Abstract
Objective
Up to one in four patients living with epilepsy (PwE) mentions financial constraints as a reason for loss to follow-up at the Ndera tertiary neuropsychiatry hospital. Therefore, we evaluated the annual direct medical cost (DMC) and direct non-medical cost (DnMC) of epilepsy and calculated costs assuming different follow-up frequency.
Materials and Methods
DMC data were obtained from a descriptive retrospective study of medical records, pharmacy dispensation and hospital logs of PwE, following their initial consultation in 2018 and who adhered to the normal clinical practice of monthly consultations for one year. DnMC data were collected through structured interviews of PwE in a cross-sectional cohort in August 2020. DnMC included biomedical care costs (eg, transportation, hospitality) and non-biomedical costs (traditional healer visits). We report weighted means for total costs, health insurance costs, and out-of-pocket costs (OoP).
Results
Mean annual total cost was 389.4 US$, of which 226.2 US$ was covered by the Rwandan Health Insurance co-payment for DMC and 163.2 US$ was OoP paid by patients. Mean weighted annual DMC (n = 55) was 248.9 US$. Mean weighted annual DMC for medical consultations and antiseizure medication accounted for 30.7 US$ and 161.7 US$, respectively. Based on structured interviews (n = 69), mean weighted annual DnMC for biomedical care was 73.0 US$. Mean DnMC for traditional healer care was 67.6 US$. Weighted annual total OoP was 163.2 US$ or 20% of the GDP per capita. OoP consisted of 14% DMC co-payment, 45% biomedical DnMC, and 41% traditional healer DnMC.
Conclusion
Epilepsy-related costs at a tertiary center are an important economic burden for PwE and Rwandan Health Insurance. Biomedical and traditional healer DnMC constitute 86% of total OoP. Future prospective studies should evaluate outcomes and costs of reduced visit frequency, indirect costs, and costs of comorbidities.
Introduction
Epilepsy is a chronic neurological disorder that results in a substantial disease burden on patients, their families, and society.Citation1,Citation2 Of the estimated 70 million people living with epilepsy (PwE) globally, 80% live in low and middle income countries.Citation2–4 The condition affects people of all ages, gender, race and economic classes across the world.Citation5 The prevalence of epilepsy in Rwanda was estimated at 49 per 1000 people in 2005 and confirmed in a door-to-door survey in 2018.Citation6,Citation7
PwE need long-term follow-up through regular visits. In Rwanda, patients are requested to adhere to a standard clinical practice of monthly outpatient clinic visits. The dispensation of anti-seizure medication (ASM) is also monthly. PwE have access to epilepsy care in primary healthcare centers, secondary district/province hospitals or tertiary referral centers. The tertiary CARAES neuropsychiatric hospital at Ndera (Kigali, Rwanda) is one of the referral centers for mental health, including epilepsy.Citation8
In 2018, up to 33% of PwE who attended the CARAES neurology outpatient clinic for the first time were lost to follow-up after 19 months. Of those, more than one in four cited financial reasons as the cause for discontinuation.Citation9 There was a clear need to better understand the impact of direct medical costs (DMC) and direct non-medical costs (DnMC) for PwE attending the center.
Cost-of-illness (CoI) studies provide data on the economic burden and may become important as they may enhance public health decision-making.Citation10 Only a limited number of studies are available in low- and middle-income countries on the patients’ burden of the cost of epilepsy.Citation11–16
In Rwanda, community-based health insurance (CBHI) provides partial co-payment for DMC. An annual subscription fee of minimum 3.6 US$ per family member is due, defined by income and economic class.Citation17,Citation18 Depending on patient income, the CBHI reduces Out of Pocket (OoP) cost of DMC between 85–100% for outpatient consultations, technical investigations, and anti-seizure medication (ASM).Citation19,Citation20
In addition to DMC, DnMC related to biomedical care for transportation, accommodation, hospitality and eventual psychological therapy, and physiotherapy are not covered by the CBIH. Lastly, a substantial amount of PwE seek additional non-biomedical care such as spa treatment or traditional healer care, which increases DnMC and patient OoP.Citation21,Citation22 In Rwanda, seeking care from traditional healers varies from 6.4% to 26%.Citation6,Citation7,Citation9
Overall, OoP costs for general and specialized healthcare can be substantial and often prohibitive for persons living in a low-income setting.Citation20,Citation21 In this first-of-its-kind study in Rwandan PwE, we determined epilepsy-specific DMC, biomedical DnMC, and traditional healer DnMC of PwE attending the outpatient neurology clinic at the CARAES neuropsychiatric hospital.
Materials and Methods
Study Setting and Design
The study was performed at the outpatient neurology department of the tertiary referral center at the CARAES neuropsychiatric hospital at Ndera (Kigali, Rwanda). Approval was obtained from CARAES Ndera Ethics Committee (012/CNEC/2020).
To calculate DMC, we conducted a retrospective review of medical records, pharmacy dispensation and hospitalization logs of all PwE newly presenting at the center between January 1st and December 31st, 2018. PwE were included when i) they were aged 18 years or older; ii) they attended all monthly follow-up consultations during one year; and, iii) they had no other comorbidities or other medical conditions. Data from a 12-month period following their first visit were included and considered as the baseline data.
To calculate DnMC we identified a prospective convenience cohort of PwE attending their monthly outpatient consultation in August 2020. Structured interviews were completed to estimate biomedical and traditional healer DnMC. PwE were enrolled when i) they were 18 years of age or older; and, ii) had provided informed consent. Data collected included but were not limited to i) residence of patients; ii) cost of round-trip transportation; iii) cost of food and beverage; iv) cost of eventual accommodation; v) time spent at the hospital including waiting time, time for consultation and technical or laboratory investigations; vi) time spent on travel; and, vii) frequency and cost of use of non-biomedical care, eg, traditional healers, over the past year.
Demographics and Epilepsy Characteristics
Seizure-onset, epilepsy-type and seizure-frequency were extracted from the hospital’s electronic and/or paper medical records. Seizure onset and type were categorized according to the 2017 International League Against Epilepsy classification.Citation23,Citation24
Cost Evaluation
DMC and DnMC by cost variable and eventual co-payment between CBHI and PwE are shown in . Mean and median DMC and DnMC were calculated based on observed values. Subsequently, we corrected to a weighted mean and median for each variable. Total weighted average was calculated as the sum of weighted variables. A mid-year 2019 exchange rate of 884 Rwandan Franc (RwF) to one US$ was applied.
Table 1 Co-Payment Structure for DMC and DnMC for PwE in Rwanda
For patients exempt from a co-payment according to their insurance plan, the respective OoP was set to 0US$.
DMC
Epilepsy-specific annual DMC calculated based on the total cost during 12-month observation period, resulting from consultations, hospitalization, technical and laboratory investigations, administrative actions (eg, opening of medical file cost, medication bags, medical certificates etc.) and dispensed ASM. ASM costs were calculated based on the hospital pharmacy dispensing cost of the branded substance. The outpatient consultation fee in the center was calculated according to the type of physician that had been attending (psychiatrist, neurologist, or general practitioner with experience in epilepsy supervised by neurologist). The cost of each variable was provided by the hospital accounting department in RwF.
Costs covered by the CBHI and OoP DMC were calculated using the applicable reimbursement rate according to the health insurance status of the PwE.
Biomedical and Traditional Healer DnMC
DnMC were calculated using patient reported costs during structured interviews using a predefined questionnaire. If the patient reported data related to a single visit, the data were extrapolated to the number of visits over a one-year period for both medical and traditional healer care.
We did not include costs associated with physiotherapy, psychological and social counseling due to lack of consistent data availability, although these are considered as DnMC.Citation25
In-kind payments of traditional healer care were adjusted to 2019 values from historical prices.
Indirect Costs
Our study was not designed to measure indirect costs. We collected data on mode and time of transportation and time spent in the hospital, to better understand the burden of monthly follow-up visits. This amount was not monetized. The distance in kilometers (Km) from the village center to the CARAES Ndera hospital was calculated using Google Maps.
DMC, DnMC and OoP Change by Varying Visit Frequency
We evaluated the impact reduced frequency follow-up visits would have on DMC, DnMC and OoP with scenario A once every two months and scenario B once every three months. As higher costs in the first year of follow-up due to diagnostic work-up may be assumed, we conservatively analyzed costs after the first year with reduced healthcare utilization.Citation21,Citation26 As fewer diagnostic interventions and better seizure control can be obtained after the first year, we reduced technical investigations, laboratory investigations and administrative costs by 95% and reduced hospitalizations by 50%.Citation21 We kept traditional healer DnMC stable for each scenario, this resulted in changes of DMC and biomedical DnMC and eventual OoP. Total OoP costs were compared between the current observed values, scenario A and B and put into perspective with the total 2019 Rwandan GDP per capita.Citation27 This was a single exploratory analysis, and no formal pharmaco-economic model was built.
Data Analysis
Data were processed in Microsoft Excel following a double data entry process. Statistical analyses were performed using Excel and SPSS for Fisher Exact test, differences of the mean and Chi-square. Costs were presented as mean ± standard deviation (SD) US$, median US$ (minimum, maximum). Categorical variables were presented by proportion.
Results
Patient Samples
In August 2020, records of 175 PwE newly presenting in 2018 were identified and 55 (31.4%) records qualified for retrospective chart review. Structured interviews to assess DnMC were conducted with 69 PwE in August 2020.
Socio-Demographic Characteristics and Epilepsy Characteristics
Socio-demographic data and epilepsy characteristics are summarized in . The two samples proved very similar in composition including age group distribution. Differences were observed for mean age, age at first seizure and geographical composition with more PwE coming from city of Kigali in the interviewed group. Seizure-onset, seizure type and abnormalities of EEG results were comparable between groups, with tonic-clonic seizures being the most frequently reported seizure type. Nearly 85% of PwE reported no seizures in the past month.
Table 2 Socio-Demographic and Epilepsy Characteristics
Cost Evaluation
Total Costs
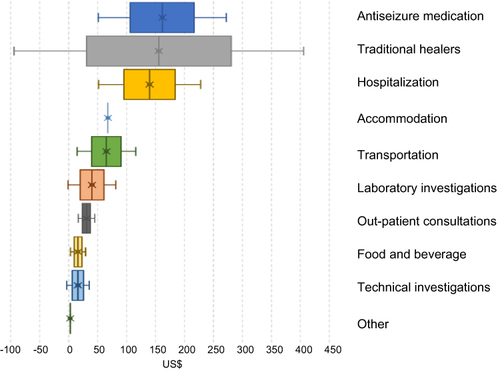
Weighted mean total, health insurance and OoP DMC were 389.4, 226.2 and 163.2 US$, respectively (). Univariate analysis identified ASM and hospitalization costs as the most important factors in DMC ().
Table 3 Annual DMC and DnMC, Unweighted and Weighted Mean and Relative Proportion of Each Cost Variable (in US$)
DMC
A total of 682 medical consultations were completed, averaging 12.4 consultations per PwE per year. Technical investigations in 43 PwE included 55 electroencephalograms (EEG), five computed tomography scans and one electrocardiogram. Laboratory investigations were performed in 46 PwE. ASM was prescribed as monotherapy to 22 PwE (40%) and as polytherapy to 33 PwE (60%). Three PwE were hospitalized during the retrospective observational period.
The observed, unweighted total mean annual DMC per PwE was 248.8 ± 142.7 US$ () with an annual median cost of 217.8 US$ (Supplementary Table 1). The unweighted OoP DMC per PwE was 27.0 ± 19.1 US$ with a median of 21.5 US$.
DnMC Biomedical Care
Over 12 months, PwE spent 76.3 ± 56.1 US$ (unweighted) on food, beverage, transportation, and accommodation (). The mean annual transportation cost for PwE from Kigali (n=40) was 50.0 US$ vs 121.4 US$ for PwE from the provinces (n=29). One patient needed accommodation to enable monthly visits.
Weighted mean and median biomedical OoP DnMC, were 73.0 and 61.2 US$ respectively (Supplementary Table 2), which constituted up to 45% of total DnMC OoP for PwE.
DnMC Traditional Healer Care
In total, 37/69 (53.6%) PwE, of whom 21 (56.8%) were male, sought traditional healer care on their own initiative, with 21/37 (56.8%) living in Kigali and 16/37 (43.2%) in the provinces. Thirty PwE reported a financial or in-kind contribution. The number of interactions in the past year varied between one-to-many times. One PwE paid with a goat, estimated at 46,490 RwF 2019 monetary value adjusted from 2014 prices.Citation28
The mean unweighted annual non-biomedical care costs (n=30) yielded 155.5 ± 249.8 US$, with one outlier of 1131.2 US$. The median annual cost was 49.5 US$ ().
After weighing of each variable, the mean and median were 67.6 and 21.5 US$ respectively, around 41% of all OoP costs.
Indirect Costs
Public transportation was the most commonly used means of transport by 59 (85.5%) PwE (). Mean ± SD and median distance of aroundtrip to the clinic were 83.2 ± 92.1km and 40km. Per visit, mean round trip travel time was 4h42 ± 3h00 and mean time at the hospital was 4h10min ± 2h04min, including time for technical and laboratory investigations. 11 minutes were spent at the consultation. The mean and median total monthly time per visit exceeded 8 hours. We calculated a mean annual loss of 13.3 working days per patient over a one-year period.
Table 4 Time Spent per Visit per Patient (Travel, Waiting Time, and Consultation)
Cost Burden of DMC, DnMC and OoP in Relation to a Change in Frequency of Follow-Up Consultations
We estimated the cost of follow-up as from the second year onwards, using the scenarios of unchanged monthly frequency (currently monthly), two-monthly or bi-monthly interval (scenario A), and three-monthly or quarterly interval (scenario B) (see ).
Figure 2 Changes in annual total and OoP cost burden in current monthly follow-up consultations, scenario A (bi-monthly consultations) and scenario B (quarterly consultations).
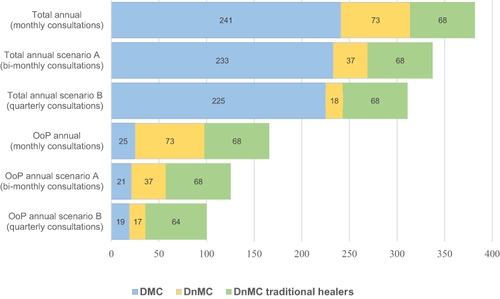
After the first year of treatment and with visits occuring monthly, weighted total mean DMC, CBHI coverage and OoP for DMC, were 198.6, 181.2 and 17.5 US$ respectively, representing a cost reduction of 20% compared to the first year of follow-up. Total OoP, including DMC and all DnMC, reduced only 3% to 158.2 US$. For scenario A and B, total costs decreased by 12% and 18% respectively. DMC costs born by the CBHI were reduced by 6% and 9% in case of scenario A and scenario B, respectively.
Total OoP changed from 163.2 US$ to 125.2 US$ for scenario A and 106.2 US$ for scenario B, representing a 23% and 35% reduction compared to current OoP costs (). Traditional healer DnMC increased to 54% of OoP for scenario A and 64% for scenario B. At a 2019 GDP per capita of 820.025 US$, OoP in the current follow-up schedule, and for scenario A and B represented 20%, 15% and 13% of total annual income, respectively.
Discussion
This cost of illness study in adult patients in a tertiary epilepsy center in Rwanda provides insight into the economic burden from individual and health insurance perspective.
Our data add to other studies illustrating the high economic burden of epilepsy on patients, families, medical services, or society, with the total annual OoP patient contribution amounting to 20% of the GDP per capita.Citation11–13
We estimated the weighted epilepsy specific annual total costs and DMC at 389.4 and 248.8 US$, respectively. The patient OoP costs amount to 163.2 US$. Only very few data on DMC in Africa are published.Citation14,Citation29 The total DMC of epilepsy in Rwanda is higher than in LMICs, eg, Burundi, India, Colombia, Nigeria, Democratic Republic RC and Bhutan,Citation11,Citation14,Citation15,Citation30–32 yet comparable to a study in Nigeria.Citation29
After adjusting for inflation, great variability when comparing cost structure of DMC was observed, probably related to differences in local healthcare organization. For example, the DMC in the DRC found a low DMC of technical investigations as they were not available at the study site. In South-Africa, ASM was free of charge. Therefore, any comparison to our data is strenuous.
In Europe, highly variable mean annual direct cost for epilepsy was reported in 2011 with a mean annual cost of 5221 €, varying between 1715 € in Bulgaria to 10,246 € in Germany.Citation33
DMC
The outpatient consultation was most frequently performed by a general practitioner under supervision of the neurologists, which is not uncommon in a low resource setting.Citation16 The rate of technical investigations is comparable to those observed in the literature.Citation22,Citation34 Laboratory costs up to 33.6US$ during the first year of follow-up, were often required for ASM blood level measurement. In primary healthcare centers, ASM blood level testing is not available and therefore cost of epilepsy management at the referral center likely overestimated mean cost in primary and secondary settings.
Three patients (5.5%) were hospitalized, resulting in an unweighted OoP of 26.7 US$, which constitutes 3% of GDP per capita. The burden of OoP costs for hospitalizations for individual patients is high, nonetheless on the total population, weighted cost only constituted 6% of the total OoP DMC. In our univariate analysis, hospitalization was a driver for DMC, which has also been observed in Europe and the US.Citation35,Citation36
The weighted annual mean ASM cost of 161.7 US$ represented 65% of total annual DMC. As the study was conducted at a referral center, ASM cost may be higher compared to primary and secondary centers as a broad range of ASM is available at the center. Also, 60% of patients were on polytherapy, increasing ASM cost.Citation37–39 The contribution of ASM to DMC is similar to other countries, eg, 67% in Russia and 81% in Nigeria and has also been observed in other LMIC such as India.Citation14,Citation16,Citation20,Citation21,Citation40 The cost associated with ASM in our study may be at the high end as we used pricing of the branded substance as a reference.Citation39
Biomedical DnMC
Biomedical DnMC amounted to 73.0US$, with a median of 61.2US$. The transportation costs were up to 84% of biomedical care DnMC, because of the long distance to be covered when seeking care at the tertiary neurology department. Our results were high compared to a study in Morocco with a mean transport cost per patient per year of 26.9 US$.Citation15 The median cost of transportation was similar to 64.9 US$ related to hospital visits in South Africa.Citation32
The burden of biomedical DnMC and resulting OoP decreased substantially when we assumed a lower follow-up frequency. Future prospective studies could be considered to study epilepsy outcomes, treatment adherence, and costs to evaluate the impact of a lower visit frequency in PwE.
Traditional Healers DnMC
More than 53% of PwE reported seeking traditional healer care, which is higher than 26% reported in 2005.Citation5 Non-biomedical care was not limited to PwE from rural areas, as 58.0% of PWE were from the urban region of Kigali. Similarly high numbers were reported in DRC and Uganda, at 48.8% and 34.8% respectively.Citation21,Citation41 The variability in seeking traditional healer care among PwE in sub-Saharan Africa may be explained by country-related differences with 99.5% traditional healers in Ghana offering epilepsy care, to 62.6% healers in Nigeria, and less than 6% in Kenya.Citation42
Annual traditional healer DnMC, all OoP costs, amounted to 41% of the total OoP cost, or 7.2% of the Rwandan GDP per capita.Citation27 This was lower compared to other LMIC, eg, Democratic Republic of Congo and Morocco.Citation15,Citation21 Our data contained an outlier of more than 1100 US$, adding to the variability of non-biomedical DnMC.Citation43 The role of traditional and faith healers in the management of epilepsy does require further investigations, especially as the DnMC in our study is high in contrast to the biomedical care pathway.Citation44
Indirect Costs
Indirect costs were not monetized, but we measured the burden of travel and waiting time.
The burden of hospital visit is highlighted by mean hospital time of 4 hours for one consultation of 11 minutes, in combination with a mean travel time of more than 4 hours. Similar observations have been made at different tertiary centers in other countries and may be related to the high number of patients seeking care at the tertiary health center. The “three long and a short” phenomenon has been proposed to explain this discrepancy: long registration time, long waiting time to see a doctor, long time waiting to be billed, and a short time spent seeing the doctor.Citation45
Future studies addressing total costs including indirect costs (loss of productivity, loss of working days due to seizures) are highly needed.
Study Limitations
We acknowledge several limitations to our study. The single center, mixed design with retrospectively collected DMC and cross-sectionally collected DnMC may have biased the results and is not representative for all PwE in Rwanda. For example, biomedical DnMC for transportation may have been underestimated as a higher proportion of patients was from Kigali region.
Cross-sectional studies are also subject to recall bias.Citation30 Our interviewers were trained to minimize errors in the collection of accurate data, nonetheless, we were not able to monetize DnMC related to, for example, social support, physiotherapy, etc.
Second, due to our inclusion and exclusion criteria, we were not able to account for costs of comorbidities or refractory epilepsy. Future studies should include PwE with comorbidities and refractory epilepsy, to allow for quantification of costs across subpopulations, which may be substantial.
Third, our study did account for biomedical epilepsy care outside the center, eg, health center visits in case of injuries after a seizure. Future studies need to include these costs, which undoubtedly will increase the total cost of illness as DMC is considered to be annually higher among persons with active seizures.Citation46
The implementation of study protocols to quantify the health service use and cost of epilepsy should be adapted and tailored to an LMIC to improve the understanding of real burden of epilepsy, also in Rwanda.Citation47
Conclusions and Recommendations
This exploratory study demonstrated the high economic burden for adult PwE at a tertiary epilepsy center of epilepsy-specific DMC, biomedical DnMC and traditional healer DnMC. The annual OoP patient cost was nearly 20% of the GDP per capita. OoP DMC only represented 14% of annual epilepsy specific OoP, with biomedical care DnMC and traditional healer DnMC accounting for 45% and 41% of OoP, respectively.
Further prospective studies are warranted to document the cost of epilepsy in Rwanda and explore whether a reduction in the frequency of follow-up visits could result in a decrease of total and OoP DnMC together with the feasibility of a holistic and integrated decentralized epilepsy care.
To address the traditional healer OoP, a public health plan of epilepsy co-management with traditional healers is required as they hold a pivotal role for patients in their local communities.
Abbreviations
ASM, anti-seizure medication; CBHI, community-based health insurance; DMC, Direct Medical Cost; DnMC, Direct non-Medical Cost; GDP, gross domestic product; LMIC, low- and middle-income countries; PwE, persons living with epilepsy; SSA, sub-Saharan Africa; US$, United States dollar.
Availability of the Data
The data supporting the findings of the study can be obtained on request from Dirk E Teuwen, corresponding author.
Ethics Approval and Consent to Participate
The study protocol and data collection forms were reviewed and approved by the Ethical Review Committee of the CARAES neuro-psychiatric hospital (012/CNEC/2020). Data for the direct medical costs were collected electronically, and the names of the PwE were anonymized prior to data processing. Informed consent was obtained from all PwE in the study of the DnMC.
Author Contributions
All authors made a significant contribution to the work reported, whether to conception, study design, execution, acquisition of data, analysis, and interpretation, or to all of these. All took part in drafting, revising or critically reviewing the article, and gave final approval of the version to be published. Authors have agreed on the journal to which the article has been submitted and are accountable for all aspects of the work.
Disclosure
DET was an employee of UCB Pharma at the time of the study and is now retired. PD received consultancy fees from UCB Pharma, Merck and Novartis. PAMJB received speaker and consultancy fees from UCB Pharma, LivaNova, and Medtronic, and research grants from the same companies through his institution. The authors have no other competing interests. The abstract of this paper was presented at the 2021 7th Congress of the European Academy of Neurology (EAN) as a poster presentation reporting interim findings. The poster’s abstract (EPO-250) was published in ‘EAN 2021 Abstract Book. Eur J Neurol 2021;28S1,597 (https://www.ean.org/fileadmin/user_upload/ean/congress-2021/EAN2021AbstractBook.pdf.)
Acknowledgments
The authors thank the PwE having participated in the non-medical cost survey and Emmanuel Ntakiyisumba, Solange Mukamazimpaka, Rosine Mukamusoni, Michel Nshimiyimana, staff at the CARAES Neuropsychiatry hospital, involved in the data collection. We thank Floribert Biziyaremye and Anna-Marie Teuwen for their support in data collection and cleaning.
Additional information
Funding
References
- Saxena S, Li S. Defeating epilepsy: a global public health commitment. Epilepsia Open. 2017;2(2):153–155. doi:10.1002/epi4.12010
- Owolabi LF, Owolabi SD, Adamu B, Jibo AM, Alhaji ID. Epilepsy treatment gap in Sub-Saharan Africa: meta-analysis of community-based studies. Acta Neurol Scand. 2020;142(1):3–13. doi:10.1111/ane.13246
- Ngugi AK, Kariuki SM, Bottomley C, Kleinschmidt I, Sander JW, Newton CR. Incidence of epilepsy: a systematic review and meta-analysis. Neurology. 2011;77(10):1005–1012. doi:10.1212/WNL.0b013e31822cfc90
- Ngugi AK, Bottomley C, Kleinschmidt I, Sander JW, Newton CR. Estimation of the burden of active and life-time epilepsy: a meta-analytic approach. Epilepsia. 2010;51(5):883–890. doi:10.1111/j.1528-1167.2009.02481.x
- Yemadje LP, Houinato D, Quet F, Druet-Cabanac M, Preux PM. Understanding the differences in prevalence of epilepsy in tropical regions. Epilepsia. 2011;52(8):1376–1381. doi:10.1111/j.1528-1167.2011.03099.x
- Sebera F, Munyandamutsa N, Teuwen DE, et al. Addressing the treatment gap and societal impact of epilepsy in Rwanda--results of a survey conducted in 2005 and subsequent actions. Epilepsy Behav. 2015;46:126–132. doi:10.1016/j.yebeh.2015.03.028
- Dedeken P, Sebera F, Mutungirehe S, et al. High prevalence of epilepsy in Northern Rwanda: exploring gender differences. Brain Behav. 2021;11(11):e2377. doi:10.1002/brb3.2377
- Health service packages for public health facilities. Rwanda; 2017. Available from: https://www.moh.gov.rw/fileadmin/user_upload/Moh/Publications/Legal_Framework/Public_health_Facilities_service_packages_in_Rwanda-1.pdf. Accessed December, 2020.
- Van Steenkiste F, Sebera F, Nsanzabaganwa W, et al. An ambispective cohort study on treatment outcomes of patients with epilepsy in a tertiary epilepsy center in Rwanda and recommendations for improved epilepsy care. Epilepsia Open. 2019;4(1):123–132. doi:10.1002/epi4.12304
- Rabarison KM, Bish CL, Massoudi MS, Giles WH. Economic evaluation enhances public health decision making. Front Public Health. 2015;3:164. doi:10.3389/fpubh.2015.00164
- Wibecan L, Fink G, Tshering L, et al. The economic burden of epilepsy in Bhutan. Trop Med Int Health. 2018;23(4):342–358. doi:10.1111/tmi.13035
- Hong Z, Qu B, Wu XT, Yang TH, Zhang Q, Zhou D. Economic burden of epilepsy in a developing country: a retrospective cost analysis in China. Epilepsia. 2009;50(10):2192–2198. doi:10.1111/j.1528-1167.2009.02185.x
- Wagner RG, Bertram MY, Gómez-Olivé FX, et al. Health care utilization and out-patient, out-of-pocket costs for active convulsive epilepsy in rural northeastern South Africa: a cross-sectional survey. BMC Health Serv Res. 2016;16:208. doi:10.1186/s12913-016-1460-0
- Nsengiyumva G, Druet-Cabanac M, Nzisabira L, Preux PM, Vergnenègre A. Economic evaluation of epilepsy in Kiremba (Burundi): a case-control study. Epilepsia. 2004;45(6):673–677. doi:10.1111/j.0013-9580.2004.36303.x
- Kissani N, Benkhadda S, Arkha S, Louhab N. Le coût de l’épilepsie dans la ville de Marrakech et sa région [the cost of epilepsy in Marrakech city and its area]. AMEEJ. 2016;5(1):21–24.
- Krishnan A, Sahariah SU, Kapoor SK. Cost of epilepsy in patients attending a secondary-level hospital in India. Epilepsia. 2004;45(3):289–291. doi:10.1111/j.0013-9580.2004.63102.x
- Nyandwi A, Umuhoza S, Uwaliraye P, Musange SF. Towards sustainability if the community-based health insurance in Rwanda: successes, challenges, and opportunities. SPARC Africa; 2021. Available from: https://sparc.africa/2021/09/towards-sustainability-of-The-community-based-health-insurance-in-rwanda-successes-challenges-and-opportunities/. Accessed November 25, 2022.
- Lu C, Chin B, Lewandowski JL, et al. Towards universal health coverage: an evaluation of Rwanda Mutuelles in its first eight years. PLoS One. 2012;7(6):e39282. doi:10.1371/journal.pone.0039282
- Woldemichael A, Gurara D, Shimeles A. The impact of community based health insurance schemes on out-of-pocket healthcare spending: evidence from Rwanda. IMF WORKING PAPERS; 2019. Available from: https://www.imf.org/-/media/Files/Publications/WP/2019/WPIEA2019038.ashx. Accessed November 25, 2022.
- Ezeala-Adikaibe B, Onwuekwe I, Ekenze S, Achor J, Onwukwe. J. Estimated direct cost of treating epilepsy per month in Southeast Nigeria. Internet J Neurol. 2009;13:1.
- Siewe Fodjo JN, Mandro M, Wonya’rossi D, et al. Economic burden of epilepsy in rural Ituri, democratic Republic of Congo. EClinicalMedicine. 2019;9:60–66. doi:10.1016/j.eclinm.2019.03.010
- Liu J, Liu Z, Meng F. The economic burden of epilepsy in a sample of people with epilepsy in China. Epilepsy Res. 2013;103(2–3):288–293. doi:10.1016/j.eplepsyres.2012.07.015
- Fisher RS, Cross JH, D’Souza C, et al. Instruction manual for the ILAE 2017 operational classification of seizure types. Epilepsia. 2017;58(4):531–542. doi:10.1111/epi.13671
- Fisher RS, Cross JH, French JA, et al. Operational classification of seizure types by the international league against epilepsy: position paper of the ILAE commission for classification and terminology. Epilepsia. 2017;58(4):522–530. doi:10.1111/epi.13670
- Pato Pato A, Cebrián Pérez E, Cimas Hernando I, Lorenzo González JR, Rodríguez Constenla I, Gude Sampedro F. Analysis of direct, indirect, and intangible costs of epilepsy. Neurologia. 2011;26(1):32–38. doi:10.1016/j.nrl.2010.10.002
- Chin JH. Epilepsy treatment in sub-Saharan Africa: closing the gap. Afr Health Sci. 2012;12(2):186–192. doi:10.4314/ahs.v12i2.17
- World Bank GDP per Capita; 2020 Available from: https://data.worldbank.org/country/rwanda?view=chart. Accessed November 25, 2020.
- Rwembeho S. Goat meat prices up. New Times; December 03, 2014. Available from: https://www.newtimes.co.rw/article/113868/News/goat-meat-prices-up#:~:text=A%20medium%2Dsized%20goat%20is,most%20places%20in%20the%20province. Accessed December, 2020.
- Sanya EO, Kolo PM, Adekeye A, Mustapha K, Ademiluyi BA, Ajayi K. Cost of epilepsy care in a Nigerian tertiary hospital. Niger Postgrad Med J. 2013;20(4):266–271.
- Ughasoro MD, Onwujekwe OE, Ojinnaka NC. Economic cost of treatment of childhood epilepsy in Enugu, southeast Nigeria. Int J Technol Assess Health Care. 2014;30(4):469–474. doi:10.1017/S0266462314000518
- Fandiño-Franky J, Silfvenius H. World-wide disparities in epilepsy care: a Latin American outlook. Epilepsia. 1999;40(Suppl 8):48–54. doi:10.1111/j.1528-1157.1999.tb00948.x
- Wagner RG, Kabudula CW, Forsgren L, et al. Epilepsy care cascade, treatment gap and its determinants in rural South Africa. Seizure. 2020;80:175–180. doi:10.1016/j.seizure.2020.06.013
- Gustavsson A, Svensson M, Jacobi F, et al. Cost of disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21(10):718–779. doi:10.1016/j.euroneuro.2011.08.008
- Guerrini R, Battini R, Ferrari AR, et al. The costs of childhood epilepsy in Italy: comparative findings from three health care settings. Epilepsia. 2001;42(5):641–646. doi:10.1046/j.1528-1157.2001.27300.x
- Quintana M, Fonseca E, Sánchez-López J, et al. The economic burden of newly diagnosed epilepsy in Spain. Epilepsy Behav. 2021;125:108395. doi:10.1016/j.yebeh.2021.108395
- Begley C, Wagner RG, Abraham A, et al. The global cost of epilepsy: a systematic review and extrapolation. Epilepsia. 2022;63(4):892–903. doi:10.1111/epi.17165
- Haroon A, Tripathi M, Khanam R, Vohora D. Antiepileptic drugs prescription utilization behavior and direct costs of treatment in a national hospital of India. Ann Indian Acad Neurol. 2012;15(4):289–293. doi:10.4103/0972-2327.104338
- Sarangi SC, Kaur N, Tripathi M. Need for pharmacoeconomic consideration of antiepileptic drugs monotherapy treatment in persons with epilepsy. Saudi Pharm J. 2020;28(10):1228–1237. doi:10.1016/j.jsps.2020.08.013
- Beghi E, Garattini L, Ricci E, Cornago D, Parazzini F; EPICOS Group. Direct cost of medical management of epilepsy among adults in Italy: a prospective cost-of-illness study (EPICOS). Epilepsia. 2004;45(2):171–178. doi:10.1111/j.0013-9580.2004.14103.x
- Guekht A, Mizinova M, Kaimovsky I, Danilenko O, Bianchi E, Beghi E. The direct costs of epilepsy in Russia. A prospective cost-of-illness study from a single center in Moscow. Epilepsy Behav. 2016;64:122–126. doi:10.1016/j.yebeh.2016.08.031
- Rutebemberwa E, Ssemugabo C, Tweheyo R, Turyagaruka J, Pariyo GW. Biomedical drugs and traditional treatment in care seeking pathways for adults with epilepsy in Masindi district, Western Uganda: a household survey. BMC Health Serv Res. 2020;20(1):17. doi:10.1186/s12913-019-4879-2
- Esan O, Appiah-Poku J, Othieno C, et al. A survey of traditional and faith healers providing mental health care in three sub-Saharan African countries. Soc Psychiatry Psychiatr Epidemiol. 2019;54(3):395–403. doi:10.1007/s00127-018-1630-y
- Anand P, Othon GC, Sakadi F, et al. Guinea epilepsy project. Epilepsy and traditional healers in the Republic of Guinea: a mixed methods study. Epilepsy Behav. 2019;92:276–282. doi:10.1016/j.yebeh.2019.01.017
- Kissani N, Cherkaoui Rhazouani O, Souirti Z, et al. Epilepsy in Morocco: realities, pitfalls and prospects. Epilepsia Open. 2020;6(1):13–21. doi:10.1002/epi4.12440
- Chao J, Lu B, Zhang H, Zhu L, Jin H, Liu P. Healthcare system responsiveness in Jiangsu Province, China. BMC Health Serv Res. 2017;17(1):31. doi:10.1186/s12913-017-1980-2
- Moura LMVR, Karakis I, Zack MM, Tian N, Kobau R, Howard D. Drivers of US health care spending for persons with seizures and/or epilepsies, 2010–2018. Epilepsia. 2022;63:2144–2154. doi:10.1111/epi.17305
- Tulleners R, Blythe R, Dionisio S, Carter H. Resource use and costs associated with epilepsy in the Queensland hospital system: protocol for a population-based data linkage study. BMJ Open. 2021;11(12):e050070. doi:10.1136/bmjopen-2021-050070