?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
There is a paucity of preference-based (utility) measures of health-related quality of life for patients with ischemic heart disease (IHD); in contrast, the Seattle Angina Questionnaire (SAQ) is a widely used descriptive measure. Our objective was to perform a systematic review of the literature to identify IHD studies reporting SAQ scores in order to apply a mapping algorithm to convert these to preference-based scores for secondary use in economic evaluations.
Methods
Relevant articles were identified in MEDLINE (Ovid), EMBASE (Ovid), Cochrane Library (Wiley), HealthStar (Ovid), and PubMed from inception to 2012. We previously developed and validated a mapping algorithm that converts SAQ descriptive scores to European Quality of Life-5 Dimensions (EQ-5D) utility scores. In the current study, this mapping algorithm was used to estimate EQ-5D utility scores from SAQ scores.
Results
Thirty-six studies met the inclusion criteria. The studies were categorized into three groups, ie, general IHD (n=13), acute coronary syndromes (n=4), and revascularization (n=19). EQ-5D scores for patients with general IHD were in the range of 0.605–0.843 at baseline, and increased to 0.649–0.877 post follow-up. EQ-5D scores for studies of patients with recent acute coronary syndromes increased from 0.706–0.796 at baseline to 0.795–0.942 post follow-up. The revascularization studies had EQ-5D scores in the range of 0.616–0.790 at baseline, and increased to 0.653–0.928 after treatment; studies that focused only on coronary artery bypass grafting increased from 0.643–0.788 at baseline to 0.653–0.928 after grafting, and studies that focused only on percutaneous coronary intervention increased in score from 0.616–0.790 at baseline to 0.668–0.897 after treatment.
Conclusion
In this review, we provide a catalog of estimated health utility scores across a wide range of disease severity and following various interventions in patients with IHD. Our catalog of EQ-5D scores can be used in IHD-related economic evaluations.
Introduction
Economic evaluations with cost-effectiveness analyses are important in the decision-making process for health resource allocation. Cost-effectiveness analysis involves estimation of the incremental cost of a new intervention as well as its incremental net health benefit, in comparison with a reference. To facilitate the comparison of different interventions, it is important that the health effects be reported in standardized units. Current guidelines recommend that the metric of choice for reporting health benefits in cost-effectiveness analysis is the quality-adjusted life-year.Citation1–Citation5
A variety of techniques have been developed to assess patient quality of life. Available instruments can be generally classified into two major categories, ie, descriptive measurement instruments or preference-based methods. Descriptive measurement instruments are designed to measure quality of life across important aspects of a patient’s health state, such as physical, psychosocial, or functional well-being.Citation6 Such instruments provide a score for each health domain and a quantitative measure that represents a patient’s current health state. In contrast, preference-based or utility instruments, such as the European Quality of Life-5 Dimensions (EQ-5D), add a valuation component to a patient’s reported health state.Citation7 These instruments are designed to reflect both a quantitative description of a patient’s health state and society’s preference for that particular health state. This preference component is the primary distinction between a utility instrument and a descriptive measurement instrument. Preference-based instruments allow for the calculation of quality-adjusted life-years.
In ischemic heart disease (IHD) research, there is an abundance of published literature on the Seattle Angina Questionnaire (SAQ), a descriptive quality of life instrument. The SAQ is a validated descriptive instrument that evaluates quality of life in patients with IHD across five domains, specifically physical limitation, treatment satisfaction, angina frequency, angina stability, and disease perception.Citation8 In contrast, there is a paucity of studies that report utility weights for patients with IHD.Citation3 The absence of available and up-to-date utility weights is a substantial limitation when performing economic analyses in IHD. To address this lack of utility information, we have previously published a mapping algorithm to convert SAQ descriptive scores to utility weights, based on the EQ-5D preference-based utility instrument.Citation9,Citation10
In this study, we extended our previous work by performing a systematic review of the literature to identify all previous studies that used the SAQ to measure health state, and then applied our validated mapping algorithm to create a comprehensive catalog of utility weights across the spectrum of IHD, with the intention that our catalog be used for future economic evaluations in IHD.
Materials and methods
Search strategy
First, we conducted a systematic review of the published literature, conforming to the standards recommended by the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.Citation11 We used the search terms “Seattle Angina Questionnaire”, “SAQ”, or slight modifications of these terms (see Supplementary material for full search strategy) to identify potentially relevant citations from inception to November 7, 2012 using the following medical literature databases: MEDLINE (Ovid), EMBASE (Ovid), Cochrane Library (Wiley), HealthStar (Ovid), and PubMed. We subsequently performed a citation search in Google Scholar (Google), Web of Science (Thomson Reuters), and Scopus (Elsevier) to identify articles citing the original paper by Spertus et alCitation8 that first examined the validity and reliability of the SAQ. Finally, we searched major clinical trial registries (clinicaltrials.gov and clinicaltrialsregister.eu) from inception to November 7, 2012 for studies that used the SAQ as an outcome measure, using the search terms “Seattle Angina Questionnaire” or “SAQ”.
Upon removal of duplications, two independent reviewers (SF and HCW) screened each reference. We utilized a hierarchal approach, screening citations by title, then abstract, and finally by full text to determine relevance. Reviewers assessed the eligibility of these selected articles according to two prespecified inclusion criteria, ie, that publication was in English and that mean scores and standard errors (or the ability to calculate standard errors from the available data) were reported for all five domains of the SAQ. Although the SAQ has been translated into multiple languages, the original SAQ validation studies were based on the English version; as such, we restricted our algorithm to English articles. All five domains were needed to utilize our mapping algorithm. Exclusion criteria were articles that reported on experimental interventions (eg, transmyocardial laser revascularization, herbal medicine) that are not part of standard therapy. The following information was extracted from eligible studies: baseline characteristics of study participants (age, gender); inclusion and exclusion criteria for each study, interventions (eg, myocardial infarction, revascularization) and follow-up duration; and reported SAQ scores and standard errors.
Data synthesis
We have previously created and published a prediction algorithm using multivariable linear regression modeling, with the utility weight from the EQ-5D being our response variable of interest. Details of the derivation and validation of the mapping algorithm are available elsewhere.Citation9 In brief, all model fitting was done using Bayesian methods. The posterior probability distribution for each of the model parameters was estimated using Markov Chain Monte Carlo simulation methods, with noninformative prior distributions for all model parameters. The data for model development were from 1,992 consecutive patients who underwent coronary angiography in 2004 as part of the Alberta Provincial Project for Outcome Assessment in Coronary Heart Disease database. The final mapping algorithm was a linear regression model, with the dependent variable being the EQ-5D, and a conditional distribution of Yi∼N(μi,σi). The specification of the mean was given by:
with the following parameter estimates:
intercept 0.4388 (0.4015–0.4763), β AF 0.0010 (0.0007–0.0013), β AS −0.0002 (−0.0005 to 0.0000), β DP 0.0023 (0.0020–0.0027), β PL 0.0019 (0.0017–0.0022), β TS 0.0004 (−0.0001 to 0.0008).
Using the posterior distribution for the coefficients of the final linear regression mapping algorithm, we calculated the EQ-5D based on the scores for the five SAQ domains for each included study. To fully incorporate uncertainty in the estimated EQ-5D utilities, we assumed that the inputted SAQ values from each paper had a normal distribution, based on the mean and standard error. We sampled from this distribution to calculate the mean and 95% credible interval of the estimated EQ-5D.
The mapping algorithm and EQ-5D estimates were calculated using WinBUGS version 1.4 (Medical Research Council, London, UK).
Results
Study selection
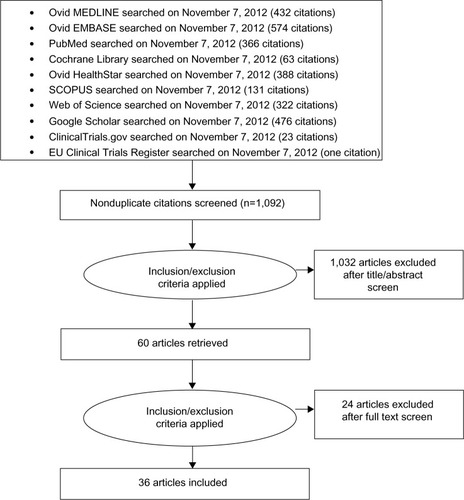
We identified 2,776 citations from various sources using our search criteria. After removing duplications, 1,092 articles were screened to identify articles in English that were potentially relevant and that reported scores and standard errors (or standard deviation and sample size, or confidence intervals, in order to calculate the standard error) for all five domains of the SAQ. Full review was done on 60 articles. We excluded 24 of these articles because they provided SAQ scores following experimental interventions, ie, neurostimulation (six articles), autologous bone marrow transplant (three articles), transmyocardial laser revascularization (six articles), herbal medicine (two articles), fibroblast growth factor (one article), granulocyte colony-stimulating factor (one article), cognitive behavioral therapy (one article), and other (four articles). A total of 36 articles met our eligibility criteria and were included in the final analysis. presents the flow diagram of our review process.
Study characteristics
The 36 studies in our systematic review represent a wide spectrum of patients with IHD. Eight of these studies focused exclusively on patients with stable angina,Citation12–Citation19 and four included patients with a previous myocardial infarction.Citation12,Citation20–Citation22 Four studies specifically assessed SAQ in patients with advanced IHD unsuitable for revascularization.Citation18,Citation23–Citation25 These studies reported SAQ scores in patients with general angina, or specifically with severe or refractory angina. Five studies were restricted to an elderly population,Citation23,Citation26–Citation29 one study was restricted to women with IHD,Citation30 and one study reported SAQ data in diabetic patients with IHD.Citation17 SAQ data were compared among South Asians versus Europeans with IHD in one study,Citation31 while another study reported the SAQs of Caucasians and African Americans with IHD.Citation20 The studies ranged from cross-sectional evaluations with no follow-up to longitudinal studies with follow-up ranging from 7 days to a mean of 6 years and 11 months.
Given our intent to form a catalog such that estimated utility scores can be easily referenced, we categorized the 36 included articles in three groups, as shown in –. Thirteen studies focused on general IHD patients (), four focused on patients with recent acute coronary syndrome (), and 19 assessed revascularized patients (), of which eight included only patients who underwent coronary artery bypass grafting (CABG)Citation23,Citation28,Citation29,Citation32–Citation36 and six included only patients who had percutaneous coronary intervention.Citation19,Citation21,Citation27,Citation37–Citation39
Table 1 General ischemic heart disease
Table 2 Acute coronary syndrome, MI, and acute chest pain
Table 3 Revascularization
Predicted EQ-5D
The SAQ scores from the original publications and the calculated EQ-5D scores are shown in –. The estimated baseline EQ-5D scores for the general IHD patients were in the range of 0.605–0.843, increasing to 0.649–0.877 post follow-up (). The baseline range was 0.706–0.796 for the studies focused on patients with a recent acute coronary syndrome, increasing to 0.795–0.942 post follow-up (). The revascularization studies had EQ-5D scores in the range of 0.616–0.790 at baseline, increasing to 0.653–0.928 after treatment (). Studies that included only CABG as the revascularization modality had an EQ-5D score range that increased from 0.643–0.788 at baseline to 0.653–0.928 after CABG; the studies that focused only on percutaneous coronary intervention had scores that increased from 0.616–0.790 at baseline to 0.668–0.897 after treatment.
Discussion
In this report, we have provided a comprehensive catalog of predicted EQ-5D utility scores for patients with IHD. We first performed a systematic review of the literature to identify studies that reported SAQ scores and then applied our previously validated mapping algorithm to convert SAQ scores to EQ-5D scores. The studies included in our systematic review represent a broad spectrum of IHD patients and assessed quality of life at baseline and/or following a broad range of nonpharmacologic, medical, or surgical interventions.
Patient-reported health status has gained an increasingly important role in the decision-making process for health resource allocation.Citation40 Patient health status independently predicts mortality, cardiovascular events, hospitalizations, and costs of care in cardiovascular illnesses.Citation41–Citation43 Current methodologic guidelines emphasize the importance of preference-based measures in comparative effectiveness studies of health technologies. For example, the National Institute for Health and Clinical Excellence suggests that EQ-5D is the preferred method in quantifying the health outcome of various interventions.Citation44 However, in many circumstances, preference-based instruments have not been included in cardiovascular studies. In the absence of such information, mapping techniques such as that applied in the current study can be used to estimate utility weights from available descriptive quality of life data.Citation45
Dyer et al recently published a summary of available EQ-5D scores from the entire spectrum of cardiovascular diseases,Citation46 and were able to identify 18 studies in IHD. They observed significant heterogeneity in the reported EQ-5D scores across these studies, in the range of 0.45–0.88. We believe our study is an important addition to this early work, by providing utility scores on additional studies in IHD, covering a wide spectrum of revascularization modalities and patient populations. Similar to the previous work by Dyer et al, we found heterogeneity between studies. This heterogeneity in utility weights between studies underscores the importance of a catalog such as ours. When researchers are developing economic models, it is essential that the utility weights inputted are reflective of the population being studied. Our catalog provides detailed information on the population being evaluated, as well as interventions, which will provide researchers with the information needed such that they can utilize the most appropriate utility weights when developing economic models.
Our mapping algorithm was designed to estimate EQ-5D scores using the scores and standard errors in all five domains of the SAQ.Citation9 An important limitation is that we had to exclude studies that did not publish scores on all five domains of the SAQ. However, our final catalog included estimated EQ-5D scores across a wide range of baseline patient demographics, disease severity, and various treatment interventions. A weakness of our systematic review is that we failed to capture studies that did not use the name of the SAQ scale in the text of the paper and failed to cite the source of the questionnaire.
In conclusion, in the current era of budgetary constraints, cost-effectiveness analysis has become increasingly important in decision-making for health resource allocation. In the absence of directly measured individual patient preference-based data, our catalog of estimated EQ-5D scores can be useful in IHD-related economic evaluations.
Author contributions
HCW was involved in the conception, design, acquisition, analysis and interpretation of the data, and critically revised the manuscript. SFZ was involved in the conception and design, acquisition of data, and interpretation of the data, and drafted the manuscript. WW was involved in conception of the study, performed the systematic search, and revised the manuscript critically. MCB was involved in the acquisition of data, analysis and interpretation of data, and revised the manuscript critically. All authors approved the final manuscript for publication and agree to be accountable for all aspects of the work.
Acknowledgments
HCW is supported by a Distinguished Clinical Scientist Award from the Heart and Stroke Foundation of Canada.
Supplementary material
The following method describes the search strategy used to collect the references analyzed in this study. This strategy had three primary facets, outlined below.
Identification of materials in the primary databases of medical literature that referenced the Seattle Angina Questionnaire. These databases were MEDLINE (Ovid), EMBASE (Elsevier), OVID HealthStar, MEDLINE (PubMed), and the Cochrane Library (Wiley).
Use of the citation mapping tools Google Scholar (Google), Scopus (Elsevier), and Web of Science (Thomson Reuters), to find all available references to the paper in which Seattle Angina Questionnaire was first described by John Spertus et al in the Journal of the American College of Cardiology in 1995. The search strategy was to locate the original article by Spertus et al and export the references that the tool identified as having cited that article.
Use of the major clinical trial registries to determine the studies that used the SAQ as an outcome measure. These registries have simple search functions, and so our search terms were “Seattle Angina Questionnaire” or “SAQ”. The strategy then underwent peer review by a librarian experienced in the creation and review of systematic search strategies.
Search strategy
The following search strategy was applied to MEDLINE (Ovid), HealthStar (Ovid), and EMBASE (Ovid). It was adapted for use in PubMed by updating the syntax to match that offered in the PubMed search tool. When searching the Cochrane Library, only the words “Seattle Angina Questionnaire” were used. Databases were searched from inception until 2013.
(Development and evaluation of the Seattle Angina Questionnaire: a new functional status measure for coronary artery disease).m_titl.
seattle angina questionnaire.mp.
seattle angina questionnaire.tw.
(seattle adj3 angina).af.
(angina adj3 questionnaire).af.
saq.mp.
or/1–6.
spertus ja.au.
and 8.
Disclosure
The authors report no competing interests in this work.
References
- National Institute for Health and Clinical ExcellenceGuide to the Methods of Technology AppraisalLondon, UKNational Institute for Clinical Excellence2004
- Canadian Agency for Drugs and Technologies in HealthGuidelines for the Economic Evaluation of Health Technologies: Canada3rd edOttawa, ON, CanadaCanadian Agency for Drugs and Technologies in Health2006
- LongworthLBuxtonMSculpherMSmithDEstimating utility data from clinical indicators for patients with stable anginaEur J Health Econ20056434735316193322
- World Health OrganizationMaking Choices in Health: WHO Guide to Cost-Effectiveness AnalysisGeneva, SwitzerlandWorld Health Organization2003
- DrummondMFSculpherMJTorranceGWO’BrienBJStoddartGLMethods for the Economic Evaluation of Health Care Programmes3rd edOxford, UKOxford University Press2005
- Llewellyn-ThomasHAHealth state descriptions. Purposes, issues, a proposalMed Care199634Suppl 12DS109DS1188969319
- DolanPModeling valuations for EuroQol health statesMed Care19973511109511089366889
- SpertusJAWinderJADewhurstTADevelopment and evaluation of the Seattle Angina Questionnaire: a new functional status measure for coronary artery diseaseJ Am Coll Cardiol19952523333417829785
- WijeysunderaHCTomlinsonGNorrisCMGhaliWAKoDTKrahnMDPredicting EQ-5D utility scores from the Seattle Angina Questionnaire in coronary artery disease: a mapping algorithm using a Bayesian frameworkMed Decis Making201131348149321127316
- BrooksREuroQol: the current state of playHealth Policy1996371537210158943
- MoherDLiberatiATetzlaffJAltmanDGPreferred reporting items for systematic reviews and meta-analyses: the PRISMA statementAnn Intern Med2009151426426919622511
- SpertusJADewhurstTDoughertyCMNicholPTesting the effectiveness of converting patients to long-acting antianginal medications: the Quality of Life in Angina Research Trial (QUART)Am Heart J2001141455055811275919
- BeltrameJFWeekesAJMorganCTavellaRSpertusJAThe prevalence of weekly angina among patients with chronic stable angina in primary care practices: the Coronary Artery Disease in General Practice (CADENCE) StudyArch Intern Med2009169161491149919752407
- MakolkinVIOsadchiyKKTrimetazidine modified release in the treatment of stable angina: TRIUMPH studyTRImetazidine MR in patients with stable angina: unique metabolic PatHClin Drug Investig20042412731738
- StonePHGratsianskyNABlokhinAHuangIZMengLERICA InvestigatorsAntianginal efficacy of ranolazine when added to treatment with amlodipine: the ERICA (Efficacy of Ranolazine in Chronic Angina) trialJ Am Coll Cardiol200648356657516875985
- MaxwellAJZapienMPPearceGLMacCallumGStonePHRandomized trial of a medical food for the dietary management of chronic, stable anginaJ Am Coll Cardiol2002391374511755284
- DeatonCKimbleLPVeledarEThe synergistic effect of heart disease and diabetes on self-management, symptoms, and health statusHeart Lung200635531532316963363
- AndrellPEkreOGripLFatality, morbidity and quality of life in patients with refractory angina pectorisInt J Cardiol2011147337738219880202
- LoweHCOesterleSNHeKLMacNeillBDBurkhoffDOutcomes following percutaneous coronary intervention in patients previously considered “without option”: a subgroup analysis of the PACIFIC trialJ Interv Cardiol2004172879115104770
- OhldinAYoungBDerlethAEthnic differences in satisfaction and quality of life in veterans with ischemic heart diseaseJ Natl Med Assoc200496679980815233490
- NeilNRamseySDCohenDJResource utilization, cost, and health status impacts of coronary stent versus “optimal” percutaneous coronary angioplasty: results from the OPUS-I trialJ Interv Cardiol200215424925512238418
- PettersenKIReikvamAStavemKReliability and validity of the Norwegian translation of the Seattle Angina Questionnaire following myocardial infarctionQual Life Res200514388388916022080
- GelsominoSLorussoRLiviUCost and cost-effectiveness of cardiac surgery in elderly patientsJ Thorac Cardiovasc Surg201114251062107321492881
- FathiRHaluskaBShortLMarwickTHA randomized trial of aggressive lipid reduction for improvement of myocardial ischemia, symptom status, and vascular function in patients with coronary artery disease not amenable to interventionAm J Med2003114644545312727577
- MooreRKGrovesDBatesonSHealth related quality of life of patients with refractory angina before and one year after enrolment onto a refractory angina programEur J Pain20059330531015862480
- GrahamMMNorrisCMGalbraithPDKnudtsonMLGhaliWAAPPROACH InvestigatorsQuality of life after coronary revascularization in the elderlyEur Heart J200627141690169816717072
- AgarwalSSchechterCZamanAAssessment of functional status and quality of life after percutaneous coronary revascularisation in octogenariansAge Ageing200938674875119755713
- MacDonaldPStadnykKCossettJKlassenGJohnstoneDRockwoodKOutcomes of coronary artery bypass surgery in elderly peopleCan J Cardiol19981410121512229852935
- FruitmanDSMacDougallCERossDBCardiac surgery in octogenarians: can elderly patients benefit? Quality of life after cardiac surgeryAnn Thorac Surg19996862129213510616989
- BroddadottirHJensenLNorrisCGrahamMHealth-related quality of life in women with coronary artery diseaseEur J Cardiovasc Nurs200981182518602346
- BaineyKRNorrisCMGuptaMAltered health status and quality of life in South Asians with coronary artery diseaseAm Heart J2011162350150621884867
- AscioneRReevesBCTaylorFCSeehraHKAngeliniGDBeating heart against cardioplegic arrest studies (BHACAS 1 and 2): quality of life at mid-term follow-up in two randomised controlled trialsEur Heart J200425976577015120887
- AngeliniGDCullifordLSmithDKEffects of on- and off-pump coronary artery surgery on graft patency, survival, and health-related quality of life: long-term follow-up of 2 randomized controlled trialsJ Thorac Cardiovasc Surg2009137229530319185140
- KarolakWHirschGButhKLegareJFMedium-term outcomes of coronary artery bypass graft surgery on pump versus off pump: results from a randomized controlled trialAm Heart J2007153468969517383313
- ChaudhurySSharmaSPawarAAPsychological correlates of outcome after coronary artery bypass graftMed J Armed Forces India2006623220223
- WagnerTHSethiGHolmanWCosts and quality of life associated with radial artery and saphenous vein cardiac bypass surgery: results from a Veterans Affairs multisite trialAm J Surg2011202553253521872209
- de QuadrosASLimaTCRodriguesAPQuality of life and health status after percutaneous coronary intervention in stable angina patients: results from the real-world practiceCatheter Cardiovasc Interv201177795496020824752
- WongMSChairSYChanges in health-related quality of life following percutaneous coronary intervention: a longitudinal studyInt J Nurs Stud20074481334134216982057
- WeintraubWSSpertusJAKolmPEffect of PCI on quality of life in patients with stable coronary diseaseN Engl J Med2008359767768718703470
- RumsfeldJSAlexanderKPGoffDCJrCardiovascular health: the importance of measuring patient-reported health status: a scientific statement from the American Heart AssociationCirculation2013127222233224923648778
- MommersteegPMDenolletJSpertusJAPedersenSSHealth status as a risk factor in cardiovascular disease: a systematic review of current evidenceAm Heart J2009157220821819185627
- HeidenreichPASpertusJAJonesPGHealth status identifies heart failure outpatients at risk for hospitalization or deathJ Am Coll Cardiol200647475275616487840
- ChanPSSotoGJonesPGPatient health status and costs in heart failure: insights from the eplerenone post-acute myocardial infarction heart failure efficacy and survival study (EPHESUS)Circulation2009119339840719139382
- National Institute for Health and Clinical ExcellenceBriefing Paper for Methods Review Workshop on Key Issues in Utility MeasurementLondon, UKNational Institute for Health and Clinical Excellence2007
- BrazierJEYangYTsuchiyaARowenDLA review of studies mapping (or cross walking) non-preference based measures of health to generic preference-based measuresEur J Health Econ201011221522519585162
- DyerMTGoldsmithKASharplesLSBuxtonMJA review of health utilities using the EQ-5D in studies of cardiovascular diseaseHealth Qual Life Outcomes201081320109189
- LeungYWGrewalKGravely-WitteSSuskinNStewartDEGraceSLQuality of life following participation in cardiac rehabilitation programs of longer or shorter than 6 months: does duration matter?Population Health Management201114418118821241185
- ZhangZMahoneyEMStablesRHDisease-specific health status after stent-assisted percutaneous coronary intervention and coronary artery bypass surgery: one-year results from the Stent or Surgery trialCirculation2003108141694170012975252
- KimJHendersonRAPocockSJHealth-related quality of life after interventional or conservative strategy in patients with unstable angina or non-ST-segment elevation myocardial infarction: one-year results of the third Randomized Intervention Trial of unstable Angina (RITA-3)J Am Coll Cardiol200545222122815653019
- HoferSBenzerWSchusslerGvon SteinbuchelNOldridgeNBHealth-related quality of life in patients with coronary artery disease treated for angina: validity and reliability of German translations of two specific questionnairesQual Life Res200312219921212639066
- ArnoldSVMorrowDAWangKMERLIN-TIMI 36 InvestigatorsEffects of ranolazine on disease-specific health status and quality of life among patients with acute coronary syndromes: results from the MERLIN-TIMI 36 randomized trialCirc Cardiovasc Qual Outcomes20081210711520031797
- ArnoldSVSpertusJAJonesPGXiaoLCohenDJThe impact of dyspnea on health-related quality of life in patients with coronary artery disease: results from the PREMIER registryAm Heart J2009157610421049.e104119464415
- Asadi-LariMPackhamCGrayDGender difference in health-related needs and quality of life in patients with acute chest painBr J Cardiol2005126459464
- de Jong-WattWJArthurHMAnxiety and health-related quality of life in patients awaiting elective coronary angiographyHeart & Lung200433423724815252414