Abstract
Background
Understanding the value of new anticoagulation therapies compared with existing therapies is of paramount importance in today’s cost-conscious and efficiency-driven health care environment. Edoxaban and rivaroxaban for stroke prevention in nonvalvular atrial fibrillation (NVAF) patients with CHADS2 scores ≥2 have been evaluated in pivotal trials versus warfarin. The relative value of edoxaban versus rivaroxaban would be of interest to health care stakeholders and patients who prefer a once-daily treatment option for long-term stroke prevention in NVAF.
Objective
To evaluate the relative cost-effectiveness of two once-daily regimens of novel oral anticoagulation therapy – edoxaban (60 mg/30 mg dose-reduced) versus rivaroxaban (20 mg/15 mg dose-reduced) – for stroke prevention in NVAF patients from a US health-plan perspective.
Materials and methods
A Markov model simulated lifetime risk and treatment of stroke, systemic embolism, major bleeding, clinically relevant nonmajor bleeding, myocardial infarction, and death in NVAF patients treated with edoxaban or rivaroxaban. Efficacy and safety data were derived from a network meta-analysis that utilized data from patients enrolled in ENGAGE AF-TIMI 48 and ROCKET-AF. Health care cost and utility data were obtained from published sources. Incremental cost-effectiveness ratios of <US$50,000, $50,000–$150,000, and >$150,000 per quality-adjusted life year (QALY) gained were used as thresholds for “highly cost-effective”, “cost-effective”, and “not cost-effective” treatment options, respectively, as per American Heart Association/American College of Cardiology guidelines.
Results
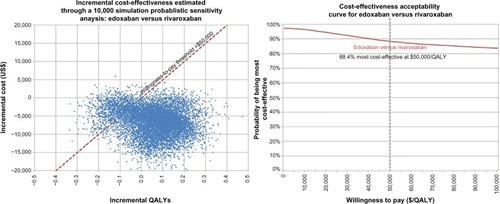
Edoxaban was dominant relative to rivaroxaban, such that it was associated with lower total health care costs and better effectiveness in terms of QALYs in the base-case analysis. Results were supported by probabilistic sensitivity analyses that showed edoxaban as either dominant or a highly cost-effective alternative (incremental cost-effectiveness ratio <$50,000) to rivaroxaban in 88.4% of 10,000 simulations.
Conclusion
Results of this study showed that the once-daily edoxaban (60 mg/30 mg dose-reduced) regimen is a cost-saving or highly cost-effective treatment relative to rivaroxaban (20 mg/15 mg dose-reduced) for stroke prevention in NVAF patients with CHADS2 ≥2.
Introduction
Atrial fibrillation (AF) affects approximately 2.3 million people in the US, and is associated with a fivefold increase in stroke compared to patients without AF.Citation1–Citation3 Oral anticoagulation with the vitamin K antagonist (VKA) warfarin has been the standard of care for stroke prevention in people with nonvalvular AF (NVAF).Citation4–Citation6 However, VKAs have numerous limitations, including a variety of food and drug interactions, slow onset of action, high discontinuation rates, narrow therapeutic range, and variable patient dose response, which require routine laboratory monitoring.Citation6–Citation8 In recent years, several non-VKA novel oral anticoagulants (NOACs; dabigatran, rivaroxaban, apixaban, and edoxaban) have been approved in the US as alternatives to warfarin for stroke prevention in NVAF patients. These newer agents do not require routine monitoring, have faster onset of action, bear fewer food and drug interactions compared to VKA therapy, and offer the promise to provide practical and more convenient oral anticoagulation (OAC) treatment.Citation6–Citation8
As new OAC therapies come to market, the need to understand their “value” is of paramount importance in today’s cost-conscious health care environment. Recently, the American College of Cardiology/American Heart Association Task Force on Performance Measures and Task Force on Practice Guidelines proposed the inclusion of cost-effectiveness/value assessment and recommendations in practice guidelines and performance measures.Citation9 The cost-effectiveness of warfarin therapy compared to aspirin/no therapy for stroke-prevention NVAF anticoagulation has been well established.Citation10–Citation12 Consensus has emerged from the large and ever-growing body of economic literature about the comparative costs and cost-effectiveness of anticoagulation therapies for stroke prevention in NVAF patients that NOACs are cost-effective alternatives to warfarin for stroke prevention in NVAF.Citation13–Citation19 While data on the particular value of one NOAC versus another NOAC are scant, this is a subject of growing interest to health care decision makers.
Edoxaban, a factor-Xa inhibitor, was approved in 2015 by the US Food and Drug Administration as a once-daily NOAC for stroke prevention in NVAF.Citation20 Data from the Phase III pivotal trial ENGAGE AF-TIMI 48 have shown that a once-daily edoxaban 60 mg regimen was noninferior in the risk of stroke/systemic embolism (SE) when compared to warfarin, with significantly lower risk of major bleeding (Daiichi Sankyo, data on file, 2013).Citation21 Among patients with creatinine clearance ≤95 mL/min, edoxaban reduced the risk of stroke/SE by 32%, with lower risk of major bleeding by 16% relative to warfarin.Citation20 Although no head-to-head randomized controlled studies have evaluated the efficacy and safety of edoxaban in direct comparison with other NOACs, several network meta-analyses have been presented or published that indirectly compared the efficacy and safety of NOACs (including edoxaban).Citation22–Citation28
The objective of this study was to evaluate the relative cost-effectiveness of two once-daily NOAC-therapy options – edoxaban (60 mg/30 mg dose-reduced) versus rivaroxaban (20 mg/15 mg dose-reduced) – for stroke prevention in NVAF patients from a US health-plan perspective. We were interested in comparing edoxaban to rivaroxaban for multiple reasons. First, rivaroxaban is the most commonly prescribed NOAC in the US and dominates the NVAF stroke-prevention market.Citation29 Second, the pivotal trials of edoxaban – ENGAGE AF-TIMI 48 (Daiichi Sankyo, data on file, 2013)Citation21 and rivaroxaban ROCKET-AFCitation30 – were more similar in study design than the trials for other NOACs, as both studies utilized once-daily treatment and limited enrollment to patients with CHADS2 scores ≥2. Finally, we believed the relative value of edoxaban versus rivaroxaban would be of interest to health care stakeholders and patients who prefer a once-daily treatment option for chronic stroke prevention in NVAF.
Materials and methods
Model design
A health-state transition (semi-Markov) model was developed using Microsoft Excel 2013. The Markov modeling approach has been used for other published economic evaluations of NOAC therapy in recent years, as reviewed and summarized in recent publications.Citation13,Citation14,Citation16,Citation17 The economic model compared two hypothetical NVAF patient cohorts initiating treatment with either once-daily edoxaban (60 mg/30 mg dose-reduced) regimen or once-daily rivaroxaban (20 mg/15 mg dose-reduced) for stroke prevention on a chronic basis. The patient cohorts simulated in the model consisted of CHADS2 score ≥2 patients (consistent with the study populations in ENGAGE AF-TIMI 48 (Daiichi Sankyo, data on file, 2013)Citation21 and ROCKET-AFCitation30) with a starting age of 72 years (the median ages of patients in ENGAGE AF-TIMI 48 and ROCKET-AF were 72 years and 73 years, respectively). These patients transitioned between discrete health states in the model to replicate the natural course of changes in health status on a monthly basis over a remaining lifetime horizon (up to maximum age of 100 years).
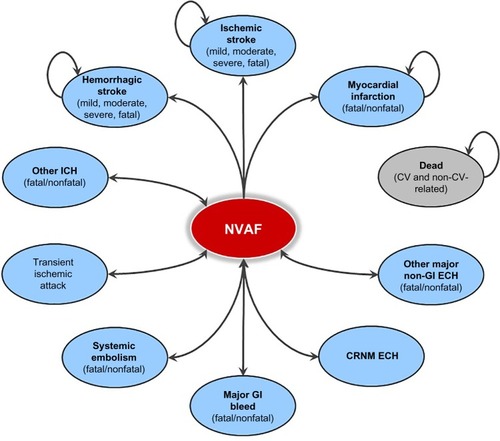
A schematic presenting the model health states and transition pathways is shown in . All patients begin in the NVAF health state. During any given model cycle, patients can either remain in their current health state, experience a clinical event, or die. Consistent with other published models evaluating OAC therapy, the following clinical events were included in the model: ischemic stroke (first and recurrent), transient ischemic attack (TIA), SE, hemorrhagic stroke (first and recurrent), other intracranial hemorrhage (ie, subdural and epidural hematoma), major gastrointestinal bleed, other major nongastrointestinal extracranial bleed, clinically relevant nonmajor extracranial bleed, myocardial infarction (MI), event-related death, and death from other causes. Also consistent with other models,Citation31,Citation32 both ischemic stroke and hemorrhagic stroke were modeled as closed health states, such that after experiencing the first stroke patients would transition to a post-stroke state where they could experience only stroke recurrence or die. Nonfatal stroke events were stratified by severity: mild stroke (modified Rankin score 0–2), moderate stroke (modified Rankin score 3–4), and severe stroke (modified Rankin score 5). Patients experiencing an MI entered a post-MI health state where they were allowed to experience other clinical events, including subsequent MI. The post-stroke and post-MI states were included to account for residual deficits as a result of these events. All other clinical events were modeled as transient health states, such that patients who survived an event would return to the NVAF “well” state without any residual deficit. All clinical events have the potential of being fatal, except TIA and clinically relevant nonmajor bleeds. Institutional Review Board (IRB) approval was not required for this economic model using simulated cohorts of patients.
Clinical event risks and health state-transition probabilities
Warfarin served as the reference treatment in the Markov model, and its transition probabilities were based on the warfarin event rates stratified by CHADS2 score (as per the format of the data from the overall population in ENGAGE AF-TIMI 48 (Daiichi Sankyo, data on file, 2013)Citation21 and reflecting differing underlying risk of thrombotic events) and consolidated into a single value weighted by CHADS2-score distribution (). The rationale for this was supported by the data from the pivotal trials of edoxaban (Daiichi Sankyo, data on file, 2013)Citation21 and rivaroxaban,Citation30 which showed that their relative efficacy versus warfarin did not differ by CHADS2 score, so there was no need to stratify the thrombotic event risks by CHADS2 score (). Consistent with the approach taken by other published cost-effectiveness analyses, the risk of ischemic stroke, TIA, MI, and bleeding events (including hemorrhagic stroke) in our model increased with age, using factors of 1.40,Citation33–Citation36 1.73,Citation37 1.30,Citation31,Citation32,Citation34,Citation38,Citation39 and 1.97,Citation31,Citation32,Citation34,Citation36,Citation40 respectively, for each decade increase in age. The distribution of stroke severity was based on data from ENGAGE AF-TIMI 48 (Daiichi Sankyo, data on file, 2013).Citation21
Table 1 Patient characteristics, clinical event rates, and stroke-severity distribution
Event rates for patients receiving edoxaban or rivaroxaban were calculated based on risk ratios relative to warfarin obtained from a network meta-analysis of data from Phase III pivotal trials where rivaroxaban and edoxaban were compared to warfarin ().Citation22 Patients either continue OAC therapy or discontinue OAC therapy temporarily or permanently at any time. Patients who discontinue edoxaban and rivaroxaban were assumed in the model to receive aspirin therapy. Event rates for second-line aspirin therapy were obtained from a published NOAC cost-effectiveness modeling study that used data from a meta-analysis of clinical trials ().Citation41,Citation42 The risk of recurrent ischemic or hemorrhagic stroke was independent of treatment, and was set to 2.7% for both the edoxaban- and rivaroxaban-treatment arms to be consistent with other recently published OAC-therapy economic evaluations.Citation31,Citation32,Citation43
Mortality
Case-fatality rates for modeled clinical events are presented in . Cardiovascular mortality outside clinical events explicitly represented in the model was separately accounted for using a cardiovascular mortality risk-ratio estimate of 0.87 for both edoxaban versus warfarin and for rivaroxaban versus warfarin, as estimated from the network meta-analysis.Citation22 In addition to event-related mortality, allowance was made in the model for patients to die from other causes. This underlying mortality risk unrelated to clinical events was based on age-specific US life tables.Citation44 A multiplier of 1.34 was applied to the general mortality rate to account for the increased mortality risk for NVAF patients relative to the general population.Citation31,Citation32 In addition, mortality risk for patients who survived clinical events was further increased according to the mortality-risk multipliers presented in .
Table 2 Mortality estimates for model inputs
Treatment discontinuation
All patients were assumed to discontinue NOAC therapy temporarily for the model cycle (1 month) after an acute clinical event occurred. In addition, patients could continue OAC therapy, or discontinue OAC therapy temporarily or permanently in future model cycles subsequent to clinical events. Assumptions about permanent discontinuation of OAC therapy following clinical events mirrored those used in other published economic evaluations.Citation31,Citation32 All patients discontinue NOAC therapy permanently following hemorrhagic stroke or MI, which is consistent with assumptions used in other models.Citation31,Citation32 Fifty-six percent of patients discontinue NOAC therapy permanently and 44% temporarily stop therapy for 1 month after intracranial hemorrhage (other ICH).Citation31,Citation32 Following a major extracranial hemorrhage, 25% of patients will discontinue NOAC therapy permanently, and 75% will stop therapy temporarily for 1 month.Citation31,Citation32 Patients who discontinue NOAC therapy permanently were assumed to receive aspirin.Citation31,Citation32 In addition, the model assumed an annual permanent treatment discontinuation rate of 5% unrelated to clinical events to account for medication nonadherence.
Utilities and disutilities
NVAF patients entered the model with a baseline utility of 0.836, consistent with baseline utility for patients enrolled in ENGAGE-AF TIMI 48 assessed by the EQ-5D™, a standardized instrument for use as a measure of health outcome.Citation45 Disutility associated with all clinical events was applied for the full 1-month cycle in which an acute clinical event occurred; otherwise, disutility associated with chronic health states was applied across the full duration of time in which a patient remained in a particular chronic health state ().
Table 3 Health state utilities and disutilities
Costs
The wholesale acquisition cost of edoxaban (US$9.24 per day for both 60 mg and 30 mg) and rivaroxaban ($10.49 per day for both 20 mg and 15 mg) were used in the analysis.Citation46 Health care expenditures associated with each health state in the model were derived from published literature, diagnosis-related group data from the Healthcare Cost and Utilization Project,Citation47 and from Centers for Medicare & Medicaid Services (CMS) fee schedules, adjusted where necessary to 2014 levels using the “ Medical care” component of the US Consumer Price Index (). Future costs and life years (LYs) and quality-adjusted LYs (QALYs) were discounted by 3% annually after the first year, as recommended by pharmacoeconomic guidelines published by the Academy of Managed Care Pharmacy.Citation48
Table 4 Cost inputs
Analyses
The cost-effectiveness of edoxaban relative to rivaroxaban was assessed using an incremental cost-effectiveness ratio (ICER), which is calculated as the incremental cost per QALY gained. ICERs of <$50,000, $50,000–$150,000, and >$150,000 per QALY gained were proposed as thresholds for “high value/highly cost-effective”, “intermediate value/cost-effective”, and “low value/not cost-effective” treatment options, respectively, as per the American Heart Association/American College of Cardiology statement on cost/value methodology in clinical practice guidelines and performance measures.Citation9
Probabilistic sensitivity analysis, which allows all model parameters to be varied simultaneously, was conducted to test the robustness of model pa pa parameter values and their impact on the ICERs. Second-order Monte Carlo simulation with 10,000 iterations where the value of each model parameter was randomly sampled from the probability distribution (either normal, γ-, lognormal, or triangular distribution, as uniquely determined for each type of model parameter) of base-case value was performed. Results were depicted on a cost-effectiveness plane and transformed into a cost-effectiveness acceptability curve. In addition, a series of one-way sensitivity analyses was performed to determine the independent impact of key model parameters on model results. The mean starting age of the cohort was varied from 60 years to 80 years. The acquisition cost of edoxaban was varied ±13.5% to match the acquisition cost of rivaroxaban on the upper end of the bound, while all clinical event costs were varied ±10% and all utility decrements varied ±25%, as is typically done in modeling sensitivity analyses. An additional one-way sensitivity analysis was performed where clinical events were varied from the lower and upper bounds of their 95% confidence intervals.
Results
Base-case analysis
In the base-case analysis, while the estimated lifetime mean number of thrombotic events per patient was similar between treatment groups, the mean number of hemorrhagic events was lower for edoxaban relative to rivaroxaban (). These findings resulted in a numerically higher mean number of QALYs for edoxaban (7.299 versus 7.238), and lower mean total health care cost for edoxaban than rivaroxaban ($45,358 versus $49,472 per patient) (). Therefore, edoxaban was economically dominant over rivaroxaban in the base-case analysis. Across both therapies, about 24% of total health care cost was attributable to acute events, 31% was attributable to time spent in chronic health states, and the remaining 45% of total costs came from the OAC drugs themselves.
Table 5 Analysis results
Sensitivity analyses
In one-way sensitivity analyses, when the acquisition cost of edoxaban was increased by 13.5% to the same level as rivaroxaban, at $10.49 per day, edoxaban remained dominant over rivaroxaban, with cost savings of $1,382 per patient (mean per patient cost of $48,090 edoxaban versus $49,472 rivaroxaban) and higher QALYs (7.299 versus 7.238) (). The cost-effectiveness of edoxaban relative to rivaroxaban was not sensitive to age. Edoxaban remained the economically dominant therapy versus rivaroxaban when cost parameters were varied ±10% from their base values and utilities were varied ±25% from their base values. Although not reported in , edoxaban also remained the economically dominant therapy versus rivaroxaban when risks of clinical events were varied from the lower and upper bounds of their 95% confidence intervals.
Table 6 Results of one-way sensitivity analyses
In the Monte Carlo probabilistic sensitivity analysis with 10,000 model iterations, in which all model parameters were randomly sampled from their distributions, edoxaban yielded an ICER <$50,000 per QALY gained in 88.4% of the 10,000 simulations ().
Discussion
This study assessed the cost-effectiveness of edoxaban versus rivaroxaban as treatment for stroke prevention among patients with NVAF from a US health-plan perspective. Our analysis found that edoxaban was associated with greater quality-adjusted life expectancy at lower total health care costs than rivaroxaban. This finding of economic dominance was robust under a series of one-way sensitivity analysis where event-treatment cost and health state-utility estimates were varied. The cost-effectiveness of edoxaban relative to rivaroxaban for stroke prevention was further supported by probabilistic sensitivity analysis where all model parameters were randomly sampled from their distribution, and ICER estimates fell below $50,000 per QALY gained in 88.4% of model simulations. These results were primarily driven by the lower number of nonintracranial major and clinically relevant nonmajor bleeding events in the edoxaban cohort, resulting in lower bleeding-related health care cost and bleeding-related quality-of-life impairment and mortality.
As new OAC therapies come to market, the need to understand their value compared with existing therapies is of paramount importance in today’s cost-conscious and efficiency-driven health care environment. There have been numerous published cost-effectiveness analyses comparing edoxaban and rivaroxaban with warfarin.Citation34,Citation45,Citation49–Citation59 These studies have consistently showed that edoxaban and rivaroxaban are cost-effective relative to warfarin. However, few studies have set out to assess the particular value or cost-effectiveness of one NOAC versus another NOAC, and where such analyses have been conducted (albeit using an indirect comparison approach), there has been substantial inconsistency and contradiction between their findings.Citation13,Citation17
Edwards et alCitation60 found rivaroxaban to be economically dominant over dabigatran in the UK setting, but Kansal et alCitation58 found dabigatran to dominate rivaroxaban in the Canadian setting. In the Canadian model by Wells et al,Citation61 rivaroxaban was dominated by apixaban, yet apixaban is either a dominant strategy or a dominated strategy compared with dabigatran, depending on the dose of dabigatran evaluated. In the UK model by Lip et al,Citation31 apixaban was cost-effective relative to both rivaroxaban and dabigatran, with ICERs well below the commonly assumed threshold of £20,000 per QALY gained. Similarly, Lanitis et alCitation62 reported that in the French setting, apixaban dominates both rivaroxaban and dabigatran, with rivaroxaban either dominating or having favorable ICERs compared with dabigatran. By contrast, the UK model by Zheng et alCitation63 showed dabigatran to be economically dominant over both rivaroxaban and apixaban, while Coyle et alCitation64 found both apixaban and dabigatran dominating rivaroxaban in the Canadian setting. None of these studies were from the perspective of US health care payers. In consideration of the fact that rivaroxaban is the most commonly prescribed NOAC in the US, the relative value of edoxaban relative to rivaroxaban is an important consideration for clinicians and payers. To the best of our knowledge, this is the first study formally to evaluate the cost-effectiveness of edoxaban relative to rivaroxaban.
In the absence of head-to-head comparative trials, cost-effectiveness analysis comparing one NOAC to another requires reliance on clinical data derived from network meta-analysis that indirectly compares one treatment versus another. Several researchers have conducted network meta-analyses of pivotal trial data to assess the relative efficacy and safety of edoxaban versus other NOACs. While these studies differ in methodology and the inclusion of data from patients with CHADS2 scores of 1, they consistently showed rivaroxaban 20 mg was associated with a higher risk of major bleeding and the composite of major and clinically relevant major bleeding, than edoxaban 60 mg. To be consistent with the study population in ENGAGE AF-TIMI 48 and ROCKET-AF (both studies enrolled patients with CHADS2 scores ≥2), we purposefully chose to use data from a network meta-analysis of data from patients with CHADS2 scores ≥2, which showed that among patients with NVAF and CHADS2 scores ≥2, edoxaban (60 mg/30 mg dose-reduced) had similar efficacy to rivaroxaban for the risk of stroke and SE (relative risk 0.90, 95% confidence interval 0.70–1.16 for composite of stroke/SE) and substantially lower risk of major bleeding compared with rivaroxaban (relative risk 0.76, 95% confidence interval 0.52–1.10).Citation22 In other indirect comparisons analyses, Skjøth et alCitation25 and Fu et alCitation26 drew similar conclusions that edoxaban has similar efficacy to rivaroxaban for the risk of stroke and SE, but substantially lower risk of major bleeding.
Limitations
The economic model we developed for this study has several potential limitations. First, many of the model’s data inputs were derived from a network meta-analysis of clinical trial data. Indirect treatment comparisons through network meta-analysis of clinical trials has its own inherent limitations. Although we used data from an analysis of patients with CHADS2 scores ≥2 as an attempt to minimize biases, the comparison did not control for all differences in patient baseline characteristics, such as warfarin time in therapeutic range. The relative efficacy of an NOAC to warfarin depends on the quality of warfarin control. The amount of time warfarin patients spent in the target therapeutic range was higher in ENGAGE AF-TIMI 48 (median 68.4%) than ROCKET-AF (median 58%). This variation would be expected to favor the rivaroxaban-versus-warfarin comparison rather than the edoxaban-versus-warfarin comparison, thus leading to a conservative estimate for the cost-effectiveness of edoxaban.
Another potential study limitation comes from the fact that participants in clinical trials are likely to have received closer management and had better adherence to therapy than patients who would be treated in a nontrial, real-world population. Therefore, the efficacy, safety, and tolerability observed from clinical trials may be better than what would occur in actual clinical practice.
We also note that many data parameters required for an economic model that would include dabigatran and apixaban, the other two NOACs marketed in the US, were not available in the published literature for the subgroup of patients with CHADS2 scores ≥2, as the pivotal trials of these agents included patients with CHADS2 scores ≥1. Other researchers who have attempted indirectly to compare apixaban and dabigatran to rivaroxaban have also acknowledged the challenges for adequately controlling the heterogeneity in patient baseline characteristics and study design.Citation13,Citation31,Citation65–Citation72 For similar reasons, we were unable to pursue analysis for apixaban and dabigatran. The comparative effectiveness of edoxaban relative to all marketed NOACs should be addressed in future observational studies in the real-world setting. Finally our model and analyses were based on costs and resource-use data specific for the US, and thus results are not necessarily generalizable to other countries, due to differences in health care practices and financing.
Conclusion
Our cost-effectiveness analysis over a remaining lifetime horizon provides a comprehensive assessment of the health care resources, mortality risk, and quality-of-life impairment incurred in NVAF patients receiving lifetime once-daily OAC therapy for stroke prevention. Our base-case analysis findings, along with the results of sensitivity analyses, suggest that edoxaban is an economically attractive alternative to rivaroxaban for stroke prevention in NVAF patients. In an era of evidence-based medicine, comparative effectiveness and economics research can inform health care stakeholders in their resource-allocation decisions. Future research is warranted to evaluate further the economic implications of edoxaban therapy in the real-world setting.
Disclosure
Funding for this study was provided by Daiichi Sankyo Inc. (Parsippany, NJ, USA), manufacturer of edoxaban. At the time the study was conducted, WJK and XY were employees of Daiichi Sankyo Inc.; EAM and WSW served as consultants to Daiichi Sankyo Inc. and received honoraria for their services. WSW also discloses funding in part by an Institutional Development Award (IDeA) from the National Institute of General Medical Sciences of the National Institutes of Health under grant number U54-GM104941 (PI: Binder-Macleod). JDM, GML, AMF, and OVT were employed by Truven Health Analytics Inc., which received contracted research funding from Daiichi Sankyo Inc. for conducting the study. An earlier version of this study was presented as a poster (I22) at the Academy of Managed Care Pharmacy (AMCP) Nexus 2015, Orlando, FL, October 26–29, 2015, with the abstract published in Circulation: Cardiovascular Quality and Outcomes (2015;8:A104). The authors report no other conflicts of interest in this work.
References
- GoASHylekEMPhillipsKAPrevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) studyJAMA2001285182370237511343485
- GershBJTsangTSSewardJBThe changing epidemiology and natural history of nonvalvular atrial fibrillation: clinical implicationsTrans Am Clin Climatol Assoc2004115149159 discussion 159–16017060964
- KannelWBBenjaminEJCurrent perceptions of the epidemiology of atrial fibrillationCardiol Clin20092711324vii19111760
- YouJJSingerDEHowardPAAntithrombotic therapy for atrial fibrillation: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice GuidelinesChest20121412 Supple531Se575S22315271
- FurieKLGoldsteinLBAlbersGWOral antithrombotic agents for the prevention of stroke in nonvalvular atrial fibrillation: a science advisory for healthcare professionals from the American Heart Association/American Stroke AssociationStroke201243123442345322858728 ErrataStroke2013443e20 Stroke20124312e181
- JanuaryCTWannLSAlpertJS2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm SocietyJ Am Coll Cardiol20146421e1e7624685669
- SarafKMorrisPGargPSheridanPStoreyRNon-vitamin K antagonist oral anticoagulants (NOACs): clinical evidence and therapeutic considerationsPostgrad Med J201490106752052825085900
- KatsnelsonMSaccoRLMoscucciMProgress for stroke prevention with atrial fibrillation: emergence of alternative oral anticoagulantsCirculation2012125121577158322451607
- AndersonJLHeidenreichPABarnettPGACC/AHA statement on cost/value methodology in clinical practice guidelines and performance measures: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures and Task Force on Practice GuidelinesCirculation2014129222329234524677315
- GageBFCardinalliABAlbersGWOwensDKCost-effectiveness of warfarin and aspirin for prophylaxis of stroke in patients with nonvalvular atrial fibrillationJAMA199527423183918457500532
- SorensenSVDewildeSSingerDEGoldhaberSZMonzBUPlumbJMCost-effectiveness of warfarin: trial versus “real-world” stroke prevention in atrial fibrillationAm Heart J200915761064107319464418
- JowettSBryanSMantJCost effectiveness of warfarin versus aspirin in patients older than 75 years with atrial fibrillationStroke20114261717172121512184
- LimoneBLBakerWLKlugerJColemanCINovel anticoagulants for stroke prevention in atrial fibrillation: a systematic review of cost-effectiveness modelsPLoS One201384e6218323626785
- LimoneBLBakerWLMearnsESWhiteCMKlugerJColemanCICommon flaws exist in published cost-effectiveness models of pharmacologic stroke prevention in atrial fibrillationJ Clin Epidemiol201467101093110225018102
- von SchéeleBFernandezMHogueSLKwongWJReview of economics and cost-effectiveness analyses of anticoagulant therapy for stroke prevention in atrial fibrillation in the USAnn Pharmacother201347567168523606551
- KasmeridisCApostolakisSEhlersLRasmussenLHBorianiGLipGYCost effectiveness of treatments for stroke prevention in atrial fibrillation: focus on the novel oral anticoagulantsPharmacoeconomics2013311197198024085625
- KansalARZhengYPokoraTSorensenSVCost-effectiveness of new oral anticoagulants in the prevention of stroke in patients with atrial fibrillationBest Pract Res Clin Haematol201326222523723953910
- ManiHLindhoff-LastENew oral anticoagulants in patients with nonvalvular atrial fibrillation: a review of pharmacokinetics, safety, efficacy, quality of life, and cost effectivenessDrug Des Devel Ther20148789798
- FerreiraJMircoASystematic review of cost-effectiveness analyses of novel oral anticoagulants for stroke prevention in atrial fibrillationRev Port Cardiol201534317919125727748
- Daiichi SankyoSavaysa (edoxaban) [package insert] Available from: http://dsi.com/prescribing-information-portlet/getPIContent?productName=Savaysa&inline=trueAccessed January 2, 2016
- GiuglianoRPRuffCTBraunwaldEEdoxaban versus warfarin in patients with atrial fibrillationN Engl J Med2013369222093210424251359
- FernandezMMWangJYeXSystematic review and network meta-analysis of the relative efficacy and safety of edoxaban versus other nonvitamin K antagonist oral anticoagulants among patients with nonvalvular atrial fibrillation and CHADS2 score ≥2SAGE Open Med20153111
- MessoriAFaddaVMarateaDTrippoliSMarinaiCTesting the therapeutic equivalence of novel oral anticoagulants for thromboprophylaxis in orthopedic surgery and for prevention of stroke in atrial fibrillationInt J Clin Pharmacol Ther201553321121925295718
- VerdecchiaPAngeliFBartoliniCSafety and efficacy of non- vitamin K oral anticoagulants in non-valvular atrial fibrillation: a Bayesian meta-analysis approachExpert Opin Drug Saf201514172025311731
- SkjøthFLarsenTBRasmussenLHLipGYEfficacy and safety of edoxaban in comparison with dabigatran, rivaroxaban and apixaban for stroke prevention in atrial fibrillation: an indirect comparison analysisThromb Haemost2014111598198824577485
- FuWGuoHGuoJRelative efficacy and safety of direct oral anticoagulants in patients with atrial fibrillation by network meta-analysisJ Cardiovasc Med (Hagerstown)2014151287387925304034
- AssiriAAl-MajzoubOKanaanAODonovanJLSilvaMMixed treatment comparison meta-analysis of aspirin, warfarin, and new anticoagulants for stroke prevention in patients with nonvalvular atrial fibrillationClin Ther2013357967984.e223870607
- Biondi-ZoccaiGMalavasiVD’AscenzoFComparative effectiveness of novel oral anticoagulants for atrial fibrillation: evidence from pair-wise and warfarin-controlled network meta-analysesHSR Proc Intensive Care Cardiovasc Anesth201351405423734288
- Drugs.comUS pharmaceutical sales – Q4 20132014 Available from: http://www.drugs.com/stats/top100/salesAccessed January 2, 2016
- PatelMRMahaffeyKWGargJRivaroxaban versus warfarin in nonvalvular atrial fibrillationN Engl J Med20113651088389121830957
- LipGYKongnakornTPhatakHCost-effectiveness of apixaban versus other new oral anticoagulants for stroke prevention in atrial fibrillationClin Ther2014362192210.e2024508420
- DorianPKongnakornTPhatakHCost-effectiveness of apixaban vs. current standard of care for stroke prevention in patients with atrial fibrillationEur Heart J201435281897190624513791
- PistersRLaneDAMarinFCammAJLipGYStroke and thromboembolism in atrial fibrillationCirc J201276102289230423001018
- WangYXieFKongMCLeeLHNgHJKoYCost-effectiveness of dabigatran and rivaroxaban compared with warfarin for stroke prevention in patients with atrial fibrillationCardiovasc Drugs Ther201428657558525319314
- No authors listedRisk factors for stroke and efficacy of antithrombotic therapy in atrial fibrillation: analysis of pooled data from five randomized controlled trialsArch Intern Med199415413144914578018000 ErratumArch Intern Med1994154192254
- National Institute for Health and Clinical Excellence (NICE)Apixaban (Eliquis®) for the prevention of stroke and systemic embolism in people with non-valvular atrial fibrillation. Single technology appraisal (STA) submitted by Bristol-Myers Squibb and Pfizer1782012 Available from: http://www.nice.org.uk/guidance/ta275/documents/stroke-and-systemic-embolism-prevention-nonvalvular-atrial-fibrillation-apixaban-bristolmyers-squibb-and-pfizer2Accessed January 2, 2016
- BosMJvan RijnMJWittemanJCHofmanAKoudstaalPJBretelerMMIncidence and prognosis of transient neurological attacksJAMA2007298242877288518159057
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in AdultsExecutive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III)JAMA2001285192486249711368702
- FreemanJVZhuRPOwensDKCost-effectiveness of dabigatran compared with warfarin for stroke prevention in atrial fibrillationAnn Intern Med2011154111121041570
- AriesenMJClausSPRinkelGJAlgraARisk factors for intracerebral hemorrhage in the general population: a systematic reviewStroke20033482060206512843354
- SorensenSVKansalARConnollySCost-effectiveness of dabigatran etexilate for the prevention of stroke and systemic embolism in atrial fibrillation: a Canadian payer perspectiveThromb Haemost2011105590891921431243
- HartRGBenaventeOMcBrideRPearceLAAntithrombotic therapy to prevent stroke in patients with atrial fibrillation: a meta-analysisAnn Intern Med1999131749250110507957
- EastonJDLopesRDBahitMCApixaban compared with warfarin in patients with atrial fibrillation and previous stroke or transient ischaemic attack: a subgroup analysis of the ARISTOTLE trialLancet Neurol201211650351122572202 ErratumLancet Neurol201211121021
- HeronMHoyertDLMurphySLXuJKochanekKDTejada-VeraBDeaths: final data for 2006Natl Vital Stat Rep20095714113419788058
- MagnusonEAVilainKWangKCost-effectiveness of edoxaban vs warfarin in patients with atrial fibrillation based on results of the ENGAGE AF-TIMI 48 trialAm Heart J201517061140115026678636
- First DatabankFDB MedKnowledge: drug pricing Available from: http://www.fdbhealth.com/fdb-medknowledge-drug-pricingAccessed January 22, 2016
- Agency for Healthcare Research and QualityHealthcare Cost and Utilization Project (HCUP)2013 Available from: http://www.ahrq.gov/research/data/hcup/index.htmlAccessed January 2, 2016
- Academy of Managed Care Pharmacy (AMCP)The AMCP Format for Formulary Submissions: Version 3.1Alexandria (VA)AMCP2012 Available from: http://amcp.org/practice-resources/amcp-format-formulary-submisions.pdfAccessed January 2, 2016
- KrejczyMHarenbergJWehlingMObermannKLipGYCost-effectiveness of anticoagulation in patients with nonvalvular atrial fibrillation with edoxaban compared to warfarin in GermanyBiomed Res Int2015201587692325853142
- RognoniCMarchettiMQuagliniSLiberatoNLEdoxaban versus warfarin for stroke prevention in non-valvular atrial fibrillation: a cost-effectiveness analysisJ Thromb Thrombolysis201539214915424973057
- MearnsEDolehYColemanCICost-effectiveness of high-dose edoxaban compared to adjusted-dose warfarin for prevention of stroke and systemic embolism in non-valvular atrial fibrillationPoster presented at: European Society for Cardiology Congress 2014August 30–September 3, 2014Barcelona, Spain
- MenschAStockSStollenwerkBMüllerDCost effectiveness of rivaroxaban for stroke prevention in German patients with atrial fibrillationPharmacoeconomics201533327128325404426
- MoraisJAguiarCMcLeodEChatzitheofilouIFonseca SantosIPereiraSCost-effectiveness of rivaroxaban for stroke prevention in atrial fibrillation in the Portuguese settingRev Port Cardiol201433953554425241380
- KrejczyMHarenbergJMarxSObermannKFrölichLWehlingMComparison of cost-effectiveness of anticoagulation with dabigatran, rivaroxaban and apixaban in patients with non-valvular atrial fibrillation across countriesJ Thromb Thrombolysis201437450752324221805
- RognoniCMarchettiMQuagliniSLiberatoNLApixaban, dabigatran, and rivaroxaban versus warfarin for stroke prevention in non-valvular atrial fibrillation: a cost-effectiveness analysisClin Drug Investig2014341917
- KleintjensJLiXSimoensSCost-effectiveness of rivaroxaban versus warfarin for stroke prevention in atrial fibrillation in the Belgian healthcare settingPharmacoeconomics2013311090991824030788
- HarringtonARArmstrongEPNolanPEJrMaloneDCCost-effectiveness of apixaban, dabigatran, rivaroxaban, and warfarin for stroke prevention in atrial fibrillationStroke20134461676168123549134
- KansalARSharmaMBradley-KennedyCDabigatran versus rivaroxaban for the prevention of stroke and systemic embolism in atrial fibrillation in Canada: comparative efficacy and cost-effectivenessThromb Haemost2012108467268222898892
- LeeSAngladeMWPhamDPisacaneRKlugerJColemanCICost-effectiveness of rivaroxaban compared to warfarin for stroke prevention in atrial fibrillationAm J Cardiol2012110684585122651881
- EdwardsSJHamiltonVNhereraLTrevorNBartonSRivaroxaban for the Prevention of Stroke and Systemic Embolism in People with Atrial Fibrillation: A Single Technology AppraisalLondonBMJ-TAG2011
- WellsGCoyleDCameronCTherapeutic Review: Safety, Effectiveness, and Cost-Effectiveness of New Oral Anticoagulants Compared with Warfarin in Preventing Stroke and Other Cardiovascular Events in Patients with Atrial FibrillationOttawaCanadian Collaborative for Drug Safety, Effectiveness and Network Meta-Analysis2012 Available at http://cadth.ca/media/pdf/NOAC_Therapeutic_Review_final_report.pdfAccessed January 2, 2016
- LanitisTCottéFEGaudinAFKachanerIKongnakornTDurand-ZaleskiIStroke prevention in patients with atrial fibrillation in France: comparative cost-effectiveness of new oral anticoagulants (apixaban, dabigatran, and rivaroxaban), warfarin, and aspirinJ Med Econ201417858759824831811
- ZhengYSorensenSVGonschiorAKComparison of the cost-effectiveness of new oral anticoagulants for the prevention of stroke and systemic embolism in atrial fibrillation in a UK settingClin Ther2014361220152028.e225438722
- CoyleDCoyleKCameronCCost-effectiveness of new oral anticoagulants compared with warfarin in preventing stroke and other cardiovascular events in patients with atrial fibrillationValue Health201316449850623796283
- CopeSClemensAHammèsFNoackHJansenJPCritical appraisal of network meta-analyses evaluating the efficacy and safety of new oral anticoagulants in atrial fibrillation stroke prevention trialsValue Health201518223424925773559
- LipGYLarsenTBSkjøthFRasmussenLHIndirect comparisons of new oral anticoagulant drugs for efficacy and safety when used for stroke prevention in atrial fibrillationJ Am Coll Cardiol201260873874622575324
- CameronCCoyleDRichterTSystematic review and network meta-analysis comparing antithrombotic agents for the prevention of stroke and major bleeding in patients with atrial fibrillationBMJ Open201446e004301
- PinkJPirmohamedMHughesDAComparative effectiveness of dabigatran, rivaroxaban, apixaban, and warfarin in the management of patients with nonvalvular atrial fibrillationClin Pharmacol Ther201394226927623619028
- BakerWLPhungOJSystematic review and adjusted indirect comparison meta-analysis of oral anticoagulants in atrial fibrillationCirc Cardiovasc Qual Outcomes20125571171922912382
- SchneeweissSGagneJJPatrickARChoudhryNKAvornJComparative efficacy and safety of new oral anticoagulants in patients with atrial fibrillationCirc Cardiovasc Qual Outcomes20125448048622787066
- RasmussenLHLarsenTBGraungaardTSkjøthFLipGYPrimary and secondary prevention with new oral anticoagulant drugs for stroke prevention in atrial fibrillation: indirect comparison analysisBMJ2012345e709723129490
- ManthaSAnsellJAn indirect comparison of dabigatran, rivaroxaban and apixaban for atrial fibrillationThromb Haemost2012108347648422740145
- CanestaroWJPatrickARAvornJCost-effectiveness of oral anticoagulants for treatment of atrial fibrillationCirc Cardiovasc Qual Outcomes20136672473124221832
- SullivanPWLawrenceWFGhushchyanVA national catalog of preference-based scores for chronic conditions in the United StatesMed Care200543773674915970790
- SullivanPWSlejkoJFSculpherMJGhushchyanVCatalogue of EQ-5D scores for the United KingdomMed Decis Making201131680080421422468
- EckmanMHRosandJGreenbergSMGageBFCost-effectiveness of using pharmacogenetic information in warfarin dosing for patients with nonvalvular atrial fibrillationAnn Intern Med20091502738319153410
- VilainKRMagnusonEALiHCosts and cost-effectiveness of carotid stenting versus endarterectomy for patients at standard surgical risk: results from the Carotid Revascularization Endarterectomy Versus Stenting Trial (CREST)Stroke20124392408241622821614
- YouJHNovel oral anticoagulants versus warfarin therapy at various levels of anticoagulation control in atrial fibrillation – a cost-effectiveness analysisJ Gen Intern Med201429343844624132628