Abstract
Objective
This study aims to estimate the direct medical cost of COVID-19 hospitalizations and to utilize prevalence estimates from Jaber Al-Ahmad Hospital to estimate the direct medical cost of all hospitalized adult patients in Kuwait using a decision tree analysis.
Methods
A cost-of-illness model was developed. The Ministry of Health perspective was considered, direct medical costs were estimated from July 1st to September 30th, using a bottom-up approach. The mean cost per hospitalized patient was estimated using a decision analysis model. Prevalence estimates of ambulance use, use of ER, ICU admission, and mortality were considered in the current study. Patients aged 18 years and above with a confirmed diagnosis of COVID-19 were included. One-way sensitivity analysis and probabilistic sensitivity analysis (PSA) were performed.
Results
Data for 2986 patients were analyzed. The mean age was 61 (SD= 11) years old. Most of the patients were Kuwaiti (2864, 95.91%), and more than half were females (1677, 56.16%). Of the total hospital admissions, 417 patients (14%) were admitted to the ICU. The average length of the hospital stay was 11 (SD= 9) days, and among all hospital admissions, 270 (9.04%) patients died. The total estimated direct medical cost of hospitalized patients at Jaber Al-Ahmad Hospital was $47,213,768 (14,283,203.6 KD). The average cost of hospital stay per patient was estimated at $15,498 (4,688.60 KD). The weighted average cost per hospitalized patient in Kuwait was estimated at $16,373 (4,953.08 KD). The total direct medical cost of hospitalized COVID-19 patients in Kuwait during the study period was estimated at $174,372,450 (52,751,502 KD).
Conclusion
The COVID-19 pandemic constituted a significant burden on the Kuwaiti healthcare system. The findings of this study urge the need for preventive care strategies to reduce adverse health outcomes and the economic impact of the pandemic.
Introduction
Since late 2019, almost every country worldwide has been affected by coronavirus disease 2019 (COVID-19). On February 24, 2020, the Kuwaiti government reported the first case of COVID-19 in Kuwait. The first wave of the pandemic extended from March 2020 to January 2021, followed by a shorter second wave from March to April 2021. According to the latest statistics, around 667,290 COVID-19 cases and more than 2,570 deaths were reported in Kuwait by August 2023.Citation1
Kuwait has a well-developed and modern healthcare system, providing accessible and comprehensive healthcare services to its citizens and residents. The healthcare system is predominantly government-funded and operated by the Ministry of Health (MOH). Healthcare services are free to citizens and heavily subsidized for legal residents. In addition to the public healthcare system, Kuwait has a private healthcare sector that provides healthcare services to those who can afford private healthcare facilities.
At the beginning of the COVID-19 crisis, the Kuwaiti MOH policy required hospital admission of every suspected COVID-19 patient to Jaber Al-Ahmad Hospital, a general governmental hospital. However, with the accelerated numbers of infected people, the policy was changed to admit only confirmed cases of COVID-19 who required hospital care. Jaber Al-Ahmad Hospital was then dedicated mostly to Kuwaiti COVID-19 patients.
The COVID-19 pandemic has had a profound economic impact on healthcare systems worldwide. The wide spread of the infection, the increased number of patients, and the serious complications of COVID-19 have intensified healthcare resources and resulted in a catastrophic increase in healthcare costs.Citation2 According to the American Hospital Association, the economic impact of COVID-19 on America’s hospitals and healthcare systems is over $202.6 billion.Citation3
The direct medical costs, including hospitalization costs, constitute a large portion of the total economic impact of the COVID-19 pandemic. Several studies found that COVID-19 was associated with high rates of admission and extensive hospital resource utilization.Citation2,Citation4,Citation5 According to Moon et al, about one in every five COVID-19 admissions was transferred to the intensive care unit (ICU) and required special care services.Citation6 Generally, the overall cost of treating a patient in the ICU is significantly higher compared to that in general wards.Citation2 In the literature, several studies from different countries focused on the economic impact of hospitalized patients with COVID-19. According to a study done in Singapore, the cost associated with hospitalized patients with COVID-19 was substantially higher with an approximate value of $41.96 million.Citation7 A study done in the US found that the mean cost per hospitalization for a COVID-19 patient was $21,752, which is higher than costs associated with comparable health conditions such as influenza and pneumonia.Citation8 Another US study compared direct medical costs between patients with COVID-19 and non-COVID patients and found that COVID patients had higher costs compared to non-COVID patients due to higher rates of hospitalization and complications related to COVID-19.Citation9 Looking at the Gulf area, there was a study that assessed the economic impact of COVID-19 in Saudi Arabia and found that hospitalization cost associated with treating COVID-19 patients is considered a significant burden on the healthcare system.Citation5
Like other healthcare systems, the MOH in Kuwait has incurred the cost of treating COVID-19 patients. Various studies have looked at patient characteristics and clinical outcomes associated with COVID-19 patients and the epidemiology of the epidemic in Kuwait.Citation10–14 Three studies have evaluated the economic impact of COVID-19 in Kuwait. The first study by NUR et al estimated the total cost of COVID-19 to be $488.5 (147.4 KD) million in 2021; this cost included costs on the healthcare system and patient costs due to loss of productivity.Citation15 A second earlier study by the same authors focused on the direct medical cost of treating COVID-19 at a general hospital in Kuwait.Citation16 The total treatment cost of admitted patients was estimated at $3,561,585 (1,074,644 KD). The last study by Abuhadida et al estimated the direct medical cost of COVID-19 patients admitted to intensive care units at the Ministry of Health affiliated hospitals. Over one year (April 2020 – March 2021), the total cost was reported to be $52,125,774 (15,795,689 KD).Citation17
Understanding the economic impact of COVID-19 on the healthcare system is crucial as it provides a comprehensive understanding of the pandemic’s effects, informed policymaking, efficient resource allocation, and ensuring a sustainable and resilient healthcare system for the future. Identifying major cost components of COVID-19 helps to plan for future prevention and treatment strategies. This allows for better preparedness and resilience against future pandemics or health crises. Furthermore, estimating the cost of COVID-19 will guide policymakers to develop strategic plans to optimize budgets and resource allocation. Moreover, the estimated cost of the COVID pandemic can be used as input to evaluate the cost-effectiveness of different COVID-19 vaccines and to better equip decision-makers to implement the most effective treatment intervention.
There are several strategies through which healthcare systems can reduce the cost of future pandemics while maintaining the quality of healthcare services. First, is the use of telemedicine for providing healthcare services to reduce in-person visits. The second is to promote preventive measures such as vaccines. Third, government healthcare sectors may collaborate with the private sector for the production and distribution of medical supplies. Finally, is the use of value-based healthcare which is an efficient strategy for allocating healthcare resources.
This study aims to estimate the economic impact of COVID-19 among hospitalized patients in Kuwait considering a healthcare perspective. Specifically, the study aims to estimate the direct medical cost of COVID-19 hospitalizations at Jaber Al-Ahmad Hospital. This study also aims to utilize prevalence estimates from Jaber Al-Ahmad Hospital to estimate the direct medical cost of all hospitalized patients in Kuwait using a decision tree analysis.
Methods
Study Design
A cost-of-illness model was developed using data from Jaber Al-Ahmad Hospital and the MOH in Kuwait (). Jaber Al-Ahmad Hospital is the largest tertiary public hospital in Kuwait. It was operated in 2019 with a capacity of 1200 beds. The hospital provides a wide range of diagnostic and medical services for inpatients and outpatients including trauma centers, casualty services, dental services, and obstetrics and gynecology services. During the COVID-19 crisis, Jaber Al-Ahmad Hospital became the nationally designated COVID center and was operated at its highest capacity, including 28 wards with 50 beds each, and eight ICUs with 20 beds each. During the data collection period (July 1st -September 30th), only COVID-19 patients were admitted to Jaber Al-Ahmad Hospital. In addition, admissions were mostly for Kuwaiti patients. The MOH perspective was considered. In the model, direct medical costs of hospitalized patients with COVID-19 were investigated, which is the cost that is directly related to the provision of care. Indirect and intangible costs were not considered. Direct medical costs of hospitalized patients were estimated over three months using a bottom-up approach. All cost estimates were converted to 2021 values by applying the US yearly healthcare inflation rate. Prevalence estimates of using an ambulance, use of ER, ICU admission, and mortality were considered in the current study.
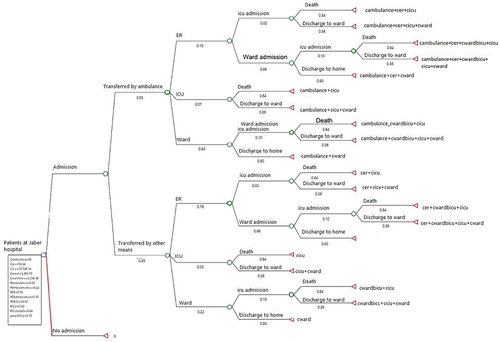
Figure 1 Decision tree model with assigned outcome probabilities and cost variables. Outcomes that do not represent cost are assigned zero values. Arrow represents point where average weighted cost per hospitalized COVID-19 patient is estimated.
Study Population
Adult patients aged 18 years and above with a confirmed diagnosis of COVID-19 were included in this study. Both genders and all nationalities were included. Adult patients admitted and discharged on the same day were excluded.
Economic Model
Direct medical costs associated with hospitalized COVID-19 patients were identified at the following points:
The patient is transferred by an ambulance.
The patient is seen in the ER.
The patient is admitted to the ward or ICU.
Model Assumptions
The model was built on the following assumptions:
A patient is admitted once to the ICU during the hospital stay.
A patient who is discharged to the ward will be discharged to home alive. The average length of ward stay after ICU discharge was assumed to be the same as the average length of ward stay before ICU admission, which was calculated to be 6 days based on the given hospital data.
A patient who was admitted to the ward and then transferred to the ICU will be assigned a different cost than a patient admitted only to the ward. This is because the average length of stay in the ward before admission to ICU is shorter than the average length of stay in the ward without ICU admission.
A patient who is admitted and discharged on the same day is excluded from the model.
A three-month (July 1st – September 30th) period was the time frame of the study.
All patients transferred from other healthcare facilities were transferred by ambulance.
Data Sources
Prevalence Estimates
All prevalence estimates were calculated using real patient data from Jaber Al-Ahmad Hospital electronic medical records (EMRs). During the COVID-19 outbreak in Kuwait, Jaber Al-Ahmad Hospital was the nationally designated COVID center and was operated at its full capacity. Thus, data obtained from the hospital represent the COVID-19 population in Kuwait. In addition, it is the only public hospital in Kuwait that has EMRs. The EMRs include information on patients who were admitted to the hospital. The authors did not have access to information that could identify individual participants during or after data collection. The data collection period was from July 1st to September 30th, 2020. The following prevalence estimates were calculated:
Rate of patients transferred to the hospital by ambulance.
Rate of using the ER.
Rate of ICU admission.
Rate of ward admission.
Mortality rate during hospital stay.
Cost Data
The cost of hospital stay is obtained from a book published by the Kuwaiti MOH.Citation18 The book “cost analysis and performance evaluation for government health services” has estimates on the average cost of inpatient stays and outpatient visits for all public hospitals except Jaber Al-Ahmad Hospital. The latter is the newest public hospital in Kuwait with an expected high operational cost. In Kuwait, there are six tertiary public hospitals with different costs per hospital night due to the variability in the number of working staff, quality of services, and medical devices. To substitute for the unavailable cost data of Jaber Al-Ahmad Hospital, cost data from Al-Amiri Hospital was used. Among the six hospitals, Al-Amiri Hospital has the highest average cost per ICU/ward night and thus, it best represents the cost at Jaber Al-Ahmad Hospital. The last version of the book for the year 2016–2017 is used for the current study. The book provides the average cost per hospital night in ICUs and wards for each public hospital. The estimated average cost considers various cost elements including staff salaries, drugs, lab tests, radiology, food, and other consumables. For example, if the cost per ICU night is $1,322.22 (400 KD) in one public hospital, this number would include in its estimation the cost of all the previously mentioned elements. In addition, the cost per ER visit is calculated using the same method. The average cost per ambulance run was obtained from experts in the MOH. Patients whose data were not available were excluded from descriptive, outcome, and cost analyses. summarizes the variables used for the cost analysis.
Table 1 Summary of the Cost Variables Used for the Cost Analysis
Cost Calculation
Overall Cost of Hospitalized COVID-19 Patients in Kuwait
A prevalence-based method was used to estimate the economic burden of hospitalized COVID-19 patients. In this method, the prevalence of hospitalized COVID-19 patients during a specific period (three months) was measured and assigned a cost using a bottom-up approach. In this approach, the mean cost per unit (ie, patient) is calculated and multiplied by the total number of units (ie, patients). All cost estimates were converted to 2021 US dollar value.
Data Analysis
The data analysis is divided into three parts. First, descriptive statistics were used to present the sociodemographic and clinical characteristics of the study participants. Categorical variables were measured as percentages and frequencies; continuous variables were expressed as mean and standard deviation. In the second part, the direct medical costs of hospitalized patients at Jaber Al-Ahmad Hospital were estimated over the study period. The average cost for each patient was measured and summed to obtain the total cost for all patients at the hospital (ie, a bottom-up approach). This was done using the following steps:
Calculate the length of hospital stay (ICU or ward) for each patient.
Multiply the average cost per hospital night per patient by length of hospital stay.
Add the cost of the following when applicable:
Average cost per ambulance run
Average cost per ER visit
Add the cost for all patients to obtain the total direct medical cost.
Also, the hospitalization cost for COVID-19 patients was categorized based on the level of care. Using the physician’s opinion, three stages of care were identified based on the severity of the patient’s condition. Stage 1 includes patients who are on room air. Stage 2 includes patients who use oxygen starting from 1 liter to 15 liters and those on high-flow nasal cannula (HFNC). Stage 3 includes patients on Continuous positive airway pressure (CPAP), bilevel positive airway pressure (BiPAP), mechanical ventilation (MV), and extracorporeal membrane oxygenation (ECMO). Parts 1 and 2 of the data analysis were done using Excel App.
The third part and primary analysis of this study was done by decision analysis modeling. The TreeAge Pro Healthcare 2022 software was used for data analysis. A decision tree was built (see : Decision tree model with assigned outcome probabilities and cost variables) mapping out the possible outcomes of COVID-19 patients admitted to the hospital and assigning probabilities that each outcome (mortality, discharge to ward, discharge to home) will occur as well as its average cost (in US dollar). The following patients’ pathways are illustrated by the decision tree:
The patient is transferred by ambulance, presented to the ER, and admitted to the ICU, followed by either patient death or discharge to the ward.
The patient is transferred by ambulance, presented to the ER, and admitted to the ward, followed by either ICU admission or discharge to home.
The patient is transferred by ambulance and directly admitted to the ICU, followed by either patient death or discharge to the ward.
The patient is transferred by ambulance and directly admitted to the ward, followed by either ICU admission or discharge to home.
For patients who are not transferred by the ambulance (ie transferred by other means), pathways (1–4) are followed.
A folding back technique was used to estimate the expected value (weighted average cost) per hospitalized patient. This technique works by multiplying the probability that each outcome will occur by its cost, and it starts from the right side of the decision tree (: Decision tree model with assigned outcome probabilities and costs variables) and works leftward. The mean cost per hospitalized patient was also provided at terminal nodes (indicated by triangles at the end of the tree).
Sensitivity Analysis
One-way sensitivity analysis and probabilistic sensitivity analysis (PSA) were performed for the decision tree analysis using the TreeAge software. For the one-way sensitivity analysis, ±20% range was used. These sensitivity analyses aimed to test the robustness of the estimated average cost of hospitalized COVID-19 patients. This is due to uncertainties in the selected parameter estimates, such as cost or probabilities of events. A tornado diagram was made to illustrate the sensitivity of the estimated cost to the variables used in the model.
Ethics statement: This study was approved by the Permanent Committee for Coordination of Medical and Health Research at the Ministry of Health (approval number: 1596/2020), and the Health Science Center ethics committee (approval was sent via e-mail on 5/5/2020). No informed consent was needed for this study.
Results
Part 1: Study Sample and Descriptive Statistics
During the study period, 3895 patients with confirmed COVID-19 infection were admitted to Jaber Al-Ahmad Hospital. Thirty-two (0.82%) patients were admitted and discharged on the same day and were excluded from the data analysis. Data for the remaining 3863 patients were investigated. Data were available for 2986 patients who represent the final sample size. The mean age was 61 (SD= 11) years old. Most of the patients were Kuwaiti (2864, (95.91%)), and more than half were female (1677, (56.16%)). Almost all admitted patients were diagnosed with pneumonia. Admitted cases were either severe or moderate as indicated by X-ray, oxygen saturation (spo2), and the need for ICU admission. Most cases (2916, (97.66%)) were moderate. Of the total hospital admissions, 417 patients (14%) were admitted to the ICU and spent an average of 18 (SD= 12.61) days. Hospital mortality was 9.04% (270 patients) while ICU mortality was 63.79% (266 patients). summarizes the sociodemographic and clinical characteristics of the study participants. Common comorbidities among the study population were investigated. The most common first comorbidities were diabetes mellitus (1515, (52.21%)) followed by hypertension (994, (34.25%)) ().
Table 2 Socio-Demographic and Clinical Characteristics of Hospitalized COVID-19 Patients
Table 3 Common Comorbidities Among Hospitalized COVID-19 Patients
Part 2: Cost Analysis (Estimating the Direct Medical Cost of Hospitalized Patients at Jaber Al-Ahmad Hospital)
Over the study period (July 1st – September 30th), the total estimated direct medical cost of hospitalized patients at Jaber Al-Ahmad Hospital was $47,213,768 (14,283,203.60 KD). This included the cost of hospital stay, use of ER, and ambulance runs. The estimated total inpatient stay cost was $46,278,151 (14,000,158.84 KD). More than two-thirds of the total cost was attributed to ward admissions (69.17%), and almost one-third were related to ICU admissions (30.82%). The average length of stay in ICU was 18 (SD= 12.61) days compared to 9 (SD= 5) days in ward admissions only. The average cost of hospital stay per patient was estimated at $15,498 (4,688.60 KD) at Jaber Al-Ahmad Hospital. The average cost per hospital stay in the ICU and ward was $35,482 (10,734.01 KD) and $11,115 (3,362.65 KD) respectively. . Summarizes the breakdown of the estimated hospitalization costs among COVID-19 hospitalized patients at Jaber Al-Ahmad Hospital. The estimated total inpatient costs by the severity of the patient’s condition are summarized in .
Table 4 Estimated Direct Medical Costs of Hospitalized COVID-19 Patients at Jaber Al-Ahmad Hospital
Table 5 Total Inpatient Costs by Severity of Patient Condition
Part 3: Decision Tree Analysis
Base Case Analysis
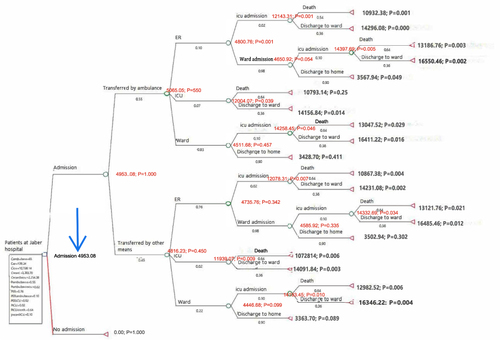
Data were analyzed by decision analysis modeling and the base case results are shown in (: Base case results using decision analysis modeling). The weighted average cost per hospitalized patient in Kuwait was estimated at $16,373 (4,953.08 KD). During the study period, there were an estimated number of 10,650 COVID-19 patients who were admitted to different hospitals in Kuwait. Thus, the total direct medical cost of hospitalized COVID-19 patients in Kuwait during the study period is 10,650 x $16,373= $174,372,450 (52,751,502 KD). summarizes the prevalence estimates used in the decision tree analysis. The prevalence estimates were obtained by analyzing data from patients at Jaber Al-Ahmad Hospital. Cost variables are presented in .
Table 6 Prevalence Estimates Used in the Decision Tree Analysis
Figure 2 Base case results using decision analysis modeling. Outcomes that do not represent cost are assigned zero values. The arrow indicates the weighted average cost (in Kuwaiti dinar) per a hospitalized COVID-19 patient in Kuwait. 1 KD=3.22 US$ on Oct. 17, 2022.
Sensitivity Analysis
One-Way Sensitivity Analysis
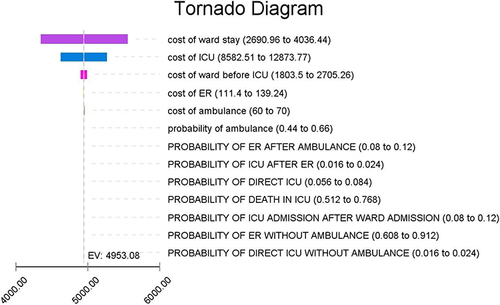
A Tornado diagram was created for one-way sensitivity analyses for all variables in the model (: One-way sensitivity analysis on all variables. Boxes represent range of values used in sensitivity analysis for each variable). The overall cost was most sensitive to the average cost of ward stay, the average cost of ICU stay, and the average cost of ward stay before ICU admission. Varying the average cost of ward stay over ±20% range resulted in approximately ± $1,983.33 (600 KD) effect on the overall estimated cost. When the mean ICU stay cost varied between $28,370 (8,582.51KD) and $42,555 (12,873.77KD), the total cost ranged from $163,046,155 (49,325,049 KD) to $185,690,809 (56,175,555 KD). The mean cost of ward stay before ICU admission had a minimal effect of ±$138.83 (42 KD) on the overall estimated cost.
Figure 3 One-way sensitivity analysis on all variables. Boxes represent range of values used in sensitivity analysis for each variable. ICU: intensive care unit, ER: emergency room, EV: expected value. EV= weighted average cost (in Kuwaiti dinar) per a hospitalized COVID-19 patient in Kuwait. All costs are represented in Kuwaiti Dinar. 1 KD=3.22 US$ on Oct. 17, 2022.
Probabilistic Sensitivity Analysis (Monte Carlo Simulation)
A probabilistic sensitivity analysis (PSA) was conducted using all the variables in the model. A Monte Carlo simulation was run for 10 thousand iterations giving an average expected cost per hospitalized COVID-19 patient of $16,355 (4,947.71 KD) (95% CI: $16,197 (4,899.85 KD) – $16,513 (4, 995.58KD)) and thus, an overall cost of $174,179,437 (52,693,111.5 KD) (95% CI: $172,494,571 (52,183,402.5 KD)– $175,864,654 (53,202,927 KD)) ().
Table 7 Results of Probabilistic Sensitivity Analysis (US$ (KD) 2021 Values)
Discussion
This study evaluates the economic impact of COVID-19 on the Kuwaiti healthcare system. It quantifies the direct medical costs associated with COVID-19 hospitalizations at Jaber Al-Ahmad Hospital. To the best of our knowledge, this is the first study in Kuwait that examines the direct medical costs associated with the COVID-19 epidemic. The costs estimated in this study were specific to hospitalization costs, ER visit costs, and ambulance run costs.
We found that the most common comorbidities among Kuwaiti patients were diabetes mellitus and hypertension, which supported findings from previous studies.Citation10,Citation12,Citation19 These comorbidities can significantly impact the economic burden and outcomes for individuals and the Kuwaiti healthcare system in the context of COVID-19.Citation20–22 COVID-19 patients with hypertension and diabetes often experience more severe symptoms and complications. This can lead to longer hospital stays, increased use of medical resources, and higher healthcare costs. Targeted public health strategies, early intervention, and proper management can help reduce the economic impact of such comorbidities.
The percentages of ICU admission and hospital mortality in our study were comparable to those reported by previous studies.Citation5,Citation10,Citation12,Citation19 The noted differences were not large and could be attributed to differences in the characteristics of the study population and the treatment protocol at the time of the study. Also, ICU mortality was similar in this study compared to existing studies. We found that 63.79% of patients admitted to ICU died compared to 56% and 68%; a higher percentage was reported by Alshukry et alCitation11,Citation23,Citation24 ICU admission and hospital mortality in COVID-19 patients significantly impact hospitalization costs due to the increased level of care, specialized interventions, prolonged stays, and the need for a comprehensive approach to managing severe cases. Efforts to enhance patient outcomes and optimize resource utilization are important in mitigating the economic burden on the Kuwaiti healthcare systems.
In our cohort, the average cost of ICU admission per patient was more than three times higher than general ward admission. These findings align with studies in other countries, where ICU costs incurred by the average patient were higher than general hospital admissions.Citation3–5,Citation25 The actual amounts estimates across studies varied, with some higher than the present study,Citation4,Citation25 and some lower,Citation3,Citation5 which may be explained by differences in treatment protocols, personnel cost, and rate of utilization of health resources.
Despite higher average costs associated with the ICU per patient, general ward admission was the largest contributor to the overall cost estimates. Understanding that ward admissions contribute significantly to the cost of COVID-19 hospitalization compared to ICU admissions can guide policymakers and healthcare systems to manage resources effectively and improve overall healthcare delivery. They can focus on enhancing capacity, staffing, and equipment for general wards to efficiently manage a larger number of patients. Also, healthcare systems can develop and implement cost-effective care models tailored to ward admissions to ensure that patients receive appropriate care while minimizing unnecessary costs.
In this research, a model was developed to map out all possible outcomes for a COVID-19 patient arriving at the hospital. While some studies relied on proxy diseases, such as pneumonia and influenza, to estimate costs related to COVID-19,Citation3,Citation23,Citation26–28 a decision tree model was used in the current study to identify points where costs are incurred and thus, mitigate future economic burden. Worldwide, the literature has evaluated the economic impact of the COVID-19 pandemic; however, none of the encountered studies has utilized decision tree modeling for this purpose.Citation3,Citation4,Citation23
This study used nationally representative data to estimate the total direct medical cost of hospitalized COVID-19 patients. Several studies in Kuwait have examined the epidemiological, clinical, and sociodemographic characteristics of COVID-19.Citation10–14 None of these studies has evaluated the cost of COVID-19.
In this study, the total estimated direct medical costs associated with hospitalized COVID-19 patients in Kuwait was $174,372,450 (52,751,502 KD). Estimating the cost of hospitalized COVID-19 patients in Kuwait can provide valuable insights for the healthcare system, policymakers, and stakeholders to optimize resource allocation, improve efficiency, and enhance the overall response to the pandemic. On the regional level, estimating the cost of hospitalized COVID-19 patients in Kuwait can promote collaboration, knowledge sharing, and unified efforts among Gulf countries. These collaborative initiatives can enhance healthcare systems, optimize resource allocation, and improve preparedness to address current and future healthcare challenges in the region.
This study has several limitations. The first is related to the specific types of costs we captured. We looked mainly at the hospitalization costs of COVID-19 patients. Other direct medical costs are related to the epidemic and were incurred by the MOH in Kuwait. These unaddressed costs include the cost of outpatient visits, cost of home visits, cost of building temporary COVID-19 hospitals, cost of COVID-19 testing, cost of vaccination, and other related medical costs.
Another limitation is that we were not able to obtain the inpatient cost from Jaber Al-Ahmad Hospital. Instead, we utilized cost data from another general hospital (Al-Amiri Hospital). This is because cost data for Jaber Al-Ahmad Hospital was not released by the MOH at the time of this study. The latest edition of the cost analysis book by the MOH was in 2017 when Jaber Al-Ahmad Hospital was not operating.Citation18
Also, we may underestimate the overall cost of hospitalized COVID-19 patients in Kuwait. This is because we used cost data from another hospital and for the time before the epidemic. Thus, special costs related to COVID-19 were not captured. These costs include the cost of overtime shifts for the healthcare team, the cost of personal protective equipment (PPE), the cost of COVID-19 tests, and other special costs.
Another limitation is related to the generalizability of the data. Prevalence estimates used in the decision tree modeling were obtained from patients at Jaber Al-Ahmad Hospital. At the time of the study, the hospital policy restricted the admission mostly to Kuwaiti patients. Thus, the prevalence estimates may not reflect all hospitalized COVID-19 patients in Kuwait.
The last limitation is related to the missing data. The EMRs at Jaber Al-Ahmad Hospital did not include information on 877 patients and these patients were excluded from the cost analysis. So, the cost of managing hospitalized COVID patients may be overestimated or underestimated. To overcome this issue, sensitivity analyses were performed to provide the reader with a possible range of the total estimated cost.
Further Studies
Future studies can focus on several areas to enhance the understanding of the economic impact of COVID-19 on the Kuwaiti healthcare system and society. A comprehensive cost analysis that investigates provider costs and indirect costs, such as loss of productivity, is recommended. Also, studying the economic impact of COVID-19 in the long term is advisable. This may include the cost of treating post-COVID conditions, vaccination costs, and other public health intervention costs. In addition, the Kuwaiti healthcare system needs studies that develop standardized methods for collecting and analyzing cost data related to COVID-19 and other diseases. Lastly, future studies may assess the cost and effectiveness of government policies that aim at mitigating the financial impact of COVID-19 on the healthcare system.
Conclusion
The COVID-19 epidemic constituted a significant burden on the Kuwaiti healthcare system. The direct medical cost of hospitalized patients was estimated in our study at more than $160 million (50 million KD). The findings of this study urge the need for future strategies to reduce the health impact of the epidemic and thus, minimize the economic burden on The Ministry of Health in Kuwait. The use of telemedicine and remote monitoring of mild patient cases is one way to reduce the spread of the infection and thus, manage the cost. In addition, public hospitals in Kuwait need to enhance the utilization of electronic medical records, this should save time and effort and minimize duplication of tests and procedures. Finally, the Ministry of Health in Kuwait should invest in research to support the implementation of value-based healthcare, which aims at reducing costs and optimizing patient outcomes.
Data Ethical Consideration
Patient data used in this study was anonymized, hence, no informed consent was needed.
Disclosure
The authors report no conflicts of interest in this work.
Additional information
Funding
References
- World Health Organization COVID-19 Dashboard; Geneva2020. Available from: https://covid19.who.int/. Accessed June 27, 2024.
- Ghaffari Darab M, Keshavarz K, Sadeghi E, et al. The economic burden of coronavirus disease 2019 (COVID-19): evidence from Iran. BMC Health Serv Res. 2021;21(1):132. doi:10.1186/s12913-021-06126-8
- Kaye AD, Okeagu CN, Pham AD, et al. Economic impact of COVID-19 pandemic on healthcare facilities and systems: international perspectives. Best Pract Res Clin Anaesthesiol. 2021;35(3):293–306.
- Di Fusco M, Shea KM, Lin J, et al. Health outcomes and economic burden of hospitalized COVID-19 patients in the United States. J Medl Eco. 2021;24(1):308–317. doi:10.1080/13696998.2021.1886109
- Khan AA, AlRuthia Y, Balkhi B, et al. Survival and estimation of direct medical costs of hospitalized COVID-19 Patients in the Kingdom of Saudi Arabia. Int J Environ Res Public Health. 2020;17(20):7458. doi:10.3390/ijerph17207458
- Moon R, Brown H, Rosenthal N. Healthcare resource utilization of patients with COVID-19 Visiting US Hospitals. Value Health. 2022;25(5):751–760. doi:10.1016/j.jval.2021.12.005
- Cai Y, Kwek S, Tang SSL, et al. Impact of the COVID-19 pandemic on a tertiary care public hospital in Singapore: resources and economic costs. J Hosp Infect. 2022;121:1–8. doi:10.1016/j.jhin.2021.12.007
- Tsai Y, Vogt TM, Zhou F. Patient characteristics and costs associated with COVID-19-related medical care among medicare fee-for-service beneficiaries. Ann Intern Med. 2021;174(8):1101–1109. doi:10.7326/M21-1102
- DeMartino JK, Swallow E, Goldschmidt D, et al. Direct health care costs associated with COVID-19 in the United States. J Manag Care Spec Pharm. 2022;28(9):936–947. doi:10.18553/jmcp.2022.22050
- Hamadah H, Alahmad B, Behbehani M, et al. COVID-19 clinical outcomes and nationality: results from a Nationwide registry in Kuwait. BMC Public Health. 2020;20(1):1384. doi:10.1186/s12889-020-09490-y
- Alkhamis M A, Al Youha S, Khajah M M, et al. Spatiotemporal dynamics of the COVID-19 pandemic in the State of Kuwait. Inter J Infect Dis. 2020;98(98):153–160. doi:10.1016/j.ijid.2020.06.078
- Alshukry A, Ali H, Ali Y, et al. Clinical characteristics of coronavirus disease 2019 (COVID-19) patients in Kuwait. PLoS One. 2020;15(11):e0242768. doi:10.1371/journal.pone.0242768
- Alsairafi Z, Naser AY, Alsaleh FM, et al. Mental health status of healthcare professionals and students of health sciences faculties in Kuwait during the COVID-19 Pandemic. Int J Environ Res Public Health. 2021;18(4):2203. doi:10.3390/ijerph18042203
- Salman A, Sigodo KO, Al-Ghadban F, et al. Effects of COVID-19 lockdown on physical activity and dietary behaviors in Kuwait: A Cross-sectional study. Nutrients. 2021;13(7):2252. doi:10.3390/nu13072252
- Nur AM, Aljunid SM, Almari M. The Economic Burden of the COVID-19 Pandemic in State of Kuwait. Clinicoecon Outcomes Res. 16:111–122. doi:10.2147/CEOR.S442913
- Nur AM, Aljunid SM, Almari M. Cost of in-patient management of COVID-19 patients in a general hospital in Kuwait. BMC Health Serv Res. 23(1):1314. doi:10.1186/s12913-023-10287-z
- buhadida S, Alzaid S, Elshazeley M, et al. financial burden and average cost of covid-19 per patient admitted to the intensive care unit in Kuwait. Ann Public Health. 2022;1:663.
- Ministry of Health. Cost Analysis and Performance Evaluation for Government Health. Kuwait: Budget and Control Department - Cost Accounting Section; 2017.
- Ansari KA, Alwazzeh MJ, Alkuwaiti FA, et al. Early determinants of mortality in hospitalized covid-19 patients in the eastern province of Saudi Arabia. Int J Gen Med. 2022;15:1689–1701. doi:10.2147/IJGM.S349598
- Russell CD, Lone NI, Baillie JK. Comorbidities, multimorbidity and COVID-19. Nat Med. 2023;29(2):334–343. doi:10.1038/s41591-022-02156-9
- Singh AK, Misra A. Impact of COVID-19 and comorbidities on health and economics: focus on developing countries and India. Diabetes Metab Syndr. 2020;14(6):1625–1630. doi:10.1016/j.dsx.2020.08.032
- Zidan N, Dey V, Allen K, et al. Understanding comorbidities and health disparities related to COVID-19: a comprehensive study of 776936 cases and 1362545 controls in the state of Indiana, USA. JAMIA Open. 2023;6(1):ooad002. doi:10.1093/jamiaopen/ooad002
- Lone SA, Ahmad A. COVID-19 pandemic - an African perspective. Emerg Microbes Infect. 2020;9(1):1300–1308. doi:10.1080/22221751.2020.1775132
- Sadeghi A, Eslami P, Dooghaie Moghadam A, et al. COVID-19 and ICU admission associated predictive factors in Iranian patients. Caspian J Intern Med. 2020;11(Suppl 1):512–519. doi:10.22088/cjim.11.0.512
- Shrestha S, Kompaniyets L, Grosse SD, et al. Estimation of coronavirus disease 2019 hospitalization costs from a large electronic administrative discharge database, March 2020-July 2021. Open Forum Infect Dis. 2021;8(12):ofab561. doi:10.1093/ofid/ofab561
- Campbell JD, Whittington MD, Rind DM, Pearson SD alternative pricing models for remdesivir and other potential treatments for covid-19; updated report. institute for clinical and economic review; 2020.
- FAIR Health. The projected economic impact of the COVID-19 pandemic on the US healthcare system; 2020.
- Bartsch SM, Ferguson MC, McKinnell JA, et al. The potential health care costs and resource use associated with COVID-19 in the United States. Health Aff. 2020;39(6):927–935. doi:10.1377/hlthaff.2020.00426
