Abstract
Objective:
This study compared adherence and persistence of three branded antidepressants: the serotonin and norepinephrine reuptake inhibitors (SNRIs) duloxetine and venlafaxine XR, and the selective serotonin reuptake inhibitor (SSRI) escitalopram; and generic selective SSRIs, and examined demographic and clinical predictors of adherence and persistence in patients with major depressive disorder in usual care settings.
Method:
A total of 44,026 patients (18 to 64 years) from a large commercial administrative claims database were classified as initiators of duloxetine (n = 7,567), venlafaxine XR (n = 6,106), escitalopram (n = 10,239), or generic SSRIs (n = 20,114) during 2006. Adherence was defined as the medication possession ratio of ≥0.8 and persistence as the length of therapy without exceeding a 15-day gap. Pairwise comparisons from multivariate logistic regression and Cox proportional hazards models were performed to examine predictors of adherence and persistence.
Results:
Adherence rate after one year was significantly higher in duloxetine recipients (38.1%) than patients treated with venlafaxine XR (34.0%), escitalopram (25.4%), or generic SSRIs (25.5%) (all P < 0.01). Duloxetine recipients stayed on medication longer (158.5 days) than those receiving venlafaxine XR (149.6 days), escitalopram (129.1 days), or generic SSRIs (130.2 days) (all P < 0.001). Compared with patients treated with escitalopram or generic SSRIs, venlafaxine XR recipients had better adherence and longer persistence (P < 0.001). In addition, being aged 36 years or more, hypersomnia, anxiety disorders, and prior use of antidepressants were associated with increased adherence and persistence, while the opposite was true for comorbid chronic pain conditions, alcohol and drug dependence, and prior use of amphetamine.
Conclusion:
Compared with SSRIs, the SNRIs appear to have better adherence and persistence. Among SNRIs, duloxetine had statistically significantly better adherence and persistence than venlafaxine XR, though differences were relatively small and further research is needed to assess whether these translate into clinically and economically meaningful outcomes. Adherence and persistence with antidepressant therapy were associated with age, multiple comorbid conditions, and prior use of medications.
Introduction
Major depressive disorder (MDD) is among the most prevalent and costly psychiatric disorders.Citation1–Citation3 Antidepressants are the mainstay treatment of MDD and optimal antidepressant treatment includes the selection of the right medication and delivery at a fully therapeutic dose for a sufficient treatment duration.Citation4,Citation5
However, antidepressant nonadherence remains a challenging problem in the treatment of depression. Treatment is often accompanied by premature discontinuation and switching of antidepressant medications,Citation8 which may be associated with likelihood of relapse and higher health-care costs.Citation9,Citation10 Research demonstrates that 28% of patients discontinue use of their antidepressant medication within the first month, and by three months, at least 40% have discontinued use.Citation11 Approximately 16% of patients remain on therapy for more than 90 days without evidence of therapy changes, titration in dose, or being only partially compliant.Citation12 The early discontinuation of antidepressant medication is statistically associated with a 77% increase in the risk of relapse.Citation10
In many cases, poor adherence or discontinuation of therapy was thought to be an effect related primarily to adverse events or lack of therapeutic response.Citation13 However, there are multiple factors that may put patients at risk for poor adherence or discontinuation. Many patient-related, disease-related, medication-related, and physician-related factors, along with the health care system and costs may influence a patient’s adherence to medication therapy.Citation13–Citation21
The second generation of antidepressants, such as selective serotonin (5-HT) reuptake inhibitors (SSRIs) and serotonin and norepinephrine (NE) reuptake inhibitors (SNRIs), are commonly used in the treatment of depression. Although findings are inconsistent, some studies suggest that SNRIs that modulate both 5-HT and NE activity may be more effective than SSRIs for patients with more severe major depression.Citation22,Citation23 Although some antidepressants are grouped into the same class, they may have different pharmacological and clinical profiles.Citation24–Citation27
At the time of the analyses, three branded antidepressants commonly used in the treatment of depression in the United States were two SNRIs: duloxetine (DLX) and venlafaxine (VLX) and one SSRI: escitalopram (ECP). Recent research showed that DLX-treated patients had more comorbid conditions, especially chronic pain-related diseases, and that ECP-treated patients were very similar to generic SSRI (GSSRI)-treated patients in demographic characteristics and comorbid conditions.Citation28 Branded antidepressants are usually more expensive than GSSRIs. However, little is known about treatment patterns and the clinical and economic consequences of patients treated with branded antidepressants compared with GSSRIs. The objectives of this study were to examine treatment adherence and persistence with the three branded antidepressants DLX, VLX, and ECP, and GSSRIs in the treatment of major depression, and to examine demographical and clinical predictors of adherence and persistence with antidepressant therapy in the usual clinical setting.
Patients and Methods
Data source and sample selection
This retrospective analysis of claims data employed medical, pharmacy, and enrollment information from the Thomson Reuters MarketScan Commercial Claims and Encounters Databases, which includes de-identified administrative claims databases of employees, spouses, and dependents with employer-sponsored commercial insurance. Inpatient and outpatient medical and pharmacy claims are linked to enrollment data for a variety of plan types. This database captures the annual health care information of approximately 20 million individuals, including inpatient and outpatient medical claims linked to pharmacy and enrollment data for a variety of health insurance plan types. Each medical claim includes at least one International Classification of Diseases (ICD), 9th Edition, Clinical Modification (ICD-9-CM) diagnostic code to describe the patient’s clinical condition. All pertinent patient information in the database was encrypted and de-identified. The MarketScan database is publicly available as a fee-for-service database and has been used for a number of previous retrospective and prospective analysis projects.Citation29,Citation30
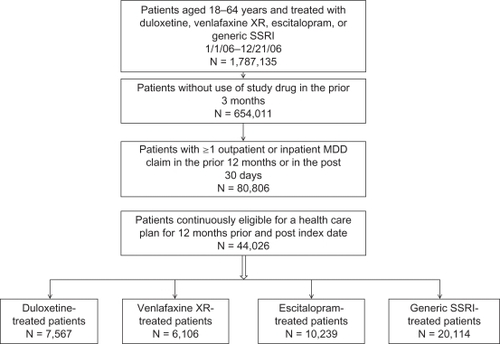
Patients were included in the study if they had a first prescription fill for DLX, VLX, ECP, or a GSSRI in 2006, had no active prescriptions of the same study medication in the three months prior to the index date, and had one or more inpatient or outpatient claims associated with a diagnosis of MDD (ICD-9-CM: 296.2 and 296.3) one year prior to or one month after the study medication was initiated. Patients had to be 18 to 64 years of age, commercially insured, and have continuous enrollment in the previous and following twelve months. Patients initiated on more than one study medication (DLX, VLX, ECP, or GSSRIs) during 2006 at different times were grouped into the first medication initiation cohort while those starting on more than one type of study medication on the index date were excluded from the study. Patients were grouped into four mutually exclusive cohorts: DLX, VLX, ECP, or GSSRI. The study design and sample selection are illustrated in .
Adherence and persistence
Medication adherence was assessed using the medication possession ratio (MPR), defined as the sum of the days’ supply of study medication within one year after the index date divided by 365 days.Citation6,Citation7 Adherence to therapy was defined as an MPR ≥ 0.8. Medication persistence was defined as the number of days from the index date to the earliest of the ending date of the last prescription, the date of the first gap of more than 15 days between prescriptions, or the end of the study period of twelve months, whichever came first.Citation6,Citation7
Pretreatment variables
Pretreatment variables included demographic characteristics (age, gender, geographic region of residence, and health plan type), comorbidities, and prior use of medications. Comorbidities included 20 chronic pain conditions, sleep disorders, psychiatric disorders, and other physical disorders (see for detail) that are associated with safety, efficacy, or adherence of antidepressant treatment.Citation28,Citation31–Citation37 Prior use of medications included specified therapeutic classes, as well as selected individual drugs known to be used in treating depression, psychosis, bipolar disorders, anxiety, sleep disorders, or chronic pain that are known to be associated with physicians’ choice of antidepressants.Citation4,Citation33,Citation38,Citation39 All medications were identified on the basis of National Drug Codes.
Table 1 Comorbid conditions and ICD-9-CM diagnosis codes
Statistical analyses
Summary statistics were presented as means and standard deviations for continuous variables and as percentages for categorical variables. Demographic characteristics at the index date of study medication initiation, comorbid conditions, and medications used in the preindex period (one year prior to index date) were compared between the four medication cohorts. Chi-square tests were performed for comparisons of categorical variables and analysis of variance for comparisons of continuous variables. Kaplan–Meier survival curves were produced to show times to discontinuation of the four study medication cohorts.
Pairwise comparisons were conducted to examine the differences in adherence and persistence between the four study medication cohorts, adjusting for demographic variables, comorbid conditions, and prior medication use. The Tukey–Kramer method was used to adjust for multiple comparisons.
A multivariate stepwise logistic regression and Cox proportional hazards regression analyses were conducted to determine variables that independently predicted adherence and time to discontinuation (persistence) in the study, adjusting for all the variables in the model. Independent variables for the multivariate stepwise logistic regression included study medications, demographics, comorbid disorders, and concomitant medications in the pre-study period. Odds ratios (ORs) and 95% confidence intervals (CI) from the logistic regression model were used to examine the associations of predicting variables with adherence. The larger the odds ratio was, the higher the likelihood of adherence to the study medication. Hazard ratios (HRs) and 95% confidence intervals from the Cox proportional hazards model were used to examine associations of predicting variables with time to discontinuation of medication. The smaller the hazard ratio was, the less the likelihood of discontinuation of the medication.
Sensitivity analyses were conducted to compare group differences in adherence and persistence. First, adherence and persistence in the six months after initiation were computed. Second, persistence was estimated using an alternative allowable 30-day gap. Third, 17-ICD classes of systemic diseases as comorbid conditions were used instead of selected diseases for multivariate logistic and Cox proportional hazards regression modeling. All statistical analyses were performed using SAS (v 9.1; SAS institute, Inc, Cary, NC).
Results
A total of 44,026 patients with continuous enrollment in the health plan for twelve months prior to and post index date were included in the study. Demographic characteristics of the sample by medications are reported in . The sample was primarily female and had a mean age ranging from 43.7 to 47.2 years by medications (P < 0.0001). Within each medication cohort, approximately one-third of the sample was aged 46 to 55 years. Most of the sample had a Preferred Provider Organization (PPO) health plan which was highest in the DLX group (P < 0.0001), and more patients from each drug group lived in the South (P < 0.0001).
Table 2 Demographic characteristics of patients initiated on duloxetine, venlafaxine XR, escitalopram, or generic SSRIs
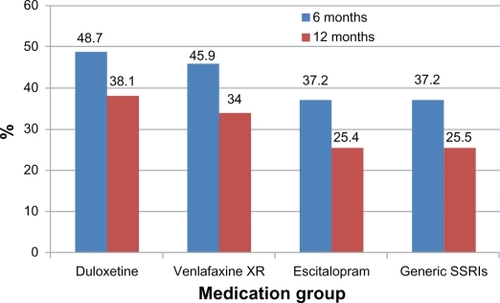
presents adherence to antidepressant therapy across four medications. In the six months after medication initiation, antidepressant adherence was highest for DLX (48.7%), followed by VLX (45.9%), and ECP and GSSRIs (37.2%). In the twelve months after medication initiation, adherence rate declined for all medication cohorts. DLX was still highest (38.1%) and ECP and GSSRIs were lowest (25.4% and 25.5%, respectively). Pairwise comparisons showed that DLX had a significantly higher adherence rate than the three comparators and that VLX had a significantly higher adherence rate than ECP and GSSRIs at six months and twelve months (all P < 0.01).
Figure 2 Antidepressant adherence (%) in patients with major depressive disorder in the six months and twelve months after medication initiation.
In the twelve months after medication initiation, average length of therapy (persistence) was 158.5 days (SD = 133.9, median = 95.0) with DLX; 149.6 days (SD = 129.9, median = 90.0) with VLX; 129.1 days (SD = 119.8, median = 90) with ECP; and 130.2 days (SD = 120.7, median = 90.0) with GSSRIs, respectively. Pairwise comparisons showed that the average persistence duration was significantly longer in DLX-treated patients compared to patients treated with VLX (P < 0.001), ECP (P < 0.001), or GSSRIs (P <0.001). Length of therapy was significantly longer in VLX-treated patients compared to patients treated with ECP (P < 0.001) or GSSRIs (P < 0.001). However, ECP and GSSRIs did not significantly differ in length of therapy (P > 0.05).
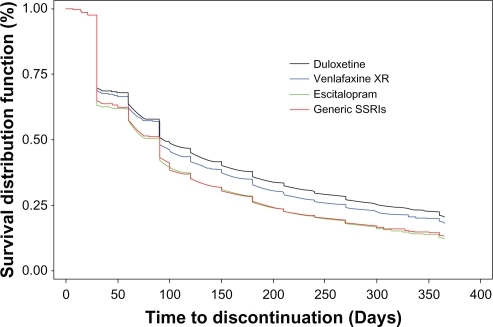
shows the Kaplan–Meier curves (time to discontinuation) of different antidepressant therapies in the twelve months after medication initiation. In the first 30 days, about 30% of patients discontinued their therapy across all treatment groups. After 30 days, DLX and VLX appeared to be different from ECP and GSSRIs and after 90 days, DLX was less likely to be discontinued than VLX. The median time to discontinuation was 95 days in DLX-treated patients, 90 days in VLX-treated patients, 90 days in ECP-treated patients, and 90 days in GSSRI-treated patients. Altogether, DLX-treated patients were less likely to discontinue than patients treated with VLX, ECP, or GSSRIs (P < 0.001).
Figure 3 Time to discontinuation with different antidepressant therapy in patients with major depressive disorder in the twelve months after medication initiation.
presents the multivariate stepwise logistic and Cox proportional hazards regression results for adherence and discontinuation with medication therapy, respectively. ORs and HRs were used to describe the strength of the associations between significant variables and adherence and discontinuation in the final model. Compared with GSSRIs, patients treated with DLX were more likely to be adherent (OR = 1.66, CI: 1.57–1.76), followed by VLX (OR = 1.43, CI: 1.34–1.52). The OR for ECP was 0.99, indicating ECP and GSSRIs were very similar in adherence after adjustment for demographics, comorbid conditions and prior use of medications. Also, patients were more likely to remain adherent if they were older (36 years and above), had comorbid hypersomnia, and had used medications including VLX, ECP, other antide-pressants, anticonvulsants, and antimigraine medications in the prior year (). However, patients were less likely to be adherent if they had comorbid chronic pain diseases (headaches, low back pain, and fibromyalgia), alcohol and drug dependence, and prior use of amphetamines, opioids, and muscle relaxants.
Table 3 Multivariate logistic regression and Cox proportional hazards regression: predictors of adherence or persistence with antidepressant therapy
As shown in , compared with GSSRIs, patients treated with DLX were less likely to discontinue medication therapy in the twelve months after initiation (HR = 0.81, CI: 0.78–0.83), followed by VLX (HR = 0.85, CI: 0.83–0.88). ECP was very similar in the likelihood of discontinuation to GSSRIs (HR = 1.02, CI: 1.00–1.05). Predictors associated with decreased likelihood of discontinuation with antide-pressant therapy included older age (36 years and above), hypersomnia, anxiety disorders, and prior use of VLX, ECP, other antidepressants, modafinil, anticonvulsants, and antimigraine medications. Factors associated with increased likelihood of discontinuation were chronic headaches, low back pain, alcohol and drug dependence, and prior use of benzodiazepines, amphetamine, and opioids.
In sensitivity analyses the group differences in adherence and persistence across the four medication cohorts had no essential changes 1) if patients were followed for six months, 2) if an alternative allowable 30-day gap was used to estimate persistence, and 3) if 17-ICD classes of systemic diseases were used to capture comorbid diseases instead of selected comorbid diseases. Similar predictors of adherence and discontinuation were also observed for 6-month and 12-month follow-ups and for an allowable 15-day and 30-day gap.
Discussion
This study examined adherence and persistence with three branded antidepressants (DLX, VLX, and ECP) and GSSRIs in usual clinical settings. Our results showed that the adherence rate was 46% for VLX, 49% for DLX, and 37% for ECP and GSSRIs in the six months after initiation and declined markedly in the second six months for all antide-pressants. Patients treated with DLX were more adherent to and stayed on medication longer than patients treated with VLX, ECP, or GSSRIs. VLX-treated patients had better adherence and longer persistence with therapy than patients treated with ECP or GSSRIs. However, ECP was similar to GSSRIs in adherence and persistence. In addition, multiple demographic and clinical pretreatment factors were associated with treatment adherence and persistence.
The adherence rate was 38.1% and 34.0% for DLX and VLX and approximately 25% for the SSRIs in the year after initiation. About 30% of patients discontinued their medication within 30 days. The American Psychiatric Association treatment guideline recommends at least four to eight weeks of treatment during the acute phase followed by 16 to 20 weeks of treatment following remission during the continuation phase.Citation40 The American College of Physicians guideline recommends treatment for four to nine months after a satisfactory response in patients with a first episode of MDD and an even longer duration of therapy for patients who have had two or more episodes of depression.Citation41 Given the consequence of early premature discontinuation and nonadherence,Citation10,Citation33 it is important to improve patient adherence to medication therapy and give long enough therapy to reduce relapse and hospitalization and costs.
SNRIs (DLX and VLX) have better adherence and longer persistence than SSRIs including ECP. Over the 1-year study period, the difference in adherence between SNRIs and SSRIs was 9% to 12% and the difference in length of therapy was 19 to 29 days. There are several possible explanations. First, there were differences in demographic and clinical characteristics of patients initiating SNRIs and SSRIs. SNRI-treated patients are more likely to be female, older, and were more complex (recurrent, with more severe and comorbid disorders) than SSRI-treated patients.Citation28 These patients may need longer therapy and better adherence. Second, SNRIs may have better effects than SSRIs for severe patients.Citation22,Citation23 Third, SNRIs are similar to SSRIs in safety profiles.
Compared with VLX, DLX appears to have better adherence and persistence. The advantage of DLX over VLX may share similar reasons to those for SNRIs over SSRIs and may be attributed to the differences in clinical and pharmacological profiles between the two SNRIs.Citation24,Citation25 DLX-treated patients are more complicated and have more comorbid conditions, especially chronic pain diseases, than VLX-treated patients.Citation28,Citation39 Compared to VLX, DLX is a relatively balanced SNRI, displaying high affinity for both serotonin and norepinephrine transporters.Citation24 In addition to MDD and anxiety, DLX has indications for fibromyalgia and DPNP and has shown efficacy for chronic low back pain.Citation42 However, the differences in adherence (4%) and persistence (nine days) were relatively small, though they were statistically significant. Further research needs to examine if the small differences could be translated into clinically and economically meaningful outcomes.
ECP is the only branded SSRI in the United States. Our results show that ECP has very similar adherence and persistence profiles compared to GSSRIs. This finding is not surprising because ECP is an SSRI and has similar clinical and pharmacological profiles compared to other SSRIsCitation43 and because ECP-treated patients are also very similar to GSSRI-treated patients in demographics and comorbid conditions.Citation28
Consistent with previous studies,Citation13–Citation18,Citation20,Citation21 this study found that multiple demographical and clinical factors were associated with adherence and persistence. For example, older patients were more likely to be adherent with antidepressant therapy. Eaddy and colleaguesCitation12 studied the association between SSRI utilization patterns and use of health care services and reported that patients who discontinued therapy in the first 90 days tended to be younger. Certain comorbid diseases can increase or decrease the odds of discontinuation of antidepressant therapy. Patients with chronic headaches, low back pain, and alcohol and drug dependence were more likely to discontinue therapy, while patients with hypersomnia were more likely to remain adherent. Also, the prior use of certain medications can affect adherence and persistence. Patients who have been prescribed VLX, ECP, anticonvulsants, and antimigraine medications have decreased odds of discontinuation, while patients with prior use of benzodiazepines, amphetamine, and opioids have increased odds of discontinuation. It would be warranted to investigate why certain comorbid disorders and medications are related to poor adherence and early discontinuation with antidepressant therapy.
Limitations
Several limitations must be considered in this retrospective study using a claims database. Claims database analyses have potential selection bias, miscoding of information and consequent biases in estimation. Also, adherence and persistence were estimated based on the presence of a claim for a filled prescription rather than real consumption of the medication as reported by patients or assessed by objective measures. Other limitations of this study include: the lack of detailed clinical data on the severity of depression, illness history, duration of current episode, and patient responses to antidepressants; and the lack of detailed social demographic data on education, ethnicity, employment status, income, and family environment; and the absence of information about physician and patient belief and preference. Demographic and clinical differences were observed between the cohorts of patients initiating SNRIs and SSRIs. While attempts were made to control for these baseline differences in measured variables through regression analysis, potential differences in the above unmeasured variables are unaccounted for – except in as much as they are correlated with measured variables. Prospective observational studies are needed to examine whether these findings can be generalized to the real-world clinical setting. In addition, although adherence and persistence were statistically different across study medications, further research is needed to examine whether the statistical differences can be translated into clinically and economically meaningful consequences.
Conclusion
The adherence rate was 34% to 38% for SNRIs and approximately 25% for SSRIs in the year after initiation. About 30% of patients discontinued their medication within 30 days. DLX and VLX treated patients had better adherence and longer length of therapy with the medication than patients treated with ECP or GSSRIs. While DLX treated patients had statistically significantly better adherence and persistence than VLX, the observed differences were relatively small and further research is needed to examine if these differences translate into clinically and economically meaningful outcomes. Adherence and persistence between ECP and GSSRIs were similar. In addition, multiple demographic and clinical factors are associated with adherence and persistence. Given the clinical and economic benefits of better adherence and persistence with antidepressant therapy, targeting interventions to patients who are at high risk for nonadherence and early discontinuation of therapy should be considered an important part of medication therapy for major depression.
Acknowledgements
The authors thank Dr Jarrett Coffindaffer and Ms Teri Tucker of i3 Statprobe for their assistance in preparing this manuscript. This study was funded by Eli Lilly and Company.
Disclosure
X Liu is a former employee, while Y Chen and D Faries are current employees of Eli Lilly and Company.
References
- KesslerRCChiuWTDemlerOMerikangasKRWaltersEEPrevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey ReplicationArch Gen Psychiatry20056261762715939839
- World Health OrganizationThe World Health Report 2004: Changing History, Annex Table 3: Burden of disease in DALYs by cause, sex, and mortality stratum in WHO regions, estimates for 2002World Health OrganizationGeneva, Switzerland2004
- GreenbergPEKesslerRCBirnbaumHGThe economic burden of depression in the United States: how did it change between 1990 and 2000?J Clin Psychiatry2003641465147514728109
- StaffordRSMacDonaldEAFinkelsteinSNNational Patterns of Medication Treatment for Depression, 1987 to 2001Prim Care Companion J Clin Psychiatry2001323223515014590
- CaleyCFKandoJCSSRI efficacy-finding the right doseJ Psychiatr Pract20028334015985852
- CantrellCREaddyMTShahMBReganTSSokolMCMethods for evaluating patient adherence to antidepressant therapy: a real-world comparison of adherence and economic outcomesMed Care20064430030316565629
- CramerJARoyABurrellAMedication compliance and persistence: terminology and definitionValue Health200811444718237359
- RuhéHGHuyserJSwinkelsJAScheneAHSwitching antidepressants after a first selective serotonin reuptake inhibitor in major depressive disorder: a systematic reviewJ Clin Psychiatry2006671836185517194261
- KhandkerRKKruzikasDTMcLaughlinTPPharmacy and medical costs associated with switching between venlafaxine and SSRI antidepressant therapy for the treatment of major depressive disorderJ Manag Care Pharm20081442644118597572
- MelfiCAChawlaAJCroghanTWHannaMPKennedySSredlKThe effects of adherence to antidepressant treatment guidelines on relapse and recurrence of depressionArch Gen Psychiatry199855112811329862557
- LinEHVon KorffMBushTSimonGEWalkerERobinsonPThe role of the primary care physician in patients’ adherence to antidepressant therapyMed Care19953367747823648
- EaddyMTDrussBGSarnesMWReganTSFrankumLERelationship of total health care charges to selective serotonin reuptake inhibitor utilization patterns including the length of antidepressant therapy: results from a managed care administrative claims databaseJ Manag Care Pharm20051114515015766321
- NantzELiu-SeifertHSkljarevskiVPredictors of premature discontinuation of treatment in multiple disease statesPatient Prefer Adherence20093314319936143
- BosworthHBVoilsCIPotterGGSteffensDCThe effects of anti-depressant medication adherence as well as psychosocial and clinical factors on depression outcome among older adultsInt J Geriatr Psychiatry2008312913417563920
- BullochAGPattenSBNon-adherence with psychotropic medications in the general populationSoc Psychiatry Psychiatr Epidemiol201045475619347238
- DemyttenaereKEnzlinPDeweWCompliance with antidepres-sants in a primary care setting, 2: the influence of gender and type of impairmentJ Clin Psychiatry200162Suppl 22S34S37
- DemyttenaereKBonnewynABruffaertsRClinical factors influencing the prescription of antidepressants and benzodiazepines: results from the European study of the epidemiology of mental disorders (ESEMeD)J Affect Disord2008110849318329721
- LinEHVon KorffMLudmanEJEnhancing adherence to prevent depression relapse in primary careGen Hosp Psychiatry20032530331012972220
- ClaxtonAJCramerJPierceCA systematic review of the associations between dose regimens and medication complianceClin Ther2001231296131011558866
- PompiliMSerafiniGDel CasaleAImproving adherence in mood disorders: the struggle against relapse, recurrence and suicide riskExpert Rev Neurother20099985100419589049
- WardenDTrivediMHWisniewskiSRPredictors of attrition during initial (citalopram) treatment for depression: a STAR*D reportAm J Psychiatry20071641189119717671281
- NelsonJCMazureCMJatlowPIBowersMBJrPriceLHCombining norepinephrine and serotonin reuptake inhibition mechanisms for treatment of depression: a double-blind, randomized studyBiol Psychiatry20045529630014744472
- PapakostasGIThaseMEFavaMNelsonJCSheltonRCAre antide-pressant drugs that combine serotonergic and noradrenergic mechanisms of action more effective than the selective serotonin reuptake inhibitors in treating major depressive disorder? A meta-analysis of studies of newer agentsBiol Psychiatry2007621217122717588546
- BeiqueJCLavoieNde MontignyCDebonnelGAffinities of venlafaxine and various reuptake inhibitors for the serotonin and nor-epinephrine transportersEur J Pharmacol19983491291329669506
- CiprianiAFurukawaTASalantiGComparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments meta-analysisLancet200937374675819185342
- BeiqueJCde MontignyCBlierPDebonnelGVenlafaxine: discrepancy between in vivo 5-HT and NE reuptake blockade and affinity for reuptake sitesSynapse19993219821110340630
- Duloxetine hydrochloridePrescribing informationIndianapolis, INLilly USA LLC2009
- LiuXCChenYFariesDMinerCSwindleRImpact of comorbidities on antidepressant initiation: duloxetine, venlafaxine, and escitalopram versus other SSRIs38th American College of Clinical Pharmacology Annual Meeting2009 Sept 13–15San Antonio, TX
- CrownWHFinkelsteinSBerndtERLingThe impact of treatment-resistant depression on health care utilization and costsJ Clin Psychiatry20026396397112444808
- MatzaLSRajagopalanKSThompsonCLde LissovoyGMisdiagnosed patients with bipolar disorder: comorbidities, treatment patterns, and direct treatment costsJ Clin Psychiatry2005661432144016420081
- IosifescuDVBankierBFavaMImpact of medical comorbid disease on antidepressant treatment of major depressive disorderCurr Psychiatry Rep2004619320115142472
- IosifescuDVClementi-CravenNFraguasRCardiovascular risk factors may moderate pharmacological treatment effects in major depressive disorderPsychosom Med20056770370616204427
- LiuXCYeWWatsonPTepperPUse of benzodiazepines, hypnotics, and anxiolytics in major depressive disorder: association with chronic pain diseasesJ Nerv Ment Dis201019854455020699718
- OngJCGressJLSan Pedro-SalcedoMGManberRFrequency and predictors of obstructive sleep apnea among individuals with major depressive disorder and insomniaJ Psychosom Res20096713514119616140
- SheltonCFactors impacting the selection of antidepressant treatment in patients with major depressive disorder at risk for nonadherenceCNS Spectr200914151920397587
- VaccarinoALSillsTLEvansKRKalaliAHMultiple pain complaints in patients with major depressive disorderPsychosom Med20097115916219073755
- WuEQGreenbergPEYangEYuAPBen-HamadiRErderMHTreatment persistence, healthcare utilisation and costs in adult patients with major depressive disorder: a comparison between escitalopram and other SSRI/SNRIsJ Med Econ20091212413519566483
- KroenkeKKrebsEEBairMJPharmacotherapy of chronic pain: a synthesis of recommendations from systematic reviewsGen Hosp Psychiatry20093120621919410099
- YeWYZhaoYRobinsonRSwindleRPredictors of treatment initiation with duloxetine compared with venlafaxine XR among patients with major depressive disorder in US managed-care setting13th International Meeting of the International Society for Pharmacoeconomics and Outcomes Research2008 May 3–7Toronto, ON
- KarasuTBGelenbergAMerriamAEWangPAmerican Psychiatric Association practice guideline for the treatment of patients with major depressive disorderAm J Psychiatry2000157145
- QaseemASnowVDenbergTDForcieaMAOwensDKUsing second-generation antidepressants to treat depressive disorders: a clinical practice guideline from the American College of PhysiciansAnn Intern Med200814972573319017591
- SkljarevskiVZhangSChappellASWalkerDJMurrayIBackonjaMMaintenance of effect of duloxetine in patients with chronic low back pain: a 41-week uncontrolled, dose-blinded studyPain Med20101164865720546509
- GartlehnerGGaynesBNHansenRAComparative benefits and harms of second-generation antidepressants: background paper for the American College of PhysiciansAnn Intern Med200814973475019017592