Abstract
Objectives
Gastrointestinal (GI) intolerance is associated with adverse outcomes in critically ill patients receiving enteral nutrition (EN). The objective of this analysis is to quantify the cost of GI intolerance and the cost implications of starting with semi-elemental EN in intensive care units (ICUs).
Study design
A US-based cost–consequence model was developed to compare the costs for patients with and without GI intolerance and the costs with semi-elemental or standard EN while varying the proportion of GI intolerance cases avoided.
Materials and methods
ICU data on GI intolerance prevalence and outcomes in patients receiving EN were derived from an observational study. ICU stay costs were obtained from literature and the costs of EN from US customers’ price lists. The model was used to conduct a threshold analysis, which calculated the minimum number of cases of GI intolerance that would have to be avoided to make the initial use of semi-elemental formula cost saving for the cohort.
Results
Out of 100 patients receiving EN, 31 had GI intolerance requiring a median ICU stay of 14.4 days versus 11.3 days for each patient without GI intolerance. The model calculated that semi-elemental formula was cost saving versus standard formula when only three cases of GI intolerance were prevented per 100 patients (7% of GI intolerance cases avoided).
Conclusion
In the US setting, the model predicts that initial use of semi-elemental instead of standard EN can result in cost savings through the reduction in length of ICU stay if >7% of GI intolerance cases are avoided.
Plain language summary
The economic impact of gastrointestinal intolerance and use of semi-elemental nutrition in the ICU has not previously been modeled to the authors’ knowledge. A model was developed to analyze the costs of using semi-elemental versus polymeric enteral nutrition in an intensive care unit (ICU) cohort in the USA.
The model shows the following:
The costs associated with gastrointestinal intolerance in the ICU in terms of length of stay constitute a high burden in the US health care system.
Preventing gastrointestinal intolerance by initial use of semi-elemental instead of polymeric formula could lead to potential cost savings by reducing ICU length of stay.
Introduction
Inadequate nutritional intake can adversely affect the clinical course in critically ill patients. Specialized nutritional support, given either parenterally or enterally, is often required to improve patient outcomes and reduce morbidity and mortality. The 2016 American Society for Parenteral and Enteral Nutrition (ASPEN)/Society of Critical Care Medicine (SCCM) Nutrition Support Guidelines for Critically Ill Adults recommend first the use of early enteral nutrition (EN) because of data demonstrating the improvement in patient outcomes such as reduction in infectious complications, in the length of mechanical ventilation, and in the overall length of hospital stay.Citation1 Second, EN is preferred over the early use of parenteral nutrition because of earlier return of normal gut function and reduction in health care costs.Citation1 In the intensive care unit (ICU) setting, Peake et al reported that ~40% of patients required EN support.Citation2
Gastrointestinal (GI) intolerance, characterized by upper (e.g., nausea, vomiting) or lower GI symptoms (e.g., diarrhea), poses a significant problem in patients admitted to ICUs and often limits the ability to achieve adequate daily protein and caloric intake. Feed intolerance often arises from impaired gastroduodenal motility and nutrient absorption.Citation3 Depending on the underlying medical condition, the definition of feeding intolerance, and the nutritional support, GI intolerance can be frequent in the ICU. A study showed that 36% of enterally fed patients had an incident of diarrhea during the ICU stay.Citation4 Delayed gastric emptying and intra-abdominal hypertension are other common GI symptoms in ICU patients, reported in 60%Citation5 and 27% of patients, respectively.Citation6 A multinational study concluded that >40% of patients had GI symptoms during the first week of ICU stay.Citation7 GI intolerance in the ICU increases the risk of malnutrition and the ability to tolerate routine EN support, which has been associated with poor patient outcomes including an increased length of stay (LOS), longer days on mechanical ventilation, and higher mortality rates.Citation3
The ASPEN/SCCM guidelines note that “no clear benefit to patient outcome has been shown in the literature for the routine use of specialty formulas in a general ICU setting” (expert consensus) and that “small peptide formulations should be used in the patient with persistent diarrhea, with suspected malabsorption or lack of response to fiber” (expert consensus).Citation1 The European Society for Parenteral and Enteral Nutrition guidelines also note that the clinical trial evidence for the impact of semi-elemental EN versus standard EN in ICU patients is contradictory with two trials showing a reduction in diarrhea, one showing an increase in diarrhea, and one trial showing no difference. The European Society for Parenteral and Enteral Nutrition guidelines conclude that “As no clear cut advantage of peptide-based formulae has been demonstrated in these studies and taking into account the higher price, we concluded that the use of peptide-based formulas should not be recommended (Grade C).”Citation8
Though a standard polymeric formula (containing whole proteins and mainly long chain type of triglycerides) used as first-line EN may be adequate in a variety of clinical settings, a more specialized semi-elemental formula, containing peptides and mostly medium chain type of triglycerides, may still offer clinical benefits for some high-risk, critically ill patients.
Alexander et al summarized the nutritional and health benefits of semi-elemental formulas in various nutritionally high-risk populations, including those with Crohn’s disease, short bowel syndrome, acute and chronic pancreatitis, cerebral palsy, cystic fibrosis, cerebrovascular accidents, immunocompromised patients, and ICU patients.Citation9 An adult ICU population may contain patients with these conditions at the time of admission to the ICU. They reported that a 100% whey semi-elemental formula would lead to fewer cases of GI intolerance than a standard formula because the enzymatically hydrolyzed whey protein helps facilitate gastric emptying and reduces the risk for reflux and aspiration, although the comparative data specific to adult ICU patients did not demonstrate improved GI tolerance. In addition, semi-elemental formulas may improve the fat absorption and help promote better GI tolerance because of their high proportion of medium-chain triglycerides as a percentage of the total fat content.Citation10 Semi-elemental EN has been demonstrated to have a benefit in upper GI intolerance symptoms in children with development delay switched from standard EN in a retrospective study.Citation11 However, the evidence for upper GI intolerance in adult ICU patients is contradictory. In one trial conducted in acutely injured adult patients in the ICU the prevalence of elevated gastric residuals was similar between semi-elemental EN and standard EN.Citation12 Conversely, a retrospective study in abdominal surgery patients showed that the average maximum gastric residual volume (GRV) of patients receiving semi-elemental EN during their ICU stays was significantly lower than that of patients receiving standard EN.Citation13
Given the improved outcomes in critically ill patients receiving enteral feeding, and the higher acquisition costs of semi-elemental formulas compared with standard formulas, we have developed an ICU cohort simulation cost–consequence model. The model explores the cost and consequences of assuming different proportions of GI intolerance cases avoided by early introduction of a semi-elemental formula rather than a standard formula.
Materials and methods
Model specifications
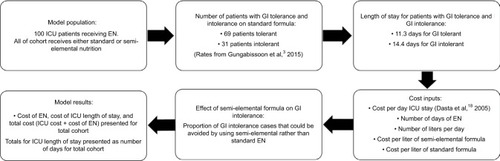
We developed a US-based cost–consequence model in Microsoft Excel to compare the total ICU costs for patients with and without GI intolerance who are receiving EN in the ICU, and to quantify the economic impact of early utilization of a semi-elemental formula instead of a standard formula. Using a standard formula as the comparator is a conservative approach because it represents the EN standard of care of most ICU patients. The time frame is short term as it assesses the costs during the ICU stay. The overview of the model is summarized in .
Figure 1 Model outline.
Defining the incidence of GI intolerance and impact on length of ICU stay
A comprehensive literature review (PubMed, MEDLINE, and the Cochrane Library between 2005 and 2015) was performed to identify the incidence and the economic burden of GI intolerance among critically ill patients. Published data are limited in this field. The most robust publication on this topic was a multicenter, international study by Gungabissoon et al, which was used as the foundation of the cost–consequence model.Citation3
In a retrospective analysis of the 2009 International Nutrition Survey of 167 ICUs from 21 countries,Citation14 Gungabissoon et al reported an incidence of 30.5% of adult ICU patients developing GI intolerance that required interruption of EN feeding.Citation3 The analysis included patients on mechanical ventilation for at least 48 hours requiring at least 72 hours stay in the ICU setting. The 1,888 patients indexed in the study were composed of the following diagnostic categories: respiratory (31%), neurologic (16%), trauma (13%), sepsis (11%), cardiovascular medical (8%), cardiovascular surgical (5%), GI surgical (5%), GI medical (3%), and other (8%). Feed intolerance was defined as one or more of large GRV, abdominal distension, vomiting/emesis, significant diarrhea, or subjective discomfort requiring interruption of EN. The median time to intolerance from initiation of enteral feeding (on average after 34.9 hours) was 3 days (range 1–12 days). Feed intolerance was associated with a reduction in the quantity of nutrients delivered, fewer ventilator-free days, longer ICU stay, and increased mortality ().
Table 1 Comparison of outcomes between enteral feeding intolerant and tolerant patients
The large study conducted by Gungabissoon et alCitation3 was prompted by previous studies that had reported the relationships between feed intolerance and mortality, pneumonia, and length of ICU stay, but were based on small cohorts in a limited number of centers.Citation6,Citation15
In the model, it was assumed that, for every 100 ICU patients receiving EN, 31 will develop GI intolerance and 69 will remain GI tolerant based on Gungabissoon et al findings.Citation3 The mean length of ICU stay in the model was 14.4 days for patients with GI intolerance and 11.3 days for those who were GI tolerant.Citation3
Improved tolerance with semi-elemental formula versus standard formula
No controlled trial or observational data in the literature reported an estimate of the number of cases of GI intolerance that could be avoided in an adult population by using a semi-elemental EN formula compared to a standard formula in a general ICU setting. However, some studies were identified but were not used as base case estimates in the model because they were for diarrhea outcomes only,Citation16 contained a high protein rather than standard EN for comparison,Citation17 and retrospectively collected data for intra-abdominal patients only.Citation13 The model allows the user to vary the proportion of GI intolerance cases avoided and calculates the threshold number of GI cases avoided for the semi-elemental formula to be cost saving versus the standard formula.
Economic data
The estimated cost of ICU stay was $4,714 per day, based on the value of $3,500 reported by Dasta et al inflated to 2016 values using the US Consumer Price Index.Citation18 Dasta et al calculated the cost per day of ICU stay by multiplying daily hospital charges by hospital-specific cost-to-charge ratios, as it was a multicenter study. This cost represents an average ICU stay cost, as Dasta et al performed their analysis on data from trauma, surgical, and medical ICUs. In the model, it was assumed that patients received 1.5 L of standard or semi-elemental formula for 8 days based on the average duration found in the Gungabissoon et al study.Citation3 At a cost per liter of $10.17 for the standard formula (Isosource®; Nestlé Health Science) and $36.67 for the semi-elemental formula (Peptamen®; Nestlé Health Science), this equates to the costs of $122.04 and $440.04, respectively, per episode of EN (publicly available 2016 customer list prices).
Sensitivity analysis
We conducted one-way sensitivity analyses to examine the impact of variation in single parameters on the results. We assessed the results if 1) GI intolerance resulted in only one additional day in ICU; 2) the incidence of GI intolerance was reduced from 31% to 22% based on the lowest incidence observed in the Gungabissoon et al study (Latin America region);Citation3 3) the LOS was reduced from 14.4 to 7 days for GI-tolerant cases (and from 11.3 to 5.5 days for GI-intolerant cases); and 4) the cost per ICU day was decreased by 20% from $4,714 to $3,771.
Results
Cost of GI intolerance
Based on a population of 100 patients entering the model, 31 of whom are expected to develop GI intolerance, the total length of ICU stay is 1,226.1 days, compared to the total length of ICU stay of 1,130.0 days in patients without GI intolerance. Therefore, GI intolerance accounts for 96.1 additional days in the ICU (3.1 additional days per GI-intolerant patient), resulting in an additional cost of $453,015 for the cohort.
Economic impact of initial use of a semi-elemental formula
Using the model, we calculated for the 100-patient cohort that a semi-elemental formula would start to be cost saving compared with a standard formula when only 7.0% of GI-intolerant cases (3/31, rounded up to the nearest whole case) are avoided by using semi-elemental EN in all patients and with the base case estimate of 3.1 additional days in the ICU per intolerant patient applied. The ICU and EN cost implications are detailed in .
Table 2 Costs (US$) of managing the total ICU cohort, assuming that use of semi-elemental formula avoids 7% of GI intolerance (three cases)
Sensitivity analysis
We ran sensitivity analyses by varying single inputs as previously described. For each of the scenarios, we calculated what would be the minimum efficacy for the semi-elemental formula to be cost saving versus the standard formula. The efficacy, defined as the proportion of GI cases avoided by using the semi-elemental formula rather than standard EN, varied from 3.5% to 21.8% ().
Table 3 Results of sensitivity analysis varying model inputs
Discussion
ICU care expends a large proportion of hospital resources, despite a relatively low proportion of beds allocated to caring for critically ill patients. Prolonged ICU stays, often characterized as ICU admissions beyond 7–15 days, have been shown to be associated with high mortality rates and consume significant health care resources.Citation19,Citation20–Citation22 Beyond initial hospitalization, prolonged ICU stays are associated with an increased risk for hospital readmission, death within 30 days of hospital discharge, and long-term physical disability on discharge.Citation23–Citation25 There are several ICU quality measures that have been implemented to reduce the length of ICU stays and the potential complications associated with long-term mechanical ventilation in the ICU. Particularly, the 2016 ASPEN/SCCM Nutrition Support Guidelines for Critically Ill Adults recommends early EN because of significant clinical data demonstrating that early EN improves patient outcomes through a reduction in infectious complications, length of mechanical ventilation, and overall length of hospital stay.Citation1
Although the clinical benefit of EN is well acknowledged, Gungabissoon et al reported that approximately one-third of critically ill patients developed GI intolerance which was associated with more frequent interruptions in enteral feedings and a reduction in delivery of daily protein and caloric requirements.Citation3 Despite adjusting for patient characteristics and disease severity, GI intolerance was an independent risk factor for prolonged ICU stay and resulted in a significantly higher 60-day mortality rate (30.8% versus 26.2%; p=0.04). Tirlapur et al recently found that diarrhea was associated with increased ICU stay and mortality after controlling for demographic and clinical characteristics, which provide further evidence of the association between GI intolerance and negative clinical outcomes in the ICU.Citation26
There is a limited and conflicting evidence base regarding the additional benefit of semi-elemental formula in ICU patients. As seen in some populations outside the ICU, these patients, representing a heterogeneous population (condition, severity, and therapeutic procedures), could still benefit from a semi-elemental formula compared with use of other formulas because the hydrolyzed protein and modified fat components are more readily absorbed, and the formula may be better tolerated than the standard formulaCitation9 or elemental formula.Citation27 Semi-elemental formula is approximately three times more expensive than standard formula; so, it is important to demonstrate that the additional expenditure will realize an improved outcome for the patient and an efficient use of resources.
We describe a cost–consequence model for an ICU cohort to estimate the potential savings with the initial use of a semi-elemental formula and to explore how many cases of GI intolerance would need to be avoided for the semi-elemental formula to be cost saving versus the standard formula. Three small studies of semi-elemental formula versus standard formula assessing adult patients in the ICU were identified, but none were prospective randomized trials assessing a range of GI intolerance outcomes for semi-elemental EN versus standard EN in a broad population of ICU patients. Jakob et al conducted a study on 89 adult ICU patients (medical and surgical).Citation16 The proportion of patients experiencing diarrhea during their ICU stay was lower in the semi-elemental group (64% versus the standard formula group [70%]) but was not statistically significant (risk ratio 0.91 [95% CI 0.68–1.22, p=0.65]). There were 0 days where feeding was interrupted because of diarrhea in the semi-elemental group and 2 days in the standard formula group (p=0.28). Liu et al studied 72 patients who recently underwent intra-abdominal surgery and received EN.Citation13 This retrospective trial found that the mean LOS in the ICU for the semi-elemental formula group was shorter than that for the standard formula group (6.2±0.8 versus 6.8±1.5 days). This study also demonstrated that the prevalence of suspended feeding due to high GRV resulted in a relative risk reduction of 30% in the semi-elemental formula group compared to the standard formula group. Additionally, the prevalence of diarrhea was 33% lower in the semi-elemental formula group. In a study conducted by Seres and Ippolito on 49 adult ICU patients (medical, surgical, cardiothoracic), the authors reported a 30% relative risk reduction of abdominal distension in the semi-elemental group versus the high protein polymeric formula group and a 40% reduction in the number of days with GI events (4.29 versus 7.13 days, p=0.0489).Citation17 These results suggest that the proportion of GI intolerance cases avoided with the semi-elemental formula is likely to be greater than the efficacy threshold calculated as being cost saving in the base case analysis (7.0%) or in the sensitivity analysis (3.5%–21.8%). Based on the published clinical data, if receiving the semi-elemental rather than standard formula leads to 30% of cases of GI intolerance (10 cases) avoided, then it would reduce the ICU stay by 28.8 days, representing a saving of $135,905 in the ICU cost of stay. The total savings for the cohort would be $104,105 lower for the semi-elemental formula cohort when the costs of EN are added to the ICU stay cost.
From the costs set out in , the relatively low cost of formula feed compared to the overall daily cost of an ICU stay can be observed. Thus, an intervention that reduces the length of ICU stay has the potential to realize significant cost savings. Gungabissoon et al reported that GI intolerance increased the median duration of ICU stay from 11.3 to 14.4 days.Citation3 Therefore, the higher cost of the semi-elemental compared with the standard formula is readily offset by the reduced incidence of GI intolerance and its associated ICU costs. Additionally, the Gungabissoon study reported that 50% of patients developed feeding intolerance between days 1 and 3 after EN initiation.Citation3 This finding further supports the initial use of the semi-elemental formula as a prudent strategy across the heterogeneous population of ICU patients for whom it is difficult to predict upfront if they are susceptible to develop digestive and absorption problems, because an overall cost saving is still observed in our model when three cases of GI intolerance are avoided for a cohort of 100 patients. Patient status (e.g., injury severity score, multiple organ dysfunction score), general conditions (e.g., abdominal surgery), and GI function (e.g., acute gastrointestinal injury grade), as well as biochemical indexes and treatment measures, should be considered as they represent potential risk factors for feeding intolerance.Citation28
There are several limitations to our study. First, no specific clinical trial data are available in the literature to estimate the proportion of GI intolerance cases that could be avoided by using semi-elemental nutrition versus standard nutrition in a diverse ICU population across the range of GI intolerance outcomes, as one trial was a retrospective analysis in patients with recent intra-abdominal surgery only,Citation13 one trial considered diarrhea outcomes only,Citation16 and the other trial compared a semi-elemental to a high-protein formula and not a standard polymeric formula.Citation17 Therefore, the model explored the threshold proportion of GI intolerance cases avoided, which resulted in cost savings with semi-elemental formula versus standard formula in the model. It should be noted that not all patients in the ICU setting will require a semi-elemental formula to avoid GI intolerance, as the incidence of GI intolerance varies depending on various factors including the underlying condition for admission. However, it can be difficult to predict GI intolerance a priori on ICU admission. Therefore, this model indicates that feeding the whole ICU cohort of 100 patients with a semi-elemental formula would be cost saving if three cases of GI intolerance are avoided. Second, this analysis only considers costs incurred within the ICU setting, and any further hospital cost savings outside of the ICU have not been assessed. Additional benefits of shortening ICU stays, such as improvement of long-term functional status, reduction in long-term mortality, and reduction in risk for hospital readmissions, have not been captured. Pendharkar et al reported that feeding intolerance in patients with acute pancreatitis was associated with poorer health-related quality of life (HRQoL).Citation29 It is, therefore, important to consider the overall consequences of GI intolerance on these broader factors: HRQoL, hospital readmission rates, time to recovery, and long-term outcomes alongside short-term ICU costs.
A randomized trial including a broad range of patients using enteral feeding in the ICU and assessing the impact of semi-elemental formula versus standard formula on LOS, recovery time outside the hospital, HRQoL, mortality, and overall treatment costs is required to enable the cost-effectiveness of semi-elemental nutrition to be more fully assessed. Assuming the proportion of patients with feed intolerance is 31% in ICU patients receiving standard EN and 28% in patients receiving semi-elemental nutrition, a trial of semi-elemental EN versus standard EN would require a sample size of n=3,627 per arm to achieve 80% power to detect this difference with a significance level of 5%. This represents the modeled simulation of a 7% reduction in feed intolerance in order for semi-elemental EN to be cost saving. A 25% reduction in feed intolerance (31% versus 23%) would require a sample size of n=482 per arm to achieve 80% power to detect this difference with a significance level of 5%.
To conclude, in theory, semi-elemental EN may be more easily digested, although there is no randomized clinical trial evidence to indicate this in the critically ill across the full range of GI intolerance outcomes. This analysis has been based on the best level of evidence currently available in the literature, but it is a modeled simulation only. Several guidelines recommend considering semi-elemental EN in particular cases, but clinicians may be reluctant to trial a semi-elemental EN due to the higher cost. This model shows that use of semi-elemental EN in 100 patients in the ICU would be cost saving versus standard polymeric EN if it led to 7% fewer feeding interruptions due to GI intolerance, which extrapolates to 6.75 fewer days LOS in the ICU. Further large randomized controlled trials are required to confirm whether semi-elemental EN can reduce GI intolerance-related feeding interruptions versus standard polymeric EN across the typical range of patients presenting in the ICU.
Acknowledgments
The development of the cost–consequence model described in this manuscript by SIRIUS Market Access was funded by Nestle S.A. Nestlé is a manufacturer of semi-elemental and polymeric enteral nutrition formulas.
Disclosure
The authors report no conflicts of interest in this work.
References
- McClaveSATaylorBEMartindaleRGSociety of Critical Care MedicineAmerican Society for Parenteral and Enteral NutritionGuidelines for the provision and assessment of nutrition support therapy in the adult critically III patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.)JPEN J Parenter Enteral Nutr201640215921126773077
- PeakeSLChapmanMJDaviesARGeorge Institute for Global HealthAustralian and New Zealand Intensive Care Society Clinical Trials GroupEnteral nutrition in Australian and New Zealand intensive care units: a point-prevalence study of prescription practicesCrit Care Resusc201214214815322697623
- GungabissoonUHacquoilKBainsCPrevalence, risk factors, clinical consequences, and treatment of enteral feed intolerance during critical illnessJPEN J Parenter Enteral Nutr201539444144824637246
- FerrieSEastVManaging diarrhoea in intensive careAust Crit Care200720171317424790
- NguyenNQNgMPChapmanMFraserRJHollowayRHThe impact of admission diagnosis on gastric emptying in critically ill patientsCrit Care2007111R1617288616
- ReintamAParmPKitusRStarkopfJKernHGastrointestinal failure score in critically ill patients: a prospective observational studyCrit Care2008124R9018625051
- Reintam BlaserAPoezeMMalbrainMLBjorckMOudemansvan StraatenHMStarkopfJGastro-Intestinal Failure Trial GroupGastrointestinal symptoms during the first week of intensive care are associated with poor outcome: a prospective multicentre studyIntensive Care Med201339589990923370829
- KreymannKGBergerMMDeutzNEESPEN (European Society for Parenteral and Enteral Nutrition)ESPEN guidelines on enteral nutrition: intensive careClin Nutr200625221022316697087
- AlexanderDDBylsmaLCElkayamLNguyenDLNutritional and health benefits of semi-elemental diets: a comprehensive summary of the literatureWorld J Gastrointest Pharmacol Ther20167230631927158547
- HegaziRAWischmeyerPEClinical review: optimizing enteral nutrition for critically ill patients – a simple data-driven formulaCrit Care201115623422136305
- MinorGOchoaJBStormHPerimanSFormula switch leads to enteral feeding tolerance improvements in children with developmental delaysGlob Pediatr Health201632333794X16681887
- Mowatt-LarssenCABrownROWojtysiakSLKudskKAComparison of tolerance and nutritional outcome between a peptide and a standard enteral formula in critically ill, hypoalbuminemic patientsJPEN J Parenter Enteral Nutr199216120241738214
- LiuMYTangHCHuSHChangSJPeptide-based enteral formula improves tolerance and clinical outcomes in abdominal surgery patients relative to a whole protein enteral formulaWorld J Gastrointest Surg201681070070527830042
- AlberdaCGramlichLJonesNThe relationship between nutritional intake and clinical outcomes in critically ill patients: results of an international multicenter observational studyIntensive Care Med200935101728173719572118
- MentecHDupontHBocchettiMCaniPPoncheFBleichnerGUpper digestive intolerance during enteral nutrition in critically ill patients: frequency, risk factors, and complicationsCrit Care Med200129101955196111588461
- JakobSMButikoferLBergerDCoslovskyMTakalaJA randomized controlled pilot study to evaluate the effect of an enteral formulation designed to improve gastrointestinal tolerance in the critically ill patient-the SPIRIT trialCrit Care201721114028599662
- SeresDSIppolitoPRPilot study evaluating the efficacy, tolerance and safety of a peptide-based enteral formula versus a high protein enteral formula in multiple ICU settings (medical, surgical, cardiothoracic)Clin Nutr201736370670927161892
- DastaJFMcLaughlinTPModySHPiechCTDaily cost of an intensive care unit day: the contribution of mechanical ventilationCrit Care Med20053361266127115942342
- BeckerGJStrauchGOSaranchakHJOutcome and cost of prolonged stay in the surgical intensive care unitArch Surg198411911133813426437374
- FakhrySMKercherKWRutledgeRSurvival, quality of life, and charges in critically III surgical patients requiring prolonged ICU staysJ Trauma199641699910078970553
- HeylandDKKonopadENoseworthyTWJohnstonRGafniAIs it “worthwhile” to continue treating patients with a prolonged stay (>14 days) in the ICU? An economic evaluationChest199811411921989674469
- LipsettPASwobodaSMDickersonJSurvival and functional outcome after prolonged intensive care unit stayAnn Surg2000231226226810674619
- Delle KarthGMeyerBBauerSNikfardjamMHeinzGOutcome and functional capacity after prolonged intensive care unit stayWien Klin Wochenschr200611813–1439039616865643
- CardenGPGrahamJWMcLennanSCeliLALong-term outcome of long stay ICU and HDU patients in a New Zealand hospitalCrit Care Shock2008111263423766668
- ChelluriLImKABelleSHLong-term mortality and quality of life after prolonged mechanical ventilationCrit Care Med2004321616914707560
- TirlapurNPuthuchearyZACooperJADiarrhoea in the critically ill is common, associated with poor outcome, and rarely due to Clostridium difficileSci Rep201662469127094447
- MakolaDElemental and semi-elemental formulas: are they superior to polymeric formulas?Pract Gastroenterol2005345972
- XuLWangTChenTYangWQLiangZPZhuJCIdentification of risk factors for enteral feeding intolerance screening in critically ill patientsSaudi Med J201738881682528762434
- PendharkarSAAsraniVDasSLAssociation between oral feeding intolerance and quality of life in acute pancreatitis: a prospective cohort studyNutrition20153111–121379138426429659
