Abstract
Background
Data on the economic burden of head and neck cancers (HNCs) in Germany is scarce. About 16%–28% of these cancers are associated with human papillomavirus (HPV) infection. Therefore, the study reported here aimed to assess the annual costs of HPV-related HNCs incurred by hospitalization, inpatient rehabilitation, and sick leave in Germany in 2008.
Methods
A cross-sectional retrospective analysis of five German databases covering hospital treatment, inpatient rehabilitation, and sick leave in 2008 was performed. All hospital, inpatient rehabilitation, and sick leave cases due to HNCs in 2008 were analyzed. Associated numbers of HNC hospitalizations, health care resource use, and costs were identified and extracted using the International Classification of Diseases, tenth revision (ICD-10; World Health Organization, Geneva, 1990) codes C01–C06, C09–C14, and C32 as the main diagnoses. Resources were valued with German official prices in 2008 euros (€). The annual costs of HPV-related HNCs were estimated based on the percentage of HNCs likely to be attributable to HPV infection.
Results
In 2008, there were 63,857 hospitalizations, 4898 inpatient rehabilitations, and 17,494 sick leaves due to HNCs, representing costs of €365.78 million. The estimated annual costs associated with HPV-related HNCs were €78.22 million, mainly attributed to males (80%). Direct costs accounted for 84% (80% for hospital treatment, 4% for inpatient rehabilitation) and indirect costs due to sick leave accounted for 16% of HPV-related HNC costs.
Conclusion
The economic burden of HPV-related HNCs in Germany in 2008 has been underestimated, since costs incurred by outpatient management, outpatient chemotherapy, long-term care, premature retirement, and premature death were not included. However, as far as we are aware, this study is the first analysis to investigate the economic burden of HNCs in Germany. The estimated annual costs of HPV-related HNCs contribute to a significant economic burden in Germany and should be considered when assessing the health and economic benefits of HPV vaccination in both sexes.
Introduction
Head and neck cancers (HNCs) comprise a broad spectrum of cancers in various anatomical sites, including the lips, oral cavity, oropharynx, pharynx, and larynx.Citation1–Citation3 The incidence and mortality rates of these cancers vary worldwide and are generally higher in developing countries.Citation2,Citation4 The highest incidence of these cancers is observed in males and in those older than 50 years.Citation2,Citation3 In 2008, HNCs accounted for 133,664 new cancers and were responsible for more than 63,000 deaths in Europe.Citation5
In Germany in 2008, there were 9520 new cancers of the oral cavity and pharynx (International Classification of Diseases, tenth revision [ICD-10]Citation6 codes C00–C14) in males and 3490 in females, and 3610 new cancers of the larynx (ICD-10 C32) in males and 510 in females.Citation7 Oral cavity and pharynx cancers represented the fifth most common cancers in males (3.9%) and the fifteenth most common in females (1.6%); while larynx cancer was the sixteenth most common cancer in males (1.5%) and the twenty-second most common in females (0.2%).Citation7 The standardized incidence rate (Europe) per 100,000 was 19.1 in males and 5.9 in females for oral cavity and pharynx cancers, and 6.9 in males and 0.9 in females for larynx cancer.Citation7 There were 3776 deaths due to oral cavity and pharynx cancers in males and 1170 in females, as well as 1275 deaths due to larynx cancer in males and 209 in females; the standardized mortality rate (Europe) per 100,000 was 7.4 in males and 1.8 in females for oral cavity and pharynx cancers, and 2.4 in males and 0.3 in females for larynx cancer.Citation7
The well-known major risk factors for HNCs include tobacco smoking and alcohol consumption, which act synergistically. Poor oral hygiene is also regarded as a possible risk factor for oral cavity cancer.Citation1,Citation7 In addition, numerous studies have shown the increasing role of sexually transmitted human papillomavirus (HPV) infection in the incidence of HNCs.Citation1,Citation2,Citation4,Citation8,Citation9 The HPV-associated proportions vary greatly according to the anatomic site of the HNC; examples include oral cavity cancer (16%9 and 23.5%2), oropharynx cancer (28.2%9 up to 72.0%2), pharynx other (21.3%9 and 24.0%2), other sites in the lip, oral cavity and pharynx areas (28.2%9 up to 72.0%2), or larynx cancer (average 21.3%, range 5.0%–24.0%).Citation9 The wide variations in reported HPV prevalence may depend on the HPV diagnostic methodology, especially in earlier studies.
The precursor lesion of HNCs is squamous intraepithelial neoplasia (SIN), which is graded from 1 (mild) to 3 (severe, carcinoma in situ).Citation10 The prevalence and incidence of SIN in Germany as a whole are unknown.Citation10 In the region of Thuringia in Germany, the average annual crude incidence of SIN 3 (HNC in situ) was 0.14 per 100,000 persons during 1996–2005.Citation9
Treatment of HNCs focuses on surgery, radiotherapy, chemotherapy, or a combination of these (so-called multimodal therapy).Citation2,Citation11,Citation12 Early stage disease is treated by one modality, whereas multimodal therapy is frequently applied in advanced disease states.Citation2,Citation11,Citation12 However, the overall prognosis remains poor. According to an analysis of the regional Thuringian cancer registration database in Germany, there was no significant improvement of the 5-year overall survival rate of HNCs from 1996 to 2005, though treatment strategies have changed to more frequently applied multimodal therapy.Citation11
A number of studies assessing the disease burden and cost of HPV-related HNCs exist;Citation2–Citation4,Citation12–Citation16 however, disease burden and cost are poorly documented in Germany because, as far as we are aware, no studies of the German setting exist. Therefore, the objective of the study reported here was to estimate the economic burden due to hospitalization, inpatient rehabilitation, and sick leave of HPV-related HNCs in Germany in 2008.
Materials and methods
Study design
The study was based on a retrospective cross-sectional analysis of five German databases that cover hospitalizations,Citation17 distribution of diagnosis-related groups (DRGs) and major categories of treatment during hospital stay,Citation18 inpatient rehabilitation,Citation19 and sick leave,Citation20,Citation21 each with the reference year 2008. These databases are described in detail following.
Associated numbers of HNC hospitalizations, health care resource use, and unit costs were identified and extracted using the ICD-10 codes C01–C06, C09–C14, and C32 as the main diagnoses, henceforth called “cancers of interest.” Depending on the different anatomic sites, these diseases were classed within five cancer categories: (1) oral cavity (C02–C06: tongue other, gum, floor of mouth, palate, mouth other), (2) oropharynx (C01, C09–C10: base of tongue, tonsil, oropharynx), (3) pharynx other (C11–C13: nasopharynx, piriform sinus, hypopharynx), (4) other sites (C14: other/ill-defined sites in the lip, oral cavity and pharynx), and (5) larynx (C32: larynx). The extracted numbers of cases refer to resource consumption units and not to patients. Annual costs of HPV-related HNCs were estimated by considering the cancer-specific proportions attributable to HPV infection (not sex-specific).Citation2,Citation9
The annual cost of HNCs was estimated by considering the expenditure of social insurance bodies as proxies for direct medical costs incurred by hospital treatment and inpatient rehabilitation. Indirect costs due to sick leave were estimated using the human capital approach, which measures productivity losses by multiplying the work time lost as a consequence of illness by the gross earnings of the individuals affected. Resources were valued with German official prices in 2008 euros (€).
Outpatient management and patients’ co-payments and out-of-pocket expenses were not considered. Further information on which components were and were not included in the study is presented in .
Table 1 Cost components of the analysis
Estimation of direct costs incurred by hospitalization
The annual cost incurred by hospital treatment (medical attendance, care, drugs, devices, physical therapy, board and lodging) of HNCs was based on the number of hospitalizations and the average cost per hospital stay. The number of hospital stays with a main diagnosis of the cancers of interest was extracted from the hospital statistics published by the Federal Statistical Office Germany (Destatis).Citation17 These statistics are by law exhaustive for all GermanyCitation17 and provide information on the number of hospitalizations by ICD-10 code, age group, and sex.Citation17
The average hospital treatment cost per hospitalization for HNCs was derived from the type and number of German diagnosis-related group (G-DRG) positions reimbursed for a main diagnosis of the cancers of interest. G-DRG data are by law exhaustive for all GermanyCitation18 and are published by the Institute for the Hospital Remuneration System as “G-DRG Browser,”Citation18 which provides information on type and frequency of reimbursed G-DRGs per ICD-10 main diagnosis as well as type and frequency of major treatment categories such as surgery, radiotherapy, and medical treatment per reimbursed G-DRG position.
Costs for each extracted G-DRG position related to a main diagnosis of the cancers of interest were calculated multiplying the cost weight of each extracted G-DRG positionCitation18 with the Germany-wide average base rate of €2803.05 in 2008.Citation22,Citation23 The cost weight is a DRG-specific factor that depends on diagnosis, secondary diagnosis, age, whether or not surgery is conducted, type of surgical procedures, and complications. The cost weight thus reflects the intensity of resource consumption during hospital stay relative to the average case value, which is represented by the base rate in monetary terms.
For all G-DRG positions, the G-DRG Browser only lists the top-20 main diagnoses. If a case has a main diagnosis that is among the top 20 of a certain DRG, this case shows up in the browser data. If a rare main diagnosis uses a G-DRG that is used by many other more frequent main diagnoses, it will not show up in the browser. The extrapolation of costs from the number of cases in the G-DRG Browser to the number of cases from the hospital statistics was done directly for cancers of interest with less than 30% of missing cases compared with the hospital statistics. In the case of cancers of interest with more than 30% of missing cases compared with the hospital statistics, the extrapolation was supplemented by collection of aggregate anonymized data on the distribution of G-DRG positions for treatment of these cancers of interest in one hospital to identify potential important missing G-DRGs.
Hospital treatment costs extrapolated from the G-DRG BrowserCitation18 data were stratified by sex assuming the same distribution for costs as for the number of hospitalizations extracted from the hospital statistics.Citation17
Estimation of direct costs incurred by inpatient rehabilitation
For HNC patients, rehabilitation care includes nutritional counseling, therapy for dysphagia, psychosocial training to accept a changed appearance, training in the use of prosthesis, restoration of oral communication ability, and manual lymphatic drainage. The annual cost incurred by inpatient rehabilitation due to the cancers of interest after acute hospital cancer treatment was based on the number and average duration of rehabilitation stay (in days) and the average cost per day.
The number of rehabilitation stays with a main diagnosis of the cancers of interest was extracted from the rehabilitation statistics published by the holder of the German Public Pension Insurance (DRV).Citation19 These statistics are by law exhaustive for all GermanyCitation19 and provide information on the number of inpatient rehabilitation stays and duration in days by ICD-10 three-digit code and sex.Citation19 Outpatient rehabilitation was not included in this study, as the related data are aggregated over disease groups,Citation19 thus preventing ICD-10 three-digit codes from being extracted.
The average cost per day of inpatient rehabilitation was also derived from rehabilitation statistics.Citation19 Total costs of €2,689.84 millionCitation19 divided by a total of 24,120,180 days (804,006 cases with a mean of 30 days per stay)Citation19 resulted in an average cost of €111.52 per day for inpatient rehabilitation. This average cost per day is not disease-specific.
The number, length of stay, and cost of inpatient rehabilitation stays were stratified by sex.
Estimation of indirect costs incurred by sick leave
The annual cost incurred by sick leave due to the cancers of interest was based on the number of sick leaves, the average duration per case in days, and cost per day.
The number and duration of sick leaves were estimated in two steps. In the first step, the number of sick leave cases and average duration per sick leave case in days due to the cancers of interest, each by sex, were extracted from statistics covering the population of all compulsory members (ie, insured without co-insured dependants and pensioners) of the Local Statutory Health Insurance (SHI) fund (AOK), which is the biggest of the SHI funds in Germany. These statistics are available via the Information System of Federal Health Monitoring (GBE).Citation20 As these data are not exhaustive for all Germany, a second step was applied to extrapolate the numbers and duration of sick leave cases by sex extracted from the AOK statisticsCitation20 to the total German compulsory SHI member population, based on statistics of the total German SHI population published by the Federal Ministry of Health (Bundesministerium für Gesundheit), the KM6 statistics.Citation21 This was done based on the sex-specific share compulsory AOK members took in the total compulsory SHI member population in 2008, available from the KM6 statistics.Citation21
Using the human capital approach,Citation24 the overall employee compensation per employee per day was used as cost per day of sick leave. The overall employee compensation per employee per day in 2008 was derived from the Statistical Yearbook.Citation25 An overall employee compensation of €1225.84 billionCitation25 divided by 35,845,000 employeesCitation25 and 365 days resulted in €93.69 per employee per day.
The number, duration (in days), and costs incurred by sick leave were stratified by sex.
Estimation of annual costs of HNCs and of HPV-related HNCs
The annual cost of HNCs was estimated by adding costs incurred by hospitalization, inpatient rehabilitation, and sick leave. These annual costs were stratified by direct and indirect costs as well as by sex.
A separate calculation was made to estimate the total annual cost of HPV-related HNCs, considering the cancer-specific proportions attributable to HPV infectionCitation2,Citation9 (). This was also stratified by direct and indirect costs as well as by sex.
Table 2 Average and limits of head and neck cancer-specific proportions attributable to human papillomavirus infection
Statistical methods
Due to the nature of the databases used,Citation17–Citation20 which exclusively provide average values of all the cases comprised, no measure of variability could be quoted for the estimated cost figures for HNCs. However, this is deemed acceptable, as the hospital and rehabilitation statististicsCitation17,Citation19 are by law exhaustive for all Germany.Citation17,Citation19 In addition, the G-DRG-related base rateCitation22,Citation23 to estimate costs incurred by hospitalization and the cost per day of inpatient rehabilitationCitation19 to estimate costs incurred by inpatient rehabilitation each are Germany-wide averages.Citation19,Citation22,Citation23 Hence, the use of Germany-wide averages and the fact that the data are exhaustive allowed us to refrain from sensitivity analysis, as no variability was expected.
However, for the estimation of HPV-related costs, the average values and limits of the cancer-specific proportions attributable to HPV infection () were applied to receive a range of these costs. When no explicit lower limit was reported, the available average value was used as a substitute for the respective lower limit () to avoid speculative assumptions. All analyses were performed using Microsoft® Excel 2007 (Microsoft, Redmond, WA, USA).
Results
Direct costs incurred by hospitalization
Number of hospitalizations
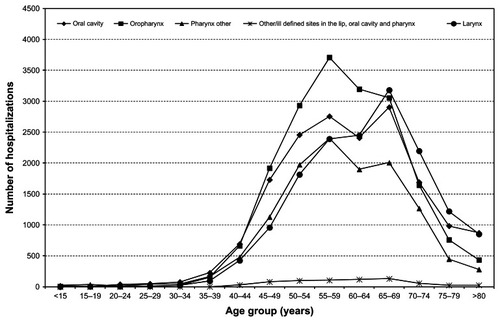
In 2008, there were 63,857 hospitalizations for HNCs in Germany: 50,869 for males (80%) and 12,988 for females (20%). The number of hospitalizations by cancer category and sex is given in . The most frequent was oropharynx cancer (29%), followed by cancer of the oral cavity (26%), larynx (25%), pharynx other (19%), and other sites (1%). The distribution of the number of hospitalizations by age group and cancer category is given in . The number of hospitalizations increased starting from age 35–39 years. Hospitalizations for oropharynx and pharynx other cancers peaked in the 55–59 year age group, whereas all remaining HNC hospitalizations peaked in the 65–69 year age group (). Considering all HNCs together, the number of hospitalizations showed a bimodal age distribution; hospitalizations were most frequent in the 55–59 year age group (n = 11,355), followed closely by the 65–69 year age group (n = 11,276). Of all hospitalizations due to HNCs, 78% were for patients between 40 and 69 years of age; 53% and 38% were for patients older than 60 and 65 years, respectively.
Table 3 Resource consumption units by head and neck cancer category and sex in Germany in 2008 (any inconsistencies are due to rounding)
Major categories of treatment
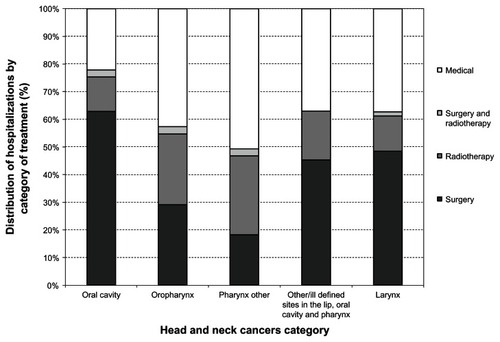
The distribution of the hospitalizations by major treatment categories for each HNC category was derived from the G-DRG codes extracted from the G-DRG Browser.Citation18 This distribution is displayed in and shows some variation depending on the cancer category. Considering all HNCs together, most of the hospitalizations (not patients) were linked to surgical procedures exclusively (41%), followed by medical treatment (37%) and radiotherapy exclusively (19%). Combination treatment of surgery and radiotherapy accounted for 2% of the hospitalizations. All important G-DRGs for HNC treatment seemed to be accounted for in the G-DRG Browser as the hospital data showed.
Costs
Compared with the hospital statistics,Citation17 more than 30% of hospitalizations were missing in the G-DRG BrowserCitation18 for six of the 13 ICD-10 codes related to HNCs: C03 (gum), C05 (palate), C06 (mouth other), C11 (nasopharynx), C12 (piriform sinus), and C14 (other/ill-defined sites in the lip, oral cavity, and pharynx). However, the collected anonymized hospital data for these six ICD-10 codes showed that no important G-DRGs were missed compared with the extracted G-DRG Browser data. Hence, average costs per hospitalization derived from the cost weight of each extracted G-DRG positionCitation18 and the Germany-wide average base rateCitation22,Citation23 were used for the extrapolation of costs from the number of hospitalizations in the G-DRG Browser to the number of hospitalizations from the hospital statistics for all 13 ICD-10 codes for HNCs. In 2008, HNC hospitalizations had a total cost of €293.66 million in Germany, of which €228.75 million were attributed to males (78%) and €64.91 million to females (22%). The distribution of these costs by cancer category and sex is given in . The main contributors to these costs were oral cavity (37%) and oropharynx cancers (27%).
Table 4 Annual costs (€) by head and neck cancer category and sex in Germany in 2008 (any inconsistencies are due to rounding)
Direct costs incurred by inpatient rehabilitation
In 2008, there were 4898 inpatient rehabilitations for HNCs in Germany – 3798 for males (78%) and 1100 for females (22%) – corresponding to a total of 117,506 days of inpatient rehabilitation for HNCs. The number of inpatient rehabilitations and length of stay by cancer category and sex are given in . Based on an average cost of €111.52 per day, the cost incurred by inpatient rehabilitation was €13.10 million, of which €10.05 million was attributed to males (77%) and €3.05 million to females (23%). Annual costs for inpatient rehabilitation by cancer category and sex are given in . The main contributors to these costs were oropharynx (31%) and oral cavity cancers (29%).
Indirect costs incurred by sick leave
In 2008, compulsory AOK members comprised 5,409,955 males and 4,067,300 females.Citation21 There were 5224 sick leave cases due to HNCs for males, corresponding to a total of 190,379 sick leave days, and 760 sick leave cases due to HNCs for females, corresponding to a total of 25,477 sick leave days.Citation20 In 2008, the total German compulsory SHI member population (insurance members who were working) comprised 15,374,034 males and 14,174,791 females.Citation21 Hence, the factors were 15,374,034/5,409,955 = 2.8414 for males and 14,174,791/4,067,300 = 3.4851 for females to extrapolate cases and days of sick leave from compulsory AOK members to the total German compulsory member population.
There were 17,494 cases (85% for males, 15% for females) and 629,809 days (86% males, 14% females) of sick leave due to HNCs in Germany in 2008. The number of sick leaves and the duration in days by cancer category and sex are displayed in . At a cost of €93.69 per workday lost, indirect costs incurred by sick leave are estimated at a total of €59.01 million, with €50.69 million attributed to males (86%) and €8.32 million to females (14%). The distribution of these costs by cancer category and sex is given in . The main contributors to these costs were oral cavity (30%) and oropharynx cancers (28%).
Annual costs incurred by hospitalization, inpatient rehabilitation, and sick leave
In 2008, the total annual cost of HNCs amounted to €365.78 million in Germany, mainly driven by males (79%). Of this total cost, 84% comprised direct costs (80% hospitalization, 4% inpatient rehabilitation) and 16% indirect costs incurred by sick leave. The stratification of this total cost by cost category and sex is displayed in .
Table 5 Total annual costs (€ million) of head and neck cancers by cost category and sex in Germany in 2008 (any inconsistencies are due to rounding)
The cancer category-specific prevalence rates of HPV in HNCCitation2,Citation9 () applied to the values in resulted in the average and range of total annual HPV-related cost of HNCs stratified by cost category and sex (). The economic burden of HNCs attributable to HPV infection amounted to an average of €78.22 million (80% males compared with 20% females) with a range of €66.41 million to €137.57 million.
Table 6 Average and range of total annual human papillomavirus-related costs (€ million) of head and neck cancers by cost category and sex in Germany in 2008 (any inconsistencies are due to rounding)
Discussion
This study estimated that the annual cost due to hospitalization, inpatient rehabilitation, and sick leave incurred by HPV-related HNCs in Germany in 2008 was €78.22 million, which was mainly attributed to males (80%), with 84% of the total comprised of direct costs (80% hospitalization, 4% inpatient rehabilitation) and 16% indirect costs due to sick leave.
The present study used a cross-sectional approach to estimate these annual costs. The data used to estimate the number of hospitalizations,Citation17 inpatient rehabilitations,Citation19 and sick leavesCitation20 are from patients with at least one such resource consumption in the reference year. Thus, as the numbers refer to resource use or consumption and not to single patients in that year,Citation17–Citation20 no patient level information is available with respect to comorbidities or numbers of hospitalizations, inpatient rehabilitations or sick leaves, each per patient per year. Additionally, for hospital treatment, no incident cases with high resource consumption can be distinguished from prevalent cases with less resource consumption due to the nature of the databasesCitation17,Citation18 available. Thus, the estimated average cost of hospitalization due to HNCs of €4599 (from €3571 for larynx cancer up to €6546 for cancer of other sites)Citation18,Citation22,Citation23 reflects the average cost of all HNC cases treated in the hospital. It is consequently lower than the average cost per patient or per new case, as patients may be hospitalized several times per year. For example, in The Netherlands, cost was €21,858 per HNC patient for the first 2 years following diagnosis and decreased to €423 during the 10 years of follow-up (1996 values).Citation14
In Germany in 2008, there were 17,130 incident cases of HNCs (13,130 males and 4000 females).Citation7 The 5-year partial prevalence (ie, number of patients alive with a diagnosis of cancer for no longer than 5 years who are likely to receive primary treatment) is the best suited reference point to be compared with the number of treated cases in 2008 found in this study. The 5-year partial prevalence amounted to about 46,900 patients with HNCs in Germany in 2008.Citation7 These 5-year partial prevalence data compare well to 63,857 hospitalizations, found in the present study for the year of 2008 in Germany. However, the numbers of cancers of interest to which we applied specific proportions attributable to HPV infection might have been slightly overestimated. Coding systems often limit data accuracy, and some of the ICD-10 codes used in the present study to identify HNCs of interest covered specific locations that have not yet been formally linked to HPV (eg, nasopharynx).
The estimation of costs incurred by sick leave was based on the sex-specific extrapolation of the AOK dataCitation20 to the total German compulsory SHI member population in 2008.Citation21 This extrapolation may have been limited by the fact that the age distribution is not given in the AOK dataCitation20 and compulsory AOK members are of somewhat lower socioeconomic status than average.Citation26 In 2008, compulsory AOK members had 11.74 days of sick leave per sick leave case and 106.5 sick leave cases per 100 members.Citation27 The total German compulsory SHI member population had 12.45 days of sick leave per sick leave case and 95.1 sick leave cases per 100 members.Citation28 Therefore, the bias introduced by the extrapolation of the cancer-specific sick leave data of the compulsory AOK membersCitation20 to the total German compulsory SHI member populationCitation21 may be minimal. In addition, more than half (53%) of the hospitalizations for HNCs were for patients older than 60 years (); this is past the average age of retirement of 60.7 years in Germany in 2008.Citation29 Hence, the mentioned minimal extrapolation bias only affects a relatively small amount of indirect costs due to sick leave of employed patients with HNCs – that is, those younger than the average retirement age.
However, as the other half of the hospitalizations for HNCs were for patients younger than 60 years () – that is, below the average retirement age in Germany,Citation29 the expected increase in HNC incidence, especially in younger age groups,Citation1,Citation7 will lead to an increase in indirect costs due to loss of productivity in addition to an increase in direct costs incurred by treatment of patients with HNCs.
Several factors contribute to the strength of the present study. Most importantly, the data sources used for the number of the cancer-specific hospitalizationsCitation17 and inpatient rehabilitationsCitation19 were by law exhaustive for all Germany. These databases were also used in previous cost-of-illness (CoI) analyses.Citation30–Citation32 In addition, the quality of coding and case allocation of complex head and neck surgery cases within the G-DRG system was improved in 2008 compared with the years before.Citation33 Thus, the G-DRG-based costs of hospitalizations incurred by HNCs used in the study presented here are very likely to represent valid cost estimates.
Limitations of this study are mainly linked to the cost components covered compared with the components of overall CoI. This study covered only three out of eleven components of overall CoI (); it excluded important expenses categories such as outpatient management and patients’ co-payments and out-of-pocket expenses, which are likely to be important contributors to the total economic burden of HNC management. In addition to the restrictions already mentioned, costs incurred by complications, side effects, or sequelae of the treatment of HNCs, such as side effects relating to dysphagia or mucositis, usually managed in outpatient care, were not included. Management costs of dysphagia are reported to range between US$153 and US$710Citation34 and between €3480 and €4764 per episode of mucositis.Citation13 Given these factors, it is clear that this study underestimated the total annual cost of HNCs and of HPV-related HNCs in Germany in 2008 to a considerable extent. However, to avoid speculative assumptions and maintain a conservative approach, no attempts were made to roughly estimate the potential contribution of all the costs not included.
Due to the differences in study designs, national health care systems, unit costs, incidence patterns, and in cost components covered, the results of the present study are difficult to compare with those of other CoI analyses of HPV-related HNCs.Citation2–Citation4,Citation12–Citation16 However, the results of our study are similar to results found for FranceCitation2 with respect to hospital costs. Costs incurred by hospitalization for HNCs amounted to €284.43 million (2007 values), with €73.95 million attributable to HPV infection in France,Citation2 compared with €293.66 million and €62.49 million, respectively, in our study in Germany (2008 values).
Costs incurred by HPV-related HNCs are significant in males rather than females (80% for males in the present study). There is growing evidence of a causal role for HPV in HNCs.Citation35 Over the past decades, the proportion of HPV-positive oral cancers has significantly increased, while, at the same time, HPV-negative cancers have decreased.Citation1,Citation36,Citation37 As since 2008 – the reference year for cost estimation in the present study – 5 years have passed, the impact of a change in resource consumption and in unit costs (prices) should be discussed. An increase in resource consumption due to an increase in the incidence of HPV-related HNCCitation1,Citation36,Citation37 could not be considered as the nature of the databasesCitation17,Citation19,Citation20 available does not allow incident cases to be distinguished from prevalent cases. The impact of increasing unit costs, however, could be examined using 2011 as the most recent common reference year.Citation38–Citation40 The Germany-wide average base rate of €2803.05 in 2008Citation22,Citation23 for calculation of direct costs incurred by hospitalization increased to €2963.82 in 2011,Citation38 an average annual percentage change (APC) of 1.02%. The average cost of €111.52 per day for inpatient rehabilitation in 2011Citation19 increased to €113.20 in 2011,Citation39 an APC of 1%. The overall employee compensation per employee per day for calculation of indirect costs incurred by sick leave increased from €93.69 in 2008Citation25 to €98.99 in 2011,Citation40 an APC of 1.02%. Assuming these APCs were also applicable during 2008 and through to 2013, and a steady resource consumption during 2008 to 2013, leads to an expected economic burden of HPV-related HNCs of an average of €85.60 million with a range of €72.69 million to €150.57 million in 2013 based on extrapolating the values for 2008 given in . This is an increase of about 9.5% from 2008 to 2013. When also considering the increase in the incidence of HPV-related HNCs,Citation1,Citation36,Citation37 the increase in the economic burden of HPV-related HNCs would be even higher over the 5-year period.
HPV vaccination has demonstrated high prophylactic efficacy against pre-cancerous lesions of the cervix, vulva, and vagina. Recently, the quadrivalent HPV vaccine has demonstrated high clinical efficacy on anal pre-cancers in males.Citation41 One can speculate that HPV vaccination might extend protection against other cancers associated with HPV 16 and 18. Therefore, data from the present study could be useful for decision-makers who must assess the potential effect of HPV vaccination on the incidence of HNCs in males and females.
Conclusion
To our knowledge, this study is the first analysis to have investigated the economic burden of HNCs incurred by hospitalization, inpatient rehabilitation, and sick leave in Germany. The estimated annual costs of HPV-related HNCs contribute to a significant economic burden of at least €78.22 million in Germany; this information could be useful for decision-makers in terms of assessing whether an HPV vaccination strategy would be cost-effective in Germany, considering the potential vaccine’s impact on the burden of HPV-associated HNCs. Further, these costs are underestimated since, inter alia, outpatient management and management of precursor lesions could not be included, as there is currently no data on these. Hence, further research is required to fully estimate the economic burden of HPV-related HNCs in Germany.
Acknowledgments
The authors are grateful to L Moro, employee of Sanofi Pasteur MSD (SPMSD), Lyon, France, at the time of conduct of the study and writing of the manuscript, and to N Largeron and E Préaud, employees of SPMSD, for their comments on an earlier version of the manuscript.
Disclosure
This study was funded by an unrestricted grant from SPMSD. JPK has received remunerations from SPMSD. PKS and XC are employees of IGES Institut, Berlin, Germany, and have worked on projects of IGES Institut that have been funded by SPMSD. VR is an employee of SPMSD, manufacturer of one HPV vaccine.
This study was presented at the 27th International Papillomavirus Conference, Berlin, Germany, September 17–22, 2011 and at the 14th Annual European Congress of the International Society for Pharmacoeconomics and Outcomes Research, Madrid, Spain, November 5–8, 2011.
References
- BlombergMNielsenAMunkCKjaerSKTrends in head and neck cancer incidence in Denmark, 1978–2007: focus on human papillomavirus associated sitesInt J Cancer2011129373374120878955
- St GuilyJLBorgetIVainchtockARémyVTakizawaCHead and neck cancers in France: an analysis of the hospital medical information system (PMSI) databaseHead Neck Oncol201022220809978
- MenzinJLinesLMManningLNThe economics of squamous cell carcinoma of the head and neckCurr Opin Otolaryngol Head Neck Surg2007152687317413405
- ParkinDMBrayFChapter 2: The burden of HPV-related cancersVaccine200624Suppl 3S3/112516949997
- FerlayJShinHRBrayFFormanDMathersCParkinDMGLOBOCAN 2008 v 1.2, cancer incidence and mortalityworldwide in 2008: IARC CancerBase No 10 [web page on the Internet]LyonInternational Agency for Research on Cancer2010 Available from: http://globocan.iarc.frAccessed April 27, 2012
- World Health Organization (WHO)International Classification of Diseases 10th revisionGenevaWHO1990
- Robert Koch Institute, Society of Cancer Registries in GermanyKrebs in Deutschland 2007/2008Cancer in Germany 2007/2008BerlinRobert Koch Institute, Society of Cancer Registries in Germany2012 German
- KlussmannJPWeissenbornSJWielandUPrevalence, distribution, and viral load of human papillomavirus 16 DNA in tonsillar carcinomasCancer200192112875288411753961
- KreimerARCliffordGMBoylePFranceschiSHuman papillomavirus types in head and neck squamous cell carcinomas worldwide: a systematic reviewCancer Epidemiol Biomarkers Prev200514246747515734974
- Guntinas-LichiusOWendtTBuentzelJThuringian Head and Neck Cancer Study GroupHead and neck in situ carcinoma: survival analysis of the Thuringian cancer registration databaseOral Oncol2010464e5e920227329
- Guntinas-LichiusOWendtTBuentzelJHead and neck cancer in Germany: a site-specific analysis of survival of the Thuringian cancer registration databaseJ Cancer Res Clin Oncol20101361556319568769
- LeeJMTuriniMBottemanMFStephensJMPashosCLEconomic burden of head and neck cancer. A literature reviewEur J Health Econ200451708015452768
- PetermanACellaDGlandonGDobrezDYountSMucositis in head and neck cancer: economic and quality-of-life outcomesJ Natl Cancer Inst Monogr200129455111694566
- van AgthovenMvan IneveldBMde BoerMFThe costs of head and neck oncology: primary tumours, recurrent tumours and long-term follow-upEur J Cancer200137172204221111677108
- EkwuemeDUChessonHWZhangKBBalamuruganAYears of potential life lost and productivity costs because of cancer mortality and for specific cancer sites where human papillomavirus may be a risk factor for carcinogenesis-United States, 2003Cancer2008113Suppl 102936294518980277
- HuDGoldieSJThe economic burden of noncervical human papillomavirus disease in the United StatesAm J Obstet Gynecol20081985500. e1e718455524
- Federal Statistical Office GermanyTiefgegliederte Diagnosedaten der Krankenhauspatientinnen und -patienten 2008Deeply structured diagnostic data of hospital patients 2008Federal Statistical Office GermanyWiesbaden, Germany2009 Available from: https://www-ec.destatis.deAccessed January 4, 2011 German
- Institute for the Hospital Remuneration System in GermanyGDRGBrowser_2008_Par21_100202.zip (G-DRG V2009 Daten 2008 gem. § 21 KHEntgG – G-DRG Browser) 2010Editor Institute for the Hospital Remuneration System in GermanySiegburg, Germany2010 Available from: http://www-g-drg.deAccessed March 15, 2010 German
- German Public Pension InsuranceStatistik der Deutschen Rentenversicherung. Band 174. Rehabilitation 2008Statistics of the German Public Pension Insurance. Volume 174. Rehabilitation 2008BerlinGerman Public Pension Insurance2009 German
- Federal Health Monitoring GermanyArbeitsunfähigkeit bei AOK-Mitgliedern ohne Rentner. Jahr 2008: Arbeitsunfähigkeitsfälle, Arbeitsunfähigkeitstage, Tage je Fall (Gliederungsmerkmale: Jahre, Deutschland, Geschlecht, ICD-10)Inability to work of compulsory members of the Local Statutory Health Insurance (AOK) without pensioners (cases and days of inability to work, days of inability to work per 100,000 compulsory members, days per case). Classification: years, Germany, sex, ICD-10Federal Health Monitoring Germany2008Editor Federal Statistical Office Germany, Branch BonnBonn, Germany2010 Available from: http://www.gbe-bund.de/oowa921-install/servlet/oowa/aw92/dboowasys921.xwdevkit/xwd_init?gbe.isgbetol/xs_start_neu/&p_aid=3&p_aid=91546134&nummer=683&p_sprache=D&p_indsp=-&p_aid=70513394Accessed December 7, 2010 German
- German Federal Ministry of HealthMitgliederstatistik KM6 2008Membership statistics KM6 2008German Federal Ministry of Health2008Bonn Available from: http://www.bmg.bund.de/fileadmin/redaktion/excel_statistiken/krankenversicherung/KM6-juli-08.xlsAccessed January 11, 2011 German
- PlatzerHZukünftige Vergütungsstrukturen der KrankenhäuserFuture remuneration structures of hospitalsMunichAOK Bavaria2008 Available from: http://www.oberender-online.de/fileadmin/oberender/pdf/Platzer_ExpertentagungUniBayreuth_08052008.pdfAccessed December 12, 2011 German
- von der SchulenburgJMPrenzlerASchurerWCancer management and reimbursement aspects in Germany: an overview demonstrated by the case of colorectal cancerEur J Health Econ201010 Suppl 1S21S2620012133
- Graf von der SchulenburgJMGreinerWJostFHanover Consensus GroupGerman recommendations on health economic evaluation: third and updated version of the Hanover ConsensusValue Health200811453954418194408
- Federal Statistical Office GermanyStatistical Yearbook 2010 for the Federal Republic of Germany including International TablesWiesbadenFederal Statistical Office Germany2010 German
- SchneeMSozioökonomische Strukturen und Morbidität in den gesetzlichen KrankenkassenSocioeconomic structures and morbidity in the Statutory Health Insurance fundsBöckenJBraunBAmhofRGesundheitsmonitor 2008Health monitor 2008GüterslohVerlag Bertelsmann Stiftung200888104 German
- Federal Health Monitoring GermanyArbeitsunfähigkeit bei AOK-Mitgliedern ohne Rentner. Jahr 2008: Arbeitsunfähigkeitstage, Arbeitsunfähigkeitsfälle, Tage je Fall (Gliederungsmerkmale: Jahre, Kassenart, Versichertengruppe)Disability at AOK members excluding pensioners. 2008 lost work days, disability cases, days per case (Classification: years, statutory health insurance group)Federal Health Monitoring Germany2008Editor Federal Statistical Office Germany, Branch BonnBonn, Germany2010 Available from: http://www.gbe-bund.deAccessed January 22, 2011 German
- Federal Health Monitoring GermanyArbeitsunfähigkeit bei Mitgliedern der gesetzlichen Krankenkassen insgesamt ohne Rentner. Jahr 2008: Arbeitsunfähigkeitstage, Arbeitsunfähigkeitsfälle, Tage je Fall (Gliederungsmerkmale: Jahre, Kassenart, Versichertengruppe)Inability to work: days and cases of inability to work of the members of the Statutory Health Insurance (number and rate). Classification: years, sex, type of statutory health insurance organization, group of people insuredFederal Health Monitoring Germany2008Editor Federal Statistical Office Germany, Branch BonnBonn, Germany2010 Available from: http://www.gbe-bund.de/oowa921-install/servlet/oowa/aw92/dboowasys921.xwdevkit/xwd_init?gbe.isgbetol/xs_start_neu/&p_aid=i&p_aid=60283303&nummer=267&p_sprache=D&p_indsp=-&p_aid=86537257Accessed January 22, 2011 German
- German Public Pension InsuranceStatistik der Deutschen Rentenversicherung. Band 173. Rentenzugang 2008Statistics of the German Public Pension Insurance. Volume 173. Retirement 2008BerlinGerman Public Pension Insurance2009 German
- BrechtJGPoldrugoFSchädlichPKAlcoholism. The cost of illness in the Federal Republic of GermanyPharmacoeconomics199610548449310163630
- BrechtJGSchädlichPKBurden of illness imposed by osteoporosis in GermanyEur J Health Econ2000112632
- SchädlichPKBrechtJGBurden of illness imposed by venous thromboembolism as an original disease in GermanyPerfusion200316250256
- FranzDRoederNHörmannKAlbertyJENT medicine and head and neck surgery in the G-DRG system 2008HNO2008569874880 German18696019
- SculpherMJSargeantIRLoizouLAThorpeSMSpencerGMBownSGA cost analysis of Nd:YAG laser ablation versus endoscopic intubation for the palliation of malignant dysphagiaEur J Cancer199531A10164016467488416
- GoonPKStanleyMAEbmeyerJHPV and head and neck cancer: a descriptive updateHead Neck Oncol200913619828033
- NäsmanAAttnerPHammarstedtLIncidence of human papillomavirus (HPV) positive tonsillar carcinoma in Stockholm, Sweden: an epidemic of viral-induced carcinoma?Int J Cancer2009125236236619330833
- ChaturvediAKEngelsEAAndersonWFGillisonMLIncidence trends for human papillomavirus-related and -unrelated oral squamous cell carcinomas in the United StatesJ Clin Oncol200826461261918235120
- AOK-Health PartnerGermany-wide average base rate in 2011Editor AOK-BundesverbandBerlin Available from: http://www.aok-gesundheitspartner.de/bund/krankenhaus/lbfw/bfw/index_09446.htmlAccessed March 6, 2013 German
- German Public Pension InsuranceStatistik der Deutschen Rentenversicherung. Band 189. Rehabilitation 2011Statistics of the German Public Pension Insurance. Volume 189. Rehabilitation 2011BerlinGerman Public Pension Insurance2012 German
- Federal Statistical Office GermanyStatistical Yearbook Germany and International 2012WiesbadenFederal Statistical Office Germany2012 German
- GiulianoARPalefskyJMGoldstoneSEfficacy of quadrivalent HPV vaccine against HPV Infection and disease in malesN Engl J Med2011364540141121288094