Abstract
Background
Grass pollen-induced allergic rhinoconjunctivitis constitutes a large burden for society. Up to 20% of European and United States (US) populations suffer from respiratory allergies, including grass pollen-induced allergic rhinoconjunctivitis. The majority of patients are treated with symptomatic medications; however, a large proportion remains uncontrolled despite use of such treatments. Specific immunotherapy is the only treatment documented to target the underlying cause of the disease, leading to a sustained effect after completion of treatment. The aim of this study was to compare the economic consequences of treating patients suffering from allergic rhinoconjunctivitis with either a grass allergy immunotherapy tablet (AIT) or subcutaneous immunotherapy (SCIT).
Methods
A budget impact analysis was applied comparing SQ-standardized grass AIT (Grazax®; Phleum pratense, 75,000 SQ-T/2,800 BAU; ALK, Denmark) with SCIT (Alutard®; P. pratense, 100,000 SQ-U/mL; ALK, Denmark). Budget impact analysis included health care utilization measured in physical units based on systematic literature reviews, guidelines, and expert opinions, as well as valuation in unit costs based on drug tariffs, physician fees, and wage statistics. Budget impact analysis was conducted from a Danish health care perspective.
Results
Treating patients suffering from allergic rhinoconjunctivitis with grass AIT instead of grass SCIT resulted in a total reduction in treatment costs of €1291 per patient during a treatment course. This cost saving implies that approximately 40% more patients could be treated with grass AIT per year without influencing the cost of treatment.
Conclusion
Budget impact analysis showed that grass AIT is a cost-saving alternative to SCIT when treating patients with grass pollen-induced allergic rhinoconjunctivitis.
Introduction
Allergic rhinoconjunctivitis is a common allergic respiratory disorder caused by allergens such as grass or tree pollens and house dust mites. The prevalence of allergic rhinoconjunctivitis is increasing and is a major health issue worldwide. In Europe and the US, up to 20% of the adult population suffers from this condition.Citation1–Citation4 Allergic rhinoconjunctivitis is associated with symptoms such as a runny, blocked and/or itchy nose, sneezing, a gritty feeling in the eyes, and red/itchy/watery eyes, has a considerable impact on quality of life, and indirect costs arising from absenteeism from work and school, impaired sleep quality, and decreased productivity.Citation5–Citation9 Furthermore, allergic rhinoconjunctivitis is an independent risk factor for asthma or sinusitis.Citation5 This increases the societal and economic impact of allergic rhinoconjunctivitis.
Treatment strategies for allergic rhinoconjunctivitis are largely symptomatic, and include oral antihistamines, nasal corticosteroids, and eye drops.Citation10 However, the underlying allergic disease remains unaffected and symptomatic treatment offers only short-term relief.
Allergen-specific immunotherapy is the only treatment capable of activating immunomodulatory mechanisms and modifying the underlying course of the disease, thereby providing sustained relief of symptoms.Citation11 Allergen-specific immunotherapy can be administered in different formulations, such as subcutaneous immunotherapy (SCIT) and allergy immunotherapy tablets (AIT).
SCIT has been widely used throughout Europe for decades. Treatment is initiated by a uptitration phase, during which the patient is given subcutaneous injections with increasing doses of allergen over a period of several weeks. This is followed by a maintenance phase during which the patient is given the maximum tolerated dose of allergen with each injection. More recently, AIT, a new and convenient form of immunotherapy, has been approved and marketed. AIT can be self-administered at home without uptitration.
The magnitude of and similarity in efficacy between these two treatment concepts has been and is still widely discussed. SCIT is documented to be efficacious and well tolerated in patients with grass pollen-induced allergic rhinoconjunctivitis. Citation12 Sustained effectiveness of SCIT has also been demonstrated.Citation13 Several trials have likewise confirmed the benefits of AIT treatment, with sustained efficacy and a favorable safety profile in patients with grass pollen-induced allergic rhinoconjunctivitis.Citation14–Citation21
Direct comparisons between SCIT and AIT in clinical trials are still lacking, mainly because of the use of different treatment regimens and thereby difficulties in designing proper and ethical head-to-head comparisons. However, the efficacy of grass AIT and grass SCIT has recently been compared in a meta-analysis,Citation22 which concluded that the clinical effect of grass AIT is similar in magnitude to that observed for SCIT in patients with grass pollen-induced allergic rhinoconjunctivitis of the same severity.
The international economic crisis has led to an increased demand for evaluations of potential cost savings to health care systems without impacting the quality and safety of treatment, and budget impact analyses showing the economic consequences of different treatments may be highly relevant or even warranted for health care decision-makers. This study compared the economic consequences of treating patients with grass pollen-induced allergic rhinoconjunctivitis using either grass AIT or grass SCIT.
Materials and methods
Health economic analysis
A model was constructed to compare the budget impact of two standard immunotherapy treatments, ie, SQ-standardized grass AIT (Grazax®; Phleum pratense, 75,000 SQ-T/2,800 BAU; ALK, Denmark) and grass SCIT (Alutard; P. pratense, 100,000 SQ-U; ALK, Denmark). The model was developed based on clinical dataCitation21 and a recently published meta-analysis, Citation22 and all calculations were performed using Microsoft Office Excel 2007 (Microsoft, Redmond, WA).
The methodology for developing the budget impact analysis followed international health economic guidelines for budget impact analyses.Citation23 According to these guidelines, a budget impact analysis should define scenarios relevant to health care decision-makers, the perspective should be that of the budget-holder, and the outcome of the analysis should reflect scenarios of interest to the decision-maker rather than assumptions intended to be generally applicable. Therefore, our budget impact analysis included calculation of all marginal costs from a Danish health care perspective to estimate possible annual savings to health care budgets resulting from implementation of grass AIT instead of grass SCIT. The analysis also included patient and societal costs, and reported these costs separately.
General model assumptions
The economic evaluation was conducted from a Danish health care perspective and included allergy treatment for adults in both the primary and secondary sector in Denmark. The analysis included direct treatment costs (cost of medication and physician visits), direct patient costs (travel expenses), and indirect patient costs (time lost). In accordance with Danish guidelines,Citation24 a discount rate of 3% per year was applied to account for treatment duration of 3–5 years. General model assumptions are outlined in .
Table 1 General model assumptions
Resource use
Resources in terms of medication use, physician visits, and patient time were calculated and are outlined in . Health care utilization was calculated based on data collected from a review of clinical trials and standard treatment in Denmark (according to the Summary of Product Characteristics), and where data were limited, these were validated by medical experts. Expert validation was obtained from two structured workshops with Danish physicians. The wide variability in the participating physicians’ specialties is considered to contribute to the robustness of the analysis.
Table 2 Resource use (health care utilization)
Costs
Cost estimates are outlined in . Unit costs were obtained from established Danish public sources, including the Danish federal statistical office (Statistics Denmark), fees for service remuneration, and product list prices.Citation25–Citation29 All costs are reported in 2010 prices except when otherwise stated. Costs were obtained in Danish kroner and exchanged to Euro using the average 2010 exchange rate (1 Euro = 7.447366 DKK).
Table 3 Cost input (in €)
Sensitivity analysis
The robustness of the budget impact analysis was investigated using a one-way sensitivity analysis. The most sensitive resource costs were systematically calculated to investigate the sensitivity of the overall result. The sensitivity analysis was based on direct treatment costs.
Results
Treatment-related costs
The result of the budget impact analysis is shown in . Direct treatment costs for treatment with grass SCIT were estimated to be €4555 per patient for a treatment course. In comparison, the direct treatment costs for treatment with grass AIT were estimated to be €3264 per patient for a treatment course, representing a cost saving of €1291 per patient. Estimated direct and indirect patients costs were €2694 for treatment with grass SCIT and €525 for treatment with grass AIT, representing a cost saving in total patient costs of €2169. Total savings (treatment costs and patient costs) amounted to €3460. This corresponds to a decrease of 28% in direct treatment costs, a decrease of 81% in direct and indirect patient costs, and a decrease in total costs of 48%, if treatment with grass AIT is used instead of grass SCIT ().
Figure 1 Decrease in direct treatment costs, patients costs and total costs in relation to treatment with grass AIT as compared with grass SCIT.
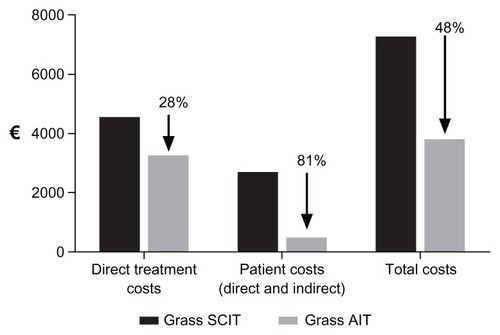
Table 4 Costs (in €) in relation to treatment with grass AIT and grass SCIT
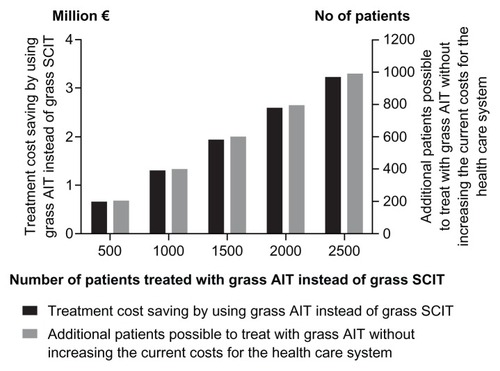
The cost savings gained by prescribing grass AIT instead of grass SCIT may be utilized to treat more patients with immunotherapy. In , the relationship is shown between the number of subjects treated with grass AIT instead of grass SCIT, cost savings when using grass AIT instead of grass SCIT, and the number of new patients who could possibly be started on grass AIT without any additional cost as compared with the current costs for grass SCIT. As shown, it is possible to treat a substantial number of new patients on grass AIT without any additional cost to the health care system. For example, if 1500 subjects were treated with grass AIT instead of grass SCIT, it would be possible to treat approximately 600 more patients per year without increasing the current costs to the health care system. This corresponds to an increase in the number of treated patients of approximately 40%.
Sensitivity analysis
The results of the one-way sensitivity analysis are shown in . The basic treatment cost saving was €1291. Resource costs were varied in both directions and, regardless of variation/adjustment, all costs were in favor of grass AIT with incremental costs for grass SCIT. Notably, variations between the general practice and hospital settings resulted in major changes in direct treatment costs, whereas the discount rate and duration of treatment had no or at least less impact on the analysis.
Table 5 One-way sensitivity analysis (direct treatment costs, in €)
Discussion
A budget impact analysis compares the costs of different treatment options seen from a health care decision-maker perspective. Therefore, the focus of this budget impact analysis was to compare the economic consequences of treating patients with grass pollen-induced allergic rhinitis using either grass AIT or grass SCIT.
The analysis showed that overall direct treatment costs as well as patient costs were lower for treatment with grass AIT than for treatment with grass SCIT. The main cost difference between the two treatments was the result of fewer physician visits being needed for grass AIT as compared with grass SCIT. The cost of medication per patient was higher for grass AIT as compared with grass SCIT, whereas the costs of physician visits, travel expenses, and lost working hours were considerably lower for grass AIT. The overall impact was reduced costs for the health care system and society (reduced physician visits and resources) as well as for individual patients (reduced travel expenses and less lost working hours). The robustness of these results was confirmed by the one-way sensitivity analysis.
The total treatment cost saving to the health care system amounted to €1291 per patient per treatment course when using grass AIT instead of grass SCIT. In 2010, approximately 1200 patients were initiated on grass SCIT treatment in Denmark (data on file). Assuming a similar continuous number of patients initiating immunotherapy treatment per year in the future, the implication for Danish society will be a treatment cost saving of more than €1,500,000 on a yearly basis if grass AIT is used as treatment instead of grass SCIT. Cost saving in this range implies that more than 450 additional patients per year could be treated with grass AIT without influencing costs. An increase in the number of patients treated per year may have additional beneficial outcomes for the health care system both in terms of additional cost savings as well as in terms of improved health status for patients. Allergic rhinitis is an independent risk factor for development of asthma.Citation5 Because asthma is a disease with considerable burden and substantial costs to both the public and private health care systems,Citation30 the potential cost savings to the health care system may be even more pronounced if patients with grass pollen-induced allergic rhinitis are treated with grass immunotherapy. In addition, having more patients on immunotherapy may decrease the use of other kinds of medication used for treatment of allergic rhinitis and/or asthma, thereby decreasing costs to the health care system in relation to these medications. Grass AIT also has a number of other advantages which may be beneficial for the health care system, but which are not included in the budget impact analysis per se.
Grass AIT is generally considered to have a significantly lower risk profile than SCIT.Citation31,Citation32 The potentially lower costs for treatment of adverse events resulting from AIT are not considered in this analysis. The main cost related to side effects and seen from a health care decision-maker perspective is for hospitalization. Hospital admissions due to side effects of immunotherapy are considered to be uncommon but, because no firm documentation on the extent of these admissions is available, they have not been addressed in this study.
Treatment with grass AIT is also simpler and more convenient than for grass SCIT because tablets can be administered at home instead of injections at a clinic. Home administration will, as mentioned above, result in fewer physician visits as compared with grass SCIT, and thereby lead to cost savings to the health care system. However, home administration is often perceived to be related to lower compliance than that achieved when treatment is given in a specialist office, leading to lower efficacy of treatment. However, a recent study evaluating compliance with grass AIT and grass SCIT indicated that compliance with both treatments was high and comparable (≥80%).Citation33
Grass AIT has also been shown to have a sustained and disease-modifying effect.Citation14,Citation21 This may lead to additional cost savings for both the individual patient and for society as a whole in terms of improved quality of life and lower costs related to absenteeism from work and decreased productivity.
Because several of the aforementioned factors are not included in the budget impact analysis due to limited data, a more comprehensive economic evaluation may be warranted to evaluate the overall health economic consequences of using grass AIT instead of grass SCIT. Further evaluation may include a cost-utility analysis to obtain data on quality of life for patients and a cost-benefit analysis to obtain data on willingness to pay.
Conclusion
In conclusion, this budget impact analysis shows that grass AIT is a cost-saving alternative to grass SCIT when treating patients with grass pollen-induced allergic rhinitis. Seen from a health care perspective, grass AIT represents an efficient use of cost and resources. Further analyses may be warranted to evaluate the overall health economic consequences of implementation of grass AIT instead of grass SCIT.
Disclosure
This health economic evaluation was funded by ALK, Denmark. SMR, UGS, JSM, LY, and LE have received grants from ALK. JNA is employed at ALK. The authors thank Anne Okkels Birk, who provided medical writing, editorial, and journal submission assistance on behalf of ALK.
References
- BauchauVDurhamSRPrevalence and rate of diagnosis of allergic rhinitis in EuropeEur Respir J20042475876415516669
- DahlRAndersenPChivatoTValovirtaEde MonchyJNational prevalence of respiratory allergic disordersRespir Med20049839840315139568
- WeissKBSullivanSDThe health economics of asthma and rhinitis. I. Assessing the economic impactJ Allergy Clin Immunol20011073811149982
- SchatzMA survey of the burden of allergic rhinitis in the USAAllergy200762 Suppl 8591617927673
- NathanRAThe burden of allergic rhinitisAllergy Asthma Proc2007283917390749
- WalkerSKhan-WastiSFletcherMCullinanPHarrisJSheikhASeasonal allergic rhinitis is associated with a detrimental effect on examination performance in United Kingdom teenagers: case-control studyJ Allergy Clin Immunol200712038138717560637
- VuurmanEFvan VeggelLMUiterwijkMMLeutnerDO’HanlonJFSeasonal allergic rhinitis and antihistamine effects on children’s learningAnn Allergy1993711211268346863
- SundbergRTorenKHoglundDAbergNBrismanJNasal symptoms are associated with school performance in adolescentsJ Adolesc Health20074058158317531771
- BousquetJKhaltaevNCruzAAAllergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen)Allergy200863 Suppl 86816018331513
- PlautMValentineMDClinical practice. Allergic rhinitisN Engl J Med20053531934194416267324
- European Medicines AgencyGuideline on the clinical development on products for specific immunotherapy for the treatment of allergic diseases2008 CHMP/EWP/18504/2006
- FrewAJPowellRJCorriganCJDurhamSREfficacy and safety of specific immunotherapy with SQ allergen extract in treatment-resistant seasonal allergic rhinoconjunctivitisJ Allergy Clin Immunol200611731932516461133
- DurhamSRWalkerSMVargaEMLong-term clinical efficacy of grass-pollen immunotherapyN Engl J Med199934146847510441602
- DurhamSEmmingerWKappADisease-modifying effect of the SQ-standardised grass allergy immunotherapy tablet is sustained 2 years after treatmentAllergy201065689690
- DahlRStenderARakSSpecific immunotherapy with SQ standardized grass allergen tablets in asthmatics with rhinoconjunctivitisAllergy20066118519016409194
- DahlRKappAColomboGEfficacy and safety of sublingual immunotherapy with grass allergen tablet for seasonal allergic rhinoconjunctivitisJ Allergy Clin Immunol200611843444016890769
- DahlRKappAColomboGSublingual grass allergen tablet immunotherapy provides sustained clinical benefit with progressive immunologic changes over 2 yearsJ Allergy Clin Immunol200812151251818155284
- FrølundLDurhamSRCalderonMSustained effect of SQ-standardized grass allergy immunotherapy tablet on rhinoconjunctivitis quality of lifeAllergy20106575375719886920
- NelsonHSNolteHCreticosPMaloneyJWuJBernsteinDIEfficacy and safety of timothy grass allergy immunotherapy tablet treatment in North American adultsJ Allergy Clin Immunol2011127728021211643
- BlaissMMaloneyJNolteHGawchikSYaoRSkonerDPEfficacy and safety of Timothy grass allergy immunotherapy tablets in North American children and adolescentsJ Allergy Clin Immunol2011127647121211642
- DurhamSREmmingerWKappALong-term clinical efficacy in grass pollen-induced rhinoconjunctivitis after treatment with SQ-standardized grass allergy immunotherapy tabletJ Allergy Clin Immunol201012513113820109743
- CalderonMAndersenJSLawtonSMeta-analysis supports that the efficacy of grass allergy immunotherapy tablets is comparable to subcutaneous immunotherapyAllergy2011Suppl 94652653
- MauskopfJASullivanSDAnnemansLPrinciples of good practice for budget impact analysis: report of the ISPOR Task Force on good research practices – budget impact analysisValue Health20071033634717888098
- Danish Medicines and Health AuthorityErfaringer med sundhedsøkonomiske analyser i ansøgninger om generelt tilskud til lægemidler2004 [Danish Medicines and Health Authority. Experiences with health economic analyses in drug reimbursement applications. 2004.]. Available from: http://laegemiddelstyrelsen.dk/da/topics/statistik,-priser-og-tilskud/tilskud-til-medicin/generelletilskud/ansoegning/sundhedsoekonomiske-analyser/erfaringer-medsundhedsoekonomiske-analy-aegemidlerAccessed July 15, 2012 Danish
- Danish Tax and Customs AdministrationSkattesatser 2009–2012 [Tax rates 2009-2012.]. Available from: http://skat.dk/SKAT.aspx?oId=2035568&vId=0&prev=2010&tab=Accessed July 15, 2012 Danish
- Statistics DenmarkEarnings Available from: http://iisboy4.dst.dk/statbank5a/SelectTable/omrade0.asp?Subjectcode=17&PLanguage=1&Shownews=OFF&tree=falseAccessed July 15, 2012
- National Board of Health DenmarkTakstsystem 2010 Vejledning (DAGS fees) [System of charges 2010 instruction (DAGS fees).]. Available from: http://www.sst.dk/publ/Publ2010/SESE/Takst/Takstvejledning_%202010.pdfAccessed July 15, 2012 Danish
- Danish Medical Association§56 Ydelser i dagtiden (wage and fees) [§56 Day time payments (wage and fees).]. Available from: http://www.laeger.dk/portal/page/portal/LAEGERDK/Laegerdk/P_L_O/Overenskomster/Honorartabel/Honorartabel%201-204-12/%C2%A7%2056%20Ydelser%20i%20dagtiden1Accessed July 15, 2012 Danish
- Danish Medicines and Health AuthorityList of medicine prices Available from: http://www.medicinpriser.dk/; http://laegemiddelstyrelsen.dk/da/topics/statistik,-priser-og-tilskud/priser-paa-medicin/prisudvikling/priser-de-seneste-5-aarAccessed July 15, 2012
- GINA Executive CommitteeGlobal Initiative for Asthma; Global Strategy for Asthma Management and Prevention, 2009Bethesda, MDNational Heart, Lung and Blood Institute, National Institute of Health2009
- RadulovicSCalderonMAWilsonDDurhamSSublingual immunotherapy for allergic rhinitisCochrane Database Syst Rev201012CD00289321154351
- PassalacquaGCompalatiECanonicaGWSublingual immunotherapy for allergic rhinitis: an updateCurr Opin Otolaryngol Head Neck Surg201119434721102336
- AndreasenJNLawtonSBæchSBSvärdMCompliance and persistence to grass immunotherapy treatment is comparable for allergy immunotherapy tablets and subcutaneous immunotherapy: a Swedish registry studyAbstract presented at World Allergy CongressDecember 4–8, 2011Cancun, Mexico