internalize it may utilize coping strategies that would be found in any stigma-reducing intervention technique (eg, cognitive reframing). Future research could probably shift away from perceived stigma at this point and focus on other forms.
Internalized stigma, or the incorporation of stigmatizing beliefs and attitudes into one’s sense of self, is potentially the most detrimental to IBD outcomes because it results in declines across physical and psychological functioning more than perceived stigma. In other disease groups, similar findings are noted.Citation77 As IBD requires substantial self-management to maintain remission, adhere to medications, follow disease surveillance protocols (eg, colonoscopy and regular laboratory testing), vaccination, and other health guidelines, stigma could potentially interfere with self-care. Internalized stigma may be the most modifiable form of stigma through cognitive and behavioral therapies, if it is detected early and remediated.
Considerably less is known about enacted stigma in IBD and is an important area for future research. Enacted stigma evaluated in other conditions demonstrates that it is a very important aspect of public health and health systems.Citation44,Citation116,Citation117 Whether it is subtle “weeding” out of an employee who is chronically ill or more direct (eg, refusing to allow an IBD patient to use the restroom), enacted stigma requires a comprehensive intervention.
Measurement of stigma and related factors is critical to proper detection and potential intervention – unfortunately, the construct itself, when present, makes it hard to measure. One tool specific to IBD is the Perceived Stigma Scale for IBD, adapted from the Perceived Stigma Scale for IBS,Citation86 which allows for quick assessment of stigma perceptions among IBD patients during routine visits. However, as we saw earlier, poor quality of life, poor treatment adherence, or low disease knowledge may also point to stigmatizing beliefs about IBD and when present, the provider should query for perceived stigma. Regardless, it is important for health care providers to ask patients about the social implications of their disease so that they may be referred to appropriate resources, including clinical health psychologists, to help mitigate the potential impacts of stigma on patient outcomes.
The development of stigma interventions has occurred for other chronic conditions,Citation46,Citation118–Citation121 and while their efficacy in reducing stigma is mixed, these interventions have merit. The RAND Corporation and the American Psychological Association have described theoretically-based multicomponent approaches to reducing stigma in mental illness which could be applicable to IBD.Citation122 These include training interventions for health professionals and the general public, which provide information on the causes of the disease (not stress or diet, but an immune-inflammatory reaction), treatments (infusions, surgeries, and ostomies), and experiences of people living with the disease (people with CD and ostomies can be athletes, like Matt Light, David Garrard, and Kevin Dineen). Educational interventions seem to hold the longest staying power when they are enhanced with a direct interpersonal contact strategy (having a guest speaker with UC or a panel discussion between IBD patients from different backgrounds).Citation123 Finally, mass media campaigns can deliver similar antistigma, educational messages although the impact of these is hard to evaluate. Patient advocacy groups have already emerged to help destigmatize IBD (eg, The Great Bowel Movement, www.thegreatbowelmovement.org) and research into their benefit could be an important next step.
Disclosure
The authors report no conflicts of interest in this work.
References
- KoJKAuyeungKKInflammatory bowel disease: etiology, pathogenesis and current therapyCurr Pharm Des2014201082109623782147
- FairburnKJoint involvement in systemic diseasePractitioner19942382142198183806
- MaconiGGridavillaDViganoCPerianal disease is associated with psychiatric co-morbidity in Crohn’s disease in remissionInt J Colorectal Dis2014291285129024986138
- MolodeckyNASoonISRabiDMIncreasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic reviewGastroenterology20121424654e42 quiz e3022001864
- LangholzECurrent trends in inflammatory bowel disease: the natural historyTherap Adv Gastroenterol201037786
- Vester-AndersenMKProsbergMVJessTDisease course and surgery rates in inflammatory bowel disease: a population-based, 7-year follow-up study in the era of immunomodulating therapyAm J Gastroenterol201410970571424642581
- SainsburyAHeatleyRVReview article: psychosocial factors in the quality of life of patients with inflammatory bowel diseaseAliment Pharmacol Ther20052149950815740531
- AlrubaiyLRikabyIDoddsPHutchingsHAWilliamsJGSystematic review of health-related quality of life measures for inflammatory bowel diseaseJ Crohns Colitis2015928429225576752
- van der HaveMvan der AalstKSKapteinAADeterminants of health-related quality of life in Crohn’s disease: a systematic review and meta-analysisJ Crohns Colitis201489310623746864
- FloydDNLanghamSSeveracHCLevesqueBGThe economic and quality-of-life burden of Crohn’s disease in Europe and the United States, 2000 to 2013: a systematic reviewDig Dis Sci20156029931225258034
- LoftusEVJrGuerinAYuAPIncreased risks of developing anxiety and depression in young patients with Crohn’s diseaseAm J Gastroenterol20111061670167721537359
- Fuller-ThomsonELateefRSulmanJRobust association between inflammatory bowel disease and generalized anxiety disorder: findings from a nationally representative Canadian studyInflamm Bowel Dis2015212341234826218145
- NahonSLahmekPDuranceCRisk factors of anxiety and depression in inflammatory bowel diseaseInflamm Bowel Dis2012182086209122294486
- GraffLAWalkerJRBernsteinCNDepression and anxiety in inflammatory bowel disease: a review of comorbidity and managementInflamm Bowel Dis2009151105111819161177
- PanaraAJYarurAJRiedersBThe incidence and risk factors for developing depression after being diagnosed with inflammatory bowel disease: a cohort studyAliment Pharmacol Ther20143980281024588323
- SzigethyECraigAEIobstEAProfile of depression in adolescents with inflammatory bowel disease: implications for treatmentInflamm Bowel Dis200915697418831071
- BelLGVollebregtAMVan der Meulen-de JongAESexual dysfunctions in men and women with inflammatory bowel disease: the influence of IBD-related clinical factors and depression on sexual functionJ Sex Med2015121557156726054013
- LewisMCAttributions and inflammatory bowel disease: patients’ perceptions of illness causes and the effects of these perceptions on relationshipsAARN News Lett19884416173389064
- van der EijkIStockbruggerRRusselMInfluence of quality of care on quality of life in inflammatory bowel disease (IBD): literature review and studies plannedEur J Intern Med20001122823410967512
- WrightEKKammMAImpact of drug therapy and surgery on quality of life in Crohn’s disease: a systematic reviewInflamm Bowel Dis2015211187119425895008
- AnanthakrishnanANGainerVSCaiTSimilar risk of depression and anxiety following surgery or hospitalization for Crohn’s disease and ulcerative colitisAm J Gastroenterol201310859460123337479
- MacknerLMCrandallWVLong-term psychosocial outcomes reported by children and adolescents with inflammatory bowel diseaseAm J Gastroenterol20051001386139215929775
- DrossmanDAPatrickDLMitchellCMZagamiEAAppelbaumMIHealth-related quality of life in inflammatory bowel disease. Functional status and patient worries and concernsDig Dis Sci198934137913862766905
- CasatiJTonerBBde RooyECDrossmanDAMaunderRGConcerns of patients with inflammatory bowel disease: a review of emerging themesDig Dis Sci200045263110695609
- LevensteinSLiZAlmerSCross-cultural variation in disease-related concerns among patients with inflammatory bowel diseaseAm J Gastroenterol2001961822183011419836
- DanielJMYoung adults’ perceptions of living with chronic inflammatory bowel diseaseGastroenterol Nurs200225839412055376
- KappelmanMDPorterCQGalankoJAUtilization of healthcare resources by U.S. children and adults with inflammatory bowel diseaseInflamm Bowel Dis201117626820564532
- BokemeyerBHardtJHuppeDClinical status, psychosocial impairments, medical treatment and health care costs for patients with inflammatory bowel disease (IBD) in Germany: an online IBD registryJ Crohns Colitis2013735536822503168
- GrayWNDensonLABaldassanoRNHommelKATreatment adherence in adolescents with inflammatory bowel disease: the collective impact of barriers to adherence and anxiety/depressive symptomsJ Pediatr Psychol20123728229122080456
- MagalhaesJDias de CastroFBoal CarvalhoPLeiteSMoreiraMJCotterJTreatment of inflammatory bowel disease: is your patient at risk of non-adherence?Acta Med Port20142757658025409212
- PirinenTKolhoKLSimolaPAshornMAronenETParent-adolescent agreement on psychosocial symptoms and somatic complaints among adolescents with inflammatory bowel diseaseActa Paediatr201210143343722122226
- TurnbullGKVallisTMQuality of life in inflammatory bowel disease: the interaction of disease activity with psychosocial functionAm J Gastroenterol199590145014547661168
- GreeneBRBlanchardEBWanCKLong-term monitoring of psychosocial stress and symptomatology in inflammatory bowel diseaseBehav Res Ther1994322172268155059
- GunnarssonCChenJRizzoJALadapoJALoflandJHDirect health care insurer and out-of-pocket expenditures of inflammatory bowel disease: evidence from a US national surveyDig Dis Sci2012573080309122790905
- RocchiABenchimolEIBernsteinCNInflammatory bowel disease: a Canadian burden of illness reviewCan J Gastroenterol20122681181723166905
- BassiADoddSWilliamsonPBodgerKCost of illness of inflammatory bowel disease in the UK: a single centre retrospective studyGut2004531471147815361497
- GunnarssonCChenJRizzoJALadapoJANaimALoflandJHThe employee absenteeism costs of inflammatory bowel disease: evidence from US National Survey DataJ Occup Environ Med20135539340123232289
- SaibilFLaiEHaywardAYipJGilbertCSelf-management for people with inflammatory bowel diseaseCan J Gastroenterol20082228128718354757
- CooperJMCollierJJamesVHawkeyCJBeliefs about personal control and self-management in 30–40 year olds living with Inflammatory Bowel Disease: a qualitative studyInt J Nurs Stud2010471500150920646707
- BarlowCCookeDMulliganKBeckENewmanSA critical review of self-management and educational interventions in inflammatory bowel diseaseGastroenterol Nurs201033111820145446
- KeeferLKieblesJLKwiatekMAThe potential role of a self-management intervention for ulcerative colitis: a brief report from the ulcerative colitis hypnotherapy trialBiol Res Nurs201214717721362636
- TaftTHKeeferLLeonhardCNealon-WoodsMImpact of perceived stigma on inflammatory bowel disease patient outcomesInflamm Bowel Dis2009151224123219180581
- ParcesepeAMCabassaLJPublic stigma of mental illness in the United States: a systematic literature reviewAdm Policy Ment Health20134038439922833051
- BrohanESladeMClementSThornicroftGExperiences of mental illness stigma, prejudice and discrimination: a review of measuresBMC Health Serv Res2010108020338040
- AbdullahTBrownTLMental illness stigma and ethnocultural beliefs, values, and norms: an integrative reviewClin Psychol Rev20113193494821683671
- StanglALLloydJKBradyLMHollandCEBaralSA systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come?J Int AIDS Soc2013161873424242268
- SmitPJBradyMCarterMHIV-related stigma within communities of gay men: a literature reviewAIDS Care20122440541222117138
- MahajanAPSaylesJNPatelVAStigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forwardAIDS200822Suppl 2S677918641472
- ScamblerGHeijndersMvan BrakelWHICRAASUnderstanding and tackling health-related stigmaPsychol Health Med20061126927017130063
- MarlowLAWallerJWardleJDoes lung cancer attract greater stigma than other cancer types?Lung Cancer20158810410725704958
- MutebiMEdgeJStigma, survivorship and solutions: addressing the challenges of living with breast cancer in low-resource areasS Afr Med J201410438325295332
- ShepherdMAGerendMAThe blame game: cervical cancer, knowledge of its link to human papillomavirus and stigmaPsychol Health2013299410924006882
- NoorABashirSEarnshawVABullying, internalized hepatitis (hepatitis C virus) stigma, and self-esteem: does spirituality curtail the relationship in the workplaceJ Health Psychol Epub 2015 Jan 20
- MarinhoRTBarreiraDPHepatitis C, stigma and cureWorld J Gastroenterol2013196703670924187444
- MooreGAHawleyDABradleyPHepatitis C: studying stigmaGastroenterol Nurs20083134635218849671
- BautistaREShapovalovDShorakaARFactors associated with increased felt stigma among individuals with epilepsySeizure20153010611226216694
- LeafferEBHesdorfferDCBegleyCPsychosocial and socio-demographic associates of felt stigma in epilepsyEpilepsy Behav20143710410925010324
- ThomasSVNairAConfronting the stigma of epilepsyAnn Indian Acad Neurol20111415816322028525
- GarbinCAGarbinAJCarloniMERovidaTAMartinsRJThe stigma and prejudice of leprosy: influence on the human conditionRev Soc Bras Med Trop20154819420125992935
- SermrittirongSVan BrakelWHStigma in leprosy: concepts, causes and determinantsLepr Rev201485364724974441
- HeijndersMLThe dynamics of stigma in leprosyInt J Lepr Other Mycobact Dis20047243744715755198
- PapadopoulosSBrennanLCorrelates of weight stigma in adults with overweight and obesity: a systematic literature reviewObesity (Silver Spring)2015231743176026260279
- PhelanSMBurgessDJYeazelMWHellerstedtWLGriffinJMvan RynMImpact of weight bias and stigma on quality of care and outcomes for patients with obesityObes Rev20151631932625752756
- CallahanDChildren, stigma, and obesityJAMA Pediatr201316779179223817389
- PuhlRMHeuerCAThe stigma of obesity: a review and updateObesity (Silver Spring)20091794196419165161
- AydemirNOzkaraCUnsalPCanbeyliRA comparative study of health related quality of life, psychological well-being, impact of illness and stigma in epilepsy and migraineSeizure20112067968521764337
- BhallaDCheaKHunCPopulation-based study of epilepsy in Cambodia associated factors, measures of impact, stigma, quality of life, knowledge-attitude-practice, and treatment gapPLoS One20127e4629623077505
- BlumeWTDerryPAStigma and its neurological and psychological effects in epilepsyCan J Neurol Sci20083540340418973055
- Carter-HarrisLLung cancer stigma as a barrier to medical help-seeking behavior: practice implicationsJ Am Assoc Nurse Pract20152724024525736473
- DrapalskiALLuckstedAPerrinPBA model of internalized stigma and its effects on people with mental illnessPsychiatr Serv20136426426923573532
- Else-QuestNMLoConteNKSchillerJHHydeJSPerceived stigma, self-blame, and adjustment among lung, breast and prostate cancer patientsPsychol Health20092494996420205038
- MatthewsAKCorriganPWRutherfordJLMental illness stigma as a barrier to psychosocial services for cancer patientsJ Natl Compr Canc Netw2003137537919761070
- HatzenbuehlerMLPhelanJCLinkBGStigma as a fundamental cause of population health inequalitiesAm J Public Health201310381382123488505
- GoffmanEStigma: Notes on the Management of Spoiled IdentityEnglewood Cliffs, NJPrentice-Hall1963
- LinkBGPhelanJConceptualizing stigmaAnn Rev Sociol200127363385
- CorriganPWWatsonACUnderstanding the impact of stigma on people with mental illnessWorld Psychiatry20021162016946807
- BoydJEAdlerEPOtilingamPGPetersTInternalized Stigma of Mental Illness (ISMI) scale: a multinational reviewCompr Psychiatry20145522123124060237
- van der BeekKMBosIMiddelBWyniaKExperienced stigmatization reduced quality of life of patients with a neuromuscular disease: a cross-sectional studyClin Rehabil2013271029103823818411
- SegalovichJDoronABehrbalkPKursRRomemPInternalization of stigma and self-esteem as it affects the capacity for intimacy among patients with schizophreniaArch Psychiatr Nurs20132723123424070991
- HilbertABraehlerEHaeuserWZengerMWeight bias internalization, core self-evaluation, and health in overweight and obese personsObesity (Silver Spring)201422798523836723
- EarnshawVAQuinnDMThe impact of stigma in healthcare on people living with chronic illnessesJ Health Psychol20121715716821799078
- JonesEEFarinaAHastorfAHMarkusHMillerDTScottRASocial Stigma: The Psychology of Marked RelationshipsNew YorkWH Freeman & Company1984
- CrandallCSMoriartyDPhysical illness stigma and social rejectionBr J Soc Psychol199534Pt 167837735733
- SheffieldBFCarneyMWCrohn’s disease: a psychosomatic illness?Br J Psychiatry19761284464501276548
- BernsteinCNSinghSGraffLAWalkerJRMillerNCheangMA prospective population-based study of triggers of symptomatic flares in IBDAm J Gastroenterol20101051994200220372115
- JonesMPKeeferLBrattenJDevelopment and initial validation of a measure of perceived stigma in irritable bowel syndromePsychol Health Med20091436737419444714
- TaftTHKeeferLArtzCBrattenJJonesMPPerceptions of illness stigma in patients with inflammatory bowel disease and irritable bowel syndromeQual Life Res2011201391139921424542
- SimrenMAxelssonJGillbergRAbrahamssonHSvedlundJBjörnssonESQuality of life in inflammatory bowel disease in remission: the impact of IBS-like symptoms and associated psychological factorsAm J Gastroenterol20029738939611866278
- Van BrakelWHMeasuring health-related stigma – a literature reviewPsychol Health Med20061130733417130068
- DibleyLNortonCExperiences of fecal incontinence in people with inflammatory bowel disease: self-reported experiences among a community sampleInflamm Bowel Dis2013191450146223624884
- KrauseMThe transformation of social representations of chronic disease in a self-help groupJ Health Psychol2003859961519177720
- BernhoferEIMasinaVMSorrellJModicMBThe pain experience of patients hospitalized with inflammatory bowel disease: a phenomenological studyGastroenterol Nurs Epub 2015 Aug 5
- Czuber-DochanWDibleyLBTerryHReamENortonCThe experience of fatigue in people with inflammatory bowel disease: an exploratory studyJ Adv Nurs2013691987199923215959
- Czuber-DochanWNortonCBredinFDarvellMNathanITerryHHealthcare professionals’ perceptions of fatigue experienced by people with IBDJ Crohns Colitis2014883584424491516
- de RooyECTonerBBMaunderRGConcerns of patients with inflammatory bowel disease: results from a clinical populationAm J Gastroenterol2001961816182111419835
- MaunderRTonerBde RooyEMoskovitzDInfluence of sex and disease on illness-related concerns in inflammatory bowel diseaseCan J Gastroenterol19991372873210633825
- JoachimGAcornSStigma of visible and invisible chronic conditionsJ Adv Nurs20003224324810886457
- SaundersBStigma, deviance and morality in young adults’ accounts of inflammatory bowel diseaseSociol Health Illn2014361020103624888541
- FrohlichDOSupport often outweighs stigma for people with inflammatory bowel diseaseGastroenterol Nurs20143712613624691083
- MoodyGAProbertCSJayanthiVMayberryJFThe attitude of employers to people with inflammatory bowel diseaseSoc Sci Med1992344594601566127
- FinlayDGBasuDSellinJHEffect of race and ethnicity on perceptions of inflammatory bowel diseaseInflamm Bowel Dis20061250350716775495
- MayberryMKProbertCSrivastavaERhodesJMayberryJFPerceived discrimination in education and employment by people with Crohn’s disease: a case control study of educational achievement and employmentGut1992333123141568648
- WykeRJEdwardsFCAllanRNEmployment problems and prospects for patients with inflammatory bowel diseaseGut198829122912353197997
- MoodyGEadenJAMayberryJFSocial implications of childhood Crohn’s diseaseJ Pediatr Gastroenterol Nutr199928S43S4510204525
- LooperKJKirmayerLJPerceived stigma in functional somatic syndromes and comparable medical conditionsJ Psychosom Res20045737337815518673
- MoskovitzDNMaunderRGCohenZMcLeodRSMacRaeHCoping behavior and social support contribute independently to quality of life after surgery for inflammatory bowel diseaseDis Colon Rectum20004351752110789749
- DanielsenAKBurcharthJRosenbergJPatient education has a positive effect in patients with a stoma: a systematic reviewColorectal Dis2013156e276e28323470040
- SimmonsKLSmithJABobbKALilesLLAdjustment to colostomy: stoma acceptance, stoma care self-efficacy and interpersonal relationshipsJ Adv Nurs200760662763518039249
- VothJSiroisFMThe role of self-blame and responsibility in adjustment to inflammatory bowel diseaseRehabil Psychol2009549910819618709
- SalterMStoma care. Overcoming the stigmaNurs Times19908667712342923
- SmithDMLoewensteinGRozinPSherriffRLUbelPASensitivity to disgust, stigma, and adjustment to life with a colostomyJ Res Pers20074178780317940585
- DanielsenAKSoerensenEEBurcharthKRosenbergJLearning to live with a permanent intestinal ostomy: impact on everyday life and educational needsJ Wound Ostomy Continence Nurs20134040741223820473
- TaftTHBallouSKeeferLA preliminary evaluation of internalized stigma and stigma resistance in inflammatory bowel diseaseJ Health Psychol20131845146022689587
- FifeBLWrightERThe dimensionality of stigma: a comparison of its impact on the self of persons with HIV/AIDS and cancerJ Health Soc Behav200041506710750322
- MayberryJFImpact of inflammatory bowel disease on educational achievements and work prospectsJ Pediatr Gastroenterol Nutr199928S343610204522
- AwofesoNConcept and impact of stigma on discrimination against leprosy sufferers – minimizing the harmLepr Rev20057610110215881045
- ParfeneCStewartTLKingTZEpilepsy stigma and stigma by association in the workplaceEpilepsy Behav20091546146619570726
- BirbeckGInterventions to reduce epilepsy-associated stigmaPsychol Health Med20061136436617130072
- BosAESchaalmaHPPryorJBReducing AIDS-related stigma in developing countries: the importance of theory- and evidence-based interventionsPsychol Health Med20081345046018825583
- BrabcovaDLovasovaVKohoutJZarubovaJKomarekImproving the knowledge of epilepsy and reducing epilepsy-related stigma among children using educational video and educational drama – a comparison of the effectiveness of both interventionsSeizure20132217918423265921
- ChambersSKMorrisBACluttonSPsychological wellness and health-related stigma: a pilot study of an acceptance-focused cognitive behavioural intervention for people with lung cancerEur J Cancer Care (Engl)201524607025053458
- ThornicroftGMehtaNClementSEvidence for effective interventions to reduce mental-health-related stigma and discriminationLancet201526410341
- HeijndersMVan Der MeijSThe fight against stigma: an overview of stigma-reduction strategies and interventionsPsychol Health Med20061135336317130071