?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Purpose
The aim of this study was to conduct a systematic literature review on the burden of schizophrenia in privately insured US patients.
Materials and methods
A systematic literature review of English language peer-reviewed journal articles of observational studies published from 2006 to 2016 was conducted using EMBASE/MEDLINE databases. Abstracts covering substantial numbers of patients with schizophrenia or schizoaffective disorder (i.e., N ≥ 100) were included for full-text review. Articles that did not clearly specify private insurance types were excluded.
Results
A total of 25 studies were reviewed; 10 included only privately insured patients; and 15 included a mix of different types of insurance. The review of the clinical burden of schizophrenia revealed the following: compared to patients with no mental disorders, those with schizophrenia had significantly increased odds of systemic disorders and both alcohol and substance abuse. Antipsychotic (AP) adherence was low, ranging from 31.5% to 68.7%. The medication possession ratio for AP adherence ranged from 0.22 to 0.73. The review of the health economic burden of schizophrenia revealed the following: patients with a recent (vs. chronic) diagnosis of schizophrenia had significantly higher frequencies of emergency department visits and hospitalizations and greater length of stay (LOS) and total annual per-capita costs. Mean all-cause hospitalizations and LOS decreased significantly after (vs. before) initiating long-acting injectable APs (LAIs). Patients also had significantly decreased mean all-cause, and schizophrenia-related, hospitalization costs after initiating LAIs. Total direct per-capita costs of care (but not pharmacy costs) for patients who were nonadherent to their oral APs within the first 90 days of their index event were significantly higher (vs. early adherent patients). Despite these potential benefits, only 0.25%–13.1% of patients were treated with LAIs across all studies.
Conclusion
Privately insured US patients with schizophrenia experience a substantial clinical and health economic burden related to comorbidities, acute care needs, nonadherence, and polypharmacy and have relatively low use of LAIs. Further study is warranted to understand prescribing patterns and clinical policies related to this patient population.
Introduction
Schizophrenia is a serious public health problem affecting approximately 1.1% of the world’s population, which includes about 3.5 million patients diagnosed in the United States; the annual incidence rate ranges from 10.2 to 22.0 per 100,000 person-years.Citation1,Citation2 It is one of the top 10 causes of disability around the world, and the mean life expectancy in Americans with schizophrenia is 12–15 years lower than in the general population.Citation3 Many patients with schizophrenia also suffer from substantial comorbidities and poor overall health habits, including personal neglect as well as alcohol and substance abuse.Citation3 Furthermore, nearly 40% of patients with schizophrenia in North America attempt suicide at some time in their lives, culminating in death by suicide in 10%.Citation4,Citation5
This profound psychiatric disorder often has its onset during an individual’s (otherwise) most formative and productive years, with nearly 75% of patients developing schizophrenia between the ages of 16 and 25 years.Citation1 The condition is also often associated with socioeconomic deprivation, and most adults with schizophrenia receive government health insurance; only 15% are covered by private insurance plans.Citation6,Citation7
Under the Patient Protection and Affordable Care Act (ACA) of 2010, which mandates coverage up to 26 years of age, many patients with early-onset schizophrenia are now insured under their parents’ employer-based health plans. According to projections from the Centers for Medicare & Medicaid Services (CMS), the impact of the federal mandate extension of commercial coverage would result in 1.2 million young adults receiving care under their parents’ health plans.Citation8 Although the prevalence of schizophrenia in privately insured patient populations is low, the overall annual US cost burden of schizophrenia is up to $63 billion, including about $23 billion (~35%) in excess direct health care costs ($8.0 billion for long-term care; $7.0 billion for outpatient care; $5 billion for medications; and $2.8 billion for hospitalization); $9 billion (~15%) in direct non-health care costs; and $32.4 billion (~50%) in total excess indirect costs.Citation9
Given a potential imminent rise in numbers of patients suffering from schizophrenia who are covered by private insurance plans, and the seriousness of this public health problem, many health care providers and other decision makers would benefit by developing an enhanced understanding of the burden of illness and unmet need of this population. Most of the contemporary understanding of the clinical and health economic (HE) burden of schizophrenia in the US has been built from studies of patients covered under publicly funded health insurance plans. Much less is known about the burden of schizophrenia in privately insured patients. Thus, the chief objective of this study was to review available real-world evidence (RWE) studies focusing on the clinical and HE burden of schizophrenia in privately insured populations.
Materials and methods
An EMBASE/MEDLINE search of peer-reviewed journal articles of observational studies in the English language clinical and HE literature, published from 2006 to 2016, was conducted. The search terms were grouped into “patient type” (e.g., “schiz*” AND “commercially insured” OR “privately insured” OR “employer sponsored”), “treatment options” (e.g., “antipsychotic” OR “antipsychotics” OR “depot” OR “LAI” OR “long-acting” OR “injectable” OR “oral medication), “clinical burden” (e.g., “relapse” OR “hospitalization” OR “admission*” OR “emergen*” OR “emergency room” OR “emergency department” OR “comorbidity” OR “remission” OR “outpatient” OR “inpatient” OR “discontinuation” OR “adherence”), and “health economic burden” (e.g., “financ*” OR “economic*” OR “cost*” OR “resource*” OR “utiliz*”). Search terms are tabulated in .
To enrich the output, a supplementary search in PubMed was conducted. This search crossed key terms (using the Boolean operator “AND”) with the names of leading HE journals (i.e., Journal of Managed Care Pharmacy, Journal of Medical Economics, Pharmacoeconomics, and Value in Health).
Abstracts of studies that evaluated the burden of schizophrenia in patients with private (i.e., mainly employer-based) insurance plans were reviewed. Reports of studies that included ≥100 patients with schizophrenia or schizoaffective disorder were included for full-text review. Any studies that assessed iatrogenic medication effects or did not specify private insurance were excluded.
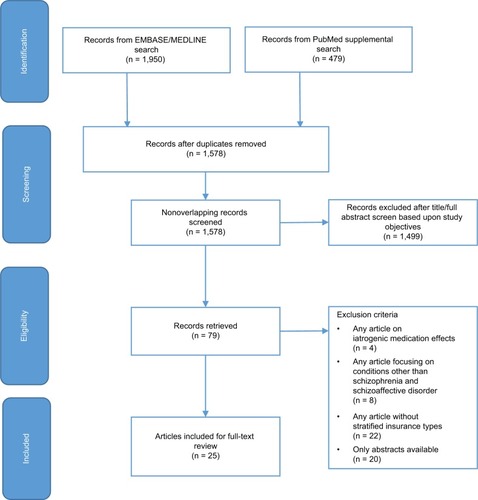
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart, which details the search and supplementary search strategies and outcomes, is shown in .
Results
Patient characteristics
After screening 1,578 unique citations, we retained 25 full-length peer-reviewed articles for the current study.Citation2,Citation6,Citation7,Citation10–Citation31 In total, this study encompassed 81,327 privately insured patients with schizophrenia and other related disorders, as categorized (in most studies reviewed in this study) by the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code of 295.xx.
Of the 25 studies covered in this literature review, 10 included only privately insured patients, and 15 included patients with a mix of different types of insurance. Privately insured patients with schizophrenia accounted for nearly half of the sample population within the systematic literature review. A total of 45.5% of patients had private insurance, 54.1% were covered under public plans (Medicare, Medicaid, Veterans Affairs), and the insurance status of the remaining 0.4% was unknown. Only data on privately insured patients are presented in the “Results” section of this study.
Patient demographics are summarized in .
Table 1 Patient characteristics
Key findings on clinical burden of schizophrenia
Clinical burden of nonremitting disease
One study report was appropriate for, and reviewed in, this section.Citation12
The 3-year prospective US Schizophrenia Case and Assessment Program (US-SCAP) study, which investigated the clinical and functional elements of remission in 2,284 adults with schizophrenia (or schizoaffective/schizophreniform disorder), found that patients who were not in remission at enrollment had significantly lower adherence to medication regimens (p < 0.001) and greater impairment of functional status and health-related quality of life.Citation12
Clinical burden of comorbidities
One study report was appropriate for, and reviewed in, this section.Citation13
A retrospective analysis of longitudinal administrative claims data from patients with schizophrenia (or schizoaffective disorder; i.e., cases) and 726,262 patients who filed at least one claim for medical services (but not for mental disorders, i.e., controls) from 1996 to 2001 in the Iowa Well-mark Blue Cross/Blue Shield plan, evaluated comorbidities. This study revealed that 33% of the studied population with schizophrenia (n = 1,074) had ≥3 chronic medical comorbidities, and only 29% of patients with schizophrenia had no claims for comorbid conditions.Citation13
Compared to patients with no mental disorders, individuals with schizophrenia had significantly increased odds of conditions that can adversely affect clinical outcomes, including 1) an approximately twofold increased odds of certain systemic disorders (e.g., odds ratio [OR] = 2.62; 95% confidence interval [CI] = 2.09–3.28 for hypothyroidism and 2.11 [95% CI = 1.36–3.28] for diabetes with complications); 2) an approximately 10-fold increased odds of other neurologic conditions (OR = 9.67; 95% CI =7.66–12.21); 3) an approximately 12-fold increased odds of alcohol abuse/dependence (OR = 12.57; 95% CI = 10.16–15.55); and 4) a 35-fold increased odds of illicit substance abuse/dependence (OR = 35.42; 95% CI= 28.35–44.27).Citation13
Clinical burden of nonadherence and effects of long-acting injectable antipsychotic (LAI) regimens
summarizes most reviewed studies that evaluated nonadherence among patients with schizophrenia.Citation2,Citation7,Citation12,Citation16–Citation19 Overall, medication adherence was suboptimal, ranging from 31.5% to 68.7%.Citation15,Citation17
Table 2 Medication adherence
According to studies included in this review, the medication possession ratio (MPR) for antipsychotic (AP) adherence ranged from 0.22 to 0.73 in privately insured patients ().Citation2,Citation18 In a study of the Thomson Reuters MarketScan IMS LifeLink database of AP prescriptions from January 1, 2008, to June 30, 2009, 44.6% of privately insured patients were nonadherent at a threshold for nonadherence of MPR < 0.80 during the 1-year follow-up period.Citation7 Patients who either newly initiated APs or were nonadherent at baseline had an eightfold increase in AP nonadherence over 1 year of follow-up.Citation7
Another study that included patients with schizophrenia focused on treatment adherence among individuals with schizoaffective disorder and either incident or prevalent disease who had records in the Clinformatics Data Mart database from January 1, 2009, to December 31, 2012. For the purposes of analysis, patients designated to have incident schizoaffective disorder had no claims for this condition during the 12 months before the index date, while those with prevalent disease did have claims in this baseline period.Citation16 Of all privately insured patients, 51% were nonadherent according to an MPR < 0.80 and 62% according to a proportion of days covered (PDC) < 0.80. Patients with incident (vs. prevalent) disease had significantly greater nonadherence (55.1% vs. 41.3%, respectively [p < 0.001] by MPR < 0.80 and 66.4% vs. 51.5%, respectively [p < 0.001] by PDC < 0.80).Citation16
Across studies, proportions of patients using LAIs ranged from 0.25%Citation31 to 13.1%.Citation10,Citation16,Citation18 An analysis by Lin et alCitation10 of a MarketScan commercial database consisting of 3,004 patients with schizophrenia who initiated LAIs (n = 394) or oral APs (n = 2,610) from 2005 to 2010 showed that adherence was significantly higher during the post-index period on LAIs compared to either the pre-LAI baseline or oral APs.
These data were supported by Peng et al’s study of 147 patients with schizophrenia who initiated LAIs and had records in the Thomson Medstat MarketScan Commercial Claims and Encounters Database from January 1, 2004, to March 31, 2008. Mean MPR increased from 0.368 within 6 months before initiating LAIs to 0.600 within 6 months afterward (p < 0.001).Citation24
Clinical burden of polypharmacy
One study report was appropriate for, and reviewed in, this section.Citation20
Patients with schizophrenia who received prescriptions for ≥1 AP, especially younger individuals around the time of the incident schizophrenia event, experienced significantly reduced adherence to these regimens compared to those receiving prescriptions for monotherapy.Citation20 In a study of 4,156 patients included in the HealthCore Integrated Research Environment (HIRE) database from January 1, 2007, to April 30, 2010, 968 (23.3%) patients received polypharmacy (vs. monotherapy) and had significantly reduced adherence to these regimens, especially younger individuals.Citation20
Key findings on HE burden
HE burden of nonremission
One study report was appropriate for, and reviewed in, this section.Citation12
Studying 2,327 adults with schizophrenia in the prospective US-SCAP trial, Haynes et alCitation12 found that health care costs were significantly higher in nonremitted (vs. remitted) patients across 3 years.
HE burden of nonadherence and effects of LAI regimens
Nine reports of six studies provided data on medication non-adherenceCitation2,Citation7,Citation10,Citation12,Citation15–Citation19 (three reports involved the same study populationCitation2,Citation10,Citation18). A claims database study of patients in the Truven MarketScan® Commercial Claims and Encounters database who initiated oral APs from January 1, 2006, to September 30, 2009, revealed significant increases in numbers of all-cause and schizophrenia-specific hospitalizations, as well as mean LOS values associated with each type of admission, among patients who were early nonadherers compared to early adherers (within 90 days of the index schizophrenia event; ).Citation2
Table 3 Health resource utilization (HRU) and costs for privately insured US patients with schizophrenia: comparisons across all studies
Another Truven MarketScan analysis, of 394 patients who initiated LAIs from January 1, 2005, to September 30, 2010, reported significant reductions in all-cause and schizophrenia-related hospitalization costs and total annual per-capita costs after (vs. before) initiating LAIs ().Citation18
In two different studies of the same population of privately insured patients with schizophrenia, mean all-cause and schizophrenia-related hospitalization costs significantly decreased after (vs. before) initiating LAIs ().Citation10,Citation18 Mean all-cause hospitalizations after initiating LAIs decreased from 1.60 days to 0.7 day (p < 0.001).Citation10 The corresponding decrease in LOS after initiating LAIs was 10.3 days for all-cause hospitalizations (p < 0.001; ).Citation10 Increased adherence and prescription drug costs were offset by annual reductions in costs for both all-cause and schizophrenia-related hospitalizations. Conversely, patients who initiated oral APs experienced significant increases in these costs ().Citation10
In the study by Peng et alCitation24 of 147 patients with schizophrenia, health resource utilization (HRU) and costs declined significantly at 6 months after (vs. 6 months before) initiating LAIs. Proportions of patients with psychiatric hospitalizations decreased from 49.7% to 22.4% (p < 0.001), and the mean LOS of psychiatric hospitalizations decreased from 7.3 to 4.7 days (p = 0.054). Introduction of LAIs was also associated with significant decreases in all-cause health care costs, which were largely due to a significant decrease in psychiatric hospitalization cost ().
A hospital claims database analysis from 2006 to 2010 by Lafeuille et alCitation27 examined HRU in relapsed patients with schizophrenia using oral APs who either remained on these medications or switched to LAIs. During 30 months of follow-up, patients using LAIs (vs. oral APs) had significantly fewer emergency department (ED) visits and rehospitalizations, with significantly (12%–19%) reduced likelihoods of each (hazard ratio [HR] 0.88, 95% CI = 0.87–0.93 [p < 0.0001] for ED visits and HR = 0.81; 95% CI = 0.76–0.87 [p < 0.0001] for rehospitalizations).
HE burden of polypharmacy
One study report was appropriate for, and reviewed in, this section.Citation23
A claims database analysis by McCombs et alCitation23 found that patients with schizophrenia who initiated treatment with ≥2 medications were more likely to be hospitalized during the first year (42.2% vs. 34.0%) and incur greater associated per-capita costs ($12,806 vs. $9,413) compared to those receiving monotherapy.
HE burden of incident (vs. prevalent) disease
Two study reports were appropriate for, and reviewed in, this section.Citation14,Citation21
One study that examined a privately insured patient population with schizophrenia in California (N = 414) from June 2001 to May 2004 found that, during a 12-month treatment period, newly diagnosed patients had significantly lower costs for all-cause (p = 0.0002) and schizophrenia-specific (p = 0.02) medication prescriptions compared to previously diagnosed individuals (). However, the newly (vs. previously) diagnosed patients also incurred significantly greater expenses for inpatient services (total p = 0.03; schizophrenia-specific p = 0.04) and all-cause outpatient medical care (p = 0.01).Citation21
Another study, conducted by Nicholl et al,Citation14 similarly assessed medical and pharmaceutical claims data for patients recently diagnosed with schizophrenia, approximately 80% of whom were covered by private insurance plans. These researchers demonstrated that patients with recently diagnosed (vs. chronic) schizophrenia had a higher rate of psychiatric hospitalization (22.3% vs. 12.4%; p < 0.0001). Resource allocation was also higher in patients with recently diagnosed illness, who had a longer average LOS in hospital (5.1 vs. 3.0 days; p = 0.0065) and made more frequent use of ED resources (). There was also a nearly twofold increase in mean annual per-capita health care costs in the year after (vs. before) schizophrenia was diagnosed ($20,654 vs. $10,177; p < 0.0001). Finally, difficulties in coping within the first year after incident schizophrenia may be reflected by a two- to fivefold increase in frequencies of alcohol or drug dependence (or substance abuse) and suicidal behaviors in recently diagnosed patients with schizophrenia who were enrolled in the PharMetrics Integrated Database from 1998 to 2007.
Discussion
This systematic literature review synthesized RWE for patients with schizophrenia over the past decade from the US private insurance payer perspective and highlighted the fact that privately insured patients with schizophrenia experienced a substantial clinical and economic burden, including suboptimal health outcomes. The outcomes examined in the current review ranged widely and included comorbidity, polypharmacy, nonremission or relapse, and treatment adherence.
Research on privately insured patients with schizophrenia has been minimal, with only 25 peer-reviewed journal articles identified in the current systematic literature review. On the other hand, the evidence presented in this study resembles findings reported for publicly insured populations (i.e., Medicaid, Medicare, and Veterans Affairs).Citation7,Citation10,Citation18,Citation30,Citation32
Published literature on Medicaid recipients and other publicly insured patients suggests that these individuals with schizophrenia may have more adverse clinical and economic outcomes, which can be attributed primarily to comorbidities, polypharmacy, less continuity of care, relapse, and poor medication adherence. For example, Williams et alCitation32 found that Medicaid payment status was significantly correlated with an approximately threefold elevation in the risk of AP polypharmacy (OR = 2.73; 95% CI = 1.11–6.68; p = 0.03) compared to other forms of insurance or no insurance.
Further, in Citrome et al’s studyCitation33 of Truven Health Analytics MarketScan® Multi-State Medicaid and Commercial insurance claim databases, prevalences of certain potentially treatment-limiting adverse risk factors (i.e., extrapyramidal symptoms, diabetes, obesity, QT interval prolongation, and hyperprolactinemia) were higher in Medicaid (vs. privately insured) patients with schizophrenia. In an analysis of the Truven Multi-State Medicaid and IMS LifeLink Health Plan claims data from 2008 to 2009, Lang et alCitation7 also reported that the mean (SD) cost per all-cause hospitalization in patients with schizophrenia was $14,528 ($21,113) in Medicaid patients compared to $9,796 ($11,462) in privately insured individuals.
Long-acting medication regimens for schizophrenia have been found to be effective in improving treatment adherence and reducing risks of relapse and hospitalization in both privately and publicly insured populations. For example, the analyses of the Truven MarketScan database by Offord et alCitation18 identified statistically significant improvements in AP adherence and reductions in hospitalizations, LOS, and mean costs, after (vs. before) initiating LAIs in 665 Medicare (as well as in 3,004 privately insured) patients with schizophrenia.Citation10 Similarly, Lafeuille et alCitation27 found that there was a 36% relative risk reduction in rehospitalization with LAIs compared to oral APs, in an analysis of electronic medical record data from the Premier Perspective Comparative Hospital Database (Premier).
Long-acting injectable therapies are generally available via hospital formularies and have also shown potential to alleviate clinical and economic burden associated with schizophrenia, but the overall use of these agents remains relatively low in both publicly and privately insured populations. In this review, only 0.25%–13.1% of privately insured patients were treated with LAIs across all studies.Citation10,Citation16,Citation18 A broad literature review on AP adherence concluded that “LAIs represent a valuable option for treating schizophrenia given the known improvement in adherence, and yet these formulations are largely underutilized.”Citation4
Although LAI therapies were found to have favorable effects in limiting the economic burden of schizophrenia management, these observations were made in only three studies.Citation7,Citation10,Citation18 Our findings should be corroborated in larger and more heterogeneous patient populations assessed in pragmatic, longitudinal studies. Ongoing issues related to LAI use include the settings in which to initiate treatment, such as first-episode psychosis and acute exacerbations of schizophrenia in a setting of prior nonadherence.Citation34
The focused scope of our systematic literature review may have precluded consideration of potential barriers to LAI use, including prior authorization requirements.Citation35,Citation36 The clinical and economic benefits in patients treated with LAIs across multiple observational studies in the present review suggest that access to LAIs within private health plans should be further assessed.
Our review also found that little information is available on young adult, privately insured patients with schizophrenia, despite the health care expansion mandate that young patients (aged ≤26 years) be eligible for coverage under their parents’ health insurance plans. Notably, although the onset of schizophrenia usually occurs in an individual’s early 20s, an accurate schizophrenia diagnosis may not be made until several years after incident psychosis.
Future research is needed to better understand the humanistic, clinical, and economic burden of schizophrenia. Such work might include meta-analyses if data are sufficiently homogeneous to be pooled. The field might be advanced by conducting a similar systematic literature review to the current study, or a meta-analysis, that also encompasses larger numbers of studies of more diverse patient populations with both employer-based and public health insurance. Other potential future lines of inquiry might involve assessments of: 1) patients with either public or commercial health insurance; 2) ex-US societies, including those with different prevailing forms of coverage (e.g., universal health care); 3) indirect and direct health care costs; 4) different patient profiles (including different age strata and “patient journeys”); and 5) distinct perspectives aside from that of the payer taken in our review (e.g., patient’s or caregiver’s perspective).
Limitations
Despite the rigorous methodology employed in this review, it is not without limitations. For example, 24 of the 25 peer-reviewed articles included in this review were retrospective, observational cohort studies of administrative claims databases. The observational nature of the studies analyzed does not enable us to conclusively rule out biases and exclude confounding on unmeasured variables, especially given that certain databases (e.g., MarketScan) analyzed in the base studies were derived from large, nonrandom (convenience) samples.
International Classification of Diseases codes used to identify patients in these studies were developed for reimbursement, not case ascertainment, purposes, opening the possibility of coding errors. Reported costs were as identified in each study and not corrected to any single inflation-adjusted annual currency values or 2016–2017 dollars. Because our study was specifically designed to evaluate US residents, its findings cannot necessarily be extrapolated to other (ex-US) populations with potentially divergent health delivery systems and practices.Citation37
Although the EMBASE/MEDLINE searches were exhaustive, given the prespecified eligibility criteria, the amount of information was still confined to only 25 peer-reviewed studies, of which fewer than half (10) included only privately insured patients: 45.5% of the total study sample population in all studies that were included. The 81,327 privately insured patients reported in the “Results” section may overestimate the actual number of patients studied, because this number did not necessarily include unique patients; certain studies (including those by Offord et al,Citation2 Lin et al,Citation10 and Offord et alCitation18) evaluated the same population.
Variables analyzed in the 25 studies were too divergent to enable meaningful pooling of the data or conducting more rigorous statistical tests of publication bias (e.g., by funnel plots) and heterogeneity (e.g., by the I2 test). In addition to a large plurality of variables contributing to the cost of burden of schizophrenia in employer-based health systems, there were relatively few studies available for each, prespecified cost component of interest. Overall, these factors precluded pooling of the data and conducting a meta-analysis, which might have otherwise strengthened our study findings.
Conclusion
Privately insured patients with schizophrenia are confronted with a substantial clinical and economic burden related to comorbidities, acute care needs, treatment nonadherence, and polypharmacy. Although not prevalent, treatment with LAIs has been shown to significantly promote adherence and reduce both overall HRU and direct health care costs, such as all-cause and schizophrenia-related hospitalization. On the basis of this systematic literature review, further research is warranted to better understand prescribing patterns and clinical policies related to managing schizophrenia and optimal ways to enhance patient outcomes.
Author contributions
All authors were involved in study design. WZ and SWG were involved in data acquisition. All authors were involved in data interpretation. SWG and WZ were involved in drafting the manuscript, and all other authors provided substantive intellectual contributions to the text and graphics. All authors reviewed and approved the final draft and take full responsibility for the study, its findings, and this report.
Acknowledgments
This study and its report were supported by Janssen Scientific Affairs, LLC (Titusville, NJ, USA), which had a role in the design of the study, drafting of the manuscript, and the decision to report the findings.
Supplementary material
Table S1 Search terms and outcomes
Disclosure
WZ, SWG, and NL are employed by WG AHA, which consults with Janssen Scientific Affairs, LLC, and other life science companies. They have no other financial interests to disclose. KJ & TBA are employees of Janssen Scientific Affairs, LLC and shareholders of Johnson & Johnson. When the study was conducted and the manuscript drafted, EG was an employee of WG AHA. The authors report no other conflicts of interest in this work.
References
- Schizophrenia and Related Disorders Alliance of America [homepage on the Internet]Schizophrenia and Related Disorders Alliance of America: About Schizophrenia Available from: http://www.sardaa.org/Accessed March 29, 2018
- OffordSLinJMirskiDWongBImpact of early nonadherence to oral antipsychotics on clinical and economic outcomes among patients with schizophreniaAdv Ther201330328628923483449
- KennedyJLAltarCATaylorDLDegtiarIHornbergerJCThe social and economic burden of treatment-resistant schizophreniaInt Clin Psychopharmacol2014292637623995856
- KaplanGCasoyJZummoJImpact of long-acting injectable anti-psychotics on medication adherence and clinical, functional, and economic outcomes of schizophreniaPatient Prefer Adherence201371171118024265549
- Fuller-ThomsonEHollisterBSchizophrenia and suicide attempts: findings from a representative community-based Canadian sampleSchiz Res Treat20163165243111
- KhaykinEEatonWFordDAnthonyCDaumitGHealth insurance coverage among persons with schizophrenia in the United StatesPsy-chiatr Serv2010618830834
- LangKFedericoVMuserEMenzinJMenzinJRates and predictors of antipsychotic non-adherence and hospitalization in Medicaid and commercially-insured patients with schizophreniaJ Med Econ2013168997100623777223
- Centers for Medicare & Medicaid Services [webpage on the Internet]Young Adults and the Affordable Care Act: Protecting Young Adults and Eliminating Burdens on Families and Businesses2010 Available from: https://www.cms.gov/CCIIO/Resources/Files/adult_child_fact_sheet.htmlAccessed May 19, 2017
- WuEQBirnbaumHGShiLThe economic burden of schizophrenia in the United States in 2002J Clin Psych20056611221129
- LinJWongBOffordSMirskiDHealthcare cost reductions associated with the use of LAI formulations of antipsychotic medications versus oral among patients with schizophreniaJ Behav Health Serv Res201340335536623579871
- CloutierMSanon AigbogunMGuerinAThe economic burden of schizophrenia in the United States in 2013J Clin Psychiatry201677676477127135986
- HaynesVSZhuBStaufferVLLong-term healthcare costs and functional outcomes associated with lack of remission in schizophrenia: a post-hoc analysis of a prospective observational studyBMC Psychiatry201212122223216976
- CarneyCPJonesLWoolsonRFMedical comorbidity in women and men with schizophrenia: A population-based controlled studyJ Gen Intern Med200621111133113717026726
- NichollDAkhrasKSDielsJSchadrackJBurden of schizophrenia in recently diagnosed patients: healthcare utilisation and cost perspectiveCurr Med Res Opin201026494395520163295
- GibsonTBJingYKimECost-sharing effects on adherence and persistence for second-generation antipsychotics in commercially insured patientsManag Care20101984047
- JoshiKLinJLingohr-SmithMFuD-JMuserETreatment patterns and antipsychotic medication adherence among commercially insured patients with schizoaffective disorder in the United StatesJ Clin Psychopharmacol201636542943527525965
- KimEGuptaSBolgeSChenC-CWhiteheadRBatesJAAdherence and outcomes associated with copayment burden in schizophrenia: a cross-sectional surveyJ Med Econ201013218519220235753
- OffordSWongBMirskiDBakerRALinJHealthcare resource usage of schizophrenia patients initiating long-acting injectable antipsychotics vs oralJ Med Econ201316223123923163287
- PyensonBGoldbergSIwasakiKBoyarskyVDiraniRA Medicaid and commercial insured claims-based study to estimate improved antipsychotic medication adherence among patients with schizophreniaJ Behav Health Serv Res201340222223323456182
- FisherMDReillyKIsenbergKVillaKFAntipsychotic patterns of use in patients with schizophrenia: polypharmacy versus monotherapyBMC Psychiatry20141434125433495
- WilsonLSGitlinMLightwoodJSchizophrenia costs for newly diagnosed versus previously diagnosed patientsAm J Pharm Benefits201132107115
- RostKHsiehYPXuSMenachemiNYoungASPotential disparities in the management of schizophrenia in the United StatesPsychiatr Serv201162661321632729
- McCombsJZolfaghariSGanapathyVImpact of drug treatment history on comparative effectiveness research in schizophreniaValue Health201114567968621839406
- PengXAscher-SvanumHFariesDConleyRRSchuhKJDecline in hos-pitalization risk and health care cost after initiation of depot antipsychotics in the treatment of schizophreniaClin Outcomes Res201131914
- DoddsTJPhutaneVHStevensBJWoodsSWSernyakMJSrihariVHWho is paying the price? Loss of health insurance coverage early in psychosisPsychiatr Serv201162887888121807825
- FitchKIwasakiKVillaKFResource utilization and cost in a commercially insured population with schizophreniaAm Health Drug Benefits201471182624991388
- LafeuilleM-HLaliberté-AugerFLefebvrePFroisCFastenauJDuhMSImpact of atypical long-acting injectable versus oral antipsychotics on rehospitalization rates and emergency room visits among relapsed schizophrenia patients: a retrospective database analysisBMC Psychiatry20131322124016390
- PanishJMDiraniRHalpernRCaoFExploratory analysis of psychiatric-related utilization and costs associated with paliperidone ER compared with other oral atypical antipsychotics using pharmacy claims from an administrative databaseJ Med Econ201013461061720879914
- StenslandMWatsonPRGrazierKLAn examination of costs, charges, and payments for inpatient psychiatric treatment in community hospitalsPsychiatr Serv201263766667122588167
- WangCCFarleyJFPatterns and predictors of antipsychotic medication use among the U.S. population: Findings from the Medical Expenditure Panel SurveyRes Social Adm Pharm2013926327521272525
- GianfrancescoFRajagopalanKWangRHospitalization risks in the treatment of schizophreniaJ Clin Psychopharmacol200626440140416855459
- WilliamsEOStockEMZeberJEPayer types associated with antipsychotic polypharmacy in an ambulatory care settingJ Pharm Health Serv Res201233149155
- CitromeLEramoAFrancoisCLack of tolerable treatment options for patients with schizophreniaNeuropsychiatr Dis Treat2015113095310426719694
- SacchettiEGrunzeHLeuchtSVitaALong-acting injection anti-psychotic medications in the management of schizophreniaEvid Based Psychiatric Care201512736
- SeaburySAGoldmanDPKalsekarISheehanJJLaubmeierKLakdawallaDNFormulary restrictions on atypical antipsychotics: impact on costs for patients with schizophrenia and bipolar disorder in MedicaidAm J Manag Care2014202e52e6024738555
- LawMRRoss-DegnanDSoumeraiSBEffect of prior authorization of second-generation antipsychotic agents on pharmacy utilization and reimbursementsPsychiatric Serv2008595540546
- MancusoASpecchiaMLLovatoEEconomic burden of schizophrenia: the European situation. A scientific literature reviewEur J Public Health201424suppl_235135224642605