Abstract
Background
Several risk scores were developed for acute coronary syndrome (ACS) patients, but their use is limited by their complexity.
Purpose
The purpose of this study was to identify predictors at admission for in-hospital mortality in ACS patients in western Romania, using a simple risk-assessment tool – the new Canada acute coronary syndrome (C-ACS) risk score.
Patients and methods
The baseline risk of patients admitted with ACS was retrospectively assessed using the C-ACS risk score. The score ranged from 0 to 4; 1 point was assigned for the presence of each of the following parameters: age ≥75 years, Killip class >1, systolic blood pressure <100 mmHg, and heart rate >100 bpm.
Results
A total of 960 patients with ACS were included, 409 (43%) with ST-segment elevation myocardial infarction (STEMI) and 551 (57%) with non-ST-segment elevation acute coronary syndrome (NSTE-ACS). The C-ACS score predicted in-hospital mortality in all ACS patients with a C-statistic of 0.95 (95% CI: 0.93–0.96), in STEMI patients with a C-statistic of 0.92 (95% confidence interval [CI]: 0.89–0.94), and in NSTE-ACS patients with a C-statistic of 0.97 (95% CI: 0.95–0.98). Of the 960 patients, 218 (22.7%) were aged ≥75 years. The proportion of patients aged ≥75 years was 21.7% in the STEMI subgroup and 23.4% in the NSTE-ACS subgroup (P>0.05). Age ≥75 years was significantly associated with in-hospital mortality in ACS patients (odds ratio [OR]: 3.25, 95% CI: 1.24–8.25) and in the STEMI subgroup (OR >3.99, 95% CI: 1.28–12.44). Female sex was strongly associated with mortality in the NSTE-ACS subgroup (OR: 27.72, 95% CI: 1.83–39.99).
Conclusion
We conclude that C-ACS score was the strongest predictor of in-hospital mortality in all ACS patients while age ≥75 years predicted the mortality well in the STEMI subgroup.
Keywords:
Introduction
Patients admitted with acute coronary syndromes (ACSs) have significant variable in-hospital outcomes.Citation1–Citation3 They have different responses and vulnerabilities to adverse events with various therapies administered at presentation. An accurate baseline risk score applied to these patients may help decide on the best treatments to reduce mortality.Citation1,Citation2
At the initial examination of the patients with symptoms of ACS, the clinical decisions are founded on the history, physical examination, electorcardiogram, and laboratory data. After hospital admission, new decisions are taken based on the clinical evolution.Citation4 Prediction of mortality in ACS is decisive in setting up the therapeutic management to improve outcome.
Several risk scores have been elaborated, the most accepted being the Global Registry of Acute Coronary Events (GRACE) and thrombolysis in myocardial infarction (TIMI) risk scores.Citation5–Citation7 Although these risk scores are well recognized and validated by several studies, their application in clinical practice remains confined. An important limitation to the use of the GRACE score is the fact that it requires a calculator and the results of several laboratory data to appreciate the risk.Citation7 The Canada acute coronary syndrome (C-ACS) risk-assessment score was elaborated recently and was found to be easy to apply and to perform well in risk assessment.Citation8
The aim of the present study was to identify clinical variables associated with in-hospital mortality in ACS patients, using a simple risk-assessment tool – the new C-ACS risk score.
Patients and methods
Patient selection
The study population consists of all consecutive ACS patients admitted to the Cardiology Clinic of Timisoara Clinical Emergency City Hospital from January 2000 to December 2015. The patients with unstable angina and non-ST-segment elevation myocardial infarction formed the non-ST-segment elevation acute coronary syndrome (NSTE-ACS) subgroup, while the patients with ST-segment elevation myocardial infarction (STEMI) were included in the STEMI subgroup.
Data extraction
Data collection was performed retrospectively from hospital records by trained data collection personnel. Baseline data were age, sex, Killip class at admission, initial heart rate (HR), initial systolic blood pressure (SBP), laboratory data, 12 leads resting electrocardiogram, and medical history. Medical history included data regarding current or recent smoking, hypertension, dyslipidemia, and diabetes mellitus.
Definition of covariates
STEMI was diagnosed in the presence of ischemic symptoms lasting >20 minutes at rest within 24 hours before admission and at least in one of the following conditions: persistent ST-segment elevation ≥1 mm in more than two contiguous electrocardiographic leads, documented new or presumed new left bundle-branch block, or documented isolated posterior myocardial infarction.Citation1
NSTE-ACS was diagnosed in the presence of ischemic symptoms lasting >20 minutes at rest within 24 hours before admission and positive cardiac markers (either creatine kinase-MB or troponin above the local laboratory-specific upper limit of normal or positive bedside troponin assay).Citation2
A patient was diagnosed with systemic arterial hypertension when found with high blood pressure during hospitalization (≥140/90 mmHg) or when taking antihypertensive therapy for a previous diagnosis of hypertension.Citation9
Dyslipidemia was diagnosed in patients with raised total cholesterol level (≥190 mg/dL), low-density lipoprotein cholesterol ≥115 mg/dL, raised triglyceride >150 mg/dL, reduced high-density lipoprotein cholesterol (<40 mg/dL in males and <50 mg/dL in females), or following a specific treatment for these lipid abnormalities.Citation10
Diabetes mellitus was diagnosed in the presence of any one of the following conditions: glycated hemoglobin ≥6.5%, fasting plasma glucose level ≥126 mg/dL, and plasma glucose ≥198 mg/dL 2 hours after 75 g oral glucose load.Citation11
Based on physical examination, the ACS patients were ranked into one of four Killip classes in the following way: Class 1 – no clinical signs of heart failure; Class 2 – mild heart failure with limited rates in the lungs, a third heart sound present, and elevated jugular venous pressure; Class 3 – with acute pulmonary edema; Class 4 – cardiogenic shock (with SBP <90 mmHg) and signs of peripheral vasoconstriction (oliguria, cyanosis, or sweating).Citation12
The C-ACS score includes clinical parameters that are easily reached at the first medical examination, at home, in the ambulance, or in the emergency department. Its great convenience is the fact that it has no need for an electrocardiogram or laboratory data. The C-ACS score ranges from 0 to 4, 1 point is assigned for the occurrence of each one of the subsequent variables: age ≥75 years, Killip class >1, SBP <100 mmHg, and HR >100 bpm. This score was deducted from the acute myocardial infarction in QuebecCitation13 and C-ACS-1Citation8 registries. It was recently validated in the Gulf Registry of Acute Coronary Events.Citation14
We estimated the initial risk of in-hospital mortality using the C-ACS risk-assessment score and estimated the discriminatory capacity of the C-ACS risk score by calculating the C-statistics for the total ACS group and the different ACS subgroups (NSTE-ACS and STEMI). The predicted mortality rates were compared with the observed ones.
Follow-up and outcomes
In-hospital deaths were assessed as adverse outcomes. Mortality was defined as all-cause deaths during hospitalization.
Statistical analysis
Data were collected and analyzed using the MedCalc 12.3.0.0 statistical software for Windows. Data were given as mean ± standard deviation (SD) when normally distributed and as frequency and percentage for categorical variables. Associations between baseline variables were evaluated using one-way analysis of variance or chi-square tests. For assessing the involvement of each variable in the studied outcomes, univariate and multivariate logistic regression models were established. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated using Cox proportional hazards models. Covariates considered for potential prognostic impact included age, sex, Killip class, HR at admission, SBP at admission, diabetes mellitus, hypertension, recent or current smoking, and C-ACS score at admission. Multivariate logistic regression analysis with forward stepwise method was used for all initial parameters that were associated with in-hospital mortality in univariate analysis. Receiver–operating characteristic (ROC) curves were utilized to determine the optimal sensitivity and specificity of the analyzed parameters. The discrimination ability of the analyzed parameters was estimated by the C-statistic, which is equivalent to the area under the ROC curve. A model with C-statistic >0.75 is considered to have a meaningful discriminatory ability. A P-value of <0.05 was considered as the threshold for statistical significance. All P-values are results of two-tailed tests.
Ethics
The study was approved by the ethics commission at City Hospital Timisoara, Romania. Written informed consent was not required as all data were abstracted anonymously.
Results
The study population included 960 ACS patients, 22% being women. The mean age was 68±11 years (range 35–85 years), 22.7% having an age ≥75 years. Of the total ACS cohort, 42.6% presented with STEMI and 57.4% with NSTE-ACS. Comorbid conditions were common. The clinical characteristics of the study patients are shown in . We observed that STEMI patients tended to be younger, of male sex, with current or recent smoking history, with lower SBP, and higher HR at presentation. The C-ACS score for all ACS patients was 0.62±0.78, being significantly higher in STEMI vs NSTE-ACS patients (P<0.001). In-hospital mortality was 11.8% in the study group, significantly higher in the STEMI subgroup (14.9%) than in the NSTE subgroup (9.6%), P<0.02. The mortality rate was also significantly higher in patients aged ≥75 years vs those <75 years in the study group (OR =1.71, 95% CI: 1.16–2.54, P=0.006) and in the STEMI subgroup (OR =4.25, 95% CI: 2.57–7.01, P<0.0001).
Table 1 Clinical characteristics of the study patients stratified by ACS presentation
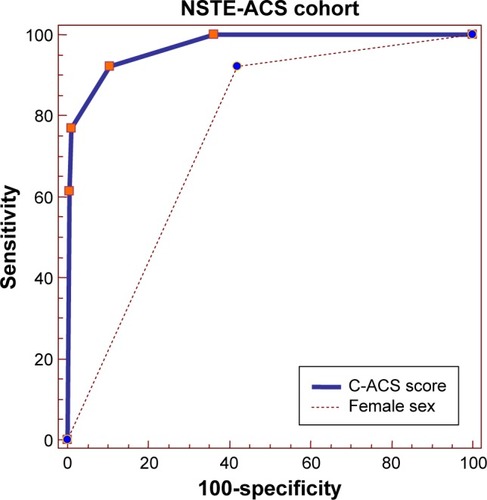
shows the observed in-hospital mortality according to the C-ACS score and the category of ACS. We observed a progressive increase in hospital mortality correlated to an increasing C-ACS score, in all ACS presentations. The predicted mortality was somewhat higher than observed mortality, but the difference was not statistically significant ().
Figure 1 Rate of in-hospital mortality stratified by C-ACS score and type of ACS.
Abbreviations: C-ACS, Canada acute coronary syndromes score; ACS, acute coronary syndrome; NSTE-ACS, non-ST-segment elevation acute coronary syndrome; STEMI, ST-segment elevation myocardial infarction.
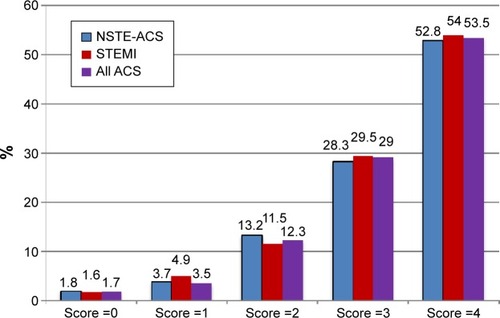
Figure 2 Comparison of observed and predicted in-hospital mortality (by C-ACS score) in the total ACS group.
The baseline variables associated with in-hospital mortality in all ACS are presented in . The ACS patients who died were more frequently older, females, smokers, with a Killip class >1, and were more likely to have at presentation an SBP <100 mmHg and an HR >100 bpm. The mean C-ACS score was significantly higher among the dead ACS patients (3.02 vs 0.54, P<0.0001). The STEMI patients who died were also more likely to be older, hypertensive, smokers, with a Killip class >1, dyslipidemia, and presented more frequently with SBP <100 mmHg and an HR >100 bpm. Their mean C-ACS score was 2.80 vs 0.61 in the STEMI survivors (P<0.0001). The NSTE-ACS patients who did not survive were more frequent females, with diabetes mellitus, a Killip class >1, and had lower SBP and higher HRs at admission. Their mean C-ACS score was 3.3, comparative to 0.48 in the NSTE-ACS survivors (P<0.0001, ).
Table 2 Univariate relationship between baseline variables and in-hospital mortality
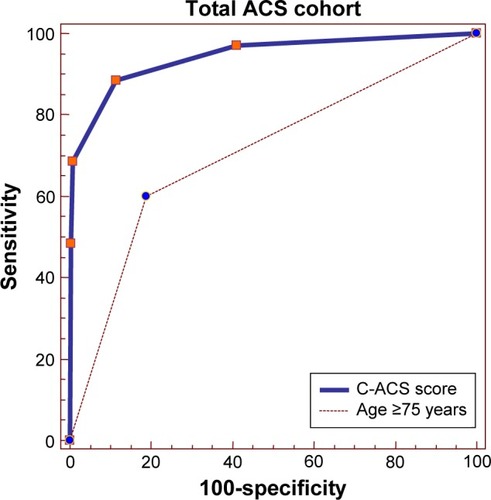
At multivariate logistic regression, we found two independent predictors of in-hospital mortality in the total ACS cohort: the C-ACS score (P<0.0001) and the age ≥75 years (P=0.016). The C-ACS score had the greatest power of discrimination in the whole ACS group, with a C-statistic of 0.94 (95% CI: 0.92–0.95). The C-statistic for age ≥75 years was 0.70 (95% CI: 0.67–0.73). The ROC curves of these variables are presented in .
Figure 3 Receiver–operating characteristic (ROC) curves for C-ACS and age ≥75 years as independent predictors of in-hospital mortality in the total ACS cohort.
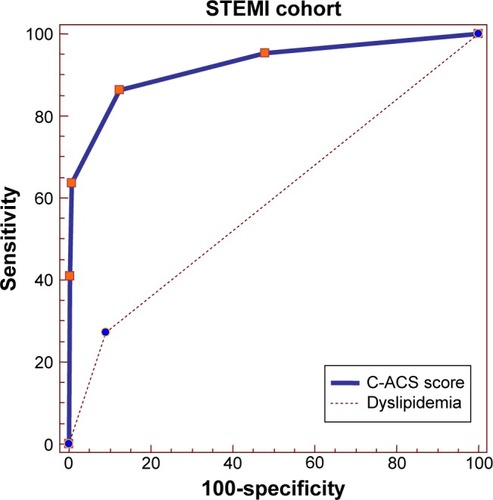
In the STEMI cohort, multivariate logistic regression also retained two independent predictors of in-hospital mortality: C-ACS score (P<0.0001) and the presence of dyslipidemia (P=0.005). The best discriminative value was observed for C-ACS score, with a C-statistic of 0.92 (95% CI: 0.89–0.94). Dyslipidemia had a C-statistic of 0.59, 95% CI: 0.54–0.63, ).
Figure 4 Receiver–operating characteristic (ROC) curves for C-ACS and dyslipidemia as independent predictors of in-hospital mortality in the STEMI cohort.
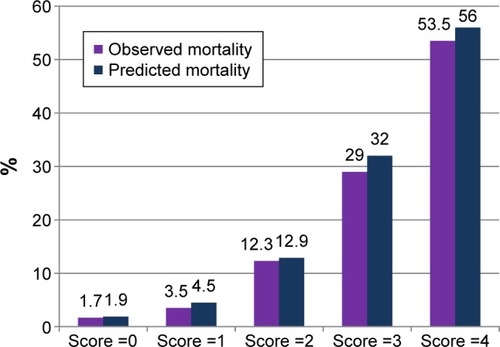
In the NSTE-ACS subgroup, multivariate logistic regression identified two independent predictors of in-hospital mortality: C-ACS score (P<0.0001) and female sex (P=0.016). Discriminative power had both the C-ACS score, with a C-statistic of 0.97 (95% CI: 0.95–0.98) and the female sex, with a C-statistic of 0.75 (95% CI: 0.73–0.78), as shown in .
Discussion
Our study was exclusively hospital based, with a retrospective recruitment of all ACS patients hospitalized in our clinic from 2000 to 2015. The mean age of the ACS was 68±11 years, 22% were women, and 22.7% were aged ≥75 years. In the Romanian Register of STEMI (RO_STEMI) patients (1997–2009) that included 19,510 patients, the mean age was 63±12 years, 32% of the patients were women, and 23.6% were aged ≥75 years.Citation15 In-hospital mortality was 11.79%, with differences between geographical regions (9%–13%). Mortality in STEMI patients aged ≥75 years was not analyzed in this registry.
Chronological age is an independent risk factor for adverse outcomes in many conditions and is often included in risk indices.Citation16 However, the assessment of C-ACS score emerged as a superior predictor when compared with chronological age, respectively, with age ≥75 years, which represents only one parameter included in the C-ACS score.
To our knowledge, this is the first study to endorse the C-ACS score in a broad spectrum of ACS patients in Romania. Comparing the predicted with the observed in-hospital mortality, we found out that, despite its simplicity, the C-ACS score enabled an accurate early risk stratification in all ACS patients.
The C-ACS score is an easy and practical risk score that includes only clinical data available at the first medical examination. In contrast to other risk-assessment tools, the C-ACS score provides an accurate estimation of risk applicable to all categories of ACS.
Over the past decades, several ACS risk estimation tools have been elaborated, developed, and validated. The GRACE score has showed an excellent performance in predicting both short- and long-term mortalities.Citation5,Citation17–Citation19 This risk score is appropriate for use in both STEMI and NSTE-ACS. Its main weakness is that it is relatively difficult to evaluate and it requires a calculator that is not always available in the daily clinical practice and also requires the results of certain laboratory data, for instance, an electrocardiogram, cardiac biomarkers, and serum creatinine levels, which may not be available at the first medical contact. The TIMI score is also applicable for use in both STEMI- and NSTE-ACS patients.Citation20,Citation21 It is easier to calculate than the GRACE score, but it also requires access to the cardiac markers and an electrocardiogram. The predictive power of the TIMI score was revealed to be poorer when compared to GRACE score.Citation6
The great advantage of the C-ACS score is that it only needs demographic and basic hemodynamic data. Regardless of the score’s simplicity, it is very useful in stratifying the risk level of ACS patients in the emergency department. It can also be applied at the patient’s home or in the ambulance, helping with the decision to send the patient to a hospital with facility of percutaneous coronary intervention (when necessary) and to choose the best medical therapy. The C-statistic for the C-ACS score was 0.94 (95% CI: 0.92–0.95) in the total ACS cohort, 0.92 (95% CI: 0.89–0.94) in STEMI patients, and 0.97 (95% CI: 0.95–0.98) in the NSTE-ACS patients.
Another risk stratification score based on demographic and initial hemodynamic data is the TIMI Risk Index. It uses age, HR, and SBP and it assigns the ACS patients into one of five risk categories. Each risk category of the STEMI patients is associated with a 24-hour, in-hospital, and 30-day mortality rate.Citation21 TIMI Risk Index was also validated in patients with NSTE-ACS.Citation22
These simpler risk stratification scores in ACS patients, welcomed by the busy clinicians, may be however less accurate when compared to the more complex ones.Citation23,Citation24 They are useful as initial risk-assessment tools, at the first medical examination, and should be followed during hospitalization by increasingly sophisticated risk evaluations.
The primary objective of a risk-prediction score is its forthcoming use in ACS patients to adapt therapy in agreement with the risk category. Until now, only limited data exist about the effect of risk assessment on mortality using traditional risk stratification scores, such as GRACE or TIMI.Citation7 Accordingly, the use of risk scores in the management of NSTEMI ACS patients was assigned by the European Society of Cardiology guidelines for a class I, with a level of evidence B,Citation2 while the American College of Cardiology/American Heart Association guidelines designated this procedure for class IIa, with a level of evidence B.Citation25
Conclusion
Our study showed that the C-ACS risk score performed well when used to evaluate the ACS patients using exclusively clinical data at first medical examination. Despite its simplicity, this risk-assessment tool was useful in all types of ACS. Age ≥75 years was associated with in-hospital mortality in the total ACS cohort and in the STEMI subgroup while female sex was associated with in-hospital mortality in the NSTE-ACS subgroup. Future studies are necessary to evaluate prospectively the C-ACS score regarding its impact on ACS therapy and subsequently on hospital mortality. We believe that the C-ACS risk score is satisfactory to guide routine clinical practice and to perform research activities concerning ACS treatment strategies.
Limitations of the study
This study has several limitations, the most important one being the fact that it is based on data collected at the level of a single center. However, the advantage of this study design was that it allowed a unitary analysis of the medical records of all patients hospitalized during the analyzed 15 years. Another limitation is related to the use of the C-ACS risk score, that, although is easy to apply, lacks precision, being more a categorical than a continuous scoring system. One of its variables, the Killip class evaluation, is totally dependent on the clinical evaluation and expertise of the examiner. We chose to use this risk score because it was applicable to the data we found in all medical records while the GRACE risk score was used in Romania only since 2012, when the European Society of Cardiology Guidelines for the management of ACSs were published.Citation1
Author contributions
AP, DAB, and MCT – conception and design of the study, statistical analysis and interpretation of data, revising the manuscript for intellectual content, and drafting the article. IMC – design of the manuscript, help in drafting manuscript, and interpretation of data. FC – acquisition and interpretation of data. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
We would like to thank attending physicians for fulfilling reports for all admitted patients and for imputting the patients’ data into electronic databases.
Disclosure
The authors report no conflicts of interest in this work.
References
- Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC)StegGJamesSKESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevationEur Heart J2012332569261922922416
- RoffiMPatronoCColletJPESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevationEur Heart J20163726731526320110
- ThygesenKAlpertJSJaffeASThe Writing Group on behalf of the Joint ESC/ACCF/AHA/WHF Task Force for the Universal Definition of Myocardial InfarctionThird universal definition of myocardial infarctionEur Heart J2012332551256722922414
- CaliffRMPieperKSLeeKLPrediction of 1-year survival after thrombolysis for acute myocardial infarction in the global utilization of streptokinase and TPA for occluded coronary arteries trialCirculation2000101192231223810811588
- ElbarouniBGoodmanSGYanRTCanadian GRACE/GRACE (2) InvestigatorsValidation of the Global Registry of Acute Coronary Event (GRACE) risk score for in-hospital mortality in patients with acute coronary syndrome in CanadaAm Heart J200915839239919699862
- D’AscenzoFBiondi-ZoccaiGMorettiCTIMI, GRACE and alternative risk scores in acute coronary syndromes: a meta-analysis of 40 derivation studies on 216,552 patients and of 42 validation studies on 31,625 patientsContemp Clin Trials20123350751422265976
- BuenoHFernández-AvilésFUse of risk scores in acute coronary and EZ-Avil’syndromesHeart20129816216822156037
- HuynhTKouzSYanATCanada acute coronary syndrome risk score: a new risk score for early prognostication in acute coronary syndromesAm Heart J2013166586323816022
- ManciaGFagardRNarkiewiczK2013 ESH/ESC Guidelines for the management of arterial hypertensionEur Heart J2013342159221923771844
- The Task Force for the management of dyslipidemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS)ReinerZCatapanoALESC/EAS Guidelines for the management of dyslipidemiasEur Heart J2011321769181821712404
- World Health OrganizationDefinition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycemia Available from: https://www.idf.org/webdata/docs/WHO_IDF_definition_diagnosis_of_diabetes.pdfAccessed March 5, 2016
- KouroshSDianaSHassanJPrediction of survival after myocardial infarction using Killip classInt J Clin Med20123563568
- PiloteLLavoieFHoVEisenbergMJChanges in the treatment and outcomes of acute myocardial infarction in Quebec, 1988–1995CMAJ200011313610920727
- Al FalehHFAlsheikh-AliAAUllahASyndrome risk score for hospital mortality in the Gulf registry of acute coronary events-2Clin Cardiol201538954254726418408
- Tatu-ChitoiuGBirkheadJLindahlBAcute Coronary Syndromes Snapshot 2009: Management and In-Hospital Outcome of STEMI Throughout ESC Member CountriesStockholmCongress of the European Society of Cardiology20105012
- FreiheitEAHoganDBEliasziwMDevelopment of a frailty index for patients with coronary artery diseaseJ Am Geriatr Soc2010581526153120633198
- GrangerCBGoldbergRJDabbousOPredictors of hospital mortality in the global registry of acute coronary eventsArch Intern Med20031632345235314581255
- LuoJGYangMHanLJiaXChenLWZhaoYValidity of the GRACE score for 6-month death or reinfarction after presentation with acute myocardial infarction in patients 80 years of age and olderCoron Artery Dis20132453754123965947
- FoxKADabbousOHGoldbergRJPrediction of risk of death and myocardial infarction in the six months after presentation with acute coronary syndrome: prospective multinational observational study (GRACE)BMJ2006333109117032691
- AntmanEMCohenMBerninkPJThe TIMI risk score for unstable angina/non-ST elevation MI: a method for prognostication and therapeutic decision makingJAMA200028483584210938172
- MorrowDAAntmanEMCharlesworthATIMI risk score for ST-elevation myocardial infarction: a convenient, bedside, clinical score for risk assessment at presentation: an intravenous nPA for treatment of infarcting myocardium early II trial substudyCirculation20001022031203711044416
- MorrowDAAntmanEMGiuglianoRPA simple risk index for rapid initial triage of patients with ST-elevation myocardial infarction: an InTIME II substudyLancet20013581571157511716882
- WiviottSDMorrowDAFrederickPDNational Registry of Myocardial InfarctionApplication of the thrombolysis in myocardial Infarction risk index in non–ST-segment elevation myocardial infarction: evaluation of patients in the National Registry of Myocardial InfarctionJ Am Coll Cardiol2006471553155816630990
- YanATYanRTTanMRisk scores for risk stratification in acute coronary syndromes: useful but simpler is not necessarily betterEur Heart J2007281072107817437970
- AmsterdamEAWengerNKBrindisRG2014 AHA/ACC guideline for the management of patients with non–ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines [published correction appears in J Am Coll Cardiol. 2014;64:2713–2714]J Am Coll Cardiol201464e139e22825260718